Abstract
Introduction
The follicular variant of papillary thyroid carcinoma (FVPTC) is the most common histologic subtype of papillary thyroid carcinoma (PTC). However, it is still controversial whether FVPTC should behave differently from classical PTC (CPTC). The present study aimed at evaluating any potential difference in clinicopathologic features and long-term outcome of FVPTC as compared with CPTC.
Patients and Methods
Of 568 patients with PTC managed from 1973 to 2004, 308 were shown to have CPTC (54.2%) and 67 (11.8%) FVPTC after histologic review. The mean (± SD) follow-up period was 11.3 (± 8.9) years. The two groups were compared in terms of clinicopathological features, treatment received, and outcome regarding recurrence and disease-specific survival.
Results
There was no difference in age and gender ratio between the CPTC and FVPTC patients. Both groups had similar tumor characteristics in terms of tumor size, presence of multifocality, capsular invasion, lymphovascular permeation, and perineural infiltration. However, FVPTC patients had significantly fewer histologically confirmed cervical lymph node metastases (P = 0.027) and extrathyroidal involvement (P = 0.005). The proportion of bilateral resection, adjuvant radioactive iodine, and lymph node dissection did not differ significantly between the two groups. The FVPTC patients had a more favorable tumor risk by DeGroot classification (P = 0.003) and MACIS (Metastasis, Age, Completeness of excision, Invasiveness, and Size) score (P = 0.026). The 10- and 15-year actuarial disease-specific survivals did not differ significantly between FVPTC and CPTC patients (96.2% versus 90.7% and 96.2% versus 89.1%, respectively).
Conclusions
Although patients with FVPTC had more favorable clinicopathologic features and a better tumor risk group profile, their long-term outcome was similar to that of CPTC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Papillary thyroid carcinoma (PTC) is the most common type (70%–80%) of thyroid carcinoma and is generally associated with an excellent prognosis. Over the past decades, it has been increasingly recognized that the conventional or classical type of PTC (CPTC) only accounts for about 50% of cases, whereas the remaining 50% of cases are made up of various histologic variants. These variants, while sharing similar nuclear and cytological features, are often diagnosed on the basis of their distinct histopathologic features. They present a considerable challenge to pathologists and physicians because of diagnostic difficulties and potential prognostic implications. Among these variants, the follicular variant of PTC (FVPTC) is the most common and accounts for up to 41% of all PTC in some reported series.1–3
Although it was first described more than 50 years ago,4 it still remains unclear whether FVPTC should behave differently and would require a different treatment protocol than CPTC. In previous series, FVPTC was noted to have a less aggressive clinical behavior in terms of a lower incidence of lymph node and distant metastases while having a similar or even better long-term survival than CPTC.3,5,6 Other groups have found that these tumors presented more aggressively and had a greater tendency for pulmonary metastases.1,7 In addition, a recent report showed that FVPTC had a higher incidence of histologic vascular invasion but was associated with a more favorable outcome than other PTC variants by multivariate analysis.8 Based on current evidence, the overall management and prognosis of FVPTC would be assumed to be similar to that of CPTC.
As data on the clinicopathologic characteristic and management for FVPTC are still incomplete, the present study aimed to examine this variant of PTC in greater detail. The study was based on clearly defined selection criteria for FVPTC and conducted retrospectively over a relatively long study period for a significantly large number of patients treated in a single institution with complete medical records and long-term follow-up.
PATIENTS AND METHODS
A total of 568 patients undergoing surgical treatment for histologically confirmed PTC had complete medical records and follow-up at the Department of Surgery, University of Hong Kong Medical Centre, Queen Mary Hospital, Hong Kong, from January 1973 to December 2004. Occult microcarcinomas diagnosed during thyroidectomy for benign thyroid pathologies were excluded. Of the 568 patients, 308 (54.2%) had CPTC and 67 (11.8%) had FVPTC. Other histologic variants included papillary microcarcinoma (n = 96, 16.9%), encapsulated (n = 30, 5.3%), tall-cell (n = 24, 4.2%), diffuse sclerosing (n = 16, 2.6%), columnar (n = 10, 1.8%), and others (n = 17, 3.0%). The histologic variants were identified after a careful review of retrieved slides by one of the authors (A.K.Y.L.) according to the standardized criteria approved by the World Health Organization.9
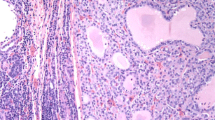
The follicular variant of PTC is made up of papillary carcinoma composed of small to medium-sized, irregularly shaped follicles with virtually no papillary structures. Grossly, many of these tumors resemble follicular neoplasms. The diagnosis of papillary carcinoma was based on demonstration of typical nuclear characteristics of PTC such as nuclear pseudo-inclusions, nuclear grooves, enlarged elongated overlapping nuclei, ground glass nuclei, and psammoma bodies.10
In patients with a preoperative diagnosis of PTC, a total or near-total thyroidectomy had increasingly been the preferred procedure of choice for many years. For those diagnosed after a unilateral lobectomy, the decision to perform a completion total thyroidectomy depended on the patient’s risk factors, tumor characteristics, the presence or absence of nodal metastases, and the patient’s choice. Selective neck dissection was performed for clinically overt or ultrasound-detected lymph node metastases, and enlarged or suspicious lymph nodes in the central compartment were either excised or sampled when clinically indicated.
All patients after surgery were followed up in a specialized combined thyroid cancer clinic attended by both clinical oncologists and surgeons to discuss and decide on the subsequent management. Details of management for high-risk patients have previously been described.11 In brief, postoperative radioactive iodine (I131) ablation (dose: 80–100 mCi), followed by whole-body scintigraphy and thyroxine suppression therapy, was given to high-risk patients. Patients were followed up regularly every third month for the first 2 years, every sixth month for the subsequent 3 years, and annually thereafter. Follow-up examinations included clinical evaluation, chest radiograph, ultrasonography of the neck (if indicated), and thyroglobulin levels without thyrotropin stimulation (since 1991). Radioactive iodine whole-body scintigraphy was repeatedly performed on patients with an elevated thyroglobulin level or in the presence of a clinically suspicious recurrence.
All relevant clinical, laboratory, radiological, and perioperative data were prospectively entered and regularly updated into a computerized thyroid database from 1995 onwards. Survival data including the cause of death were retrieved through the Hong Kong Hospital Authority territory-wide computerized medical system and from death certificates.
Statistical analysis was performed by the chi-square test or the Fisher’s exact test to compare discrete variables, and the Mann-Whitney U-test to compare continuous variables between groups. Cumulative recurrence rate and disease-specific survivals were estimated by the Kaplan-Meier method and compared by the log-rank test. A P value <0.05 was considered to indicate statistical significance. Statistical analyses were performed using the SPSS for Windows 10.0 computer software (SPSS Inc., Chicago, IL).
RESULTS
Clinicopathologic Features
The demographics and clinicopathologic features of the two histological subgroups at presentation are compared in Table 1. The groups were comparable in terms of age at diagnosis (P = 0.511) and gender (P = 0.252). Over 95% of patients in both groups had a palpable clinical solitary nodule as the main presentation. Almost one-fourth of the patients in both groups had concomitant clinically overt cervical lymph node metastases at presentation. Two patients in the CPTC group had bone metastases, whereas one patient in the FVPTC group had pulmonary metastases at presentation. With regard to pathological features, the two groups were comparable in terms of tumor size (P = 0.726), the presence of multifocal disease (P = 0.856), capsular invasion (P = 0.571), lymphovascular permeation (P = 0.438), perineural infiltration (P = 0.346), and associated lymphocytic thyroiditis (P = 0.804). However, extrathyroidal extension was significantly less frequent in FVPTC than in CPTC (26.9% versus 44.8%, P = 0.005). In addition, histological lymph node involvement was found to be a less frequent occurrence in FVPTC than CPTC (26.9% versus 42.2%, P = 0.027). In terms of tumor risk profile (Table 2), both groups were comparable when applying the AMES (Age, Metastasis to distant sites, Extrathyroidal invasion, and Size)12 risk group stratification (P = 0.264) and UICC (International Union Against Cancer) pTNM staging systems13 (P = 0.281). However, when using the Degroot classification (P = 0.003)14 and MACIS (Metastasis, Age, Completeness of excision, Invasiveness, and Size) scoring systems15 (P = 0.026). The follicular variant of PTC had a more favorable tumor risk profile than that of CPTC.
Treatment
Bilateral resections were performed for 94.5% of patients with CPTC and 89.6% with FVPTC (P = 0.142). Of the 17 patients in the CPTC group treated by lobectomy (5.5%), 12 had stage I, 3 had stage II, and 2 had stage III disease by UICC pTNM staging, whereas 6 of the 7 patients in the FVPTC group subjected to lobectomy had stage I disease and 1 had stage III disease. Both the proportion and the type of lymph node sampling or dissection were comparable between the two groups. There were 18 patients with CPTC and 4 patients with FVPTC undergoing palliative shave resection with residual tumor left after the operation, as judged by the operating surgeons. External radiotherapy and/or radioactive iodine (I131) ablation was frequently administered to these patients after operation. The proportions of patients receiving I131 ablation and/or external radiotherapy as adjuvant treatment were comparable between the two groups (Table 3).
Postoperative Tumor Recurrence and Survival
Sixty-two patients (16.5%) developed recurrence after a mean (± SD) follow-up of 11.3 (± 8.9) years after the initial surgery; 54 patients belonged to the CPTC group, and 8 patients were in the FVPTC group. In the CPTC group, 46 had locoregional recurrence, 5 had distant metastases, and 3 had both as the first detected site(s) of recurrence, whereas in the FVPTC group, 6 had locoregional recurrence and 2 had distant metastases. The site of first recurrence (locoregional versus distant) did not differ between the two groups (P = 0.421). The cumulative recurrence of CPTC and FVPTC is compared in Figure 1. The 5-, 10-, and 15-year recurrence rates for CPTC and FVPTC were 4.5%, 16.7%, 24.8%, and 4.7%, 8.3%, 8.3%, respectively (P = 0.468). In terms of disease-specific mortality, 22 patients died of recurrent thyroid carcinoma in the CPTC group, whereas only one patient in the FVPTC group died of recurrent disease. The 5-, 10-, 15-year disease-specific survival rates for CPTC and FVPTC were 95.7%, 90.7%, 89.1% and 100%, 96.2%, 96.2%, respectively (P = 0.110) (Fig. 2).
DISCUSSION
Potential differences in the clinical behavior and long-term outcome of FVPTC when compared with CPTC have been somewhat difficult to document. Most published series evaluating clinicopathologic features and outcome have suffered from drawbacks such as the lack of adoption of a specific agreed definition, inclusion of relatively few cases, and the lack of long-term follow-up.1,5,6,16 The overall management and prognosis of FVPTC was thus presumed to be similar to that of CPTC. To overcome some of these drawbacks, the present study was conducted retrospectively with a relatively long follow-up for a significantly large number of patients with clearly defined selection criteria and complete medical records.
To our knowledge, the present study comprising 67 patients diagnosed with FVPTC with follow-up over a mean of 11.3 years is one of the largest series with sufficient follow-up. A previous study reporting a series of 100 FVPTC patients with a median follow-up of 11.5 years3 was criticized for using non-conventional pathological criteria in defining FVPTC.16 The importance of selecting patients with a well-accepted and standardized pathological definition should not be underestimated. Without clearly defined histologic selection criteria, an outcome study for the variants of PTC will not be possible. The fact that the percentage of FVPTC in relation to all PTC varied widely from 9%–40% in the literature1–3 may be attributed to the lack of a standardized histopatholgic definition for FVPTC, as well as difficulties in making an accurate histological diagnosis.17 The pathological definition used in the present study was in accordance with the latest definition of FVPTC approved by the World Health Organization.9 To further standardize the quality of the pathology and at the same time minimize the inter-observer variation,10 the present study employed one dedicated endocrine pathologist with experience in thyroid cancer pathology to review all retrieved slides over the study period. Ancillary techniques such as immunohistochemistry and molecular profiling18–20 could be used for confirmation of diagnosis in the future, although their roles remain to be clarified. In our study, ancillary studies and consultation with other endocrine pathologists were done only in cases where the diagnoses were difficult to confirm.
The present study revealed that the incidence of associated lymph node metastases was significantly less in FVPTC than in CPTC. The actual incidence of cervical nodal metastases for each group may have been underestimated because central neck dissection was not performed routinely in the earlier study period. Although a sampling bias leading to a difference in the incidence of lymph nodes metastases was certainly possible, this would be unlikely because of the adoption of a standardized operative strategy to cervical lymph node for both groups of patients throughout the study period, as evident by a similar proportion as well as the types of cervical neck dissections performed for the two patient groups. Therefore, the lower incidence of lymph node metastases would appear to be a real and distinct pathological feature of FVPTC, as described in previous studie.3,5 Interestingly, apart from less frequent nodal metastases, the frequency of extrathyroidal extension of tumor was significantly lower in FVPTC, as shown in the present study. This finding also concurred with the results of a recent study that reported that FVPTC was less locally invasive and aggressive than CPTC.6 Although one previous study did suggest that multifocal disease was more common in FVPTC,5 both the present study and another previous study3 did not confirm this feature. In keeping with the two favorable clinicopathologic features, patients with FVPTC also had an overall more favorable tumor risk profile as measured by the DeGroot classification and MACIS scoring systems. Interestingly, out of the four risk-stratification systems used in the present study, the DeGroot and MACIS are known to be more specific and better predictors of tumor risk for papillary carcinoma, whereas the AMES and UICC pTNM measures are primarily tailored for well-differentiated thyroid carcinoma. The favorable risk profile did not, however, translate into a significantly improved disease-specific survival or a lower recurrence rate in the present analysis. These seemed to concur with similar findings in some recent reports.3,5 In contrast with the earlier series,1,7 pulmonary metastases did not seem to occur more frequently in FVPTC and, in addition, there was no significant difference in the postoperative recurrence pattern over the mean follow-up period of 11.3 years. The rates of both locoregional recurrence and distant metastases were similar in the two histological groups.
Despite the above findings, one must be cautious when interpreting the data because the present study was retrospective and the analysis was based on a relatively long study period in a single institution. Also, it is not possible to rule out the possibility of mistaking follicular neoplasms and/or mixed papillary carcinoma for FVPTC. Because of the overall excellent prognosis, more patients or even a longer follow-up may be necessary in showing a survival or disease-free difference between these two groups of PTC patients. Despite the very similar long-term outcome demonstrated between the groups, the authors are of the opinion that the distinction between FVPTC and CPTC should remain, as this may be of value for future tumor classification as well as genetic and molecular understanding of thyroid carcinoma.
In conclusion, patients with FVPTC presented with a more favorable clinicopathologic features and tumor risk group profile than patients with CPTC. Based on a similar long-term outcome after receiving similar treatment, the management strategy of patients with FVPTC should not be different from that of patients with CPTC.
References
Tielens ET, Sherman SI, Hruban RH, et al. Follicular variant of papillary thyroid carcinoma: a clinicopathologic study. Cancer 1994;73:424–431
Ortiz Sebastian S, Rodriguez Gonazles JM, Parilla Paricio P, et al. Papillary thyroid carcinoma: prognostic index for survival including the histological variety. Arch Surg 2000;135:272–277
Zidan J, Karen D, Stein M, et al. Pure versus follicular variant of papillary thyroid carcinoma: clinical features, prognostic factors, treatment, and survival. Cancer 2003;97:1181–1185
Crile GJ, Hazard JB. Relationship of the age of the patient to the natural history and prognosis of carcinoma of the thyroid. Ann Surg 1953:138:33–38
Passler C, Prager G, Scheuba C, et al. Follicular variant of papillary thyroid carcinoma: a long-term follow-up. Arch Surg 2003;138:1362–1366
Burningham AR, Krishnan J, Davidson BJ, et al. Papillary and follicular variant of papillary carcinoma of the thyroid: initial presentation and response to therapy. Otolaryngol Head Neck Surg 2005;132:840–844
Carcangiu ML, Zampi G, Pupi A, et al. Papillary carcinoma of the thyroid: a clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer 1985;55:805–828
Falvo L, Catanio A, D’Andrea V, et al. Prognostic importance of histologic vascular invasion in papillary thyroid carcinoma. Ann Surg 2005;241:640–646
Lloyd RV, DeLellis RA, Heitz PU, et al. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of Endocrine Organs, IARC (International Agency for Research on Cancer) Press, Lyons, France, 2004
Lloyd RV, Erickson LA, Casey MB, et al. Observer variation in the diagnosis of follicular variant of papillary thyroid carcinoma. Am J Surg Pathol 2004;28:1336–1340
Lo CY, Chan WF, Lam KY, et al. Optimizing the treatment of AMES high-risk papillary thyroid carcinoma. World J Surg 2004;28:1103–1109
Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery 1988;104:947–953
UICC (International Union Against Cancer). TNM Classification of Malignant Tumor, 5th ed. (Editors: Sobin LH, Wittlekind C), New York, Wiley-Liss, 1997
DeGroot LJ, Kaplan EL, McCormick M, et al. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metabol 1990;71:414–424
Hay ID, Bergstrath EJ, Goellner JR, et al. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 to 1989. Surgery 1993;114:1056–1058
LiVolsi VA. Pure versus follicular variant of papillary thyroid carcinoma: clinical features, prognostic factors, treatment, and survival. Cancer 2003;98:1997; author reply 1997–1998
Baloch ZW, LiVolsi VA. Follicular-patterned lesions of the thyroid: the bane of the pathologist. Am J Clin Pathol 2002;117:143–150
Zhu Z, Gandhi M, Nikiforova MN, et al. Molecular profile and clinical-pathologic features of the follicular variant of papillary thyroid carcinoma: an unusually high prevalence of ras mutations. Am J Clin Pathol 2003;120:71–77
Trovisco V, de Castro IV, Soares P, et al. BRAF mutations are associated with some histiotypes of papillary thyroid carcinoma. J Pathol 2004;202:247–251
Lo CY, Lam KY, Leung PP, et al. High prevalence of cyclooxygenase 2 expression in papillary thyroid carcinoma. Eur J Endocrinol 2005:152:545–550
Author information
Authors and Affiliations
Corresponding author
Additional information
Free paper presentation in International Surgical Week 2005, Durban, South Africa 21–25 August, 2005.
Rights and permissions
About this article
Cite this article
Lang, B.HH., Lo, CY., Chan, WF. et al. Classical and Follicular Variant of Papillary Thyroid Carcinoma: A Comparative Study on Clinicopathologic Features and Long-term Outcome. World J. Surg. 30, 752–758 (2006). https://doi.org/10.1007/s00268-005-0356-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0356-7