Abstract
Background
Limited and conflicting data exist on an association between mammographic density (MD) and re-excision rates after breast-conserving surgery (BCS). Additionally, the correlation of MD with resection of unnecessary margins during initial BCS is unknown.
Methods
All women with a diagnosis of breast cancer from 2003 to 2012 and enrolled in a larger study on MD were evaluated. Operative and pathology reports were reviewed to determine margin resection and involvement. Mammographic density was determined both by breast imaging-reporting and data system (BI-RADS) classification and by an automated software program (Volpara Solutions). Additional margins were deemed unnecessary if the lumpectomy specimen margin was free of invasive tumor [≥2 mm for ductal carcinoma in situ (DCIS)] or if further re-excision was needed.
Results
Of 655 patients, 398 (60.8 %) had BCS, whereas 226 (34.5 %) underwent initial mastectomy. The women with denser breasts (BI-RADS 3 or 4) underwent initial mastectomy more frequently than the women with less dense breasts (40.0 vs. 30.5 %, respectively; p = 0.0118). Of the patients with BCS, 166 (41.7 %) required separate re-excision. Additional margins were taken during BCS in 192 (48.2 %) patients, with 151 (78.6 %) proving to be unnecessary. In the bivariable analysis, the patients with denser breasts according to BI-RADS classification and volumetric density showed a trend toward requiring more frequent re-excision, but this association was not seen in the multivariable analysis. The rate of unnecessary margins did not differ by breast density. In the multivariate analysis, the re-excision rates increased with DCIS (p < 0.0003) and decreased with resection of additional margins (p = 0.0043).
Conclusions
Mammographic density is not associated with an increased need for re-excision or resection of unnecessary margins at initial BCS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Breast-conserving therapy (BCT) involving excision of the tumor and typically followed by radiation therapy is a widely accepted method for the treatment of invasive and in situ breast cancer (BC) because it provides long-term survival rates similar to those for mastectomy.1,2 Eligibility for BCT is assessed by the surgeon on the basis of tumor-to-breast size ratio, tumor location, and contraindications to radiation therapy.3 Although BCT and mastectomy have equivalent survival outcomes, the risk of local recurrence is higher with BCT, which has been associated with numerous factors including close or positive surgical margins.4–10 It is well-accepted that complete resection of the tumor is essential, yet the necessary margin of normal tissue surrounding the tumor has been widely debated, resulting in considerable practice variation.
Practices for defining an adequate margin range from accepting no tumor on ink to requiring 1-cm margins.11,12 Only recently has a consensus guideline for margins in breast-conserving surgery (BCS) been published.13
Positive or close margins are typically addressed with additional surgical excision through either re-excision lumpectomy or conversion to mastectomy. The rates of margin re-excision for positive or close margins vary widely, reportedly ranging between 15 and 70 % and reflecting the extreme variation in practice patterns regarding margin width.12,14–16 This can lead to significant anxiety for patients, delay adjuvant therapy, worsen cosmesis, and increase total treatment costs.14,16,17
Several studies have attempted to elucidate predictors of positive surgical margins after lumpectomy. Factors that have been linked to margin positivity include tumor size, resection volume, proportion of ductal carcinoma in situ (DCIS) in core specimens, multifocality, nodal status, lobular histology, tumors with an extensive intraductal component (EIC), and necrosis on core biopsy.3,16,18–27 Although the effect of mammographic density (MD) on margin status has been assessed through several retrospective studies, data are both limited and conflicting.3,16,28 Additionally, the impact of MD on margin positivity may be underappreciated due to use of the BI-RADS classification scheme, which relies on subjective classification.29
The extent of BC in women with dense breast tissue may be more difficult to define at the time of surgery. This could potentially lead to resection of additional unnecessary tissue at the initial lumpectomy or higher re-excision rates if tumor is present at or near the margin and not detected at the time of surgery.
We sought to evaluate the effect of MD on resection of additional margins at the time of initial BCS and the need for re-excision due to positive margins using both BI-RADS classification of MD and continuous, automated, volumetric breast density measurements.
Methods
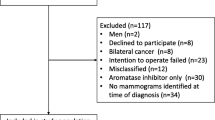
All women 18 years of age and older with a diagnosis of BC from January 2003 to December 2012 and enrolled in a larger, single-center study on MD and BC risk (n = 839) were eligible for this retrospective study. Briefly, the larger study involved collection of risk factor information with the goal of developing a BC risk model that includes MD. This study was approved by our institutional review board (HSR #15885) and was compliant with the Health Insurance Portability and Accountability Act (HIPAA).
The inclusion criteria for the larger study specified a diagnosis of BC between January 2003 and December 2012 with “for processing” mammographic images at the time of cancer diagnosis available in the picture archiving and communication system (PACS). The exclusion criteria from the larger study specified lack of bilateral digital mammography before initiation of treatment, patients without follow-up assessment or unavailable pathologic information, bilateral BC at the initial diagnosis, a new cancer diagnosis in the contralateral breast within 1 year after the initial diagnosis, and history of breast implants or reduction surgery. Patient demographics and clinical information were collected through a combination of patient survey and retrospective chart review.
Mammographic density was abstracted from existing imaging reports using the breast imaging reporting and data system (BI-RADS) category reported in the mammogram closest to the time of cancer diagnosis. The BI-RADS density definitions included the following: almost entirely fatty MD (<25 % glandular), scattered fibroglandular densities (25–50 % glandular), heterogeneous density (51–75 % glandular), and extreme density (>75 % glandular).30 Outcomes are reported for both dense breasts (BI-RADS 3 and 4) compared with less dense breasts (BI-RADS 1 and 2) and for extremely dense breasts (BI-RADS 4) compared with the other breast density categories (BI-RADS 1–3). Additionally, volumetric breast density measurements were obtained for each patient via a commercially available automated software program (Volpara Solutions, Wellington, New Zealand) using the mean calculated percentage of density.
Pathology reports were reviewed to determine tumor type, invasive tumor size, histologic grade, multifocality, presence of DCIS, stage at diagnosis, lymph node positivity, number of additional margins resected at initial BCS, and margin involvement. Margins were deemed negative if the inked margin was free of invasive tumor and if the margins were 2 mm or wider for DCIS. Unnecessary margins were defined as those resected when margins on the primary lumpectomy specimen were free of invasive tumor involvement or at least 2 mm wide for DCIS, or if separate re-excision still was needed for positive or close margins. Lymph node positivity included both macrometastases (N1 or higher) and micromatastases (N1mic), but isolated tumor cells (N0i+) were classified as node negative.31
The pathologic stage at diagnosis was determined using American Joint Committee on Cancer (AJCC) 7th edition criteria except for patients who received neoadjuvant therapy, for whom clinical stage as documented in the medical chart was recorded.31 Pathology reports were reviewed for all subsequent procedures to elicit the final surgical procedure performed (re-excision lumpectomy vs. mastectomy) for that BC event as well as surgeries performed for lymph node resection. The clinical record was additionally reviewed for cancer detection method, categorized as palpable mass, mammographic screening, or other.
The association between MD and the need for separate re-excision after BCS as well as resection of additional margins at time of initial BCS was examined in conjunction with patient clinicopathologic factors. Continuous variables were evaluated using the Kruskal–Wallis test or the Wilcoxon signed rank test as appropriate, with values reported as medians and provided interquartile ranges (IQRs). Categorical variables were analyzed using Pearson χ 2 or Fisher’s exact test. Logistic regression was used to evaluate the association between the need for re-excision after initial BCS and MD, with adjustment for variables significant on the bivariate analysis. Separate regression models were constructed to analyze this relationship, first using BI-RADS classification and then using continuous volumetric breast density. All statistical analyses were performed using SAS statistical software version 9.3 (SAS Institute, Cary, NC, USA), with p values lower than 0.05 considered significant.
Results
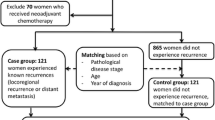
Of 839 patients with a diagnosis with BC and enrolled in the larger MD study who were eligible for this study; 655 had sufficient clinical data to be included in the analysis. Of these patients, 398 (60.8 %) had initial BCS, and 226 (34.5 %) had initial mastectomy, whereas 31 had no surgery identifiable in our medical record.
Of the 655 patients in the study population, 480 had invasive tumors (73.3 %) with a median tumor size of 1.3 cm (IQR 0.8–2.1). Ductal carcinoma in situ was present in 477 patients (72.8 %), including both patients with DCIS alone and those with concomitant invasive disease. Among the women in our study, 110 (16.8 %) had fatty MD (BI-RADS 1), 270 (41.2 %) had scattered MD (BI-RADS 2), 223 (34 %) had heterogeneously dense MD (BI-RADS 3), and 52 (8 %) had extremely dense breasts (BI-RADS 4). Women with either heterogeneously or extremely dense breasts were more likely to undergo initial mastectomy (40 %) than women with fatty or scattered glandular densities (30.5 %) (p = 0.0118). Patients with denser breasts were more likely to have stage 3 or 4 disease at the time of diagnosis (13.5 %) than patients with less dense breasts (7.6 %) (p = 0.0145). There was no significant difference in the proportion of patients with invasive disease or in the tumor size among MD categories (data not shown).
Of the 398 patients who underwent BCS, 80 (20.1 %) were classified as having fatty MD and 170 (42.7 %) as having scattered MD, whereas 121 (30.4 %) had heterogeneously dense MD, and 27 (6.7 %) had extremely dense MD according to BI-RADS classification (Table 1). The women with dense breasts were significantly younger (p < 0.0001) and had a lower body mass index (BMI) (p < 0.0001) than the women with less dense MD categories. The patients with greater MD were less likely to have their BC detected by mammography and more likely to have had a palpable tumor leading to their BC diagnosis than the women with lower MD (p = 0.0011). The women with extremely dense breasts were found to have a significantly higher rate of HER-2-neu positivity (p = 0.011) than the women falling into different MD categories. There was no significant difference across MD categories in terms of histologic tumor type, tumor grade, tumor size, or nodal involvement, although women with extremely dense breasts were significantly more likely to have multifocal disease (p = 0.041).
Additional margins were taken during the initial BCS in 192 patients (48.2 %), with margins in 151 patients (78.6 %) unnecessarily resected secondary either to clear surgical margins of the primary lumpectomy specimen or to the requirement of additional surgery for positive or close margins. No significant association was found between MD and the resection of additional margins. However, among patients with extremely dense breasts in whom additional margins were resected, none of these margins contributed to margin clearance.
Of 398 patients who had BCS, 166 (41.7 %) required separate margin re-excision due to positive or close margins (Table 2). The patients requiring re-excision were younger (p = 0.0094) and more likely to have DCIS (p < 0.0001) and multifocal disease (p = 0.0052). The women with denser breasts by traditional BI-RADS classification and by automated volumetric density showed a trend toward greater likelihood of requiring additional surgery for positive or close margins, although this difference did not reach statistical significance in the bivariable analysis (p = 0.0519 and 0.0622, respectively). Of the patients requiring additional surgery for positive or close margins, 50 (30.1 %) ultimately underwent mastectomy as their definitive surgery. The rate of conversion to mastectomy after initial BCS did not differ significantly among the MD categories in (p = 0.1149), with an overall rate for conversion to mastectomy of 12.8 %.
After adjustments for age, presence of DCIS, multifocality, and resection of additional margins at initial BCS in the multivariable logistic regression, MD was not associated with the need for re-operation regardless whether breast density was captured by BI-RADS classification or quantitatively by volumetric density. The presence of DCIS was associated with increased rates of margin involvement, whereas the resection of extra margins at initial BCS was significantly associated with decreased rates of re-excision. The association between re-excision and tumor multifocality was marginally significant in the logistic regression model using volumetric breast density but failed to reach statistical significance in the model using categorical BI-RADS classification of MD (Table 3).
Discussion
Our study demonstrated that although women with mammographically dense breasts were more likely to undergo initial mastectomy, MD was not associated with the need for re-excision after the initial BCS attempt. Additionally, when BCS was attempted, MD was not associated with a higher risk of conversion to mastectomy. Importantly, this finding was consistent when either a continuous volumetric breast density measure or a categorical, qualitative density measure was used. Although other studies have used the BI-RADS classification scheme for MD, which relies on subjective classification, the main strength of our study was the use of both BI-RADS classification and quantitative volumetric breast density measurements allowing for evaluation of density as a continuous variable to assess this relationship. Regardless of the method used to quantify breast density, our study found no association between MD and margin involvement after adjustment for other confounders.
In our study, only the presence of DCIS and the resection of additional margins during the initial BCS were consistently predictive of a need for margin re-excision. Findings have previously shown both to be associated with the need for re-excision after initial BCS.3,16,22,24,32 Thus, although the re-excision rate after BCS remains high, it does not appear that MD plays a significant role in determining margin status, and most women with initially positive margins will ultimately undergo successful BCS without conversion to mastectomy.
Our findings regarding MD and the need for re-excision after BCS and higher initial mastectomy rates in the setting of greater MD are consistent with findings from Kapoor et al.28 In addition to affirming these findings, our study demonstrated that this result holds true even when objective volumetric continuous measurements of breast density are used. In contrast, other studies have suggested that MD may have an association with margin status after BCS. A study by Bani et al.3 found that MD is associated with the need for a second operation after BCS, citing a 42 % rate of margin involvement for women with extremely dense breast compared with only 18 % for women with less dense breasts [odds ratio (OR) 3.2; 95 % confidence interval (CI) 1.2–11.0; p = 0.003]. Another study by Shin et al.16 found an association between extremely dense MD and positive surgical margins (OR 4.515; 95 % CI 1.574–12.951; p = 0.005).
Our second objective was to determine whether MD influences the rate of resection of additional margins at the time of initial BCS. We found that nearly half of the patients had additional margins resected during their initial surgery, with only one in five of these patients obtaining clear surgical margins by this additionally resected tissue. Although no association between MD and resection of additional margins was found, it is important to note that none of the additional margins resected in patients with extremely dense breasts contributed to margin clearance. It is possible that surgeons have a more difficult time assessing surgical margins intraoperatively based on tissue appearance or feel in women with extremely dense breasts, but the small sample of patients with extreme MD in our study limited this analysis.
To our knowledge, no other studies have investigated the impact of MD on resection of additional surgical margins during initial BCS. However, a study by Huston et al.32 found that complete resection of four to six margins together with the primary lumpectomy specimen improved reoperation rates from 38.7 to 17.7 %, whereas another study by Balch et al.18 found that 67 % of the additional margins resected were grossly tumor-free margins and did not require excision. The surgeons included in our study did not routinely take cavity-shave margins. Instead, resection of additional margins was performed selectively based on clinical suspicion or intraoperative imaging.
Our study was limited by the large number of patients who had insufficient data for analysis, with 165 of these patients excluded due to imaging insufficient for obtaining volumetric measurements. Additionally, only 27 patients (6.7 %) undergoing initial BCS were classified as having extremely dense breasts according to BI-RADS classification, which limited the study’s power.
In summary, our study did not find an association between MD and rate of margin involvement, nor did MD have a significant impact on the rate of conversion to mastectomy. Additionally, our study did not find an association between MD and excision of additional margins at initial BCS. Therefore, mammographic density, whether measured categorically or volumetrically, should not influence surgical decision making concerning patient candidacy for breast conservation. Newly issued guidelines likely will change practice patterns as they relate to margin re-excision, perhaps reducing unnecessary margin excision or re-excision.13 Moreover, new technologies are needed to further reduce re-excision rates after lumpectomy and to better assess margin adequacy intraoperatively.
References
Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
Bani MR, Lux MP, Heusinger K, et al. Factors correlating with re-excision after breast-conserving therapy. Eur J Surg Oncol. 2009;35:32–7.
Houssami N, Macaskill P, Marinovich ML, Morrow M. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2014;21:717–30.
MacDonald H, Silverstein MJ, Lee LA, et al. Margin width as the sole determinant of local recurrence after breast conservation in patients with ductal carcinoma in situ of the breast. Am J Surg. 2006;192:420–2.
Martin-Dunlap TM, Cyr AE, Mushawah FA, Fao F, Margenthaler JA. Does the volume of ductal carcinoma in situ impact the positive margin rate in patients undergoing breast conservation for invasive breast cancer? J Surg Res. 2013;84:228–33.
Wang SY. Shamliyan T, Virnig BA, Kane RL. Tumor characteristics as predictors of local recurrence after treatment of ductal carcinoma in situ: a meta-analysis. Breast Cancer Res Treat. 2011;127:1–14.
Wang SY, Chu H, Samliyan T, Jalal H, Kuntz HM, Kane RL, Virnig BA. Network meta-analysis of margin threshold for women with ductal carcinoma in situ. J Natl Cancer Inst. 2012;104:507–16.
Reedijk M, Hodgson N, Gohla G, Boylan C, et al. A prospective study of tumor and technical factors associated with positive margins in breast-conservation therapy for nonpalpable malignancy. Am J Surg. 2012;204:263–8.
Smitt MC, Nowels K, Carlson RW, Jeffrey SS. Predictors of re-excision findings and recurrence after breast conservation. Int J Rad Oncol. 2003;57:979–85.
Blair SL, Thompson K, Rococco J, Malcarne V, Beitsch PD, Ollila DW. Attaining negative margins in breast-conservation operations: is there a consensus among breast surgeons? J Am Coll Surg. 2009;209:608–13.
McCahill LE, Single RM, Aiello Bowles EJ, et al. Variability in re-excision following breast conservation surgery. JAMA. 2012;307:467–75.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology–American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Int J Radiation Oncol Biol Phys. 2014;88:553–64.
Ananthakrishnan P, Balci FL, Crowe JP. Optimizing surgical margins in breast conservation. Int J Surg Oncol. 2012. DOI 10.1155/2012/585670.
Sabel MS, Rogers K,Griffith K, et al. Residual disease after re-excision lumpectomy for close margins. J Surg Oncol. 2009;99:99–103.
Shin H, Han E, Moon H, et al. Nomogram for predicting positive resection margins after breast-conserving surgery. Breast Cancer Res Treat. 2012;134:1115–23.
Mullen R, Macaskill EJ, Khalil A, et al. Involved anterior margins after breast conserving surgery: Is re-excision required? Eur J Surg Oncol. 2012; 38:302–6.
Balch GC, Mithani SK, Simpson JF, Kelley MC. Accuracy of intraoperative gross examination of surgical margin status in women undergoing partial mastectomy for breast malignancy. Am Surg. 2005;71:22–7.
Beron PJ, Horwitz EM, Martinez AA, et al. Pathologic and mammographic findings predicting the adequacy of tumor excision before breast-conserving therapy. Am J Roentgenol. 1996;167:1409–14.
Dillon MF, Maguire AA, McDermott EW, Myers C, Hill AD, O’Doherty A, Quinn CM. Needle core biopsy characteristics identify patients at risk of compromised margins in breast conservation surgery. Mod Pathol. 2008;21:39–45.
Fadare O, Clement NF, Ghofrani M. High- and intermediate-grade ductal carcinoma in situ of the breast: a comparison of pathologic features in core biopsies and excisions and an evaluation of core biopsy features that may predict a close or positive margin in the excision. Diagn Pathol. 2009. DOI:10.1186/1746-1596-4-26.
Kurniawan ED, Wong MH, Windle I, et al. Predictors of surgical margin status in breast-conserving surgery within a breast screening program. Ann Surg Oncol. 2008;15:2542–9.
Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, Simunovic M. The relationship between surgical factors and margin status after breast conservation surgery for early stage cancer. Am J Surg. 2009;197:740–6.
Melstrom LG, Melstrom KA, Wang EC, Pilewskie M, Winchester DJ. Ductal carcinoma in situ: size and resection volume predict margin status. Am J Clin Oncol. 2010;33:438–42.
Neushatz AC, DiPetrillo T, Steinhoff M, et al. The value of breast lumpectomy margin assessment as a predictor of residual tumor burden in ductal carcinoma in situ of the breast. Cancer. 2002;94:1917–24.
Sakr RA, Poulet B, Kaufman GJ, Nos C, Clough KB. Clear margins for invasive lobular carcinoma: a surgical challenge. Eur J Surg Oncol. 2011;37:350–6.
Wazer DE, Schmidt-Ullrich RK, Schmid CH, Ruthazer R, Kramer B, Safaii H, Graham R. The value of breast lumpectomy margin assessment as a predictor of residual tumor burden. Int J Radiat Oncol Biol Phys. 1997;38:291–9.
Kapoor NS, Eaton A, King TA, et al. Should breast density influence patient selection for breast-conserving surgery? Ann Surg Oncol. 2013;20:600–6.
Nicholson BT, LoRusso AP, Smolkin M, Bovjerg VE, Petroni GR, Harvey JA. Accuracy of assigned BI-RADS breast density category definitions. Acad Radiol. 2006;13:1143–9.
American College of Radiology. Breast imaging reporting and data system (BI-RADS) atlas. 4th edition. American College of Radiology, Reston, 2013.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (eds). AJCC cancer staging manual. 7th ed. Springer, New York, 2010.
Huston TL, Pigalarga R, Osborne MP, Tousimis E. The influence of additional surgical margins on the total specimen volume excised and the reoperative rate after breast-conserving surgery. Am J Surg. 2006;192:509–12.
Acknowledgment
This research was supported by NIH training grant CA163177 and Department of Defense for “Building a Better Model: A Personalized Breast Cancer Risk Model Incorporating Breast Density to Stratify Risk and Improve Application of Resources,” PI: Jennifer Harvey, MD, University of Virginia, Charlottesville, Virginia, Proposal Number BC100474, Award Number W81XWH-11-1-0545, HRPO Log Number A-17074.
Conflict of Interest
Jennifer A. Harvey Volpara Solutions, Ltd. Wellington, New Zealand, Shareholder, research agreement; Hologic, Inc., Danbury CT, Shareholder, research agreement; VuComp, Inc., Dallas, TX. Research agreement. No other authors have financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Edwards, B.L., Guidry, C.A., Larson, K.N. et al. Does Mammographic Density have an Impact on the Margin Re-excision Rate After Breast-Conserving Surgery?. Ann Surg Oncol 23, 782–788 (2016). https://doi.org/10.1245/s10434-015-4917-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4917-1