Abstract
Background
Although an aggressive surgical approach to perihilar cholangiocarcinoma (PHC) has improved survival, a prognosis of advanced PHC remains unsatisfactory. The overexpression of mesenchymal–epithelial transition factor (MET) and recepteur d’origine nantais (RON) has been shown to be associated with poor prognosis in some types of cancer.
Methods
One hundred sixty-nine patients who underwent histologically curative resection for PHC were subjected to immunohistochemical analysis for MET and RON. The association between a positive expression of MET or RON and clinicopathologic features as well as the patients’ prognosis were analyzed.
Results
There were 27 patients (16 %) who had a positive expression for both MET and RON. Although clinicopathologic features in the either MET- or RON-negative group were not significantly different compared to the both MET- and RON-positive group, the prognosis tended to be worse in the patients with both MET and RON positivity. When the analysis was limited to patients with advanced-stage disease (stage III and IVa), a multivariate analysis revealed that both MET and RON positivity and lymph node metastasis were identified as independent poor prognostic factors.
Conclusions
The overall survival rate for patients with both MET and RON positivity was worse than that with either MET or RON negativity in patients with advanced PHC. The poor prognosis in these patients was not associated with unfavorable clinicopathologic features. The examination of MET and RON expression in PHC may enable a tailored method for patient classification that could not otherwise be achieved using the conventional pathologic classification system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Perihilar cholangiocarcinoma (PHC) is an intractable disease because of the anatomic complexity of the tumor location and the capacity to invade adjacent tissues such as portal veins, hepatic arteries, and liver parenchyma.1,2 Although an aggressive surgical approach to PHC has improved survival, a prognosis of advanced PHC remains poor even after curative resection.3,4 To improve the prognosis of PHC, a tailored patient management including the estimation of the malignant potential of the tumor and the establishment of effective molecular target therapy are necessary.
In patients with PHC, previous studies have shown that histologic grade, microscopic lymphatic or venous invasion, microscopic perineural invasion, lymph node metastasis, and curability (R status) are significantly correlated with poor prognosis after resection.4,5 However, even with favorable pathologic findings, some patients experience disease recurrence and die in the early postoperative period.
Mesenchymal–epithelial transition factor (MET) and recepteur d’origine nantais (RON) proto-oncogenes encode the cell surface receptors for hepatocyte growth factor (HGF) and hepatocyte growth factor—like protein (HLP), respectively.6–11 MET and RON have been demonstrated to induce mitogenesis and morphogenesis in epithelial cells and have been associated with tissue regeneration and development.12,13 The activation of MET by HGF and RON by HLP in carcinoma cells can initiate many signaling pathways that are implicated in tumor progression and metastasis.14–16 The overexpression of MET or RON in some carcinomas has been demonstrated to be associated with poor prognosis.17–22 Furthermore, cooperative signaling by MET and RON may result in more aggressive phenotypes.20 However, the coexpression profile of MET and RON in PHC specimens has not been studied. It is also unknown whether the expression of MET or RON has any association with the malignant potential of PHC.
The aim of this study was to determine the expression profile of MET and RON in curatively resected surgical specimens of PHC. The strength of MET or RON expression and its association with patient prognosis were also analyzed.
Methods
Patients
From 2001 to 2007, a total of 248 patients with PHC underwent resection at the First Department of Surgery, Nagoya University Hospital. The resected specimens were histologically examined and approved as having carcinoma of the perihilar bile duct. Patients with distant metastasis (pM1) and/or noncurative resection (R1 or 2) were excluded (n = 79), and 169 patients (including 55 patients with stage I or II disease and 114 patients with stage III or IVa disease according to International Union Against Cancer [UICC], 7th edition) who had undergone histologically curative resection were finally analyzed. Clinical and pathologic data were obtained from prospectively collected data. Figure 1 provides a low diagram of patients included and excluded from the study.
Chemicals
CONFIRM anti-total c-MET (SP44) rabbit monoclonal primary antibody (rabbit monoclonal, Ventana Medical Systems Inc., Tucson, AZ) and anti-RON antibody (EP1132Y; rabbit monoclonal; Abcam Inc., Cambridge, UK) were purchased.23 , 24
Immunohistochemistry for MET and RON
Immunohistochemistry was performed on 169 formalin-fixed, paraffin-embedded tissue Sections. (4 µm thick). Staining for MET and RON were performed using a Discovery XT automated slide preparation system (Ventana Medical Systems Inc.). Before staining, the paraffin-embedded sections were blocked with 1 % nonfat milk. The staining procedure was performed according to the manufacturer’s instructions (Ventana Medical Systems Inc.). For MET staining, the slides were incubated with the MET antibody with an amplification kit (Ventana Medical Systems Inc.) for 60 min at room temperature. For RON staining, the slides were incubated with 1:100 of the RON antibody for 12 h at room temperature. Primary antibody was detected using the DAB Map Detection Kit (Ventana Medical Systems Inc.). Universal secondary antibody (Ventana Medical Systems Inc.) was applied for 48 min at room temperature. The slides were counterstained with hematoxylin II (Ventana Medical Systems Inc.) for 4 min.
The scoring system used in this study basically followed the method used in a previously published study that demonstrated the expression of MET in cholangiocarcinoma specimens.17 Briefly, the immunoexpressions of MET and RON were categorized into three groups according to their dyeing density: no expression (−; complete absence of membrane staining), moderate expression (+; faint and partial membrane staining in at least 30 % of cancer cells), or strong expression (++; strong and complete staining in at least 30 % of cancer cells). The representative images of MET and RON expression are depicted in Fig. 2. The tissue sections were evaluated by two observers without knowledge of the clinical data. Two observers had a discussion to make a final decision when the grading of positivity was not matched among them. In this study, only the cases with strong expression either for MET or RON were considered to have positive expression because there was more discrepant grading in the group of no or moderate expression.
Statistical Analysis
Statistical analysis was performed by Student’s t test, the χ 2 test, or Fisher’s exact probability test, as appropriate. Patient survival was determined from the time of surgery to the time of death or most recent follow-up. The median follow-up periods were 1,405 days (range 15–4,845 days). Nineteen (11.2 %) of 169 PHC patients died from other causes. Four (2.4 %) the 169 PHC patients died from postoperative complications. Patients who died from other causes during follow-up with no evidence of recurrence were treated as censored cases. Postoperative survival was calculated by means of the Kaplan–Meier method, and differences in the survival curves were compared with the log-rank test. The Cox proportional hazard model was used for multivariate analysis. Analyses were performed by SPSS software, version 11 (IBM, Armonk, NY). P ≤ 0.050 was considered statistically significant.
Results
Immunohistochemical Analysis of MET and RON in PHC Specimens
MET and RON staining was localized in both the cell membrane and cytoplasm of PHC cells (Fig. 2). Positive staining for MET was demonstrated in 56 (33.1 %) of the 169 cases, whereas that for RON was demonstrated in 66 (39.1 %) of the 169 cases (Table 1).
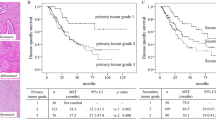
Coexpression of MET and RON and Clinicopathologic Factors
There were 27 patients who revealed a positive expression for both MET and RON. The average age of the patients in the both MET- and RON-positive group was significantly higher than that in the either MET- or RON-negative group (“other” group) (Table 2). Invasion to the portal vein was more frequently observed in the “other” group (55 of 142, 38.7 %) than the both MET- and RON-positive group (2 of 27, 7.4 %) (P = 0.002) (Table 2). Invasion to other organ was also more frequently observed in the “other” group (124 of 142, 87.3 %) than the both MET- and RON-positive group (18 of 27, 66.7 %) (P = 0.018). Nevertheless, the overall survival rate tended to be lower in the both MET- and RON-positive group than the “other” group, although it did not reach to a significant difference (P = 0.234) (Fig. 3a). The 5-year survival rate in the both MET- and RON-positive group was 37.0 %, whereas that in the “other” group was 47.9 %.
Subclass Analysis for Stage III and IVa Disease
In the subsequent analysis, we performed a subclass analysis in patients with stage IIIa, IIIb, and IVa PHC according to the UICC, 7th edition (n = 114). In the univariate analysis, 3 of 14 possible clinicopathologic prognostic factors, such as microscopic venous invasion, lymph node metastasis (pN), and both MET and RON positivity, were significantly associated with poor prognosis (Table 3). A multivariate analysis using the three significant factors identified via univariate analysis revealed that both MET and RON positivity and lymph node metastasis were identified as independent prognostic factors (Table 3). The overall survival rate was significantly lower in the both MET- and RON-positive group than the “other” group (P = 0.021) (Fig. 3b). The 5-year survival rate in the both MET- and RON-positive group was 16.7 %, whereas that in the “other” group was 39.8 %. In contrast to the results in patients with advanced stage PHC, there was no clinical impact of MET and RON expression in patients with low-stage PHC (stage I or II) (data not shown).
Discussion
In this study, the expression levels of MET and RON, two homologous receptor tyrosine kinases that are associated with cancer progression, were examined in a highly uniform patient population: curatively resected cases of PHC.25 After immunohistochemical analysis, the rates for the strong expression of MET and RON were 33.1 and 39.1 %, respectively. Although clinicopathologic features in the “other” group (either MET- or RON-negative group) were not significantly different or even worse (more portal vein and other organ invasions) compared to the both MET- and RON-positive group, the prognosis tended to be worse in the patients with both MET and RON positivity than in the patients with either MET or RON negativity. When the analysis was limited to patients with advanced-stage disease (stage III and IVa), a multivariate analysis revealed that both MET and RON positivity and lymph node metastasis were identified as independent poor prognostic factors (Table 3). The hazard ratio for MET and RON positivity (1.81) was close to that for pN1 (2.04), which is known as the strongest risk factor for poor prognosis in PHC (Table 3). These results indicated that the expression of MET and RON represents the malignant potential of PHC, which cannot be predicted using conventional pathologic findings. Moreover, the results in this study implied a therapeutic potential for combined MET and RON inhibitors, which are available in the preclinical setting as an adjuvant molecular targeting chemotherapy for advanced PHC.26–28
Miyamoto et al. examined the expression of MET and demonstrated its prognostic impact in patients with cholangiocarcinoma.17 In their study, the positive expression of MET was significantly correlated with histopathologic classification in extrahepatic cholangiocarcinoma. However, this correlation was not applied to the cases of intrahepatic cholangiocarcinoma. Additionally, in patients with intrahepatic cholangiocarcinoma, the positive expression of MET was significantly associated with poor prognosis, whereas it was not associated with poor prognosis in patients with extrahepatic cholangiocarcinoma.17 In the current study, there was no correlation between MET expression and histopathologic classification (data not shown). The previous study included patients who underwent noncurative resection. It also included patients in whom the tumor varied in location (e.g., patients with intrahepatic and extrahepatic cholangiocarcinoma). These heterogeneities in the patient population may partly explain the divergence from the results of the current study.
MET and RON are members of the same proto-oncogene family and were reported to form a noncovalent complex on the cell surface and to cooperate in intracellular signaling. The concomitant activation of these two receptors could lead to a synergistic effect and may favor, in pathologic conditions, the invasive-metastatic phenotype.29 The activation of MET and RON receptors promotes the progression, invasion, and metastasis of malignant cells both in in vivo and in vitro experiments.16 , 30,31 Therefore, it is important to investigate the coexpression of MET and RON in cancer specimens. The overexpression of MET and RON and their association with a poorer prognosis have been confirmed in urothelial carcinoma, bladder cancer, hepatocellular carcinoma, breast cancer, colorectal cancer, and ovarian cancer.32–37 However, the coexpression of MET and RON has never been investigated in cholangiocarcinoma. As is consistent with other types of solid cancer, the coexpression of MET and RON may be associated with a poor prognosis in advanced PHC patients. In our previous report reviewing 34 years of experience with 574 consecutive resections for PHC, a multivariate analysis revealed that the presence of lymph node metastasis was the strongest prognostic indicator.4 In this study, in the subclass analysis for stage III and IVa PHC, the rate of lymph node metastasis in the patients with both MET and RON positivity was not higher than that in other patients (50 vs. 59.4 %). Nevertheless, the overall prognosis was significantly worse in the patients with both MET and RON positivity. These results indicated that the examination of MET and RON expression may enable a tailored biological classification of PHC patients who cannot otherwise be delineated using conventional pathologic methods. Moreover, preoperative analysis for MET and RON expression in the biopsy samples may support clinical decision making (i.e., candidate for neoadjuvant therapy), because patients with positive MET and RON expression tend to have a poor prognosis even after the curative resection.
Dual inhibitors of MET and RON have been developed and investigated in multiple in vitro and in vivo models.26–28,38 However, only a few clinical trials using oral multikinase inhibitor targeting MET, RON, and other receptors are currently ongoing for papillary renal cell carcinoma and unresectable solid tumors.39,40 On the basis of the observations in this study, dual inhibitors for MET and RON may have a promising therapeutic potential in PHC, especially in patients with poor prognosis despite curative resection. To promote translational research for molecular targeting therapy against MET and RON, further mechanistic studies that precisely elucidate the therapeutic value of dual inhibitors for biologically malignant cholangiocarcinoma are required.
The major limitation of this study was the small sample size (n = 169). The present study also revealed no clinical importance of MET and RON expression in patients with low-stage PHC (stage I or II). We suspect that the major reasons for insignificant findings may be related to the small number of patients (n = 55) and highly favorable postoperative prognosis in these patients (80.5 % 5-year survival rate).41,42 Nevertheless, further large-scale study is necessary to determine whether the positive expression for both MET and RON has a negative prognostic impact even at low-stage PHC. Additionally, the mechanistic reason behind the poor prognosis of patients with the coexpression of MET and RON remains unknown. Among those patients, the recurrence pattern was variable for local recurrence, liver metastasis, peritoneal dissemination, and lymph node metastases (data not shown). There was no clear biological property that explained poor prognosis in the patients with coexpression of MET and RON. It is also unclear whether signaling pathways that are associated with MET and RON are intensively activated by HGF and HLP in cholangiocarcinoma. Further clinical data and mechanistic investigations are necessary to clarify these issues.
In conclusion, this study demonstrated that the overall survival rate with both MET and RON positivity was worse than that with either MET or RON negativity in patients with advanced PHC. The poor prognosis in these patients was not associated with unfavorable clinicopathologic features. The examination of MET and RON expression in PHC may enable a tailored patient classification that cannot otherwise be achieved using the conventional pathologic classification. Moreover, the results in this study implied promising therapeutic potential for dual inhibitors of MET and RON for biologically malignant PHC.
References
Sarmiento JM, Nagorney DM. Hepatic resection in the treatment of perihilar cholangiocarcinoma. Surg Oncol Clin N Am. 2002;11:893–908, viii–ix.
Young AL, Igami T, Senda Y, Adair R, Farid S, Toogood GJ, et al. Evolution of the surgical management of perihilar cholangiocarcinoma in a Western centre demonstrates improved survival with endoscopic biliary drainage and reduced use of blood transfusion. HPB (Oxford). 2011;13:483–93.
Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, et al. Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Sci. 2010;17:449–54.
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 2013;258:129–40.
Aoba T, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. Assessment of nodal status for perihilar cholangiocarcinoma: location, number, or ratio of involved nodes. Ann Surg. 2013;257:718–25.
Bottaro DP, Rubin JS, Faletto DL, Chan AM, Kmiecik TE, Vande Woude GF, et al. Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product. Science. 1991;251:802–4.
Naldini L, Vigna E, Narsimhan RP, Gaudino G, Zarnegar R, Michalopoulos GK, et al. Hepatocyte growth factor (HGF) stimulates the tyrosine kinase activity of the receptor encoded by the proto-oncogene c-MET. Oncogene. 1991;6:501–4.
Wang MH, Ronsin C, Gesnel MC, Coupey L, Skeel A, Leonard EJ, et al. Identification of the ron gene product as the receptor for the human macrophage stimulating protein. Science. 1994;266:117–9.
Wang MH, Iwama A, Skeel A, Suda T, Leonard EJ. The murine stk gene product, a transmembrane protein tyrosine kinase, is a receptor for macrophage-stimulating protein. Proc Natl Acad Sci USA. 1995;92:3933–7.
Degen SJ, Stuart LA, Han S, Jamison CS. Characterization of the mouse cDNA and gene coding for a hepatocyte growth factor–like protein: expression during development. Biochemistry. 1991;30:9781–91.
Han S, Stuart LA, Degen SJ. Characterization of the DNF15S2 locus on human chromosome 3: identification of a gene coding for four kringle domains with homology to hepatocyte growth factor. Biochemistry. 1991;30:9768–80.
Zarnegar R, Michalopoulos GK. The many faces of hepatocyte growth factor: from hepatopoiesis to hematopoiesis. J Cell Biol. 1995;129:1177–80.
Matsumoto K, Nakamura T. Emerging multipotent aspects of hepatocyte growth factor. J Biochem. 1996;119:591–600.
Christensen JG, Schreck R, Burrows J, Kuruganti P, Chan E, Le P, et al. A selective small molecule inhibitor of c-Met kinase inhibits c-Met-dependent phenotypes in vitro and exhibits cytoreductive antitumor activity in vivo. Cancer Res. 2003;63:7345–55.
Zhang YW, Su Y, Volpert OV, Vande Woude GF. Hepatocyte growth factor/scatter factor mediates angiogenesis through positive VEGF and negative thrombospondin 1 regulation. Proc Natl Acad Sci USA. 2003;100:12718–23.
Camp ER, Liu W, Fan F, Yang A, Somcio R, Ellis LM. RON, a tyrosine kinase receptor involved in tumor progression and metastasis. Ann Surg Oncol. 2005;12:273–81.
Miyamoto M, Ojima H, Iwasaki M, Shimizu H, Kokubu A, Hiraoka N, et al. Prognostic significance of overexpression of c-Met oncoprotein in cholangiocarcinoma. Br J Cancer. 2011;105:131–8.
Sotoudeh K, Hashemi F, Madjd Z, Sadeghipour A, Molanaei S, Kalantary E. The clinicopathologic association of c-MET overexpression in Iranian gastric carcinomas; an immunohistochemical study of tissue microarrays. Diagn Pathol. 2012;7:57.
Garcia S, Dales JP, Jacquemier J, Charafe-Jauffret E, Birnbaum D, Andrac-Meyer L, et al. c-Met overexpression in inflammatory breast carcinomas: automated quantification on tissue microarrays. Br J Cancer. 2007;96:329–35.
Catenacci DV, Cervantes G, Yala S, Nelson EA, El-Hashani E, Kanteti R, et al. RON (MST1R) is a novel prognostic marker and therapeutic target for gastroesophageal adenocarcinoma. Cancer Biol Ther. 2011;12:9–46.
Gray JK, Paluch AM, Stuart WD, Waltz SE. Ron receptor overexpression in the murine prostate induces prostate intraepithelial neoplasia. Cancer Lett. 2012;314:92–101.
Kim SA, Yoon TM, Lee DH, Park YL, Lee KH, Lim SC, et al. RON (recepteur d’origine nantais) expression and its association with tumor progression in laryngeal squamous cell carcinoma. Auris Nasus Larynx. 2014;41:201–6.
Ha SY, Lee J, Kang SY, Do IG, Ahn S, Park JO, et al. MET overexpression assessed by new interpretation method predicts gene amplification and poor survival in advanced gastric carcinomas. Mod Pathol. 2013;26:1632–41.
Wang Q, Quan H, Zhao J, Xie C, Wang L, Lou L. RON confers lapatinib resistance in HER2-positive breast cancer cells. Cancer Lett. 2013;340:43–50.
Dussault I, Bellon SF. From concept to reality: the long road to c-Met and RON receptor tyrosine kinase inhibitors for the treatment of cancer. Anticancer Agents Med Chem. 2009;9:221–9.
Steinig AG, Li AH, Wang J, Chen X, Dong H, Ferraro C, et al. Novel 6-aminofuro[3,2-c]pyridines as potent, orally efficacious inhibitors of cMET and RON kinases. Bioorg Med Chem Lett. 2013;23:4381–7.
Kawada I, Hasina R, Arif Q, Mueller J, Smithberger E, Husain AN, et al. Dramatic antitumor effects of the dual MET/RON small-molecule inhibitor LY2801653 in non-small cell lung cancer. Cancer Res. 2014;74:884–95.
Yan SB, Peek VL, Ajamie R, Buchanan SG, Graff JR, Heidler SA, et al. LY2801653 is an orally bioavailable multi-kinase inhibitor with potent activity against MET, MST1R, and other oncoproteins, and displays anti-tumor activities in mouse xenograft models. Invest New Drugs. 2013;31:833–44.
Follenzi A, Bakovic S, Gual P, Stella MC, Longati P, Comoglio PM. Cross-talk between the proto-oncogenes Met and Ron. Oncogene. 2000;19:3041–9.
Leelawat K, Leelawat S, Tepaksorn P, Rattanasinganchan P, Leungchaweng A, Tohtong R, et al. Involvement of c-Met/hepatocyte growth factor pathway in cholangiocarcinoma cell invasion and its therapeutic inhibition with small interfering RNA specific for c-Met. J Surg Res. 2006;136:78–84.
Herynk MH, Radinsky R. The coordinated functional expression of epidermal growth factor receptor and c-Met in colorectal carcinoma metastasis. In Vivo. 2000;14:587–96.
Comperat E, Roupret M, Chartier-Kastler E, Bitker MO, Richard F, Camparo P, et al. Prognostic value of MET, RON and histoprognostic factors for urothelial carcinoma in the upper urinary tract. J Urol. 2008;179:868–72.
Cheng HL, Liu HS, Lin YJ, Chen HH, Hsu PY, Chang TY, et al. Co-expression of RON and MET is a prognostic indicator for patients with transitional-cell carcinoma of the bladder. Br J Cancer. 2005;92:1906–14.
Chen Q, Seol DW, Carr B, Zarnegar R. Co-expression and regulation of Met and Ron proto-oncogenes in human hepatocellular carcinoma tissues and cell lines. Hepatology. 1997;26:59–66.
Lee WY, Chen HH, Chow NH, Su WC, Lin PW, Guo HR. Prognostic significance of co-expression of RON and MET receptors in node-negative breast cancer patients. Clin Cancer Res. 2005;11:2222–8.
Lee CT, Chow NH, Su PF, Lin SC, Lin PC, Lee JC. The prognostic significance of RON and MET receptor coexpression in patients with colorectal cancer. Dis Colon Rectum. 2008;51:1268–74.
Maggiora P, Lorenzato A, Fracchioli S, Costa B, Castagnaro M, Arisio R, et al. The RON and MET oncogenes are co-expressed in human ovarian carcinomas and cooperate in activating invasiveness. Exp Cell Res. 2003;288:382–9.
Zeng JY, Sharma S, Zhou YQ, Yao HP, Hu X, Zhang R, et al. Synergistic activities of MET/RON inhibitor BMS-777607 and mTOR inhibitor AZD8055 to polyploid cells derived from pancreatic cancer and cancer stem cells. Mol Cancer Ther. 2014;13:37–48.
Choueiri TK, Vaishampayan U, Rosenberg JE, Logan TF, Harzstark AL, Bukowski RM, et al. Phase II and biomarker study of the dual MET/VEGFR2 inhibitor foretinib in patients with papillary renal cell carcinoma. J Clin Oncol. 2013;31:181–6.
Shapiro GI, McCallum S, Adams LM, Sherman L, Weller S, Swann S, et al. A phase 1 dose-escalation study of the safety and pharmacokinetics of once-daily oral foretinib, a multi-kinase inhibitor, in patients with solid tumors. Invest New Drugs. 2013;31:742–50.
Robles R, Figueras J, Turrion VS, Margarit C, Moya A, Varo E, et al. Spanish experience in liver transplantation for hilar and peripheral cholangiocarcinoma. Ann Surg. 2004;239:265–71.
Juntermanns B, Sotiropoulos GC, Radunz S, Reis H, Heuer M, Baba HA, et al. Comparison of the sixth and the seventh editions of the UICC classification for perihilar cholangiocarcinoma. Ann Surg Oncol. 2013;20:277–84.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watanabe, H., Yokoyama, Y., Kokuryo, T. et al. Prognostic Value of Hepatocyte Growth Factor Receptor Expression in Patients with Perihilar Cholangiocarcinoma. Ann Surg Oncol 22, 2235–2242 (2015). https://doi.org/10.1245/s10434-014-4170-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4170-z