Abstract
Background
Tumor human leukocyte antigen class I (HLA-I) expression plays an important role in T cell-mediated tumor rejection. Loss of HLA-I is associated with cancer progression and resistance to immunotherapy, including antibodies blocking programmed death-1/programmed death-ligand 1 (PD-1/PD-L1) signaling. Our objective was to analyze a correlation between HLA-I, tumor immune infiltration, and PD-L1/PD-1 axis in bladder cancer in association with the clinicopathologic features of patients.
Methods
We analyzed 85 cryopreserved bladder tumors by immunohistochemistry to investigate the expression of HLA-I, PD-L1, PD-1, CD3, CD8, and CXC chemokine receptor 4 (CXCR4). The results were correlated with tumor stage and other clinicopathologic variables of patients.
Results
We found a strong positive correlation between tumor HLA-I expression and infiltration with CD3+ and CD8 + T cells. PD-L1 expression was positive in 15.5% of tumors and heterogeneous in 40.5%, and was linked to a more advanced tumor stage. The majority of HLA-I-positive/heterogeneous tumors also expressed PD-L1 and PD-1, which were significantly correlated with each other and with lymphocyte infiltration. Interestingly, the analysis of the simultaneous expression of both markers revealed that 85.2% of tumors with a positive/heterogeneous HLA-I phenotype and negative for PD-L1 were mostly non-invasive, representing a ‘tumor rejection’ immune phenotype.
Conclusions
High tumor HLA-I expression with absence of PD-L1 provides bladder cancer with an immune rejection mechanism. Evaluation of PD-L1 and HLA-I together should be considered in bladder cancer and may provide a new predictive biomarker of tumor invasiveness and of the response to ‘immune checkpoint’ therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bladder cancer is currently the eleventh most diagnosed tumor worldwide, with an age-adjusted incidence rate (100,000 habitants/year) of 8.9 for men and 2.2 for women. In the EU, this incidence rate is 27 for men and 6 for women, with the highest frequency reported in Spain (41.5 for men and 4.8 for women), and the lowest incidence reported in Finland (18.1 for men and 4.3 for women).1,2,3 Approximately 75% of patients with bladder cancer have non-muscle-invasive disease, i.e. tumors confined to the mucosa (stage Ta, CIS) or submucosal areas (stage T1). These tumors have a high occurrence due to a longer survival period and reduced risk of mortality compared with muscle-invasive tumors (stages T2–T4).2
Despite advances in the prevention of the disease and its progression, it is difficult to predict a benign or more aggressive course of the disease. A better understanding of the mechanisms of the immune control over tumor progression and the routes of cancer immune escape may help to predict tumor behavior and develop new biomarkers of cancer evolution.4
The cells of the immune system infiltrate into the tumor mass and tumor microenvironment, leading to the activation of complex interactions with the tumor cells and modulating the ability of the tumor to grow and disseminate.5 The antitumor immune response usually requires activation of CD8 + T lymphocytes with tumor antigenic peptides presented by the cell surface human leukocyte antigen class I (HLA-I) complex. At the same time, CD4 + T cells can stimulate the function of CD8 + T lymphocytes or negatively regulate the infiltration of these cells into the tumor via upregulation of co-inhibitory molecules, including cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), PD-L1 and PD-1, and by production of immunosuppressive cytokines (transforming growth factor-β, interleukin-10).6,7,8,9
Frequently, tumor cells lose normal cell surface expression of HLA-I molecules by different molecular mechanisms. It is one of the key routes of immune escape allowing cancer cells to proliferate and develop tumor nodes with high metastatic capacity and low immunogenicity.10 These HLA-I alterations have been described in different types of cancer, including bladder cancer, with different frequency, ranging from 15% in renal cancer to 80% in colorectal cancer.11,12 These alterations can produce a total or partial HLA-I loss (HLA-I haplotype or loss of a specific allele) and can be classified into genetic/irreversible and regulatory/reversible defects.13 HLA-I downregulation produced by regulatory alterations can be corrected by cytokines, but genetic aberrations in HLA-I genes can cause a resistance to cancer immunotherapy. Along with mutations/deletions in the β2-microglobulin (B2M; a light chain of the HLA-I complex), loss of genetic material (or loss of heterozygosity [LOH]) in chromosomes 6 and 15 (HLA-I heavy chain and B2M gene areas, respectively) represents the main molecular mechanisms leading to irreversible or ‘hard’ HLA-I aberrations.14,15 In bladder cancer, we have previously reported a coordinated downregulation of tumor expression of HLA-I heavy chain, B2M, and antigen-processing machinery (APM) components as a mechanism of low HLA-I expression.16 In addition, we detected a high incidence of LOH at chromosomes 6 and 15, which was even greater in recurrent tumors after Bacillus Calmette-Guerin (BCG) immunotherapy.17 Therefore, although urothelial carcinoma is immunotherapy responsive, the outcome can be compromised by immune escape of structural alterations causing HLA-I altered expression.
In the tumor microenvironment, there are important mechanisms of the negative control of T-cell activation, including the PD-L1/PD-1 axis of immunosuppression.7,8,9 New strategies of immunotherapy against cancer are based on blocking these ‘immune checkpoints’, leading to T-cell activation and promoting more potent antitumor immune responses.6 Since T cells play a key role in elimination of malignant cells, tumor HLA-I expression may predetermine a successful anti-PD-1/PD-L1 therapy.
However, there are no reports analyzing the role of the co-expression of tumor HLA-I and PD-L1/PD-1 molecules in the search for biomarkers linked to cancer progression and response to checkpoint blockade in bladder cancer.
In this study, we analyzed the expression of HLA-I and PDL-1 in non-metastatic bladder cancer, both alone and together, in correlation with tumor immune infiltration and in association with the clinicopathologic features of patients.
Materials and Methods
Patients and Tumor Samples
Overall, 85 bladder tumor samples were collected (between 1999 and 2014) from patients after transurethral resection of the bladder in the Urology Department of the University Hospital Virgen de las Nieves, Granada, Spain. Median follow-up time was more than 5 years. Demographic, clinical, and histological characteristics of the studied subjects and tissue samples are summarized in Table 1. Prior to the study, all medical records and tumor sections were reviewed by a uro-oncologist and a surgical pathologist. Signed informed consent, approved by the Ethics Committee of our institution, was obtained from all the patients. Tumor samples were stored in liquid nitrogen until immunohistological analysis was performed.
TNM stage was defined according to the classification of the Union for International Cancer Control (UICC),18 and tumor stage was determined according to the classification of the World Health Organization (WHO) and the International Society of Urological Pathology consensus.19
Immunohistological Analysis of Bladder Tumor Samples
Cryopreserved tumor tissue sections 4–8 μm-thick were allowed to dry at room temperature for 4–18 h, fixed in acetone at 4 °C for 10 min, and stored at − 40 °C until immunohistological analysis using the Biotin-Streptavidin System (supersensitive Multilink HRP/DAB kit; BioGenex, The Hague, The Netherlands).
Using specific mouse monoclonal antibodies, we analyzed tumor expression of the following molecules: HLA-I heavy chain/B2M cell surface complex (85 tumors; w6/32 antibody, a gift from Dr. Bodmer, Imperial Cancer Research Fund Laboratories, London, UK), lymphocyte infiltration (71 tumors; anti-CD3, clone F7.2.38 and anti-CD8, clone C8/144B, both from Dako, Glostrup, Denmark), PD-L1 (84 tumors; anti-human B7-H1, 29E.2A3 [AbD Serotec] and clone 22C3 [Merck]), PD-1 (60 tumors; BioSciences, and CXCR4 (59 tumors; Abcam). Immunolabeled tissue sections were further scanned and analyzed using a ‘Panoramic Scanner MIDI II’ and ‘Panoramic Viewer’ (3DHISTECH Ltd). Expression of the tumor-infiltrating lymphocyte markers was analyzed within the tumor mass. Total HLA-I loss was considered when < 25% of tumor cells were stained, heterogeneous when 25–75% of tumor cells were positive, and positive when > 75% of tumor cells were labeled with W6/32 mAbs, according to the criteria established by the HLA and cancer component of the 1996 International Histocompatibility Workshop.20 PD-L1 expression was defined as positive in tumor cells showing a membranous staining of any intensity in > 25% of tumor cells, heterogeneous when between 5 and 25% of tumor cells were labeled positively, and negative when < 5% of tumor cells were positive.21
Statistical Analysis
The relationship between qualitative variables was analyzed using Pearson’s Chi square test with correction for continuity, or Fisher’s exact test in cases when the validity criteria were not reached (> 20% of the expected frequencies < 5).
Differences were considered statistically significant at p < 0.05. The data were analyzed using the statistical software IBM SPSS Statistics 19 (IBM Corporation, Armonk, NY, USA).
Results
We analyzed bladder tumor samples by immunohistochemistry in order to establish the association between different characteristics of tumor immunogenicity, immune infiltration, and microenvironment (Table 2).
Depending on the pattern of immunolabeling of tumor tissues using antibodies against HLA-I, PD-1, PD-L1, and CXCR4 proteins, we were able to distinguish three types of immunolabeling patterns for each of the molecules—positive, negative, and heterogeneous (Fig. 1a, b). For the statistical analysis, in some cases we combined HLA-I and PD-L1 positive and heterogeneous tumors and compared them with negative tumors. Statistically significant differences were mostly found when we compared negative tumors with a group of tumors with positive and heterogeneous patterns.
a Representative images of bladder cancer tissue immunostaining with antibodies directed against HLA-I (w6/32 mAb), PD-L1, and CD8. b Representative images of bladder cancer tissue immunolabeling with antibodies directed against HLA-I (w6/32 mAb), PD-L1, PD-1, CD8, and CXCR4. HLA-I human leukocyte antigen class I, PD-L1 programmed death-ligand 1, PD-1 programmed death-1, CD8 cluster of differentiation 8, CXCR4 CXC chemokine receptor 4
In this study, the presence of tumor-infiltrating CD3 + and CD8 + T lymphocytes is important in the context of tumor HLA-I and PD-L1 expression. We therefore focused mostly on the analysis of intra-tumor infiltration, which has high prognostic and immunological value in cancer. In all of the studied tissue samples, high HLA-I expression correlated with strong T-cell infiltration within the tumor mass with insignificant presence of T cells on the invasive tumor margin, which is similar to our previous observations in other types of cancer.22
The percentage of tumors with negative HLA-I expression was 17.6%. A similar frequency was noted in tumors with heterogeneous HLA-I expression, while the majority of tumors were positive (64.7%). However, the anti-HLA-I antibody that we used in this study only recognizes the cell surface complex of the HLA-I heavy chain associated with the B2M light chain. Most likely, many of the analyzed tumors have additional HLA-I locus and/or allelic losses, which cannot be detected with this antibody.
We found a significant correlation between tumor HLA-I expression and infiltration with CD3 + and CD8 + T cells. Overall, 59.3% of tumors with positive/heterogeneous HLA-I expression had a high degree of lymphocyte infiltration, compared with 16.3% of HLA-I-negative tumors (p = 0.007) (Table 3).
Tumor infiltration also had a positive correlation with PD-L1 and PD-1 expression. The highest incidence of PD-L1 expression was detected in tumors with greater lymphocyte infiltration, while most of the PD-L1-negative tumors were not infiltrated with CD3 +/CD8 + T cells (p = 0.038) (Table 4). Even higher statistical significance was found between tumor T-cell infiltration and PD-1 expression, indicating that most of the tumor-infiltrating CD3 + and CD8 + T lymphocytes express these co-inhibitory molecules (p < 0.001) (Table 5).
Interestingly, 79.3% of stage T2 tumors had positive or heterogeneous PD-L1 expression compared with Ta and T1 tumors, where this expression pattern was found in only 44.4% of cases (p = 0.002) (Table 6). These data suggest that more aggressive tumors use PD-L1 expression as an immune escape mechanism to advance to muscle-invasive stage T2.
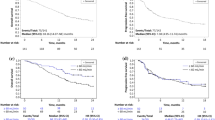
When we analyzed co-expression of HLA-I and PD-L1, we found that almost half of the studied tumors were positive/heterogeneous for both HLA-I and PD-L1, and approximately one-third were HLA-I-positive/PD-L1-negative. The double-negative and HLA-I-negative/PD-L1-positive/heterogeneous groups together represented approximately 20% of tumors (Fig. 2).
Tumors positive/heterogeneous for both HLA-I and PD-L1 demonstrated a significantly higher degree of tumor lymphocyte infiltration (68.5%, p = 0.004) (Table 7) and increased expression of PD-1 (51.5%, p = 0.001) (Table 8) compared with the remaining cases. None of the double-negative tumors showed any presence of infiltrating lymphocytes (p < 0.01) (Table 9).
In double-positive tumors, we observed an almost even number of muscle non-invasive tumors at stage Ta/T1 (51.2%) and muscle-invasive tumors at stage T2 (48.8%), compared with the remaining cases (p = 0.009) (Table 10). Notably, among tumors with the HLA-I-positive/PD-L1-negative phenotype, there were more superficial tumors at stage Ta/T1 (85.2%) and fewer tumors at the more advanced T2 stage (14.8%; p = 0.004) (Table 11). In addition, we did not find any significant correlation between the immunohistological data and tumor grade or recurrence.
Discussion
The role of altered tumor antigen presentation and HLA-I expression has recently attracted a lot of attention in light of cancer resistance to immunotherapy, especially to immune checkpoint inhibitors. Emerging data suggest that alterations in tumor antigen presentation can be a mechanism to evade antitumor immunity after immune checkpoint blockade.
In this study, using tumor immunohistology, we characterized HLA-I and PD-L1/PD-1 molecule expression, as well as lymphocyte infiltrate, in 85 bladder tumors, in correlation with the clinicopathologic features of patients. Although the majority of the tumors were positive for cell surface HLA-I, approximately 17.6% of the tumors demonstrated total loss of HLA-I expression. This number is similar to the previously reported percentage of total HLA-I in bladder tumors (25%).12 In this study, we did not analyze partial locus or allelic HLA-I alterations since we used only one antibody that recognizes a complex of HLA-I heavy chain and B2M on the surface of the tumor cells (W6/32).14
An important observation of this study is the strong correlation between HLA-I expression and tumor infiltration with CD3 + and CD8 + lymphocytes. In a recent publication, we described a similar correlation in lung cancer.21
Regarding the expression of PD-L1 in bladder cancer, there are different reports describing both positive and negative immunolabeling patterns. In our study, the majority of the tumors were positive or heterogeneous for PD-L1 expression, most of which had more advanced stage, suggesting that more aggressive tumors use PD-L1 expression as an immune escape mechanism to advance to a muscle-invasive stage. Based on published literature, the prognostic value of tumor PD-L1 expression is controversial and there is a lack of consensus on the utility of testing for PD-L1 as a predictive biomarker. According to some authors, PD-L1 expression appears to increase in higher-grade, more advanced disease, and patients with no PD-L1 expression derive some clinical benefit. On the other hand, high tumor PD-L1 expression may also be associated with an increased chance of response to immunotherapy with anti-PD-L1 antibodies, although some phase III trials have not shown PD-L1 to be a reliable predictive marker.23,24
Based on knowledge regarding the role of HLA-I expression in tumor rejection, and of the PD-L1/PD-1 axis in negative regulation of T-cell activation, one could hypothesize that the HLA-I-positive/PD-L1-negative tumor immunophenotype may promote cancer immune rejection at the early stages of bladder cancer development. Perhaps, at later stages, the emergence of another tumor phenotype (HLA-I-negative/PD-L1-positive) could facilitate tumor immune escape and progression,21 as well as metastatic dissemination. The accumulation of HLA-altered tumor phenotypes during metastatic progression, and resistance to immunotherapy, has been described in other types of cancer, including lung cancer and melanoma.25,26,27,28,29,30,31
We did not find any statistically significant correlation between HLA-I and PD-L1 analyzed separately. However, many tumors showed a heterogeneous pattern of HLA-I and PD-L1 expression and different co-expression phenotypes. Based on this, we classified tumors into four groups: HLA-I-positive/PD-L1-negative, HLA-I-negative/PD-L1-positive, double-positive, and double-negative. Statistical analysis revealed that double-positive tumors demonstrated a significantly higher degree of tumor lymphocyte infiltration, and increased expression of PD-1. This indicates that these tumors are ‘inflamed’ with a coordinated upregulation of various proinflammatory molecules. In this study, we discovered that a high percentage of tumor-infiltrating T cells express inhibitory PD-1 molecules, which represents a phenotype of an ‘exhausted lymphocyte’. The incidence of tumor PD-1/PD-L1 expression in this study is similar to a previous report.32 The expression of PD-L1 has a significant correlation with clinical response to anti-PD-1/PD-L1 antibody treatment in patients with melanoma and advanced renal cell carcinoma.33,34
Patients with HLA-I-positive/PD-L1-negative tumors demonstrated better prognosis; this immunophenotype was more frequent among muscle non-invasive tumors. Similar observations were reported in other types of malignancies, including an association with a lower incidence of tumor recurrence.35,36,37 This could suggest that the absence of PD-L1 expression is an important factor of cancer rejection, which can also serve as a predictive biomarker of less-invasive tumors and more favorable disease course. These data confirm the results demonstrating a positive correlation between tumor PD-L1 expression alone and more advanced tumor stage. In a small percentage of the studied tumors (7.15%), we detected an opposite co-expression pattern (HLA-I-negative/PD-L1-positive), which has previously been reported to be associated with more advanced lung cancer.21
At the same time, HLA-I expression seems to be an important factor of tumor rejection associated with increased lymphocyte infiltration, which changes during tumor evolution as a result of T-cell-mediated selection and elimination of HLA-I-positive tumor cells and immune escape of HLA-I-negative cells.17,22 The tumor HLA-I-positive/PD-L1-positive immunophenotype may represent an intermediate stage in this natural tumor evolution, as we have previously described in melanoma and lung cancer.21,25,26 In the early stages, positive HLA-I expression may coincide with low expression of PD-L1 (immune rejection phenotype) and progress to an escape variant with an HLA-I-negative/PD-L1-positive pattern in distant metastases (Fig. 3a, b). In addition, immunotherapy seems to induce an immune escape of tumor cells with structural genetic HLA-I alterations, which cannot be corrected by cytokines induced by immunotherapy. Previously, our group reported that recurrent bladder tumors after BCG therapy accumulate more genetic alterations in HLA-I genes (LOH-6) than tumors prior to therapy, as a result of T-cell-mediated immune selection.17
a Schematic representation of the role of tumor HLA-I and PD-L1 expression in cancer immune rejection and/or escape. b Correlation between HLA-I and PD-L1 co-expression immunophenotype and stage progression of bladder cancer. HLA-I human leukocyte antigen class I, PD-L1 programmed death-ligand 1, TCR T-cell receptor
The new generation of cancer immunotherapy aimed at eliminating the inhibitory axis of T-cell activation is currently being used in metastatic bladder cancer,38 but, in the early stages of ongoing clinical trials, it has not yet demonstrated its effectiveness.24 Our data suggest that simultaneous analysis of tumor HLA-I/PD-L1 expression might help to predict bladder cancer progression and select patients for anti-‘immune checkpoint’ immunotherapy.
Conclusions
The PD-L1/PD-1 pathway is important in cancer immunosurveillance and can potentially serve as a predictive marker for immunotherapy. HLA-I expression on tumor cells may also influence the success of anti-PD-1/PD-L1 therapy since altered tumor HLA-I expression has a high incidence in human tumors and represents a cancer immune escape mechanism. Our results show that PD-L1 is an independent factor of bladder cancer progression, suggesting that PD-L1 may be a factor promoting localized stage progression.
In addition, the majority of HLA-I-positive/PD-L1-negative tumors are at a less-advanced stage. High HLA-I is associated with greater tumor lymphocyte infiltration, and, together with low expression of PD-L1 in bladder cancer cells, represents a tumor rejection phenotype.
Based on the obtained results, we believe that the loss of HLA-I, together with upregulation of PD-L1 in bladder tumors, may be associated with poor prognosis and possibly metastatic dissemination. In case of PD-L1-positive/HLA-I-negative, more aggressive, muscle-invasive tumors, anti-PD-L1/PD-1 antibody therapy, together with upregulation of the normal expression of HLA-I (immune or gene therapy) could improve the existing protocols of bladder cancer treatment and for patient selection for immunotherapy. Additional studies and clinical trials are necessary to determine the interrelationship of HLA-I and PD-L1 in the progression of bladder cancer.
References
Ferlay J, Bray F, Forman D, et al. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10. Lyon: International Agency for Research on Cancer; 2010.
Burger M, Catto JW, Dalbagni G, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63(2):234–41.
Bosetti C, Bertuccio P, Chatenoud L, et al. Trends in mortality from urologic cancers in Europe, 1970–2008. Eur Urol. 2011;60(1):1–15.
Mendes F, Domingues C, Rodrigues-Santos P, et al. The role of immune system exhaustion on cancer cell escape and anti-tumor immune induction after irradiation. Biochimica et Biophysica Acta. 2016;1865(2):168–75.
Liu Y, Cao X. Immunosuppressive cells in tumor immune escape and metastasis. J Mol Med. 2015;94(5):509–22.
Aptsiauri N, Garcia-Lora AM, Cabrera T. MHC Class I antigens in malignant cells: immune escape and response to immunotherapy. New York: Springer Briefs in Cancer Research; 2013. p. 6.
Spranger S. Mechanisms of tumor escape in the context of the T cell-inflamed and the non-T cell-inflamed tumor microenvironment. Int Immunol. 2016;58:7250–7.
Ma W, Gilligan BM, Yuan J, Li T. Current status and perspectives in translacional biomarker reserach for PD-1/PD-L1 immune ckeckpoint blockade therapy. J Hematol Oncol. 2016;9(47):1–21.
Velcheti V, Schalper KA, Carvajal DE, et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Investig. 2014;94(1):107–16.
Aptsiauri N, Cabrera T, Garcia-Lora AM, Lopez-Nevot MA, Ruiz-Cabello F, Garrido F. MHC class I antigens and immune surveillance in transformed cells. Int Rev Cytol. 2007;256:139–89.
Cabrera T, Collado A, Fernandez MA, Ferron A, Sancho J, Ruiz-Cabello F, et al. High frequency of altered HLA class I phenotypes in invasive colorectal carcinomas. Tissue Antigens. 1998;52(2):114–123.
Cabrera T, Pedrajas G, Cozar JM, Garrido F, Vicente J, Tallada M, et al. HLA class I expression in bladder carcinomas. Tissue Antigens. 2003;62(4):324–7.
Garrido F, Cabrera T, Aptsiauri N. ‘Hard’ and ‘soft’ lesions underlying the HLA Class I alterations in cancer cells: implications for immunotherapy. Int J Cancer. 2010;127:249–56.
Maleno I, Aptsiauri N, Cabrera T, Gallego A, Paschen A, Lopez-Nevot MA, et al. Frequent loss of heterozygosity in the β2-microglobulin region of chromosome 15 in primary human tumors. Immunogenetics. 2011;63(2):65–71.
Maleno I, Romero JM, Cabrera T. LOH at 6p 21.3 region and HLA class I altered phenotypes in bladder carcinomas. Immunogenetics. 2006;58(7):503–10.
Romero JM, Jiménez P, Cabrera T, et al. Coordinated downregulation of the antigen presentation machinery and HLA class I/beta2-microglobulin complex is responsible for HLA-ABC loss in bladder cancer. Int J Cancer. 2005;113(4):605–10.
Carretero R, Cabrera T, Gil H, et al. Bacillus Calmette-Guerin immunotherapy of bladder cancer induces selection of human leukocyte antigen class I-deficient tumor cells. Int J Cancer. 2011;129(4):839–46.
Sobin LH, Gospodarowicz MK, Wittekind Ch. TNM classification of malignant tumors. UICC International Union Against Cancer. 7th ed. Wiley-Blackwell; 2009. p. 262.
Epstein JI, Amin MB, Reuter VR, Mostofi FK. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol. 1998;22:1435.
Garrido F, Cabrera T, Accolla RS, et al. HLA and cancer: 12th International Histocompatibility Workshop study. In: Charron D, ed. Genetic diversity of HLA. Functional and medical implication. In: Proceedings of the 12th international histocompatibility workshop and conference, Vol. II. Sevres: EDK; 1997. pp. 445–52.
Perea F, Sánchez-Palencia A, Gómez-Morales M, et al. HLA class I loss and PD-L1 expression in lung cancer: impact on T-cell infiltration and immune escape. Oncotarget. 2018;9(3):4120–33.
Aptsiauri N, Ruiz-Cabello F, Garrido F. The transition from HLA-I positive to HLA-I negative primary tumors: the road to escape from T-cell responses. Curr Opin Immunol. 2018;51:123–32.
Ghatalia P, Zibelman M, Geynisman DM, Plimack E. Approved checkpoint inhibitors in bladder cancer: which drug should be used when? Ther Adv Med Oncol. 2018;10:1758835918788310.
Stenehjem D, Tran D, Nkrumah MA, Gupta S. PD1/PDL1 inhibitors for the treatment of advanced urothelial bladder cancer. Onco Targets Ther. 2018;11:5973–5989.
Del Campo AB, Kyte JA, Carretero J, et al. Immune escape of cancer cells with beta2-microglobulin loss over the course of metastatic melanoma. Int J Cancer. 2014;134(1):102–13.
Zaretsky JM, Garcia-Diaz A, Shin DS et al. Mutations associated with acquired resistance to PD-1 blockade in melanoma. N Engl J Med. 2016;375(9):819–29.
Rodig SJ, Gusenleitner D, Jackson DG, et al. MHC proteins confer differential sensitivity to CTLA-4 and PD-1 blockade in untreated metastatic melanoma. Sci Transl Med. 2018;10(450):pii: eaar3342.
Sade-Feldman M, Jiao YJ, Chen JH, et al. Resistance to checkpoint blockade therapy through inactivation of antigen presentation. Nat Commun. 2017;8(1):1136.
Garrido F, Ruiz-Cabello F, Aptsiauri N. Rejection versus escape: the tumor MHC dilemma. Cancer Immunol Immunother. 2017;66(2):259–71.
Garrido F, Aptsiauri N, Doorduijn EM, Garcia Lora AM, van Hall T. The urgent need to recover MHC class I in cancers for effective immunotherapy. Curr Opin Immunol. 2016;39:44–51.
Gettinger S, Choi J, Hastings K, et al. Impaired HLA class I antigen processing and presentation as a mechanism of acquired resistance to immune checkpoint inhibitors in lung cancer. Cancer Discov. 2017;7(12):1420–35.
Galatica Z, Snyder C, Maney T, et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomark Prevent. 2014;23(12):2965–70.
Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122–133.
Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–13.
Umemoto Y, Okano S, Matsumoto Y, et al. Prognostic impact of programmed cell death 1 ligand 1 expression in human leukocyte antigen class I-positive hepatocellular carcinoma after curative hepatectomy. J Gastroenterol. 2015;50(1):65–75.
Ryschich E, Nötzel T, Hinz U, et al. Control of T-cell- mediated immune response by HLA class I in human pancreatic carcinoma. Clin Cancer Res. 2005;11(2 Pt 1):498–504.
Sabbatino F, Villani V, Yearley JH, et al. PD-L1 and HLA Class I antigen expression and clinical course of the disease in intrahepatic cholangiocarcinoma. Clin Cancer Res 2016;22(2):470–78.
Bellmunt J, Powles T, Vogelzang NJ. A review on the evolution of PD-1/PD-L1 immunotherapy for bladder cancer: the future is now. Cancer Treat Rev. 2017;54:58–67.
Acknowledgments
The authors would like to thank Svitlana Zinchenko for technical support, and Dr. Teresa Cabrera for the discussion and contribution to this work. The results of this work are part of the doctoral thesis of José Francisco Flores-Martín, within the Doctoral Program in Biomedicine at the University of Granada.
Funding
This work was supported by grants from the Spanish Institute of Health Carlos III (ISCIII, Instituto Carlos III) co-financed by the European Union (FEDER-Fondo Europeo de Desarrollo Regional) [PI12/02031, PI11/01022, PI11/01386, RETIC RD 06/020, PT13/0010/0039, PI14/01978, PI16/00752, PI17/00197] and by the Junta de Andalucía, Spain [Group CTS-143].
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Flores-Martín, J.F., Perea, F., Exposito-Ruiz, M. et al. A Combination of Positive Tumor HLA-I and Negative PD-L1 Expression Provides an Immune Rejection Mechanism in Bladder Cancer. Ann Surg Oncol 26, 2631–2639 (2019). https://doi.org/10.1245/s10434-019-07371-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07371-2