Abstract
Background
Because lymph node (LN) metastasis has been proven to be a predictor for locoregional recurrence (LRR) in papillary thyroid microcarcinoma (PTMC), better knowledge about the predictors for LN metastasis in PTMC is required.
Methods
We retrospectively reviewed 5656 PTMC patients who underwent total thyroidectomy and central neck dissection and/or lateral neck dissection between January 1997 and June 2015.
Results
Male gender (adjusted odds ratio [OR] 2.332), conventional variant (adjusted OR 4.266), tumor size >0.5 cm (adjusted OR 1.753), multiplicity (adjusted OR 1.168), bilaterality (adjusted OR 1.177), and extrathyroidal extension (ETE) (adjusted OR 1.448) were independent predictors for high prevalence of central LN metastasis (CLNM), whereas per 10-year age increment (adjusted OR 0.760) and chronic lymphocytic thyroiditis (adjusted OR 0.791) were independent predictors for low prevalence of CLNM. In addition, male gender (adjusted OR 1.489), tumor size >0.5 cm (adjusted OR 1.295), multiplicity (adjusted OR 1.801), ETE (adjusted OR 1.659), and CLNM (adjusted OR 4.359) were independent predictors for high prevalence of lateral LN metastasis (LLNM), whereas per 10-year age increment (adjusted OR 0.838) was an independent predictor for low prevalence of LLNM. There was a statistically significant difference in LRR with regard to nodal stage (p < 0.001).
Conclusions
Meticulous perioperative evaluation of LN metastasis is required for PTMC patients with the above predictors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the World Health Organization, papillary thyroid microcarcinoma (PTMC) is defined as a carcinoma less than 1 cm in size.1 With the recent widespread use of high-resolution ultrasonography (US), the current increase in the incidence of papillary thyroid carcinoma (PTC) is mainly due to earlier detection of PTMC.2 The long-term locoregional recurrence (LRR) rate of PTMC has been reported to be up to 8 % with more than 80 % of cases occurring in cervical LN (LN).3 Because LN metastasis is a proven predictor for LRR in PTMC, the concept of “node beget nodes” was suggested.3–5
The prevalence of subclinical central LN metastasis (CLNM) in PTMC has been reported to be 30–65 %.6–9 Because of difficulties in preoperative detection of CLNM, previous studies have suggested the benefit of prophylactic central neck dissection (CND) in PTMC.10,11 However, routine prophylactic CND might be associated with significantly higher morbidities, including recurrent laryngeal nerve injury and hypoparathyroidism.12 Therefore, identification of the predictive factors for CLNM would be important to avoid unnecessary CND in patients with PTMC. Moreover, identification of the predictive factors for lateral LN metastasis (LLNM) could be helpful to determine the necessity for lateral neck dissection (LND). Furthermore, clinicians should consider the possibility of undetected LN metastasis during postoperative period, particularly in PTMC patients who did not underwent neck dissection.
Previous studies of predictive factors for CLNM in PTMC yielded inconsistent data and involved sample sizes of fewer than 1000 cases.7,8,13–19 Furthermore, studies of the prediction of LLNM in PTMC were based primarily on US findings rather than surgically proven data.20,21 Therefore, the purpose of this study was to investigate the predictive factors for LN metastasis, including both CLNM and LLNM, using a large group of patients with surgically proven PTMC.
Patients and Methods
Patient Selection
This retrospective cohort study was approved by the institutional review board at Samsung Medical Center. Between January 1997 and June 2015, 5656 PTMC patients who underwent total thyroidectomy with CND and/or LND were included for analysis. The patients meeting the following criteria were excluded: age younger than 20 or older than 80 years, a previous history of thyroidectomy, non-PTC carcinomas (follicular/medullary/anaplastic), mixed type PTC, minor variants of PTC except conventional and follicular type, lobectomy cases, total thyroidectomy without CND, tumor size >1 cm, presence of distant metastasis, or follow-up duration less than 6 months (residual tumor or LN detected within 6 months after initial surgery, underwent reoperation within 6 months after initial surgery, or loss to follow-up within 6 months).
Surgical Methods
In general, surgical managements in our institution have been performed following American Thyroid Association Guidelines.22 Total thyroidectomy was performed when multiplicity, tumor bilaterality, extrathyroidal extension (ETE), or abnormal lymphadenopathy was detected during the preoperative or intraoperative examination. CND was defined as a level VI dissection, which comprised removal of all nodes and fibro-fatty tissue extending vertically from the hyoid bone to the thoracic inlet and laterally from the medial border of the common carotid artery to the midline of the trachea. Therapeutic CND was performed when abnormal lymphadenopathy was detected during the preoperative or intraoperative examination. In the clinically node-negative patients, prophylactic CND was performed based on the surgeon’s personal preference at the time of the operation or in the case of advanced primary tumors (T3/T4).22 LND, including modified radical neck dissection and selective neck dissection, was performed in cases where LLNM was confirmed preoperatively.
Histopathological Examination with Surgical Specimens
Surgical specimens were microscopically examined by two or more experienced pathologists, and the following histopathologic factors were assessed: the cell type of the main lesion, the primary tumor size (measured as the longest diameter of the largest lesion), location, multiplicity, bilaterality, ETE, lymphovascular invasion, margin involvement, LN metastasis, and the underlying conditions of the thyroid, such as chronic lymphocytic thyroiditis (CLT). To distinguish tumor bilaterality from multiplicity, multiplicity was defined as two or more lesions of PTMC in one lobe regardless of the presence of tumor bilaterality. The staging of thyroid cancer was determined in accordance with the American Joint Committee on Cancer.23
Postoperative Follow-Up
After the initial surgery, all patients underwent regular follow-up at 6- to 12-month intervals with clinical evaluations, including physical examinations, thyroid US, neck and chest computed tomography, iodine-131 scans, and serum thyroglobulin. Loss to follow-up, withdrawal, and death were censored as of the final date of follow-up. When suspicious lesions were detected, they were confirmed by US-guided aspiration biopsy with or without measurement of washout thyroglobulin level. LRR was defined as the presence of tumor or metastatic LN on cytology from aspiration biopsy or on histopathology from reoperation that developed 6 months after the initial surgery.
Statistical Analysis
Statistical analysis was performed using SPSS version 22.0 software (IBM Corp, Armonk, NY), and statistically significant differences were defined as those with p values <0.05. Continuous variables were presented as mean ± standard deviation (SD), and categorical variables were presented as the number of cases with percentage (%) and odds ratio (OR). χ 2 test and linear-by-linear association were used for categorical variables and Student’s t test for continuous variables. Multivariate analysis using logistic regression analysis was performed on the variables that achieved p values <0.05 in the univariate analysis. The Kaplan–Meier methods and log-rank test were adopted for analysis of time-dependent variables.
Results
Baseline Clinicopathological Characteristics of 5656 PTMC Patients
Of the 5656 patients, 1012 (17.7 %) were men and 4666 (82.3 %) were women. The mean age was 48.0 years, and 3394 patients (60.0 %) were older than 45 years. Conventional open surgery was performed in 5216 (91.8 %) patients, and oncoplastic (endoscopic or robotic) surgery was performed in 462 (8.2 %) patients. Prophylactic CND was performed in 4469 (79.0 %) patients, and therapeutic CND was performed in 1187 (21.0 %) patients. LND was performed in 649 (11.5 %) patients, and all LND was therapeutically performed. Because BRAF mutation analysis was only performed from 2008 in our institution, BRAF status was available for only 1772 patients. BRAF positivity among these patients was 82.6 %. The mean tumor size was 0.6 cm, and 3721 (65.8 %) patients had tumors >0.5 cm. Multiplicity, bilaterality, ETE, and CLT were seen in 1529 (27.0 %), 1538 (27.2 %), 3150 (55.7 %), and 1623 (28.7 %) patients, respectively. Tumor stages were as follows: T1 in 2491 (44.0 %); T3 in 2955 (52.2 %); and T4 in 210 (3.7 %) patients. Nodal stages were N0 in 3014 (53.3 %), N1a in 2124 (37.6 %), and N1b in 518 (9.2 %) patients.
Associations Between Clinicopathological Characteristics and CLNM in PTMC Patients
A total of 5137 patients who underwent total thyroidectomy and CND without LLNM were examined (Tables 1, 2), and 130 patients who underwent LND without LLNM were included. In univariate analysis, male gender (p < 0.001), young age (p < 0.001), conventional variant (p < 0.001), tumor size > 0.5 cm (p < 0.001), multiplicity (p < 0.001), bilaterality (p < 0.001), ETE (p < 0.001), and the absence of CLT (p < 0.001) were significantly associated with a high prevalence of CLNM. In multivariate analysis, male gender (adjusted odds ratio [OR] = 2.332, p < 0.001), conventional variant (adjusted OR 4.266, p < 0.001), tumor size >0.5 cm (adjusted OR 1.753, p < 0.001), multiplicity (adjusted OR 1.168, p = 0.026), bilaterality (adjusted OR 1.177, p = 0.018), and ETE (adjusted OR 1.448, p < 0.001) were independent predictors for high prevalence of CLNM. However, per 10-year age increment (adjusted OR 0.760, p < 0.001) and CLT (adjusted OR 0.791, p < 0.001) were independent predictors for low prevalence of CLNM.
Associations Between Clinicopathological Characteristics and LLNM in PTMC Patients
A total of 5656 patients who underwent total thyroidectomy with CND and/or LND were examined (Table 3). PTMC patients who did not undergo LND or who underwent LND without LLNM were classified as the absence of LLNM. In univariate analysis, male gender (p < 0.001), young age (p < 0.001), tumor size >0.5 cm (p < 0.001), multiplicity (p < 0.001), ETE (p < 0.001), and CLNM (p < 0.001) were significantly associated with high prevalence of LLNM. However, conventional variant (p = 0.225), bilaterality (p = 0.151), and CLT (p = 0.156) were not significantly associated with LLNM. In multivariate analysis, male gender (adjusted OR 1.489, p < 0.001), tumor size > 0.5 cm (adjusted OR 1.295, p = 0.026), multiplicity (adjusted OR 1.801, p < 0.001), ETE (adjusted OR 1.659, p < 0.001), and CLNM (adjusted OR 4.359, p < 0.001) were independent predictors for high prevalence of LLNM, whereas per 10-year age increment (adjusted OR 0.838, p < 0.001) was an independent predictor for low prevalence of LLNM. Among a total of 519 patients with LLNM, skip metastasis, defined as LLNM with no CLNM, was found in 107 (20.6 %) patients.
Association Between LRR and LN Metastasis in PTMC Patients
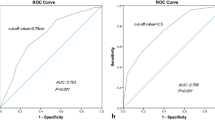
The median follow-up time was 61.7 months (range 6.0–213.8). Survival analysis was not performed due to a very few number of cause-specific deaths (only five), rather recurrence-free survival was used as the outcome of interest. LRR was observed in 126 patients (2.2 %): 122 (96.8 %) cases occurred in regional LNs and the remaining 4 (3.2 %) cases occurred in the operation bed. From the Kaplan–Meier survival analysis (Fig. 1), the recurrence-free survival rates were 99.5 % at 5 years, 99.1 % at 10 years, and 99.1 % at 15 years in N0 patients; 96.8 % at 5 years, 94.6 % at 10 years, and 93.6 % at 15 years in N1a patients; and 90.4 % at 5 years, 86.7 % at 10 years, and 86.7 % at 15 years in N1b patients. There was a statistically significant difference in the results of the log-rank test for LRR with regard to nodal stage (p < 0.001).
Discussion
We analyzed data for 5656 patients with surgically proven PTMC to investigate the predictive factors for LN metastasis, including both CLNM and LLNM. Because the sensitivity of US for detecting CLNM was <60 % and for detecting LLNM was <70 % in the previous studies, the knowledge of predictive factors of LN metastasis might compensate the sensitivity of US in preoperative period.24–26 Moreover, the identification of the predictive factors for LN metastasis would be important to avoid unnecessary neck dissection in PTMC patients, particularly who were indicated prophylactic CND.22 LN metastasis is a proven predictor for recurrence in PTMC; the concept of “node beget nodes” was suggested.3 Therefore, the assessment of the possibility of LN metastasis during postoperative period also is important, particularly in PTMC patients who did not underwent neck dissection.
To the best of our knowledge, this study is the largest study performed to date to identify predictive factors for LN metastasis in PTMC patients. From multivariate analysis, we showed that male gender, young age, conventional variant, tumor size >0.5 cm, multiplicity, bilaterality, ETE, and the absence of CLT were independent predictors for CLNM (Table 2). Moreover, we found that male gender, young age, tumor size >0.5 cm, multiplicity, ETE, and CLNM were independent predictors for LLNM (Table 3). In previous studies of CLNM, young age, male gender, tumor size >0.5 cm, multiplicity, bilaterality, and ETE were proven as independent predictors for CLNM in PTMC patients.5,8 , 14–19 Previous studies regarding LLNM, reported ETE, CLT, and CLNM as independent predictors in PTMC patients.20,21 A similarly designed study by Zhang et al. suggested that male gender, age <45 years, tumor size >0.6 cm, ETE, and multiplicity were independent risk factors for CLNM.13 ETE, multiplicity, bilaterality, and CLNM were independent risk factors for LLNM. Zeng et al. suggested that CLT is an independent predictor for LLNM in PTMC patients; however, other investigators have reported that PTC with the coexistence of CLT is less likely to be associated with ETE, advanced stage, LN metastasis, and recurrence.21,27–31 In this study, the absence of CLT was an independent predictor for CLNM but was not an indicator for LLNM. Moreover, although a previous study by Lang et al. suggested that significantly more LN metastases were observed in the conventional variant compared with the follicular variant, in our study the conventional variant was a predictor for CLNM, but not for LLNM.32
Although American Thyroid Association management guidelines recommend lobectomy in PTMC, more than 5000 PTMC patients underwent total thyroidectomy with CND and/or LND.33 Advanced tumor stages, T3 or T4, were seen in 3171 (55.9 %) patients in this study (Table 1); this incidence was higher than in previous reports, which showed an incidence of less than 30 % in PTMC patients.19,34 Moreover, the incidence of BRAF positivity in our study was greater than 80 %; this is similar to other studies in Korea, which is a BRAF-prevalent area.35–38 A strong association between BRAF mutation and aggressive clinicopathological characteristics of PTC, such as advanced stage, ETE, LN metastasis, and tumor recurrence was previously demonstrated.39 This finding regarding the incidences of advanced tumor stage and BRAF positivity also could support the geographic bias in this study. Particularly, in this study BRAF mutation status was not included in the multivariate analysis for the following reasons. First, because BRAF mutation analysis was not performed before 2008 in our institution, results were available for only 1772 patients. Second, we previously conducted a study on BRAF mutation and LN metastasis in which we showed that BRAF mutation was an independent predictor for bilaterality but not for CLNM and LLNM.40 As seen in Table 3, skip metastasis was found in 107 (20.5 %) patients, and this result was consistent with other studies.41,42 The finding that nodal stage is a predictor for LRR in PTMC patients (Fig. 1) also confirms previous reports.3–5
This study had several limitations. First, there are the inevitable inherent features of a nonrandomized, retrospective cohort study. Therefore, the patient information might not be complete and we cannot rule out the possibility of residual confounding variables of other measured or unmeasured factors. Second, our results may not be applicable to other races or countries, because this study was conducted in a BRAF-prevalent area.35,36 Third, because LND was performed only for therapeutic purpose in this study, there is the possibility of remaining subclinical LLNM. However, because LND is not generally recommended as a prophylactic procedure, this limitation is inevitable. Nevertheless, this study has several significant strengths. First, we conducted this study on a large group of patients, more than 5000 cases, from a single institution. Second, we used only surgically proven data, rather than US findings.
In conclusion, meticulous perioperative evaluation for CLNM is required for PTMC patients with male gender, young age, conventional variant, tumor size >0.5 cm, multiplicity, bilaterality, ETE, and the absence of CLT. Furthermore, meticulous perioperative evaluation for LLNM is required for PTMC patients with male gender, young age, tumor size >0.5 cm, multiplicity, ETE, and CLNM.
References
Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989;63:908–11.
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006;295:2164–7.
Hay ID, Hutchinson ME, Gonzalez-Losada T, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008;144:980–7.
Ross DS, Litofsky D, Ain KB, et al. Recurrence after treatment of micropapillary thyroid cancer. Thyroid. 2009;19:1043–8.
Pisanu A, Reccia I, Nardello O, Uccheddu A. Risk factors for nodal metastasis and recurrence among patients with papillary thyroid microcarcinoma: differences in clinical relevance between nonincidental and incidental tumors. World J Surg. 2009;33:460–8.
Wada N, Duh Q-Y, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003;237:399.
Roh JL, Kim JM, Park CI. Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis. Ann Surg Oncol. 2008;15:2482–6.
So YK, Son YI, Hong SD, et al. Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery. 2010;148:526–31.
Lim YC, Choi EC, Yoon YH, Kim EH, Koo BS. Central lymph node metastases in unilateral papillary thyroid microcarcinoma. Br J Surg. 2009;96:253–7.
Hyun SM, Song HY, Kim SY, et al. Impact of combined prophylactic unilateral central neck dissection and hemithyroidectomy in patients with papillary thyroid microcarcinoma. Ann Surg Oncol. 2012;19:591–6.
Zhang L, Liu Z, Liu Y, Gao W, Zheng C. The clinical prognosis of patients with cN0 papillary thyroid microcarcinoma by central neck dissection. World J Surg Oncol. 2015;13:138.
Mazzaferri EL, Doherty GM, Steward DL. The pros and cons of prophylactic central compartment lymph node dissection for papillary thyroid carcinoma. Thyroid. 2009;19:683–9.
Zhang L, Wei WJ, Ji QH, et al. Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab. 2012;97:1250–7.
Yang Y, Chen C, Chen Z, et al. Prediction of central compartment lymph node metastasis in papillary thyroid microcarcinoma. Clin Endocrinol (Oxf). 2014;81:282–8.
Zhao Q, Ming J, Liu C, et al. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol. 2013;20:746–52.
Kim BY, Jung CH, Kim JW, et al. Impact of clinicopathologic factors on subclinical central lymph node metastasis in papillary thyroid microcarcinoma. Yonsei Med J. 2012;53:924–30.
Lee SH, Lee SS, Jin SM, Kim JH, Rho YS. Predictive factors for central compartment lymph node metastasis in thyroid papillary microcarcinoma. Laryngoscope. 2008;118:659–62.
Kim KE, Kim EK, Yoon JH, Han KH, Moon HJ, Kwak JY. Preoperative prediction of central lymph node metastasis in thyroid papillary microcarcinoma using clinicopathologic and sonographic features. World J Surg. 2013;37:385–91.
Zhou YL, Gao EL, Zhang W, et al. Factors predictive of papillary thyroid micro-carcinoma with bilateral involvement and central lymph node metastasis: a retrospective study. World J Surg Oncol. 2012;10:67.
Kwak JY, Kim EK, Kim MJ, et al. Papillary microcarcinoma of the thyroid: predicting factors of lateral neck node metastasis. Ann Surg Oncol. 2009;16:1348–55.
Zeng RC, Li Q, Lin KL, et al. Predicting the factors of lateral lymph node metastasis in papillary microcarcinoma of the thyroid in eastern China. Clin Transl Oncol. 2012;14:842–7.
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–4.
Kim E, Park JS, Son KR, Kim JH, Jeon SJ, Na DG. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid. 2008;18:411–8.
Ahn JE, Lee JH, Yi JS, et al. Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg. 2008;32:1552–8.
Choi YJ, Yun JS, Kook SH, Jung EC, Park YL. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010;34:1494–9.
Loh KC, Greenspan FS, Dong F, Miller TR, Yeo PP. Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 1999;84:458–63.
Lee J-H, Kim Y, Choi J-W, Kim Y-S. The association between papillary thyroid carcinoma and histologically proven Hashimoto’s thyroiditis: a meta-analysis. Eur J Endocrinol. 2013;168:343–9.
Kim EY, Kim WG, Kim WB, et al. Coexistence of chronic lymphocytic thyroiditis is associated with lower recurrence rates in patients with papillary thyroid carcinoma. Clin Endocrinol (Oxf). 2009;71:581–6.
Lang BH, Chai YJ, Cowling BJ, Min HS, Lee KE, Youn YK. Is BRAFV600E mutation a marker for central nodal metastasis in small papillary thyroid carcinoma? Endocr Relat Cancer. 2014;21:285–95.
Kim SK, Woo JW, Lee JH, et al. Chronic lymphocytic thyroiditis and BRAF V600E in papillary thyroid carcinoma. Endocr Relat Cancer. 2016;23:27–34.
Lang BH, Lo CY, Chan WF, Lam AK, Wan KY. Classical and follicular variant of papillary thyroid carcinoma: a comparative study on clinicopathologic features and long-term outcome. World J Surg. 2006;30:752–8.
American Thyroid Association Guidelines Taskforce on Thyroid N, Differentiated Thyroid C, Cooper DS, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Lee X, Gao M, Ji Y, et al. Analysis of differential BRAF(V600E) mutational status in high aggressive papillary thyroid microcarcinoma. Ann Surg Oncol. 2009;16:240–5.
Kim KH, Kang DW, Kim SH, Seong IO, Kang DY. Mutations of the BRAF gene in papillary thyroid carcinoma in a Korean population. Yonsei Med J. 2004;45:818–21.
Kim TY, Kim WB, Song JY, et al. The BRAF mutation is not associated with poor prognostic factors in Korean patients with conventional papillary thyroid microcarcinoma. Clin Endocrinol (Oxf). 2005;63:588–93.
Kim SK, Kim DL, Han HS, et al. Pyrosequencing analysis for detection of a BRAFV600E mutation in an FNAB specimen of thyroid nodules. Diagn Mol Pathol. 2008;17:118–25.
Xing M. BRAF mutation in thyroid cancer. Endocr Cancer. 2005;12:245–62.
Xing M. BRAF mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev. 2007;28:742–62.
Kim SK, Woo JW, Lee JH, et al. Role of BRAF V600E mutation as an indicator of the extent of thyroidectomy and lymph node dissection in conventional papillary thyroid carcinoma. Surgery. 2015, 158(6):1500–11.
Park JH, Lee YS, Kim BW, Chang HS, Park CS. Skip lateral neck node metastases in papillary thyroid carcinoma. World J Surg. 2012;36:743–7.
Machens A, Holzhausen HJ, Dralle H. Skip metastases in thyroid cancer leaping the central lymph node compartment. Arch Surg. 2004;139:43–5.
Disclosure
The authors have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.K., Park, I., Woo, JW. et al. Predictive Factors for Lymph Node Metastasis in Papillary Thyroid Microcarcinoma. Ann Surg Oncol 23, 2866–2873 (2016). https://doi.org/10.1245/s10434-016-5225-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5225-0