Abstract
Objective
To identify the clinical and pathological predictors of central lymph node metastasis (CLNM) in patients with clinically lymph node-negative papillary thyroid microcarcinoma (PTMC).
Materials and methods
Data pertaining to 541 clinically lymph node-negative PTMC patients who underwent thyroid surgery at the Shanghai General Hospital between January 2010 and December 2013 were retrospectively analyzed. According to histopathological evidence of central lymph node involvement, patients were divided into central lymph node metastasis (CLNM)-positive and CLNM-negative groups; risk factors for CLNM were identified statistically.
Results
LNM was found in 148 (27.4%) patients. Gender (P = 0.002), age (P < 0.001), tumor size (P < 0.001), multifocality (P < 0.001), and extrathyroidal extension (P < 0.001) were significantly different between CLNM-positive and CLNM-negative groups. On multivariate analyses, male sex (odds ratio [OR] = 2.656), age <45 years (OR = 4.184), tumor size >0.575 cm (OR = 2.105), gross extrathyroidal extension (OR = 14.605) and multifocality (OR = 2.084) were independent risk factors for CLNM. Among patients who did not have any of these five risk factors, only 3.9% were found to have CLNM.
Conclusions
A relatively high prevalence of CLNM was observed in patients with clinically lymph node-negative PTMC. CLNM was associated with male sex, younger age, larger tumor size, extrathyroidal extension and multifocal PTMC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The global incidence of thyroid cancer has seen a dramatic increase since the early 1990s [1, 2]. In the period from 2002 to 2011, the incidence of thyroid cancer in USA was 11.6/100,000 population, with an annual growth rate of 5.5% [3]. In China, the incidence of thyroid cancer in the period from 2003 to 2007 was 4.44/100,000, with an annual growth rate of 14.51% [4]. Some specific aspects of the observed increase in thyroid cancer incidence are worth noting. Nearly all the registered increase is limited to the papillary histotype and most increase relates to tumors of small size (≤1 cm); the percentage of such cancers has increased to nearly 50% of all newly detected cancers. In other words, papillary thyroid microcarcinoma (PTMC), defined as papillary thyroid carcinoma (PTC) measuring ≤1 cm in maximal diameter, has contributed the most to the increased incidence of thyroid cancer. This shift may be attributable to increased use of neck ultrasonography and other imaging modalities for early diagnosis and treatment.
Overall, PTMC is associated with an excellent prognosis with 10-year survival rates of >91% and 15-year survival rates of >87% [5, 6]. However, central lymph node metastasis (CLNM) is a common occurrence in patients with PTMC (20–90% of all patients) [7, 8]. The presence of LNM in patients with PTMC is known to be associated with an increased risk of regional recurrence [9,10,11], but does not affect patient survival [12]. However, in a recent large population-based study, lymph node metastasis was shown to be associated with increased risk of mortality [13]. Therefore, risks associated with central lymph node metastasis deserve due consideration.
The expression ‘clinically lymph node negative’ implies that patients exhibited no clinical evidence of CLNM on preoperative ultrasonography (US) or computerized tomography (CT). Ultrasonography is a cost-effective and sensitive method for the detection of thyroid cancer. Unfortunately, preoperative detection of microscopic LNM is not easy owing to the limited resolution of US. The phrase “subclinical CLNM” indicates clinically lymph node-negative (CN0) patients who are found to have pathologically confirmed CLNM intraoperatively or postoperatively. Subclinical CLNM is frequently detected (25–65%) on histopathological examination of PTMC specimens [14,15,16].
For clinically lymph node-positive patients, lymphadenectomy is an obvious requirement. However, for clinically lymph node-negative cases, especially those with subclinical CLNM, the decision to perform central lymph node dissection (CLND) is not straightforward. Therefore, identification of clinical and pathological predictors of central lymph node metastasis in patients with PTMC who are clinically lymph node negative is likely to facilitate optimal therapeutic decision making. As these predictors remain uncertain, we systematically analyzed the risk factors for CLNM in clinically lymph node-negative PTMC patients. Our study differs from previous studies in that we sought to identify factors associated with subclinical CLNM in patients with PTMC who were clinically lymph node negative.
Materials and methods
Patients and methods
Data pertaining to a total of 648 consecutive patients with PTMC who were treated at the Department of Surgery, Shanghai General Hospital between January 2010 and December 2013, were retrospectively analyzed. The inclusion criteria were: (1) patients with no preoperative clinical evidence of lymph node involvement by ultrasonography (US); (2) patients who had no history of head and neck irradiation or surgery for other malignancies; (3) patients with primary tumors (those with recurrent tumors were excluded); (4) diagnosis of PTMC confirmed on histopathological examination of the surgical specimen. Finally, a total of 541 patients were enrolled in this study.
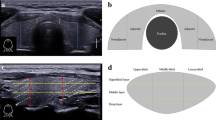
All patients underwent preoperative clinical and ultrasonographic evaluation. Preoperative thyroid ultrasound examination was performed with a Logic E9 scanner (General Electric Company, USA) equipped with a 9–12 MHz linear phased-array transducer, grayscale or color Doppler ultrasound. All preoperative US examinations were interpreted by two radiologists, each of whom had more than 15 years of experience. For each nodule, echogenicity, margin, shape and calcification pattern were recorded. Features of malignant nodules included: marked hypoechogenicity, ratio of length/width ≥1, spiculated margin, hypervascularity and the presence of microcalcification. Gross extrathyroidal extension was defined as clinical evidence of macroscopic tumor extension outside the thyroid gland based on physical examination and/or findings of ultrasound examination. LNM was suspected when US examination of lymph nodes showed increased size, rounded bulging shape, irregular margins, calcification, replacement of fatty hilum, heterogeneous texture, cystic areas and abnormal vascularity [17]. Once a lymph node was suspected to be metastatic based on US findings, it was subjected to preoperative US-guided fine-needle aspiration biopsy; patients who tested positive were excluded. CT or MRI was not routinely performed at our institution.
Surgery types included ipsilateral lobectomy + isthmectomy plus ipsilateral prophylactic central lymph node dissection (CLND) for patients with unilateral PTMC, or total thyroidectomy plus bilateral CLND for those with bilateral PTMC. CLND is routinely performed at our institution and its bound was superiorly to the hyoid bone, laterally to the carotid sheath, inferiorly to the manubrium and dorsally to the prevertebral fascia. Intraoperative frozen section was performed for all patients. Postoperative therapy included TSH suppression with levothyroxine and selective radioiodine treatment for patients with any of following clinicopathological characteristics: extrathyroidal extension; metastatic lymph nodes more than five in number or diameter >1 cm; postoperative unstimulated Tg level >5 ng/mL).
This research was approved by the Institutional Review Board and Clinical Ethics Committee of Shanghai General Hospital, Shanghai Jiaotong University School of Medicine.
Statistical analysis
Statistical analysis was performed using SPSS Version 20.0 for Mac (IBM, USA). Quantitative data are presented as mean ± standard deviation (SD). Between-group differences with respect to categorical variables were assessed with Chi squared test or Fisher’s exact test. Univariate and multivariate analysis was performed to identify variables associated with central lymph node metastasis. Between-group differences associated with P values <0.05 were considered to be statistically significant.
Results
The baseline patient characteristics are summarized in Table 1. There were 128 men and 413 women; the mean age of patients was 47.2 years (range 16–81). The mean size of tumors was 0.58 cm (range 0.05–1.0). On histopathological examination of surgical specimens, multifocality was found in 146 (30.0%) patients, central LNM was found in 148 (27.4%) patients and extrathyroidal extensions were found in 97 (17.9%) patients (gross extrathyroidal extension in 13 patients and microscopic extrathyroidal extensions in 84 patients). The average number of harvested central lymph nodes was 6.58 (range 2–35); the average number of positive lymph nodes was 0.81 (range 0–17).
Receiver operating characteristic (ROC) curve analysis was performed to determine the optimal cutoff level of PTMC size to predict the risk of CLNM. The ROC curve is shown in Fig. 1 and the optimal cutoff value was 0.575 cm (area under the curve: 0.706). Therefore, 0.575 cm was used as the cutoff level for categorization of patients in the subsequent analysis.
The predictive factors for CLNM are shown in Table 2. Male gender (P = 0.002), age <45 years (P < 0.001), tumor size >0.575 cm (P < 0.001), multifocality (P < 0.001) and extrathyroidal extension (P < 0.001) were significantly different between LN-positive and LN-negative groups. Among patients with extrathyroidal extension, those in the LN-positive and LN-negative groups showed significant differences with respect to the presence of gross extrathyroidal extension (P < 0.001) or microscopic extrathyroidal extension (P < 0.001). On multivariate analyses, male gender (odds ratio [OR] = 2.656), age <45 years (OR = 4.184), tumor size >0.575 cm (OR = 2.105), gross extrathyroidal extension (OR = 14.605) and multifocality (OR = 2.084) were found to be independent predictors of central LNM (Table 3).
Among the 127 patients who did not have any of the five risk factors, only five patients (3.9%) had CLNM (Table 4); compared to the overall incidence of CLNM in this study (27.4%), this rate is significantly low.
The mean duration of follow-up was 42.4 months (range 24–60). Patient workup during follow-up examinations included physical examination, ultrasound and serum levels of Tg, TSH and FT4 for patients who had not undergone radioactive iodine ablation; for patients who had undergone radioactive iodine ablation, whole body radioactive iodine scans were performed. Temporary hypocalcemia was found in 129 (23.8%) patients; none of the patients developed permanent hypocalcemia. Temporary unilateral recurrent laryngeal nerve injury occurred in 12 patients, all of whom recovered within 6 months. None of the patients sustained bilateral recurrent laryngeal nerve injury. Seven patients developed cervical lymph node metastasis 5 years after surgery. Ipsilateral or contralateral recurrence and distant metastasis were not found. One patient died unexpectedly of cardiovascular disease.
Discussion
PTMC accounts for up to 30% of all differentiated thyroid carcinomas [18]. The incidence rate in women is significantly higher than that in men, with a female:male ratio of approximately 3:1. In our study, the corresponding ratio was 3.23:1. PTMC is usually considered to have a relatively good prognosis [19]; however, on long-term follow-up, postoperative recurrence rates of 8–25% have been reported [20]. Factors associated with poor prognosis include extrathyroidal extension, lymph node metastasis and multifocality; these typically appear at a relatively advanced stage [21, 22]. CLNM is the most important risk factor for local recurrence [11]. In a study by Chow et al., the presence of LN metastases at diagnosis was found to be associated with a 4.2-fold and 6.2-fold higher risk of locoregional recurrence and cervical lymph node recurrence, respectively [11]. However, due to the limitations of ultrasonography, the preoperative detection rate of CLNM is typically low. In a study by Yu et al. [23], <30% of all PTMC patients with histopathologically confirmed CLNM were detected on preoperative ultrasonography. Therefore, identification of clinicopathological variables that are associated with increased risk of CLNM in patients with PTMC is of much clinical relevance.
The patients enrolled in this study showed no evidence of CLNM at diagnosis; however, LNM was found in 27.4% of these patients. The incidence of lymph node metastases in our study was slightly lower than that reported in previous literature; this is likely because we enrolled only CN0 patients, and those with clinical lymph node metastasis were excluded.
Tumor size is known to be associated with lymph node metastasis; however, the optimal cutoff level for tumor size in the context of PTMC is not clear. Lim et al. indicated an optimal cutoff level of 0.7 cm [16], while Zhang et al. [24] and Chang et al. [25] reported optimal cutoff levels of 0.6 and 0.5 cm, respectively. Prior to the analysis of risk factors, we performed ROC curve analysis for tumor diameter and determined an optimal cutoff level of 0.575 cm.
Our study revealed that male sex, age <45 years, tumor size >0.575 cm, extrathyroidal extension and multifocality were independent risk factors for CLNM among patients who were clinically non-metastatic by both univariate and multivariate analyses. These results are consistent with Yu’s report [23].
Obviously, 45 years was an important cutoff age for judging the stage of the differentiated thyroid carcinoma. Consistent with many previous studies, we found that younger age was a risk factor for CLNM [23, 26]. However, there is no convincing explanation why younger age shows opposite association with tumor stage and lymph node metastasis in the context of PTMC.
On multivariate analyses, male gender was found to be an independent predictor for CLNM, which is consistent with results of several previous studies [23, 25, 27]. Some have argued that male gender and CLNM are risk factors for recurrence of PTC [20]; we considered these factors existing internal relations.
It is believed that larger tumor size is associated with aggressive features of PTMC and we proved that tumor size was a risk factor for CLNM. In this study, we determined the cutoff level for tumor diameter by ROC curve analysis and used it to group the PTMC patients. In our research, PTMC patients with tumor size >0.575 cm were found to be more prone to central lymph node metastasis.
Previous researches have indicated multifocality as an independent risk factor for CLNM [28, 29] and we tested it in this study. The pathological multifocality rate in PTMC patients was 30.0%. The incidence of CLNM in patients with multifocal PTMC was 39.0% as compared to 23.0% in patients with unifocal disease. On multivariate analysis, the CLNM rate for patients with multifocality was higher than that in patients with unifocal PTMC (OR = 2.084; P = 0.026). Whether multifocality originates from different unrelated clones or from one focal intrathyroid spreading is uncertain. Mazeh and Jovanovic indicated that noncontiguous tumor foci originate from independent precursors [30, 31], based on their studies involving polymerase chain reaction for human androgen receptor gene or BRAF gene. However, Lombardi’s study demonstrated that multicentric papillary lesions arise from the same clone [32].
In this study, gross extrathyroidal extension was identified as an independent risk factor by multivariate logistic regression analysis (OR = 14.605, P < 0.001). The new AJCC TNM staging 8th edition (2016) re-emphasizes the critical importance of gross extrathyroidal extension as an unfavorable prognostic factor, while it downplays the significance of minor extension through the thyroid capsule, which is identified only on histological examination. However, in our study, microscopic extrathyroidal extension was also found to be significantly different between the two groups. The new edition makes it clear that gross extrathyroidal extension is a clinical finding based on radiological and/or clinical evidence of macroscopic tumor extension outside the thyroid gland. In PTMC, extrathyroidal extension refers to various extents of invasion, including invasion into strap muscles (sternohyoid, sternothyroid, thyrohyoid or omohyoid muscles), perithyroid tissues, recurrent laryngeal nerves, larynx, trachea, esophagus, prevertebral fascia, mediastinal vessels and even carotid artery.
Currently, many aspects of treatment for PTMC remain controversial, such as the indications for postoperative radioiodine thyroid ablation [33, 34], the principles of TSH suppression therapy and whether it is possible to just adopt a “watchful waiting” strategy in these patients [35]. Many scholars have voiced differing opinions on the necessity of central lymph node dissection (CLND) in clinically lymph node-negative PTMC patients, although the indications for the same have been outlined in the updated guidelines. Some have argued against CLND, citing low mortality rates (0–1%) in patients with PTMC and the lack of survival benefit accruing from CLND [36]. Moreover, CLND carries a risk of perioperative complications such as hypoparathyroidism and laryngeal nerve injury [14]. In addition, operations for recurrent lymph nodes in patients with PTC were shown to be associated with increased risk of postoperative complications [37]. In our study population, although there were no serious complications, temporary hypocalcemia and temporary unilateral recurrent laryngeal nerve injury occurred in 23.8 and 2.2% of patients, respectively. At the same time, others have reported increased risk of recurrence in PTMC patients with CLNM. Moreover, it is difficult to predict the risk of progression of subclinical central lymph node metastasis to overt clinical metastasis in the absence of intervention [11]. Further, CLND helps improve the accuracy of lymph node staging [38]. Although many previous studies have listed risk factors for PTMC, we focused on identification of factors which were associated with subclinical CLNM in patients with clinically lymph node-negative PTMC. All the factors considered to be independent predictors of CLNM can be determined preoperatively. We calculated CLNM rate of patients who had none of the five risk factors and found that it was significantly lower than the overall CLNM rate in our study population (3.9 versus 27.4%, respectively; P < 0.001). 3.9% is an extremely low percentage, which suggests a question whether it is necessary to perform prophylactic CLND in this group of patients.
Nonetheless, we acknowledge the limitations of our investigation. First, our study was a retrospective research; errors and bias in retrospective studies tend to be higher than those in prospective studies. Secondly, prophylactic CLND was performed in all patients included in our study, which may not be appropriate for clinically non-metastatic PTMC. Thirdly, “skip metastasis,” defined as lateral lymph node metastasis without central lymph node metastasis, also occurs in patients with PTC. Such cases also should be considered.
Conclusion
In conclusion, we found a high incidence of CLNM in clinically lymph node-negative PTMC patients. Subclinical CLNM in PTMC patients might be predicted by the following factors: male sex, age <45 years, tumor size >0.575 cm, gross extrathyroidal extension and multifocality. These findings may help clinicians identify patients with PTMC who are likely to benefit from CLND.
References
Vigneri R, Malandrino P, Vigneri P (2015) The changing epidemiology of thyroid cancer: why is incidence increasing. Curr Opin Oncol 27:1–7
Guay B, Johnson-Obaseki S, McDonald JT, Connell C, Corsten M (2014) Incidence of differentiated thyroid cancer by socioeconomic status and urban residence: Canada 1991–2006. Thyroid 24:552–555
SEER Cancer Statistics Review, 1975–2011. National Cancer Institute. 2013. http://seer.cancer.gov/csr/1975_2011/. Based on November 2013 SEER data submission
Liu YQ, Zhang SQ, Chen WQ, Chen LL, Zhang SW, Zhang XD (2012) Trend of incidence and mortality on thyroid cancer in China during 2003–2007. Zhonghua Liu Xing Bing Xue Za Zhi 33:1044–1048
Sciuto R, Romano L, Rea S, Marandino F, Sperduti I, Maini CL (2009) Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1503 patients treated at a single institution. Ann Oncol 20:1728–1735
Toniato A, Boschin I, Casara D, Mazzarotto R, Rubello D, Pelizzo M (2008) Papillary thyroid carcinoma: factors influencing recurrence and survival. Ann Surg Oncol 15:1518–1522
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 5:43–63
Kouvaraki MA, Shapiro SE, Fornage BD, Edeiken-Monro BS, Sherman SI, Vassilopoulou-Sellin R (2003) Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery 134:946–954
Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS (2008) Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144:980–987
Besic N, Pilko G, Petric R, Hocevar M, Zgajnar J (2008) Papillary thyroid microcarcinoma: prognostic factors and treatment. J Surg Oncol 97:221–225
Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH (2003) Papillary microcarcinoma of the thyroid—prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Hughes CJ, Shaha AR, Shah JP, Loree TR (1996) Impact of lymph node metastasis in differentiated carcinoma of the thyroid: a matched-pair analysis. Head Neck 18:127–132
Lundgren CI, Hall P, Dickman PW, Zedenius J (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106:524–531
Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Roh JL, Kim JM, Park CI (2008) Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis. Ann Surg Oncol 15:2482–2486
Lim YC, Choi EC, Yoon YH, Kim EH, Koo BS (2009) Central lymph node metastases in unilateral papillary thyroid microcarcinoma. Br J Surg 96:253–257
Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH (2008) Benign and malignant nodules: US differentiation-multicenter retrospective study. Radiology 247:762–770
Riemann B, Schober O (2009) Therapeutic strategy of papillary microcarcinoma of the thyroid gland: a nuclear medicine perspective. Minerva Endocrino 34:81–87
Jeon SJ, Kim E, Park JS, Son KR, Baek JH, Kim YS (2009) Diagnostic benefit of thyroglobulin measurement in fine-needle aspiration for diagnosing metastatic cervical lymph nodes from papillary thyroid cancer correlations with US features. Korean J Radiol 10:106–111
Guo K, Wang Z (2014) Risk factors influencing the recurrence of papillary thyroid carcinoma: a systematic review and meta-analysis. Int J Clin Exp Pathol 7:5393–5403
Lee J, Rhee Y, Lee S, Ahn CW, Cha BS, Kim KR (2006) Frequent, aggressive behaviors of thyroid microcarcinomas in Korean patients. Endocr J 53:627–632
Abboud B, Daher R, Sleilaty G, Abadjian G, Ghorra C (2010) Are papillary microcarcinomas of the thyroid gland revealed by cervical adenopathy more aggressive? Am Surg 76:306–311
Yu X, Song X, Sun W, Zhao S, Zhao J, Wang YG (2017) Independent risk factors predicting central lymph node metastasis in papillary thyroid microcarcinoma. Horm Metab Res 49:201–207
Zhang L, Wei WJ, Ji QH (2012) Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab 97:1250–1257
Chang YW, Kim HS, Kim HY (2015) Should central lymph node dissection be considered for all papillary thyroid microcarcinoma. Asian J Surg 22:1–5
Jiang LH, Chen C, Tan Z, Lu XX, Hu SS, Wang QL, Hou XX, Cao J, Ge MH (2014) Clinical characteristics related to central lymph node metastasis in cN0 papillary thyroid carcinoma: a retrospective study of 916 patients. Int J Endocrinol 2014:385787
Thompson AM, Turner RM, Hayen A, Aniss A, Jalaty S, Learoyd DL, Sidhu S, Delbridge L, Yeh MW, Clifton-Bligh R, Sywak M (2014) A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid 24:675–682
Kim KE, Kim EK, Yoon JH, Han KH, Moon HJ, Kwak JY (2013) Preoperative prediction of central lymph node metastasis in thyroid papillary microcarcinoma using clinicopathologic and sonographic features. World J Surg 37:385–391
Zhao Q, Ming J, Liu C, Shi L, Xu X, Nie X (2013) Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid micro-carcinoma. Ann Surg Oncol 20:746–752
Mazeh H, Samet Y, Hochstein D, Mizrahi I, Ariel I, Eid A (2011) Multifocality in well differentiated thyroid carcinomas calls for total thyroidectomy. Am J Surg 201:770–775
Jovanovic L, Delahunt B, McIver B, Eberhardt NL, Bhattacharya A, Lea R (2010) Distinct genetic changes characterise multifocality and diverse histological subtypes in papillary thyroid carcinoma. Pathology 42:524–533
Lombardi CP, Bellantone R, De Crea C, Paladino NC, Fadda G, Salvatori M (2010) Papillary thyroid microcarcinoma: extrathyroidal extension, lymph node metastases, and risk factors for recurrence in a high prevalence of goiter area. World J Surg 34:1214–1221
Castagna MG, Cantara S, Pacini F (2016) Reappraisal of the indication for radioiodine thyroid ablation in differentiated thyroid cancer patients. J Endocrinol Invest 39:1087–1094
Pacini F, Brianzoni E, Durante C, Elisei R, Ferdeghini M, Fugazzola L, Mariotti S, Pellegriti G (2016) Recommendations for post-surgical thyroid ablation in differentiated thyroid cancer: a 2015 position statement of the Italian Society of Endocrinology. J Endocrinol Invest 39:341–347
Pacini F (2015) Observation for newly diagnosed micro-papillary thyroid cancer: is now the time? J Endocrinol Invest 38:101–102
Appetecchia M, Scarcello G, Pucci E, Procaccini A (2002) Outcome after treatment of papillary thyroid microcarcinoma. J Exp Clin Cancer Res 21:159–164
Vini L, Hyer SL, Marshall J, A’Hern R, Harmer C (2003) Long-term results in elderly patients with differentiated thyroid carcinoma. Cancer 97:2736–2742
Levin KE, Clark AH, Duh QY, Demeure M, Siperstein AE, Clark OH (1992) Reoperative thyroid surgery. Surgery 111:604–609
Acknowledgements
All authors participated in various aspects of the study analysis and interpretation of the data, and in the development of the report. The final version was read and approved by all authors. Chunyi Gui and Min Wang conceived and designed the study and drafted the manuscript. Shenglong Qiu and Min Wang participated in data collection. Chunyi Gui and Zhihai Peng performed the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This research was approved by the Institutional Review Board and Clinical Ethics Committee of Shanghai General Hospital, Shanghai Jiaotong University School of Medicine. The requirement for written informed consent of the patients or their representatives was waived off due to the retrospective nature of this study, in accordance with the guidelines of the American Medical Association. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
No informed consent needed.
Rights and permissions
About this article
Cite this article
Gui, C.Y., Qiu, S.L., Peng, Z.H. et al. Clinical and pathologic predictors of central lymph node metastasis in papillary thyroid microcarcinoma: a retrospective cohort study. J Endocrinol Invest 41, 403–409 (2018). https://doi.org/10.1007/s40618-017-0759-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0759-y