Abstract
A positive resection margin after breast-conserving surgery (BCS) is the most important risk factor for tumor recurrence. Re-excision after BCS often results in unnecessary wider excisions, or even mastectomies and poor cosmetic results, as well as increased medical costs and patients’ anxiety. A nomogram for predicting positive resection margins may allow the surgeon to develop an individualized surgical plan. Data from 1,034 consecutive breast cancer patients with invasive or in situ breast cancer who initially underwent BCS between January 2008 and December 2009 were used to develop a nomogram for predicting positive resection margins. The nomogram was then validated independently using a cohort of 563 patients who underwent breast surgery in 2010. Multivariate logistic regression analysis showed that microcalcifications (OR 1.574, P = 0.034), grade 4 mammographic density (OR 4.515, P = 0.005), >0.5 cm difference in tumor size between magnetic resonance imaging and ultrasonography (OR 10.001, P < 0.0001), ductal carcinoma in situ (DCIS) on needle biopsy (OR 1.575, P = 0.044), and lobular component on needle biopsy (OR 3.985, P = 0.015) were independent predictors of positive resection margins. These significant variables were used to develop a nomogram for predicting positive resection margins after BCS; the AUCs of the study and the validation cohorts were 0.823 [95 % confidence interval (CI), 0.785–0.862] and 0.846 (95 % CI, 0.800–0.892), respectively. Our new nomogram using 5 variables that were determined before surgery to predict positive resection margins should aid the surgeon in developing individualized surgical plans for breast cancer patients who are scheduled for BCS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast-conserving surgery (BCS) is widely accepted as standard therapy for invasive and in situ breast cancer. BCS followed by breast irradiation for breast cancer has provided acceptable cosmetic results and long-term survival similar to mastectomy for disease-free, distant disease-free, and overall survival [1, 2]. The main disadvantage of BCS is the potential risk of local recurrence; the most important risk factor for local recurrence after BCS is positive resection margins [3, 4], which occur at frequencies ranging from 17 to 59 % [5]. When there is a positive margin after BCS, patients should undergo further surgery. However, re-excisions often result in poor cosmetic results and unnecessary wider excisions as well as increased medical costs and patients’ anxiety for unexpected additional operation.
To obtain clear resection margins and reduce re-excision rates, some surgeons obtain intraoperative assessments of the margins of excised specimens, using either analysis of frozen sections or mammography of the specimen. Although specificity rates range between 98 and 100 %, the sensitivity of frozen section analysis ranges between 65 and 78 % [6]. The accuracy of specimen mammography has been reported to be about 60 %, which is much lower than the accuracy of frozen section analysis [7]. False-negative results of frozen section analysis lead to reoperations, and false-positive results can lead to unnecessary excisions or even mastectomies. In addition, the results of these evaluations take 30 min or more after the excision is performed. Furthermore, frozen section analysis during BCS has been reported not to reduce overall local recurrence rates [8], and the majority of breast surgeons in the United States have not routinely performed intraoperative frozen section analysis to assess the status of margins during BCS [9]. Therefore, determining the risk of positive resection margins before BCS may be advantageous for both surgeons and patients.
Several factors have been associated with positive resection margins, including lobular histology, size of tumor on pathology, tumor grade, multifocality, and the presence of extensive intraductal component (EIC), and lymphovascular invasion (LVI) [10]. However, information on many of these factors is only available from evaluation of paraffin-embedded specimen after BCS. The aims of this study were to identity the preoperative predictors of positive resection margins and to develop and evaluate a nomogram for predicting positive resection margins after BCS.
Patients and methods
Patients
A prospectively maintained database (Seoul National University Hospital Breast Care Center Database) was used to retrospectively identify 1,867 patients who underwent curative surgery for invasive breast cancer or ductal carcinoma in situ (DCIS) between January 2008 and December 2009. Of these patients, 250 receiving neoadjuvant chemotherapy, 49 with unavailable preoperative imaging or pathologic results, and 534 undergoing mastectomy as their initial operation were excluded from the study. The remaining 1,034 patients who were scheduled for BCS were analyzed and their data were used to develop a nomogram. A core needle biopsy was used for preoperative diagnosis, and all patients underwent preoperative evaluations using mammography, ultrasonography (US), and magnetic resonance imaging (MRI).
External validation of the nomogram was performed using data from another 563 patients with same enrollment criteria, who underwent curative surgery between January and December 2010 at the same institution. Table 1 summarizes the clinicopathologic characteristics of the initial study cohort and the validation cohort.
Mammography
Mammography was performed using a full-field digital mammography system (Senographe DS, GE Medical Systems, Buc, France or Lorad Selenia, Hologic Inc., Bedford, USA). Mammographic density was categorized into 4 grades according to amount of fibroglandular tissue (grade 1, <25 %; grade 2, 26–50 %; grade 3, 51–75 %; and grade 4, >75 %).
Breast ultrasonography
Experienced breast radiologists performed all preoperative breast US using 5–14-MHz linear transducers (EUB-8500 scanner; Hitachi Medical, Tokyo, Japan; or IU-22; Philips Healthcare, Amsterdam, Netherlands). The radiologists reported the shape and size of each tumor and location in three-dimensions according to the BI-RADS classification system.
Breast magnetic resonance imaging
The protocol used for breast MR image acquisition and data analysis was reported previously [11]. Breast MRI was performed on a 1.5-T system (Signa; General Electric Medical Systems, Milwaukee, WI, USA) using a dedicated double-breast coil (8-channel HD breast array; General Electric Medical Systems). Prior to surgery, radiologists with 5–20 years of experience in breast imaging interpreted and recorded preoperative MRI findings using a picture archiving and communication system (PACS) according to the BI-RADS classification system.
Surgery and pathologic examination
Surgeons aimed for a grossly negative 1-cm margin during the first lumpectomy. For all patients with non-palpable lesions, the location of the tumor was determined by mammography or US-guided needle localization before surgery. When an invasive cancer or DCIS was found in the resection margin of the resected specimen, re-excision or mastectomy was performed to obtain tumor-free margins.
The resection margin was classified as positive or clear based on pathologic evaluation. The presence of DCIS or invasive cancer at the edge of a specimen constituted a positive resection margins. The presence of DCIS less than 1 mm from the resection margin in a paraffin-embedded specimen was considered to be a positive margin, in accordance with the 2011 NCCN clinical guidelines that defined margins <1 mm as inadequate [12].
Tumor size, nodal status, histology, and the status of resection margins were reported for each surgical resection. The expression of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and Ki-67 expression were evaluated by immunohistochemistry (IHC). ER and PR positivity was defined as ≥10 % positive tumor cells with nuclear staining. HER2 status was determined either by IHC or fluorescence in situ hybridization (FISH). A triple-negative breast tumor was defined as ER negative, PR negative, and HER2 negative regardless of whether it was invasive cancer or DCIS.
Statistical analysis
Descriptive statistics were used to characterize the study and validation cohorts. The variables of patients with clear resection margins and those with positive resection margins were compared using Pearson’s χ 2 tests. Multivariate logistic regression analysis was used to analyze each variable with a P value <0.05 on the Pearson’s χ 2 test. Odds ratios (ORs) and points for developing a nomogram were calculated for each variable. A receiver operating characteristics (ROC) curve was drawn and the area under the curve (AUC) was calculated to assess the discrimination power of the nomogram for the study and validation cohorts. It is generally accepted that AUC values of 0.7–0.8 represent reasonable discrimination, and those values exceeding 0.8 represent good discrimination [13]. Calibration of the nomogram was assessed graphically by plotting the actual proportions against the predicted probabilities. The vertical axis represented the actual observed incidence (actual proportion), and the horizontal axis represented the probability calculated by the nomogram (predicted probability). A perfectly accurate nomogram prediction model would result in a plot where the observed and predicted probabilities for given groups fall along the 45-degree line. The distance between the confidence interval of the actual proportion at each predicted probability and the 45-degree line is a measure of the absolute error of the nomogram’s prediction [14]. All statistical analyses were performed using SPSS Version 17.0 software (SPSS, Chicago, IL, USA) and R software Version 2.10.1 (http://www.r-project.org/). All P values were two sided, and P < 0.05 was considered significant.
Results
Clinicopathologic characteristics of the cohort used to develop the nomogram (study cohort)
Among the 1,034 patients who underwent BCS, 929 patients had invasive breast cancer with or without DCIS and 105 patients had pure DCIS on permanent pathology. The mean age at diagnosis was 48.4 years (range, 26 to 85 years). Resection margins were positive in 151 patients (14.6 %) after the initial lumpectomy. Candidate predictors for positive resection margins were selected from the preoperative clinical information, images, and pathologic data.
Results of multivariate analyses for resection margin status
Table 2 summarizes the variables where there were significant differences between patients whose excised tumors had clear margins and those with tumors having positive margins. HER2 and Ki67 were not significantly associated with the status of margin (P = 0.780 and P = 0.875, respectively).
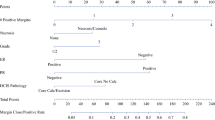
Variables found significant by Pearson’s χ 2 analysis were analyzed by multivariate logistic regression. Microcalcifications (OR 1.574, P = 0.034), grade 4 mammographic density (OR 4.515, P = 0.005), >0.5 cm difference in tumor size between MRI and US (OR 10.001, P < 0.0001), DCIS on needle biopsy (OR 1.575, P = 0.044), and lobular component on needle biopsy (OR 3.985, P = 0.015) were significantly associated with positive resection margins (Table 3). Younger age at diagnosis (OR 1.137, P = 0.557), multifocality on imaging (OR 1.665, P = 0.166), tumor size >5 cm on MRI (OR 1.622, P = 0.205), hormonal receptor status (OR 1.851, P = 0.110), and triple-negative breast tumor (OR 0.725, P = 0.476) were insignificant factors on multivariate analysis.
Development and validation of nomogram
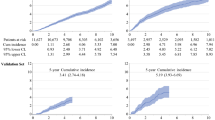
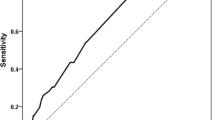
Based on the results of the multivariate analysis, a nomogram was developed to predict the likelihood of positive resection margins (Fig. 1). The nomogram included the 5 variables which were statistically significant on multivariate analysis. A total point is the sum of points for each variable and the probability of positive resection margins is the corresponding number of the total points in the nomogram. For instance, the probability of positive resection margins after BCS is <10 % if a total point is <60. When a total point is >200, the probability of positive margins is >70 %. The AUC of the study cohort was 0.823 [95 % confidence interval (CI), 0.785–0.862].
The AUC of the validation cohort was 0.846 (95 % CI, 0.800–0.892). Calibration of the nomogram was assessed using the independent validation cohort. The patients were grouped in deciles of predicted probabilities, and to calibrate the nomogram, the actual proportion of patients with positive resection margins was calculated for each decile. In general, the actual proportion of patients with positive resection margins and the predictive probability of positive resection margins were similar, according to the calibration plot. The predictive probabilities of the 7th and the 9th groups were a little higher and a little lower, respectively, than the actual probabilities of those groups (Fig. 2).
Discussion
The status of the margins of excised tumor specimens is the most important factor associated with local recurrence in patients with invasive breast cancer and DCIS who undergo BCS; however, the optimal size of tumor-free margin is still controversial. Recent studies have shown that excised invasive breast cancer with wider tumor-free margins were not necessarily associated with lower local recurrence rate [15, 16]. A similar result was reported from a recent study of 382 patients with pure lobular carcinoma who underwent BCS [17]. In DCIS patients, positive margins clearly increase the risk of ipsilateral breast tumor recurrence. In addition, there is a significant trend toward increased risk of local recurrence in patients with DCIS whose excised tumors have tumor-free margins <2 mm [18, 19]. Silverstein et al. [20] reported that patients with DCIS undergoing BCS whose excised tumors had margins <1 mm benefited from postoperative radiation therapy. NCCN guidelines have defined clear resection margins in excised invasive breast cancers as pathologically negative margin; however, for DCIS, margins <1 mm are considered in adequate [12]. According to previous studies and the 2011 NCCN guidelines, a narrow tumor-free resection margin of DCIS is a risk factor for local recurrence, and in our study, a margin <1 mm in DCIS was defined as a positive resection margin.
To avoid positive resection margins, it is important to identify the location and extent of tumor preoperatively. Imaging studies, including mammography, US, and MRI, are widely used for preoperative localization of breast tumor. However, additional imaging, such as breast MRI, does not reduce the rates of positive resection margins, re-excision, or reoperation [21, 22]. Intraoperative analysis of frozen sections aids the surgeons in deciding in a balanced manner between wider excisions for oncologic safety and cosmetic conservation of the breast [5]. Intraoperative frozen section analysis is routinely performed at Seoul National University Hospital. Among the study cohort, 97 patients (9 %) avoided reoperation because of frozen section analysis; therefore, frozen section analysis may decrease reoperation rates. However, false-positive results from frozen section analysis resulted in 103 patients (9.7 %) undergoing unnecessary wider excisions or mastectomies. Furthermore, in our institution, the false-negative rate of frozen section analysis has been 5 %. Olson et al. [23] reported a 5.8 % false-negative rate from frozen section analysis of specimens from 290 patients with positive resection margins, and Ohuchi and coworkers [24]. reported a 9.8 % margin-positive rate in 122 patients after total-circumference surgical margin shaved from the remnant breast was examined using intraoperative frozen section analysis. Moreover, Cendan et al. [25] found a false-negative rate of 22.7 % for frozen section analysis of specimens from 97.
Several studies have addressed the risk factors for positive resection margins. Lovrics et al. [10] examined specimens from 489 patients. By multivariate analysis, tumor size, ductal histology, lymphovascular invasion, multifocality, and palpability were identified as predictors of margin status. Tartter et al. [26] examined 674 patients who underwent BCS and found that younger age, family history of breast cancer, large tumor size, DCIS, and EIC were associated with positive resection margins on univariate analysis; however, only large tumor size was associated with positive margin status in multivariate analysis. Mann and coworkers [27] analyzed 1,648 patients who underwent BCS and found a re-excision rate of 17.1 %. In this study, mammographic microcalcifications, absence of mammographic mass, DCIS, high tumor grade, large tumor size, multi ocality, and lobular histology were associated with positive resection margins. We then identified predictors of positive margin status focusing on data from imaging studies and pathologic examination that were available preoperatively. We found on multivariate analysis that microcalcifications on mammography, grade of mammographic density, >0.5 cm difference in tumor size between MRI and US, DCIS, and lobular components on needle biopsy independently predicted positive resection margins in multivariate analysis.
Pleijhuie et al. [6] suggested that positive margins might be a result of the restrictive visibility of tumor and coexisting DCIS on preoperative imaging studies. Therefore, assessing the extent of DCIS during surgery is important. In our study, microcalcifications were usually discovered in patients with DCIS, and we assume that microcalcifications on mammography indicate the presence of DCIS or invasive cancer with DCIS. We also found an association between mammographic density and margin status. Several previous studies have documented the association between dense breasts and columnar cell lesions, hyperplasia without atypia, atypical hyperplasia, and even carcinoma in situ or breast cancer [28–30]. Based on these results, we can infer that epithelial hyperplasia or atypical lesions would be more frequently observed adjacent to invasive breast cancers or DCIS in dense breasts, and these characteristics of the dense breasts could be risk factors for positive resection margins.
A novel finding of our study was that a tumor appearing larger on MRI than US was a predictive for margin status. In previous studies, breast MRI has shown higher accuracy for DCIS and for invasive breast cancer with DCIS than mammography or US [31, 32]. Breast MRI enhanced nonmalignant lesions such as atypical ductal hyperplasia, lobular carcinoma in situ, ductal hyperplasia, and fibrosis [33], whereas US tended to underestimate the presence of intraductal components [34, 35]. We previously reported that breast MRI was more accurate than US for predicting tumor extent in patients with invasive cancer with DCIS or pure DCIS, whereas both breast MRI and US were useful for measuring the tumor sizes of invasive breast cancers without DCIS [36]. The difference in sizes determined by MRI and US might be related to the differences in imaging capabilities and reflect hidden DCIS or invasive cancer with DCIS that were not apparent on US images.
The association of the finding of DCIS on needle biopsy with margin status after BCS has also been previously reported [27, 37, 38]. Similar to earlier reports, we found by multivariate analysis that the presence of DCIS was a strong predictor of positive resection margins. We assume that DCIS could be detected by needle biopsy when the tumor consisted of pure DCIS or when a relatively high proportion of DCIS was adjacent to invasive breast cancer. Lobular histology has also been known to be a risk factor for positive margins [39]. In our study, most breast tumors with lobular components such as invasive lobular cancer or lobular carcinoma in situ were underestimated by preoperative US and MRI, which might have resulted in incomplete surgical excisions.
This study has strengths compared with others in the literature. First, we assembled a relatively large cohort of patients with complete results from imaging, including breast MRI and US, and pathologic examinations. Second, all patients’ data were consistently maintained by experienced radiologists and pathologists as well as breast surgeons. However, this study also has several limitations. First, this was a retrospective study and there may be bias in the analysis of data. Second, this was a single-institution study, which might have resulted in variations in the interpretations of preoperative US and MRI. Furthermore, a prospective and multi-institutional study is needed to address this issue and assess external validity of our nomogram.
In summary, using multivariate analysis, we identified 5 variables predictive of positive resection margins in excised specimens of patients undergoing BCS. The variables were microcalcifications, grade of mammographic density, >0.5 cm difference in tumor size between MRI and US, DCIS on needle biopsy, and lobular histology on needle biopsy. Based on the results of multivariate analysis, we developed a new nomogram to determine the probability of positive resection margins, and validated the nomogram using an independent cohort of breast cancer patients. Because of the high accuracy and convenience of the nomogram, its preoperative application to patients with invasive breast cancer or in situ cancer may allow breast surgeons to individualize surgical planning with regard to obtaining clear resection margins. If the nomogram indicates that the excised specimen will have a high probability of positive resection margins, the surgeon can perform a wider excision or use frozen section analysis to obtain clear resection margin during the initial BCS. In addition, the results of nomogram analysis can help patients understand the possibility of undergoing additional procedures because of positive resection margins, and help the patient choose a surgical option surgery.
References
van Dongen JA, Voogd AC, Fentiman IS, Legrand C, Sylvester RJ, Tong D, van der Schueren E, Helle PA, van Zijl K, Bartelink H (2000) Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst 92:1143–1150
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241. doi:10.1056/NEJMoa022152
Kreike B, Hart AA, van de Velde T, Borger J, Peterse H, Rutgers E, Bartelink H, van de Vijver MJ (2008) Continuing risk of ipsilateral breast relapse after breast-conserving therapy at long-term follow-up. Int J Radiat Oncol Biol Phys 71:1014–1021. doi:10.1016/j.ijrobp.2007.11.029
Mechera R, Viehl CT, Oertli D (2009) Factors predicting in-breast tumor recurrence after breast-conserving surgery. Breast Cancer Res Treat 116:171–177. doi:10.1007/s10549-008-0187-y
Coopey S, Smith BL, Hanson S, Buckley J, Hughes KS, Gadd M, Specht MC (2011) The safety of multiple re-excisions after lumpectomy for breast cancer. Ann Surg Oncol 18:3797–3801. doi:10.1245/s10434-011-1802-4
Pleijhuis RG, Graafland M, de Vries J, Bart J, de Jong JS, van Dam GM (2009) Obtaining adequate surgical margins in breast-conserving therapy for patients with early-stage breast cancer: current modalities and future directions. Ann Surg Oncol 16:2717–2730. doi:10.1245/s10434-009-0609-z
Weber WP, Engelberger S, Viehl CT, Zanetti-Dallenbach R, Kuster S, Dirnhofer S, Wruk D, Oertli D, Marti WR (2008) Accuracy of frozen section analysis versus specimen radiography during breast-conserving surgery for nonpalpable lesions. World J Surg 32:2599–2606. doi:10.1007/s00268-008-9757-8
Riedl O, Fitzal F, Mader N, Dubsky P, Rudas M, Mittlboeck M, Gnant M, Jakesz R (2009) Intraoperative frozen section analysis for breast-conserving therapy in 1016 patients with breast cancer. Eur J Surg Oncol 35:264–270. doi:10.1016/j.ejso.2008.05.007
Blair SL, Thompson K, Rococco J, Malcarne V, Beitsch PD, Ollila DW (2009) Attaining negative margins in breast-conservation operations: is there a consensus among breast surgeons? J Am Coll Surg 209:608–613. doi:10.1016/j.jamcollsurg.2009.07.026
Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, Simunovic M (2009) The relationship between surgical factors and margin status after breast-conservation surgery for early stage breast cancer. Am J Surg 197:740–746. doi:10.1016/j.amjsurg.2008.03.007
Cho N, Kim SM, Park JS, Jang M, Kim SY, Chang JM, Moon WK (2011) Contralateral lesions detected by preoperative MRI in patients with recently diagnosed breast cancer: application of MR CAD in differentiation of benign and malignant lesions. Eur J Radiol. doi:10.1016/j.ejrad.2011.03.060
Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, Erban JK, Farrar WB, Forero A, Giodano SH, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Ljung B-M, Mankoff DA, Marcom PK, Mayer IA, McCormick B, Pierce LJ, Reed EC, Sachdev J, Smith ML, Somlo G, Ward JH, Wolff AC, Zellars R (2011) NCCN clinical practice guidelines in oncology: breast cancer version 2.2011. http://www.nccn.org. Accessed 11 Nov 2011
Hosmer D, Lemeshow S (2000) Applied logistic regression. Wiley, New York
Iasonos A, Schrag D, Raj GV, Panageas KS (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26:1364–1370. doi:10.1200/JCO.2007.12.9791
Park CC, Mitsumori M, Nixon A, Recht A, Connolly J, Gelman R, Silver B, Hetelekidis S, Abner A, Harris JR, Schnitt SJ (2000) Outcome at 8 years after breast-conserving surgery and radiation therapy for invasive breast cancer: influence of margin status and systemic therapy on local recurrence. J Clin Oncol 18:1668–1675
Groot G, Rees H, Pahwa P, Kanagaratnam S, Kinloch M (2011) Predicting local recurrence following breast-conserving therapy for early stage breast cancer: the significance of a narrow (≤2 mm) surgical resection margin. J Surg Oncol 103:212–216. doi:10.1002/jso.21826
Galimberti V, Maisonneuve P, Rotmensz N, Viale G, Sangalli C, Sargenti M, Brenelli F, Gentilini O, Intra M, Bassi F, Luini A, Zurrida S, Veronesi P, Colleoni M, Veronesi U (2011) Influence of margin status on outcomes in lobular carcinoma: experience of the European Institute of Oncology. Ann Surg 253:580–584. doi:10.1097/SLA.0b013e31820d9a81
Dunne C, Burke JP, Morrow M, Kell MR (2009) Effect of margin status on local recurrence after breast conservation and radiation therapy for ductal carcinoma in situ. J Clin Oncol 27:1615–1620. doi:10.1200/JCO.2008.17.5182
Rudloff U, Brogi E, Reiner AS, Goldberg JI, Brockway JP, Wynveen CA, McCormick B, Patil S, Van Zee KJ (2010) The influence of margin width and volume of disease near margin on benefit of radiation therapy for women with DCIS treated with breast-conserving therapy. Ann Surg 251:583–591. doi:10.1097/SLA.0b013e3181b5931e
Silverstein MJ, Lagios MD, Groshen S, Waisman JR, Lewinsky BS, Martino S, Gamagami P, Colburn WJ (1999) The influence of margin width on local control of ductal carcinoma in situ of the breast. N Engl J Med 340:1455–1461. doi:10.1056/NEJM199905133401902
Turnbull L, Brown S, Harvey I, Olivier C, Drew P, Napp V, Hanby A, Brown J (2010) Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet 375:563–571
Peters NH, van Esser S, van den Bosch MA, Storm RK, Plaisier PW, van Dalen T, Diepstraten SC, Weits T, Westenend PJ, Stapper G, Fernandez-Gallardo MA, Borel Rinkes IH, van Hillegersberg R, Mali WP, Peeters PH (2011) Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET—randomised controlled trial. Eur J Cancer 47:879–886. doi:10.1016/j.ejca.2010.11.035
Olson TP, Harter J, Munoz A, Mahvi DM, Breslin T (2007) Frozen section analysis for intraoperative margin assessment during breast-conserving surgery results in low rates of re-excision and local recurrence. Ann Surg Oncol 14:2953–2960. doi:10.1245/s10434-007-9437-1
Fukamachi K, Ishida T, Usami S, Takeda M, Watanabe M, Sasano H, Ohuchi N (2010) Total-circumference intraoperative frozen section analysis reduces margin-positive rate in breast-conservation surgery. Jpn J Clin Oncol 40:513–520. doi:10.1093/jjco/hyq006
Cendan JC, Coco D, Copeland EM 3rd (2005) Accuracy of intraoperative frozen-section analysis of breast cancer lumpectomy-bed margins. J Am Coll Surg 201:194–198
Tartter PI, Kaplan J, Bleiweiss I, Gajdos C, Kong A, Ahmed S, Zapetti D (2000) Lumpectomy margins, reexcision, and local recurrence of breast cancer. Am J Surg 179:81–85
Kurniawan ED, Wong MH, Windle I, Rose A, Mou A, Buchanan M, Collins JP, Miller JA, Gruen RL, Mann GB (2008) Predictors of surgical margin status in breast-conserving surgery within a breast screening program. Ann Surg Oncol 15:2542–2549. doi:10.1245/s10434-008-0054-4
Boyd NF, Jensen HM, Cooke G, Han HL, Lockwood GA, Miller AB (2000) Mammographic densities and the prevalence and incidence of histological types of benign breast disease. Reference Pathologists of the Canadian National Breast Screening Study. Eur J Cancer Prev 9:15–24
Turashvili G, McKinney S, Martin L, Gelmon KA, Watson P, Boyd N, Aparicio S (2009) Columnar cell lesions, mammographic density and breast cancer risk. Breast Cancer Res Treat 115:561–571. doi:10.1007/s10549-008-0099-x
Yaghjyan L, Colditz GA, Collins LC, Schnitt SJ, Rosner B, Vachon C, Tamimi RM (2011) Mammographic breast density and subsequent risk of breast cancer in postmenopausal women according to tumor characteristics. J Natl Cancer Inst 103:1179–1189
Hata T, Takahashi H, Watanabe K, Takahashi M, Taguchi K, Itoh T, Todo S (2004) Magnetic resonance imaging for preoperative evaluation of breast cancer: a comparative study with mammography and ultrasonography. J Am Coll Surg 198:190–197. doi:10.1016/j.jamcollsurg.2003.10.008
Schouten van der Velden AP, Schlooz-Vries MS, Boetes C, Wobbes T (2009) Magnetic resonance imaging of ductal carcinoma in situ: what is its clinical application? A review. Am J Surg 198:262–269. doi:10.1016/j.amjsurg.2009.01.010
Liberman L, Morris EA, Dershaw DD, Abramson AF, Tan LK (2003) Ductal enhancement on MR imaging of the breast. AJR Am J Roentgenol 181:519–525
Tresserra F, Feu J, Grases PJ, Navarro B, Alegret X, Fernandez-Cid A (1999) Assessment of breast cancer size: sonographic and pathologic correlation. J Clin Ultrasound 27:485–491
Satake H, Shimamoto K, Sawaki A, Niimi R, Ando Y, Ishiguchi T, Ishigaki T, Yamakawa K, Nagasaka T, Funahashi H (2000) Role of ultrasonography in the detection of intraductal spread of breast cancer: correlation with pathologic findings, mammography and MR imaging. Eur Radiol 10:1726–1732
Shin HC, Han W, Moon HG, Yom CK, Ahn SK, You JM, Kim JS, Chang JM, Cho N, Moon WK, Park IA, Noh DY (2012) Limited value and utility of breast MRI in patients undergoing breast-conserving cancer surgery. Ann Surg Oncol. doi:10.1245/s10434-012-2289-3
Dillon MF, Maguire AA, McDermott EW, Myers C, Hill AD, O’Doherty A, Quinn CM (2008) Needle core biopsy characteristics identify patients at risk of compromised margins in breast conservation surgery. Mod Pathol 21:39–45. doi:10.1038/modpathol.3800975
Saadai P, Moezzi M, Menes T (2011) Preoperative and intraoperative predictors of positive margins after breast-conserving surgery: a retrospective review. Breast Cancer 18:221–225. doi:10.1007/s12282-011-0262-9
Chagpar AB, Martin RC 2nd, Hagendoorn LJ, Chao C, McMasters KM (2004) Lumpectomy margins are affected by tumor size and histologic subtype but not by biopsy technique. Am J Surg 188:399–402. doi:10.1016/j.amjsurg.2004.06.020
Acknowledgments
We thank the Medical Research Collaborating Center (MRCC) of Seoul National University Hospital for the excellent assistance in statistical analysis. This work was supported by National Research Foundation of Korea (NRF) Grant funded by the Korean Government (A110961) and by a grant of the Korea Health technology R&D Project, Ministry of Health & Welfare, Republic of Korea (2012-0000994).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, HC., Han, W., Moon, HG. et al. Nomogram for predicting positive resection margins after breast-conserving surgery. Breast Cancer Res Treat 134, 1115–1123 (2012). https://doi.org/10.1007/s10549-012-2124-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2124-3