Abstract
Background
The improved outcome of extremity soft tissue sarcoma patients surgically treated until 2007 at the authors’ institution was previously reported. This study updates the analysis at a later follow-up and extends the patients’ cohort to assess changes in outcomes over time for extremity and superficial trunk soft tissue sarcoma (ESTSTS) treated at a single referral center.
Methods
All consecutive patients with primary localized adult-type ESTSTS surgically treated at the authors’ institution between 1987 and 2017 were included and divided into group 1 (1987–2002) and group 2 (2003–2017) according to primary surgery year. Crude cumulative incidence (CCI) of sarcoma-specific mortality (SSM), local recurrence (LR), and distant metastases (DM) were calculated in a competing-risks framework. DM-free survival (DMFS) and post-DM survival were also assessed.
Results
The study identified 2382 patients. The median follow-up was 104 months (range, 63–127 months), and the post-DM follow-up was 76 months (range, 37–126 months). Since 2003, an increased adoption of preoperative treatments was observed: the use of chemotherapy, radiotherapy and combined chemoradiotherapy went from 10.5% to 23.7%, from 1.7% to 17.8%, and from 1% to 11.8% respectively. This change in treatment strategies was associated to an improvement in CCI-SSM (27.8% vs 19.5%; P < 0.001), CCI-LR (14.1 vs 7.5%; P < 0.001), DMFS (57.9% vs 65.8%; P = 0.004), and post-DM (12.2% vs 20.1%; P = 0.012), but not in CCI-DM.
Conclusions
Increased adoption of preoperative treatments and greater availability of medical agents in the recent years were associated to better outcomes. New treatments are eagerly awaited for further improvement of outcome for ESTSTS patients because no major changes have been observed since 2003.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Extremity and superficial trunk wall soft tissue sarcomas (ESTSTS) are a group of rare solid tumors accounting for approximately 0.5% of all adult malignant neoplasms.1 Their rarity together with their high histologic variability (>70 histologic types) constitute the main challenges for the management of these tumors and clinical research in this field. Nonetheless, during the past decades, efforts have been made to identify prognostic factors and tailor ESTSTS treatment accordingly.2
In the latter years, we have exploited available multimodal treatments, with a preference for preoperative treatments, with the aim to fine tune the approach to high-risk disease.3,4,5,6,7 In 2011 we reported the improved outcomes of patients with soft tissue sarcomas (STSs) of the extremity treated at our center between 1987 and 2007,8 and we noted a specific change in 2003, when the preference for the neoadjuvant setting had started.
In this study, we extended the time period to 2017 and updated the analysis with a longer follow-up period to assess possible further changes in survival of ESTSTS patients during recent years. Outcome trends according to histologic subgroups were also explored.
Methods
The study enrolled all consecutive adult patients with primary localized ESTSTS who underwent surgery with curative intent at Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy between January 1987 and December 2017. The study excluded patients with atypical lipomatous tumor/well-differentiated liposarcoma, classic dermatofibrosarcoma protuberans, desmoid tumor, Ewing sarcoma, or alveolar/embryonal rhabdomyosarcoma as well as patients with STSs located in the head and neck, mediastinum, abdominal cavity, or breast.
Clinical data were collected from a prospectively maintained institutional database. The data retrieved included gender, age at diagnosis, site (upper extremity, trunk wall, lower extremity, girdle), size, depth, histologic type, malignancy grade (1, 2, 3), margin status at pathology, (neo)adjuvant treatments, isolated limb perfusion (ILP), amputations, and reconstructions (vascular, plastic, and other).
Size was defined as the longest diameter at final pathology for untreated tumors, while it was defined as the longest measurement between imaging at diagnosis and final pathology for all tumors managed with any form of preoperative treatment before definitive surgery.Tumors were classified as superficial or deep according to the involvement of the investing fascia.
Histologic classification was based on 2020 World Health Organization (WHO) criteria9 and grouped into the following ten categories: dedifferentiated and pleomorphic liposarcoma (DD/pleom LPS), leiomyosarcoma (LMS), myxoid liposarcoma (MLPS), malignant peripheral nerve sheath tumor (MPNST), myxofibrosarcoma (MFS), synovial sarcoma (SS), undifferentiated pleomorphic sarcoma (UPS), solitary fibrous tumor (SFT), vascular sarcoma (vascular), and others.
All the tumors were graded according to the Fédération Nationale des Centres de Lutte Contre Le Cancer (FNCLCC) criteria (grades 1, 2, and 3).10 Surgical excisions were defined as macroscopically incomplete (R2) or complete according to the presence or absence of gross residual disease. Macroscopically complete resections were further categorized according to the closest surgical margin as either microscopically positive (tumor within 1 mm from the inked surface: R1) or negative (absence of tumor within 1 mm from the inked surface: R0).
The indication for radiotherapy (RT) was determined by a multidisciplinary team when a higher risk of relapse was estimated on clinical grounds. However, no prospectively selected criteria were used. External beam radiation was used in all such cases, and doses ranged from 45 to 70 Gy (median, 60 Gy). Chemotherapy (ChT) was administered at the discretion of the multidisciplinary institutional sarcoma board or as part of ongoing clinical trials. Anthracycline-based regimens were used, in most cases combined with ifosfamide. A shift toward the use of either ChT or RT in the preoperative setting was started in 2003, together with the concurrent administration of both treatments for higher-risk patients.
In the absence of any event after treatment, a regular follow-up evaluation was performed generally at least every 4 months for the first 2 years, every 6 months for the following 3 years, and then yearly.
Local relapse and distant metastases were prospectively recorded as events of interest on the basis of strongly suggestive imaging (magnetic resonance imaging [MRI] or computed tomography [CT] scan) evaluated at the time of follow-up visits.
Statistical Methods
Patients characteristics, treatments, and counts of outcomes’ events were described using descriptive statistics and compared by means of the standardized mean difference (SMD). The SMD is considered indicative of a possible between-group imbalance when it approaches a value of about 0.3. The SMD and the relevance of the observed differences should be assessed from a clinical point of view.11
The primary objectives of the study were incidences of sarcoma-specific mortality (SSM), local relapse (LR), and distant metastasis (DM). The secondary objectives of the study were distant metastasis-free survival (DMFS), overall distant metastasis incidence (DMI), and post-distant metastasis (post-DM) survival.
Survival and incidence times started from the date of surgery on the primary tumor for all but the post-DM survival end point. Crude cumulative incidence (CCI) curves of SSM, LR, and DM, were estimated in a competing risk setting using cumulative incidence estimates and compared using the Gray test. The study estimated CCI curves of DMI using cumulative incidence estimates considering only death as a competing event to calculate the overall incidence of DM regardless whether DM occurred as the first event, concomitant to LR or after LR, and they were compared using the Gray test. The DMFS and post-DM survival curves were estimated using the Kaplan-Meier method, and the curves were compared using the log-rank test. The study defined SSM as the time to death due to disease and death not directly attributable to disease evaluated as competing events. LR (DM) was defined as the time to the first LR (DM) and death without recurrence or DM (LR) were considered as competing events.
In DMI models, DM was defined as the time to the first DM, and death due to any cause was considered as the only competing event. DMFS was defined as the time to DM or death, whichever occurred first. Concomitant LR and DM were considered as DM. Post-DM survival was defined as the time between the first DM event (even as not-first event) to death due to any cause.
Overall and subgroup analyses by histology were performed. For all primary and secondary outcomes, comparisons between two 15-year groups (1987–2002, 2003–2017) and between six 5-year subgroups (1987–1992, 1993–1997, 1998–2002, 2003–2007, 2008–2012, 2013–2017) according to the date of primary surgery were performed.
Multivariable Cox models including 15- or 5-year groups and age, tumor size, operation period, depth, histologic type, malignancy grade, margin status, and ChT and RT (none, pre- with or without post-treatment, only post-treatment) also were performed to assess the association between the aforementioned covariates and SSM, CCI-LR, CCI-DM, and DMFS. In the CCI-LR, CCI-DM, and DMI models, the interaction term between ChT and RT was included. In three further models for SSM and DMFS/DMI, LR/DM and LR were added as time-dependent covariates, respectively. Numeric variables such as patient age and tumor size were modeled using three-knots restricted cubic splines.12 Proportionality assumption was visually inspected by evaluating the regression line slope of scaled Schoenfeld residuals against the log-transformed time for all covariates and models.
Univariable Fine and Gray models were used to perform the histology-specific subgroup analyses. In the post-DM survival analysis, the median follow-up values were estimated with the reverse Kaplan-Meier method13 on the basis of overall survival data for the whole cohort and the 15-year groups, and on the post-DM data for the patients who experienced a DM event.
The statistical analyses were performed with SAS (SAS Institute, Cary, NC, USA) and R software (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient and Tumor Characteristics
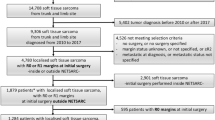
Overall, 2392 patients with primary and localized ESTSTS were surgically treated with curative intent at our institution between 1987 and 2017. The analysis excluded 10 patients who underwent R2 resection, and the remaining 2382 patients constituted the basis of the current study. Baseline patient, tumor, and treatment characteristics by 15- and 5-year subgroups are shown respectively in Tables 1 and S1.
The median follow-up period was 104 months (interquartile range [IQR], 63–127 months) in the whole series, 139 months (IQR, 120–187 months) in group 1, and 82 months (IQR, 50–113 months) in group 2. The median post-metastasis follow-up periodwas 76 months (IQR, 37–126 months) in the whole series, 139 months (IQR, 93–185 months) in group 1, and 58 months (IQR, 21–100 months) in group 2.
Incidence of Sarcoma-Specific Mortality
For the 2382 patients, 639 deaths were recorded. Of these deaths, 475 (74.3%) were sarcoma-related and thus considered in our analyses. The first event before sarcoma-related death was LR for 85 patients (17.9%), DM for 343 patients (72.2%), and synchronous LR and DM for 44 patients (9.3%). Three patients died of sarcoma-related complications and never experienced DMs or LR.
The number of sarcoma-related deaths and the 5- and 10-year SSM estimates before and since 2003 are reported in Table 2. The CCI-SSM curves (Fig. 1, panel A) differed significantly according to period (P < 0.001). The corresponding results of the subgroup analyses are shown in Table S2 and Fig. S1 (panel A), respectively.
The results of the Cox multivariable models for CCI-SSM, including the 15-year groups, are shown in Table 3. The results of a similar model for CCI-SSM, including the 5-year groups are shown in Table S3. The results of the Cox multivariable models for DMFS including LRs and DMs as additional time-dependent variables are shown in Table S4.
Incidence of Local Recurrence
Overall, 295 patients experienced LR. Of these 295 patients, 214 (72.5%) had LR as the first event. Overall, 130 patients had LR alone, whereas 165 patients had LR and DMs (LR anticipating DMs in 84 patients, concurrent in 48 patients, and posterior in 33 patients). In the first and second groups, 62 and 68 patients respectively had an LR alone, whereas 88 and 77 patients had LR and DM (LR anticipating DM in 47 and 37 patients, concurrent in 21 and 27 patients, and posterior in 20 and 13 patients, respectively).
The 5- and 10-year CCI-LR values by period are reported in Table 2. The CCI curves (Fig. 1, panel B) differed significantly according to period (P < 0.001). The corresponding results of the subgroup analyses are shown in Table S2 and Fig. S1 (panel B), respectively.
The results of the Cox multivariable models for CCI-LR, including the 15- and 5-year groups are shown in Tables 3 and S3, respectively.
Incidence of Distant Metastasis
Overall, 654 patients experienced DM. Of these 654 patients, 570 (87.2%) had DM as the first event. In 48 (8.4%) of the 570 patients, DM and LR were synchronous. Overall, 489 patients had only DM, whereas 165 had DM and LR, as reported earlier. In the first and second groups, respectively 157 and 332 patients had a DM alone, whereas 88 and 77 patients had an LR and a DM, respectively, as reported earlier.
The 5- and 10-year CCI-DM values by period are reported in Table 2. The CCI-DM curves (Fig. 1, panel C) did not differ significantly according to period (P = 0.625). The corresponding results of the subgroup analyses are shown in Table S2 and Fig. S1 (panel C), respectively.
The results of the Cox multivariable models for CCI-DM, including the 15- and 5-year groups, are shown in Tables 3 and S3, respectively.
Distant Metastasis-Free Survival and Distant Metastasis Incidence
The number of all the first DM events (occurring either as the first event or not), and the 5- and 10-year DMFS estimates before and since 2003 are reported in Table 2. Distant metastasis-free survival was significantly longer since 2003 (P = 0.004; Fig. 2). The Kaplan-Meier curves of DMFS according to 5-year groups are shown in Fig. S2.
The results of the Cox multivariable models for DMFS including the 15- and 5-year groups are shown in Table 3 and Table S3, respectively.
The results of the Cox multivariable models for DMFS including LR as an additional time-dependent variable are shown in Table S5.
The same analysis of the overall incidence of DM (DMI) is reported in the supplementary material and is consistent with that for DMFS (Fig. S3; Tables S5 and S6).
Post-Distant Metastasis Survival
The number of all the first DM events (occurring either as the first event or not) and the 5- and 10-year post-DM survival estimates before and since 2003 are reported in Table 2. Post-DM survival improved significantly since 2003 (P = 0.012; Fig. 3). The Kaplan-Meier curves of post-DM survival according to 5-year groups are shown in Fig S4. The median time from metastases to death was 19 months (IQR, 8–56 months) overall; 15 months (IQR, 8–43 months) in group 1, and 22 months (IQR, 9–67 months) in group 2.
Outcome by Histology
A comparison of outcomes before and since 2003 by histologic type showed CCI LR improvement in all but LMS and SS histologies; CCI DM improvement in none with UPS as a worsening group and a feeble improvement in the vascular sarcoma group; CCI SSM improvement in myxoid LPS, vascular sarcoma, MPNST, and SS. A significantly better DMFS was observed only in SS and a nonsignificant improvement in vascular sarcoma was also observed. Finally, due to generally smaller differences and fewer patients in each histology subgroup, only weak improvements in post-DM survival were detectable in all histologies except DD/pleom LPS and vascular sarcoma (Table 4 and Figs. S5–S10).
Discussion
In this series of patients affected by primary localized adult-type ESTSTS treated surgically at a single institution during a 30-year period, a significant improvement in SSM and CCI-LR after 2003 was observed. In addition, whereas CCI-DM as the first event did not change over time, DMFS and post-DM survival were significantly longer after 2003.
This was a retrospective study with all the limitations thereof only partially overcome by the use of prospectively collected data. Some changes were made in the definition of the most common types over the years. Therefore, some differences in histologic distribution among the study periods may be attributable to the refinement of their classification rather than to a change in the case mix.
Moreover, neither chemotherapy regimens nor radiotherapy doses and fields could be factored into our analysis. In addition, we lacked data about patients who progressed with preoperative treatments and became inoperable. However, this is a rare event (about 2% of the cases), as shown also in studies testing neoadjuvant ChT in high-risk localized ESTSTS.5,14
Finally, staging methods certainly have evolved during 30 years (e.g. from CT scan to helical CT scan) and this may have determined an earlier detection of distant spread in the recent years with some risk of confounding the comparison. In addition an improvement in surgical technique and better imaging identification certainly might have contributed to a better outcome. However if these confounders had played a major role in improving outcome, a lower percentage of marginal resections as well as a lower incidence of distant metastases as the first event (Will Rogers’ phenomenon15) would have been found in the latter period. Instead, neither of these were observed.
To the best of our knowledge, this was one of the largest series of patients with ESTSTS treated at single referral center during a 30-year period, and thanks to the large cohort size, outcomes according to histology group also could be attempted.
These results confirm and update the outcome over time reported in our previous analysis on extremity STS.8 Indeed, 5-year SSM has dropped by more than one third since 2003. As shown by analysis of subgroups, the maximum outcome improvement in terms of SSM as well as CCI-LR and DMFS was recorded since 2003. Consistently, a similar study investigating a cohort of patients treated from 1982 to 2001 could not find any change in disease-specific mortality during the considered time frame. This is similar to our findings, as changes were seen starting from 2003.16 Notably, this time point marked a change in the treatment approach to ESTSTS at our center, whereas no clinically significant differences in patients, tumor characteristics, or quality of surgical margins were observed over time. These changes can be summarized as follows: (1) a gradual shift toward the use of RT in the preoperative setting, with the proportion of preoperative RT rising from 1.7% to 17.8% after 2003, (2) an increase in the use of chemotherapy overall, mainly attributable to an increase in preoperative ChT administration, and (3) an increased use combined RT and ChT in the preoperative setting, from 1% in the first period to 11.8 % in the last period.
The administration of RT in association with conservative limb-sparing surgery is known to reduce the LR risk compared with surgery alone, especially for high-risk patients,3,4,17 and this was confirmed in our series because it was found to be significantly associated with a lower CCI-LR. Less is known about whether the timing of RT (pre- vs postoperative) has any further impact on local control. The only available randomized study showed no difference in LR between the two study arms, but the study was not powered to examine this.18,19
In the current study, improvement in local control was accompanied by an increase in RT administration in the preoperative setting. Indeed, some retrospective studies already have shown that preoperative RT may offset the negative prognostic impact of positive surgical margins.20,21,22,23 Therefore, it may be hypothesized that although the administration of preoperative RT generally does not differ from the administration of postoperative RT in terms of local control (even if the dogma of RT as standard treatment after negative margins resections is presently challenged, considering no RT at all also as an option in selected cases and in a referral institution with expert sarcoma practitioner inputs available24), this is not true in the case of close/positive margins, in which preoperative RT seems better.
Our study is consistent, with improvement of local control paralleled by an increase in the use of preoperative RT over time, showing no change in the proportion of R1 resections. In the absence of randomized data, our results add evidence in favor of preoperative RT, especially for borderline resectable cases or when close/positive margins over a critical structure can be anticipated on clinical grounds. This should also support the current shift toward the use of RT in the preoperative setting overall.
The percentage of patients who received ChT increased from 19.1% to 32.2%, mostly due to its increased use in the preoperative setting. However, this was not paralleled by a reduction in the incidence of DM as the first event. Indeed, the role of ChT in the treatment of localized ESTSTS is debated. Several randomized controlled trials (RCTs) conducted in the last 30 years have led to conflicting results, with some smaller trials showing a benefit of ChT and other larger trials not reporting any benefit at all.25,26,27,28,29 However, most of the studies that failed to show a benefit in overall survival had important limitations such as the inclusion of unselected patient populations (all sizes and malignancy grades) and the administration of suboptimal chemotherapy schedules,25,26,27 whereas more recent data have led to consideration of a role for ChT in improving systemic control for selected high-risk patients.7,30
Our study was retrospective and therefore could not give a definitive contribution to this debate. The patients who received ChT were selected over the years via a multidisciplinary decision, mostly on clinical grounds. It may be speculated that those who received ChT were the patients thought to be at higher risk. The lack of an effect may simply reflect this selection bias.
Notably, however, a shift toward the use of ChT in the preoperative setting was observed together with its concurrent use with preoperative RT. Data about the feasibility of this concurrent approach also were previously provided.31 Although proof of a better effect against the metastastic risk of the two combined methods in the preoperative setting compared with the postoperative setting is lacking, data derived from a randomized study on neoadjuvant ChT are available, which again support the use of the combined method whenever a close/positive margin can be anticipated or preservation of a critical structure is the goal.
Why then was an improvement in local control associated with an improvement in SSM with no difference in the incidence of DM? First, a reduction in LRs may itself have some direct impact on SSM because LR at critical sites may lead directly to death.
Second, it should be noted that although CCI-DM did not change over time, an improvement in DMFS and a trend toward a better overall DMI were in fact observed. The CCI-DM data are a direct measure of the short-term effects of tumor biology, which governs the early related outcome. It is indeed true that no major advances in first-line therapies were made during these 30 years. In contrast, DMFS measures the long-term effects of both tumor biology and local control. In other words, a reduction in LR may have determined a reduction in the risk of distant spread occurring after a LR, resulting in a better DMFS and DMI. It then is tempting to believe that the improvement in DMFS observed over time was related to an increased use of preoperative treatments able to reduce LR in high-risk cases. Further studies may help clinicians understand this.
Finally, a significant improvement in post-DM survival was observed since 2003, and this also may have contributed to the improvement in SSM. In fact, 5-year post-DM survival increased from 19.9 % before 2003 to 26.6 % after 2003. These gains might reflect the advancement in the treatment strategy for DM that has occurred in the last 15 years, such as a better exploitation of available cytotoxic agents and the introduction of targeted therapies particularly active for some histologic types.32 The sub-analysis of histologic types mostly confirmed these results.
In conclusion, with all the highlighted limitations, our data suggest that the outcome improvement observed since the year 2003 seems to be related to a wider use of neoadjuvant methods and changes in treatments for metastatic patients. Of course, new treatment methods are eagerly awaited, especially for high-risk ESTSTS patients.
References
Jemal A, Tiwari RC, Murray T, et al. Cancer statistics. CA Cancer J Clin. 2004;54:8–29.
Roland CL, van Houdt W, Gronchi A. The Landmark Series: multimodality treatment of extremity sarcoma. Ann Surg Oncol. 2020;27:3672–82.
Beane JD, Yang JC, White D, Steinberg SM, Rosenberg SA, Rudloff U. Efficacy of adjuvant radiation therapy in the treatment of soft tissue sarcoma of the extremity: 20-year follow-up of a randomized prospective trial. Ann Surg Oncol. 2014;21:2484–9.
Yang JC, Chang AE, Baker AR, et al. Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. J Clin Oncol. 1998;16:197–203.
Gronchi A, Palmerini E, Quagliuolo V, et al. Neoadjuvant chemotherapy in high-risk soft tissue sarcomas: final results of a randomized trial from Italian (ISG), Spanish (GEIS), French (FSG), and Polish (PSG) sarcoma groups. J Clin Oncol. 202038:2178–86.
Gronchi A, Stacchiotti S, Verderio P, et al. Short, full-dose adjuvant chemotherapy (CT) in high-risk adult soft tissue sarcomas (STS): long-term follow-up of a randomized clinical trial from the Italian Sarcoma Group and the Spanish Sarcoma Group. Ann Oncol. 2016;27:2283–8.
Gronchi A, Ferrar S, Quagliuolo V, et al. Histotype-tailored neoadjuvant chemotherapy versus standard chemotherapy in patients with high-risk soft-tissue sarcomas (ISG-STS 1001): an international, open-label, randomised, controlled, phase 3, multicentre trial. Lancet Oncol. 2017;18:812–22.
Gronchi A, Miceli R, Colombo C, et al. Primary extremity soft tissue sarcomas: outcome improvement over time at a single institution. Ann Oncol. 2011;22:1675–81.
IARC WHO Classification of Tumours-Soft Tissue and Bone Tumours. Vol 3. 5th ed. Lyon: IARC press; 2020.
Trojani M, Contesso G, Coindre JM, et al. Soft‐tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer. 1984;33:37–42.
Flury BK, Riedwyl H. Standard distance in univariate and multivariate analysis. Am Stat. 1986;40:249–51.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17:343–6.
Gronchi, A. et al. Short, full-dose adjuvant chemotherapy in high-risk adult soft tissue sarcomas: a randomized clinical trial from the Italian Sarcoma Group and the Spanish Sarcoma Group. J Clin Oncol. 2012;30:850–6.
Feinstein AR, Sosin DM, Wells CK. The Will Rogers phenomenon: stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med. 1985;312:1604–8.
Weitz J., Antonescu CR, Brennan MF. Localized extremity soft tissue sarcoma: improved knowledge with unchanged survival over time. J Clin Oncol. 2003;21:2719–25.
Callegaro D, Miceli R, Bonvalot S, et al. Impact of perioperative chemotherapy and radiotherapy in patients with primary extremity soft tissue sarcoma: retrospective analysis across major histological subtypes and major reference centres. Eur J Cancer. 2018;105:19–27.
O’Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet. 2002;359:2235–41.
Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol. 2005;75:48–53.
Gronchi A, Verderio P, De Paoli A, et al. Quality of surgery and neoadjuvant combined therapy in the ISG-GEIS trial on soft tissue sarcomas of limbs and trunk wall. Ann Oncol. 2013;24:817–23.
Dagan R, Indelicato DJ, McGee L, et al. The significance of a marginal excision after preoperative radiation therapy for soft tissue sarcoma of the extremity. Cancer. 2012;118:3199–207.
Potter BK, Hwang PF, Forsberg JA, et al. Impact of margin status and local recurrence on soft-tissue sarcoma outcomes. J Bone Joint Surg Am. 2013;95:e151.
Willeumier J, Fiocco M, Nout R, et al. High-grade soft tissue sarcomas of the extremities: surgical margins influence only local recurrence not overall survival. Int Orthop. 2015;39:935–41.
Fiore M, Ford S, Callegaro D, et al. Adequate local control in high-risk soft tissue sarcoma of the extremity treated with surgery alone at a reference centre: should radiotherapy still be a standard? Ann Surg Oncol. 2018;25:1536–43.
Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet. 1997; 350:1647–54.
Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M. A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer. 2008;113:573–81.
Woll PJ, Reichardt P, Le Cesne A, et al. Adjuvant chemotherapy with doxorubicin, ifosfamide, and lenograstim for resected soft-tissue sarcoma (EORTC 62931): a multicentre randomised controlled trial. Lancet Oncol. 2012;13:1045–54.
Pasquali S, Pizzamiglio S, Touati N, et al. The impact of chemotherapy on survival of patients with extremity and trunk wall soft tissue sarcoma: revisiting the results of the EORTC-STBSG 62931 randomised trial. Eur J Cancer. 2019;109:51–60.
Bramwell V, Rouesse J, Steward W, et al. Adjuvant CYVADIC chemotherapy for adult soft tissue sarcoma: reduced local recurrence but no improvement in survival: a study of the European Organization for Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group. J Clin Oncol. 1994;12:1137–49.
Pasquali S, Gronchi A. Neoadjuvant chemotherapy in soft tissue sarcomas: latest evidence and clinical implications. Ther Adv Med Oncol. 2017;9:415–29.
Palassini E, Ferrari S, Verderio P, et al. Feasibility of preoperative chemotherapy with or without radiation therapy in localized soft tissue sarcomas of limbs and superficial trunk in the Italian sarcoma group/grupo español de investigación en sarcomas randomized clinical trial: three versus five cycles of full-dose epirubicin plus ifosfamide. J Clin Oncol. 2015;33:3628–34.
Frezza AM, Stacchiotti S, Gronchi A. Systemic treatment in advanced soft tissue sarcoma: what is standard, what is new. BMC Med. 2017;15:109.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest. No reprints will be available from the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Danieli, M., Barretta, F., Fiore, M. et al. Refining the Approach to Patients with Primary Soft Tissue Sarcoma of the Extremities and Trunk Wall: Outcome Improvement Over Time at a Single Institution. Ann Surg Oncol 29, 3274–3286 (2022). https://doi.org/10.1245/s10434-021-11189-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11189-2