Abstract
Background
Cases of thymoma with pleural dissemination are occasionally encountered, and their management is difficult. Some reports have noted that surgical treatment for dissemination is effective, although the long-term results and clinical course details remain unclear. The current study investigated the short- and long-term outcomes of surgical resection of pleural dissemination.
Methods
A retrospective review examined the medical records for 38 patients who underwent surgical resection for pleural dissemination occurring synchronously with a primary thymoma or metachronously after complete surgical resection of a primary thymoma between 1996 and 2017 at the authors’ institution. Clinical characteristics and prognostic factors were analyzed.
Results
The patients were classified into synchronous (n = 21) and metachronous (n = 17) groups. The 10-year overall survival rate was 59% for the synchronous group and 88% for the metachronous group. The median follow-up period for all the patients was 61 months (range 4–225 months). No perioperative deaths occurred. For all the patients, the 5- and 10-year overall survival rates were respectively 91% and 82%, and the 5- and 10-year relapse-free survival rates were respectively 29% and 19%. A significantly worse prognosis was observed for patients 50 years of age or older than for those younger than 50 years (p = 0.02). For 13 patients who underwent repeat resection for pleural dissemination, the prognosis was better than for those without repeat resection (p < 0.01).
Conclusion
Surgical resection of thymoma with pleural disseminated nodules can be safely performed and provides a favorable long-term outcome. Repeat resection is considered to be effective for achieving a good prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Thymoma is the most common primary malignancy occurring in the anterior mediastinum.1 The standard treatment for Masaoka stages 1 and 2 disease is primarily surgery, with a favorable outcome often achieved.2 However, patients with thymoma often experience pleural dissemination at presentation or even after resection for the primary tumor. In fact, previous reports have shown that 7% of patients with thymoma have stage 4a disease, and recurrence manifesting as pleural dissemination occurs in 7% to 19% of thymoma patients who undergo complete resection.1,3,4
A large-scale retrospective study showed that surgical resection, even when incomplete, might contribute to treatment for invasive thymoma.3 We also previously reported that re-resection was an acceptable option for patients with recurrent thymoma after undergoing initial resection.5 In other studies that focused on thymoma cases with pleural dissemination, the benefits of surgical treatment were shown.6,7,8 However, the numbers of patients in these reports were limited, and the long-term outcomes and details of the resection procedures used for dissemination remain unclear. As a leading institution in Japan, we proactively perform resection for thymoma with dissemination.
The current study analyzed the short- and long-term outcomes of resection for pleural dissemination of thymoma in patients treated at our institution within the past two decades, the largest such cohort from a single institute reported worldwide.
Methods
Patients and Methods
Between 1996 and 2017, 288 patients underwent surgical treatment for thymoma at our hospital. Of these patients, 38 (13%) underwent resection of pleural dissemination, and 21 (7%) were found to have pleural dissemination at the time of the initial resection (i.e., thymoma Masaoka stage 4a). In the current study, these patients composed the synchronous group. In addition, 17 patients underwent resection for pleural recurrence after macroscopic complete resection of thymoma initially classified as Masaoka stages 1 to 3 or 4b (without pleural dissemination) and composed the metachronous group. The clinical records of the 38 enrolled patients were retrospectively reviewed and analyzed.
The study protocol was approved by the Ethics Review Board for Clinical Studies of Osaka University (control no. 18297). The disease stage was determined using the Masaoka staging system for thymic epithelial tumors.9 All specimens obtained by surgery were reviewed by pathologists at our hospital, and the diagnosis was determined according to the classification of the World Health Organization (WHO).10 Postoperative complications were graded according to the Clavien-Dindo classification.11
Other Methods
The details of other methods are described in the attached Supplementary File.
Results
Follow-Up Period
The interval between the initial resection for pleural dissemination nodules and the latest follow-up examination of all the patients for the overall survival (OS) analysis ranged from 3 to 225 months (median, 61 months). The median follow-up period was 59 months (range 23–146 months) in the synchronous group and 63 months (range 4–225 months) in the metachronous group.
Synchronous Group: Patient Characteristics, and Clinical, Pathologic, and Surgical Factors
The patient characteristics as well as the surgical and pathologic factors of the synchronous group are shown in Table 1. Before surgery, 13 patients (62%) underwent induction chemotherapy, which was most commonly a cisplatin-based regimen with adriamycine, sisplatin, vincristine and cyclophosphamide (ADOC) (n = 5, 39%). Of the 21 patients in this group, 19 had stage 4a disease and 2 had stage 4b disease with anterior mediastinal lymph node metastasis.
The surgical method was extended thymectomy in 10 cases (48%) and thymothymectomy in 11 (52%) cases. Lung resection was required for 17 patients, with pneumonectomy (pleuropneumonectomy) performed for 3 patients, bilobectomy for 1 patients, lobectomy for 7 patients, segmentectomy for 1 patient, and partial resection for 5 patients. Macroscopic complete resection was achieved for 16 patients (76%), whereas resection was judged to be macroscopically incomplete for 5 patients. The reasons for judging resection to be incomplete in these cases were as follows: too many pleural dissemination nodules to achieve complete resection, infiltration by a disseminated nodule of the aortic arch, and nodule infiltration to the pulmonary artery. However, in two of these cases, residual disease was well controlled by postoperative radiotherapy. Resection was ultimately judged to be complete for 18 patients.
No perioperative deaths occurred. Postoperative complications at the initial resection procedure for disseminated nodules occurred for four patients (19%), including surgical-site infection, postoperative hemorrhaging (grade 3b), cardiac herniation after a pleuropneumonectomy (grade 3b), and postoperative myasthenia gravis (MG) crisis (grade 4). In 14 patients, 1 to 10 pleural dissemination nodules were found, whereas in 7 patients, 11 or more were found.
Seven patients underwent postoperative therapy (chemotherapy for 3 patients, chemotherapy and radiotherapy for 3 patients, and radiotherapy for 1 patient). For four of these patients (57%), relapse occurred. The 5- and 10-year OS rates for the synchronous group were respectively 82% and 59%.
Metachronous Group: Patient Characteristics and Clinical, Pathologic, and Surgical Factors
Table 1 presents the patient characteristics as well as the surgical and pathological factors of the metachronous group. Seven patients received adjuvant radiotherapy, and one patient received chemoradiation therapy after resection of the primary thymoma. The mean interval between primary thymoma resection and detection of pleural dissemination recurrence was 47 months (range 12–110 months). For five patients (29%), complete video-assisted thoracoscopic surgery was selected as the surgical approach. Partial pleurectomy was performed for all the patients. Nine patients had tumors that required diaphragm resection. No operative deaths occurred. One patient (7%) had a postoperative complication, a postoperative pulmonary fistula (grade 3b), at the initial resection of disseminated nodules. In 12 patients, 1 to 10 pleural dissemination nodules were found, whereas 11 or more were found in 5 patients. Histologic “upgrading,” defined as migration of the WHO class assigned at the time of the initial diagnosis of thymoma to the WHO class assigned at the time of recurrence resection, was noted in six patients (35%). The 5- and 10-year OS rates for the metachronous group were respectively 100% and 88%.
Long-Term Outcomes for All Patients
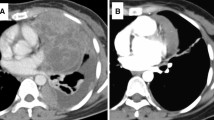
During the observation period, six deaths occurred (including 4 tumor-related deaths) in the synchronous group and 1 death occurred (not tumor-related) in the metachronous group. For all the patients, the 5- and 10-year OS rates were respectively 89% and 71% (Fig. 1a), whereas the 5- and 10-year recurrence-free survival (RFS) rates were respectively 30% and 20% (Fig. 1b).
Clinical Course After Initial Resection of Thymoma Pleural Dissemination
The clinical courses of our patients after initial resection of thymoma pleural dissemination are presented in Fig. 2. For 20 patients, relapse in the pleural cavity developed after initial resection for disseminated nodules, including 13 in the synchronous group and 7 in the metachronous group. The average interval between the first resection of disseminated nodules and relapse was 24 months in the synchronous group, and 32 months in the metachronous group. In the entire cohort, 13 patients (34%) underwent re-resection for disseminated pleural nodules, defined as two or more repeated resection procedures for pleural dissemination nodules.
Table 2 presents the characteristics of our patients with and without resection. The group without resection included three patients who received chemotherapy, five who received radiotherapy (RT), one who received both chemotherapy and RT, and four who received no treatment. The patient characteristics did not differ significantly between the patients with and those without repeat resection. To evaluate the validity of repeat resection for disseminated nodules, we also compared the OS between these two groups using the Kaplan–Meier method (Fig. S1). The patients who underwent repeat resection showed a better prognosis than those without repeat resection (p < 0.01). During the clinical course, surgical resection for disseminated regions was ultimately abandoned for 13 patients because the nodules were technically difficult to resect in 6 patients, distant metastasis was present in 4 patients, and the general condition of 1 patient was too poor for a surgical procedure to be tolerated. In addition, one patient died of an unrelated disease during the observation period, and one patient is considering treatment at this writing.
Univariate Analyses
To determine the association with the long-term outcome, a univariate analysis was performed using age (< 50 vs ≥ 50 years), gender (male vs female), macroscopic complete resection (yes vs no), time to recurrence from the first resection for thymoma disseminated nodules (< 24 vs ≥ 24 months), histologic type (B3 vs others), size of the resected nodule (< 2.5 vs ≥ 2.5 cm), dissemination type (synchronous vs metachronous), presence of perioperative complications (yes vs no), adjuvant chemotherapy (yes vs no), and treatment era (1996–2006 vs 2007–2017) as factors (Table 3). Age was the only factor shown to have a significant association with the long-term outcome (10-year OS, 10-year RFS). However, regarding RFS, the patients with 11 disseminated nodules or more tended to show a better survival than those with 10 nodules or fewer, although the difference was not significant.
Discussion
In the current study, both the feasibility and favorable long-term outcomes of surgical treatment for pleural dissemination of thymoma were demonstrated. We also found that patients who underwent repeat resection tended to have a better OS than those who did not undergo this surgery.
In Haniuda et al.1 reported a 5-year OS rate of 47% and a 10-year OS rate of 35% in a series of 15 patients who underwent resection for pleural dissemination recurrence. Thereafter, several authors added reports showing a 5-year OS of 43% to 92% and a 5-year RFS of 13% to 90% in such cases.7,12,13,14
Murakawa et al.7 were the first to divide patients into synchronous and metachronous groups according to the timing of dissemination detection and to conduct an analysis of the midterm results after surgical resection. However, their findings were limited by the relatively small number of patients examined (n = 13) and the short observation period (31 months).
Recently, using large-scale databases, Japanese and Italian researchers have shown the results from resection of thymoma with pleural dissemination,15,16 although the treatment strategy for thymoma with pleural dissemination differs among institutions and the details of the clinical courses of each patient could not be demonstrated in these nationwide investigations. The current study is the largest retrospective analysis reported by a single institution worldwide, so our findings clarifying the long-term results of surgical treatment and the clinical course details after resection performed under a consistent policy are considered to be valuable. We noted 5- and 10-year OS rates of 91% and 82%, respectively, and observed 5- and 10-year RFS rates of 29% and 19%, respectively. Such findings concerning the long-term outcome are quite compatible with other results previously reported.6,7,8
According to some studies reporting the prognosis of patients who have thymoma with pleural dissemination, macroscopic complete resection is an important factor influencing the rates of survival and recurrence.8,15,16 In our study as well, patients who underwent macroscopic complete resection tended to have a good prognosis (p = 0.06). Okuda et al.15 also noted that the number of pleural disseminated nodules (≥ 11) was a prognostic factor. In our cohort, the 10-year OS was 51% for patients with 11 or more disseminated pleural nodules and 79% for those with 10 or fewer disseminated pleural nodules, which was quite similar to their results. Regarding the mechanism underlying these phenomena, it is considered that even if macroscopic complete resection is performed, patients who have microscopic dissemination will eventually experience relapse. Therefore, it is speculated that patients with 11 lesions or more tend to have more microscopic nodules than patients with 10 or fewer lesions.
Both disease status and patient general condition differ between synchronous and metachronous dissemination cases, making it necessary to consider the treatment strategy separately for these two groups. For patients with synchronous dissemination, we proactively perform preoperative chemotherapy or steroid therapy, followed by surgery.17 Surgical resection is aggressively indicated for these patients because the reported long-term outcome after chemotherapy alone is limited (5-year OS rate, 63%),18 and it also has been shown that the prognosis of invasive and/or advanced thymoma patients who undergo surgical resection, even when incomplete, is better than that of patients without resection.19
To achieve a better rate of complete resection rate and improve the prognosis, preoperative chemotherapy or steroid therapy should be performed.20,21 Indeed, of our 21 patients, 14 (67%) received preoperative therapy, including chemotherapy for 12 patients and steroid therapy for 2 patients, with 15 patients (86%), including all who underwent preoperative therapy, achieving complete resection.
Surgical resection also is considered the first choice of treatment for metachronous dissemination.6,16 However, preoperative therapy for these patients is not proactively indicated at our institution because those with metachronous disseminated nodules might not benefit from preoperative therapy because the resectability of the disseminated nodules does not seem to be influenced by such treatment. In terms of surgical approach for resection of dissemination, thoracoscopic surgery has recently been recognized as a viable option.
Kimura et al.22 noted that a complete video-assisted thoracoscopic surgery (VATS) approach for early-stage thymoma was feasible. However, no reports have compared complete VATS for recurrent thymoma with open thoracotomy, so its safety and effectiveness remain unknown. Because thoracoscopy is useful for detailed observations of the thoracic cavity, we have performed thoracotomy with thoracoscopic assistance in most cases. However, in the current study, this approach was applied in only 4 (27%) of 15 cases. Furthermore, the proportion of complete VATS cases was low, which was consistent with the study of Marulli et al.16 This may have been the case because disseminated nodules often are present in the cardio-phrenic angle, resulting in a difficult approach with VATS alone. Improvements in the devices used may improve the availability of a complete VATS approach for pleural dissemination.
The current results indicate that repeat resection for recurrent pleural dissemination is effective. In a comparison of OS after the initial resection between patients with and without repeat resection, the former group had a significantly better prognosis than the latter. Based on our institutional policy, we perform upfront surgery for recurrence deemed completely resectable by radiologic examinations. Therefore, recurrent disease with unifocal progression tends to be considered resectable, whereas multifocal progression tends to be considered unresectable. The general condition also is included in the criteria determining indication for re-resection. Patients who have a good general condition and can tolerate an operation are therefore candidates for re-resection.
Although selection bias should be carefully considered before interpretation of the OS findings, we consider that this favorable result for patients who underwent repeat resection supports our treatment policy to resect as much of the pleural dissemination of recurrent thymoma as possible. In fact, one patient in our series underwent six different procedures, including the initial resection of stage 4 thymoma, for resection of dissemination and showed no recurrence at the final observation time point.
Among the variables analyzed in our study, only age older than 50 years was associated with a poor OS (p = 0.02), which may be attributed to the effects of age on the performance status (PS) and surgery-related endurance. We speculate that as age increases, the feasibility of surgical resection for postoperative recurrence declines.
The current study had some limitations. First, despite our study involving the largest number of cases from a single institution worldwide, it remains difficult to draw a definitive conclusion regarding the significance of surgical resection for thymoma with pleural dissemination. Furthermore, the current risk factor analysis might have been insufficient because few deaths occurred due to the relatively long survival associated with this disease. A larger study population may be needed to overcome these limitations.
In addition, this study analyzed data accumulated during a period of 20 years. In the comparison of past findings with more recent cases, the progression of surgical techniques, such as the advent of thoracoscopy, may have had some degree of influence on opportunities to perform surgical resection. Finally, because our study did not compare resection with other treatments, we were unable to evaluate the detailed effects of surgical resection on the prognosis compared with other therapeutic options.
Conclusion
Surgical resection for pleural disseminated nodules of thymoma can be safely performed and provides a favorable long-term outcome. Furthermore, repeat resection is considered to be effective for achieving good results. We recommend that surgical resection for pleural dissemination of thymoma be proactively indicated.
References
Haniuda M, Kondo R, Numanami H, Makiuchi A, Machida A, Amano J. Recurrence of thymoma: clinicopathological features, reoperation, and outcome. J Surg Oncol. 2001;78:183–8.
Shinohara S, Hanagiri T, So T, et al. Results of surgical resection for patients with thymoma according to World Health Organization histology and Masaoka staging. Asian J Surg. 2012;35:144–8.
Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1320 patients from Japan. Ann Thorac Surg. 2003;76:878–84.
Regnard J-F, Zinzindohoue F, Magdeleinat P, Guibert L, Spaggiari L, Levasseur P. Results of re-resection for recurrent thymomas. Ann Thorac Surg. 1997;64:1593–8.
Okumura M, Shiono H, Inoue M, et al. Outcome of surgical treatment for recurrent thymic epithelial tumors with reference to World Health Organization histologic classification system. J Surg Oncol. 2007;95:40–4.
Lucchi M, Davini F, Ricciardi R, et al. Management of pleural recurrence after curative resection of thymoma. J Thorac Cardiovasc Surg. 2009;137:1185–9.
Murakawa T, Karasaki T, Kitano K, et al. Invasive thymoma disseminated into the pleural cavity: mid-term results of surgical resection. Eur J Cardiothorac Surg. 2015;47:567–72.
Yano M, Sasaki H, Yukiue H, et al. Thymoma with dissemination: efficacy of macroscopic total resection of disseminated nodules. World J Surg. 2009;33:1425–31.
Masaoka A, Monden Y, Nakahara K, Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer. 1981;48:2485–92.
Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma. Cancer. 2002;94:624–32.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240:205–13.
Fabre D, Fadel E, Mussot S, et al. Long-term outcome of pleuropneumonectomy for Masaoka stage IVa thymoma. Eur J Cardiothorac Surg. 2011;39:e133–8.
Huang J, Rizk NP, Travis WD, et al. Feasibility of multimodality therapy including extended resections in stage IVA thymoma. J Thorac Cardiovasc Surg. 2007;134:1477–83; discussion 1483–1484.
Yang HC, Yoon YS, Kim HK, et al. En bloc extended total thymectomy and extrapleural pneumonectomy in Masaoka stage IVA thymomas. J Cardiothorac Surg. 2011;6:28.
Okuda K, Yano M, Yoshino I, et al. Thymoma patients with pleural dissemination: nationwide retrospective study of 136 cases in Japan. Ann Thorac Surg. 2014;97:1743–8.
Marulli G, Margaritora S, Lucchi M, et al. Surgical treatment of recurrent thymoma: is it worthwhile? Eur J Cardiothorac Surg. 2016;49:327–32.
Shintani Y, Kanzaki R, Kusumoto H, Nakagiri T, Inoue M, Okumura M. Pleuropneumonectomy for a large thymoma with multiple pleural dissemination using median sternotomy followed by posterolateral thoracotomy. Surg Case Rep. 2015;1:75.
Kashima J, Okuma Y, Murata, Watanabe K, Hosomi Y, Hishima T. Chemoradiotherapy for unresectable cases of thymic epithelial tumors: a retrospective study. J Thorac Dis. 2017;9:3911–8.
Hishida T, Nomura S, Yano M, et al. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese Nationwide Database Study. Eur J Cardiothorac Surg. 2016;49(3): 835–841.
Kanzaki R, Kanou T, Ose N, et al. Long-term outcomes of advanced thymoma in patients undergoing preoperative chemotherapy or chemoradiotherapy followed by surgery: a 20-year experience. Interact Cardiovasc Thorac Surg. 2019;28:360–7.
Kobayashi Y, Fujii Y, Yano M, et al. Preoperative steroid pulse therapy for invasive thymoma: clinical experience and mechanism of action. Cancer. 2006;106:1901–7.
Kimura T, Inoue M, Kadota Y, et al. The oncological feasibility and limitations of video-assisted thoracoscopic thymectomy for early-stage thymomas. Eur J Cardiothorac Surg. 2013;44:e214–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURE
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1.
The overall survival of all patients (n=38) according to performance of repeat resection for thymoma pleural dissemination. Patients who underwent repeat resection showed a better prognosis than those who did not (p=0.005). (PDF 46 kb)
Rights and permissions
About this article
Cite this article
Kimura, K., Kanzaki, R., Kimura, T. et al. Long-Term Outcomes After Surgical Resection for Pleural Dissemination of Thymoma. Ann Surg Oncol 26, 2073–2080 (2019). https://doi.org/10.1245/s10434-019-07330-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07330-x