Abstract
Background
Although treatment strategies for intrahepatic cholangiocarcinoma (ICC) are shifting towards multidisciplinary approaches, preoperative radiographic methods for identifying patients requiring further therapy are unclear. This study was designed to establish a prognostic grading system using preoperatively available objective biomarkers.
Methods
A novel preoperative prognostic grading system for predicting survival after surgery for ICC was developed from multivariate analysis of 134 ICC patients who underwent surgery between 1996 and 2015 using preoperatively available biomarkers.
Results
The median overall survival time and 3- and 5 year survival rates were 33.3 months, 48, and 38%, respectively. Of the preoperative biomarkers, the neutrophil-to-lymphocyte ratio (≥5), and C-reactive protein (≥5 mg/L) and carbohydrate antigen 19-9 (≥500 IU/mL) levels were independently associated with poor overall survival. Based on the presence of these factors, the preoperative prognostic grades were defined as follows: grade 1, no factor; grade 2, one factor; and grade 3, two or three factors. The median overall survival time and 3- and 5 year survival rates of patients with grade 1 (70.3 months, 66, and 53%, respectively) were higher than those of patients with grade 2 (23.4 months, 37, and 30%, respectively; P = 0.004) and grade 3 (8.8 months, 5% both; 2 vs. 3, P < 0.001). Multivariable analysis revealed that the preoperative prognostic grading system independently predicted survival after adjusting for known prognostic factors.
Conclusions
A novel biomarker-based preoperative prognostic grading system for ICC significantly stratifies survival after surgery and may identify patients requiring further treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intrahepatic cholangiocarcinoma (ICC), which originates from the secondary or more peripheral branches of the biliary tree, is the second most common primary liver cancer after hepatocellular carcinoma (HCC).1,2 Surgery has been considered a potentially curative treatment for ICC. However, the reported 5 year overall survival (OS; 15–40%) and postsurgical recurrence rates (50–60%) for ICC are unsatisfactory.3–9 Therefore, treatment strategies for advanced ICC are shifting towards multidisciplinary approaches, including neoadjuvant and adjuvant therapies.10,11 However, methods to identify patients who require further therapy are unclear.
To date, several large-sized studies have identified predictive factors for a poor prognosis after surgery. Of these, two prognostic nomograms enabled prediction of postsurgical survival in ICC patients and might identify further treatment needs.12,13 However, these nomograms require histological data, which are only available after surgery. Furthermore, the accuracy of preoperative imaging modalities detecting these tumor characteristics, such as lymph node metastasis or intrahepatic nodules, remains unsatisfactory.14,15 Therefore, there is currently no predictive model for postsurgical ICC outcomes that relies solely on factors available preoperatively. In the future, more objective assessment methods are needed for establishing the appropriate surgical strategy in ICC.
Among representative objective factors available preoperatively, there has been accumulating evidence that preoperative serum biomarkers can predict the survival of ICC patients after surgery.16 Of these, tumor markers that reflect tumor progression, such as carbohydrate antigen 19-9 (CA19-9) and carcinoembryonic antigen (CEA), have been reported to be independently associated with ICC prognosis.5,8,12 The systemic inflammatory response (SIR), which is considered to reflect host inflammatory and immune responses and plays a significant role in the determination of prognosis in various malignancies, has garnered interest as another preoperative predictive biomarker for hepatobiliary malignancies.17–24 In particular, elevated preoperative C-reactive protein (CRP) levels and neutrophil-to-lymphocyte (NLR) and platelet-to-lymphocyte (PLR) ratios have been reported to be associated with relatively poor survival. Given these previously published data, we hypothesized that a preoperative prognostic grading system incorporating SIR and tumor markers could help to predict postsurgical prognosis in ICC. Compared with other numerous prognostic factors or developing biomarkers, SIR and tumor markers are simple, inexpensive, and widely available from preoperative blood tests. In the present study, we sought to establish a novel biomarker-based preoperative prognostic grading system to identify patients who could potentially benefit from surgery, as well as those who would require further treatment.
Methods
Patients
A total of 141 ICC patients (excluding combined ICC–HCC patients) underwent hepatectomy with curative intent at Kyoto University Hospital, Kyoto, Japan, between 1996 and 2015. A total of seven patients who received preoperative therapy [neoadjuvant chemotherapy (N = 2) or unintended conversion therapy (N = 5) were excluded, because we could not comment on the statistical significance of treatment effects due to the small number of cases. Finally, 134 patients were enrolled in this retrospective study. The clinicopathological data, including sex, age, hepatitis virus markers, Child-Pugh classification, primary tumor characteristics, treatment-related variables, and survival data of these patients were retrieved from a prospectively maintained institutional database. Primary tumor characteristics and resection margins were ascertained based on final pathological findings. Tumor stages were assessed according to the American Joint Committee on Cancer (AJCC) classification system, 7th edition.25 Operative mortality was defined as death within 30 days of surgery or during the same hospitalization period; morbidity was evaluated according to the Clavien–Dindo classification system.26 The follow-up protocol and recurrence criteria were the same as those reported previously.27,28 The follow-up data were updated in April 2016. The study protocol was approved by the ethical committee of the Graduate School of Medicine, Kyoto University. Written, informed consent was obtained from all study participants.
Preoperative Biomarkers
Five preoperatively available biomarkers, including the NLR, PLR, and serum CRP, CEA, and CA19-9 levels, were analyzed preoperatively at the time of admission. In cases of tumor invasion of the hepatic hilum, complete blood count and serum CRP levels were evaluated after biliary drainage and confirmation of no sign of infection.
Surgical Procedures and Treatment Strategy
Patients in whom macroscopically curative resection was deemed possible were indicated for surgical resection as previously reported.27,28 The type of hepatectomy, which was defined according to the hepatic anatomy and resection terminology proposed by the International Hepato-Pancreato-Biliary Association in 2000, was determined according to the tumor diameter, location, presence or absence of cirrhosis, and estimated volume of the future remnant liver.29 Routine lymphadenectomy was performed around the hepatoduodenal ligament and retropancreatic area with or without para-aortic lymph nodes, except in patients with poor conditions and those diagnosed preoperatively with HCC or other diseases.27 Postsurgical adjuvant chemotherapy was administered using gemcitabine hydrochloride and tegafur–gimeracil–oteracil potassium (S-1), both of which were authorized for use in Japanese patients with biliary tract cancer in 2006 and 2007, respectively, for stage II–IV tumors classified according to the AJCC classification system.27,28
Statistical Analysis
For surgically treated patients, OS was calculated from the day of surgery to the date of death or end of the follow-up period, whereas disease-free survival (DFS) was calculated using the date of death or recurrence as the time of the terminal event according to the Kaplan–Meier method. Continuous variables, expressed as median values (range), were compared using the Mann–Whitney U test. Categorical variables were compared using χ 2 tests. Cutoff values for preoperative prognostic biomarkers that were continuous variables were determined based on the maximum significant OS differences in a Cox hazard model (i.e., the minimum P value approach). Independent prognostic factors for survival were identified using multivariate Cox proportional hazards models; variables identified as significant (P < 0.05) in the univariate analysis were entered into a multivariate model. The performance of our preoperative prognostic grading system was assessed based on homogeneity (likelihood ratio χ 2 test related to the Cox regression model) and discriminatory ability [corrected Akaike information criteria (AICc)]. The likelihood ratio test also can estimate the monotonicity of gradients. Generally, more accurate models exhibit higher likelihood ratio χ 2 values and lower AICc values than inaccurate models. Differences were considered significant at P < 0.05. Statistical analyses were performed using JMP ver. 12.1 software (SAS Institute, Cary, NC).
Results
Patient Characteristics
The demographic details of the 134 surgically treated patients are presented in Table 1. Of these, 10 patients (7%) showed postoperative para-aortic lymph node metastasis, defined as distant metastasis under the AJCC classification system. The median OS time was 33.3 months, with 3- and 5 year OS rates of 48 and 38%, respectively. The median DFS time was 14.1 months, with 3- and 5 year DFS rates of 28 and 23%, respectively.
Determining the Optimal Cutoff Value of Preoperatively Available Biomarkers and Independent Predictors
After adjusting the cutoff values by the minimum P value approach, the optimal cutoff values were determined to be CA19-9, 500 IU/mL; CEA, 5 ng/mL; NLR, 5; PLR, 120; and CRP, 5 mg/L, respectively. Furthermore, we conducted multivariate analysis to assess which biomarkers could independently predict OS after surgery among these five potential predictors. The results of the multivariate analysis identified preoperative serum CA19-9 levels ≥500 IU/mL, preoperative serum CRP levels ≥5 mg/L, and preoperative NLR ≥ 5 as independently associated with poor OS after surgery (Table 2).
Establishment and Prognostic Impact of the Novel Biomarker-Based Preoperative Prognostic Grading System
Based on the three preoperative prognostic factors identified in the multivariate analysis, the preoperative prognostic grades were defined as follows: grade 1, none of these factors; grade 2, the presence of only one factor, and grade 3, the presence of two or three factors (Supplementary Table 1). The differences in clinicopathological features among patients with different preoperative prognostic grades are shown in Table 3. Patients with grade 3 exhibited significantly higher incidences of node-positive disease (P = 0.001), vascular invasion (P = 0.021), and larger tumor (P = 0.009) than patients with grade 1, and a higher incidence of early recurrence within 6 months than patients with grade 1 and 2 (P < 0.001 and P = 0.011). Additionally, patients with grade 2 exhibited a higher incidence of vascular invasion (P = 0.012) and early recurrence within 6 months (P = 0.003) than those with grade 1.
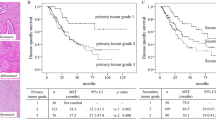
Figure 1 shows a stratification of patient survival according to the preoperative prognostic grades. The median OS time and 3- and 5 year OS rates of patients with preoperative prognostic grade 1, 2, and 3 were 70.3, 23.4, and 8.8 months; 66, 37, and 5%; and 53, 30, and 5%, respectively (Fig. 1a). Stratifications of OS according to the preoperative prognostic grading system were significant (1 vs. 2, P = 0.004; 2 vs. 3, P < 0.001). Similar results were obtained for DFS in patients undergoing hepatectic resection, with the median DFS time and 3- and 5 year DFS rates of patients with grade 1, 2 and 3 being 26.9, 10.2, and 3.4 months; 44, 10, and 4%; and 36, 10, and 4%, respectively (Fig. 1b). Stratifications of DFS according to the preoperative prognostic grading system also were significant (1 vs. 2, P < 0.001; 2 vs. 3, P = 0.004).
Overall (a) and disease-free (b) survival stratified according to the preoperative prognostic grades are shown. There were significant differences in overall (1 vs. 2, P = 0.004; 2 vs. 3, P < 0.001; log-rank test) and disease-free (1 vs. 2, P < 0.001; 2 vs. 3, P = 0.004) survival among patients with different preoperative prognostic grades
Recent studies, including our previous report, found that adjuvant chemotherapy significantly improved survival after surgery for ICC patients, especially those with lymph node metastasis.11,27 Therefore, to assess the independent prognostic impact of the preoperative prognostic grading system, multivariate analysis, adjusting for known clinicopathological factors and treatment variables, was conducted. The multivariate analysis revealed that the nodal status, resection margin, number of tumors, administration of adjuvant chemotherapy, and preoperative prognostic grading system all independently predicted OS (Supplementary Table 2). This finding suggests that the preoperative prognostic grading system independently predicted OS, regardless of tumor progression or treatment.
Efficacy Comparison of the Proposed Preoperative Prognostic Grading System and AJCC Staging System
Finally, to assess the efficacy of the preoperative prognostic grading system, we compared its prognostic power with those of the conventional AJCC staging systems (survival curves are shown in Supplementary Fig. 1). The preoperative prognostic grading system exhibited higher accuracy for survival prediction in ICC patients compared with conventional AJCC staging systems (likelihood ratio χ 2 values, 36.9 vs. 26.4; AICc value, 725.4 vs. 738.0, respectively; Table 4).
Discussion
To establish appropriate surgical strategies for ICC in the future, it is critical to identify patients accurately who are expected to have longer survival durations as well as those with high risks of recurrence. In the present study, we report our experience with ICC at a high-volume Japanese institution and demonstrate that the combination of three factors available preoperatively—the NLR, and serum CRP and CA19-9 levels—could predict the prognosis of ICC after surgery. This simple and easily administered preoperative prognosis grading system can predict survival information accurately and may identify patients who require further treatment.
During the past decade, there has been accumulating evidence that preoperative serum biomarkers can predict the survival of ICC patients after surgery. Elevated levels of tumor markers, including CA19-9 and CEA, were reported to be associated with a relatively poor prognosis in ICC.5,8,12 Particularly, CA19-9 has been well described as reflecting tumor progression.30 In the present study, elevated serum CA19-9 levels dichotomized by the minimum P value approach (cutoff value, 500 IU/mL) were independently associated with poorer OS. Although this cutoff value was higher than those reported previously, we considered this value meaningful in terms of identifying patients who did not benefit from previous surgery.5,8,12,30 Despite the significant role of the SIR in the prognostic prediction of various malignancies, including hepatobiliary malignancies, few studies have investigated its role in ICC.16–23 We demonstrated the significance of CRP and the NLR in the prediction of prognosis in ICC. Cutoff values for the NLR and CRP (5 and 5 mg/L, respectively) were deemed acceptable compared with previously reported values.19,22 Until now, a prediction classification system using these serum biomarkers has not been available. We have demonstrated successfully that a synergistic combination of the SIR and tumor markers could help to predict postsurgical prognosis in ICC.
The unsatisfactory prognosis and high recurrence rates of ICC following surgery will result in the preferential administration of multidisciplinary treatment strategies, despite the lack of established data. A recent multi-institutional study demonstrated the significance of adjuvant chemotherapy for ICC, especially in patients with lymph node metastasis.11 In fact, our previous data indicated a significant improvement in the postsurgical outcomes of patients with lymph node metastasis with the administration of adjuvant chemotherapy.27 Therefore, neoadjuvant chemotherapy is promising for patients with suspicious lymph nodes on preoperative imaging.10 However, this preoperative imaging characteristic cannot be detected accurately in certain cases. The preoperative prognostic grading system partly appears to reflect lymph node status (Table 3) and might help to diagnose nodal status in patients who present with unsuspected nodal-positive disease. Therefore, it might be best to judge the indications for multidisciplinary therapies based on both imaging findings and our proposed preoperative prognostic grading system.
This present study included only 134 consecutive patients from a single institution who underwent surgery with a long follow-up period. Therefore, our study population suffered from selection biases, including those caused by indications for surgery and other therapeutic options. The inclusion of adjuvant chemotherapy, which was introduced at our institution after 2006, in the multivariate analysis partly compensates for this limitation.27 Second, we did not evaluate other well-known inflammatory scores such as the prognostic nutritional index (PNI)31, or the Glasgow prognostic score (GPS)32 and its variants. These scores are based on the evaluation of serum CRP levels following a decrease in serum albumin concentrations. Another limitation of the present study was its retrospective design.
In conclusion, a novel biomarker-based preoperative grading system for ICC is a simple and effective method for the prediction of disease prognosis and may identify patients who require further treatment.
References
Aljiffry M, Abdulelah A, Walsh M, et al. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009;208:134–47.
Ikai I, Arii S, Okazaki M, et al. Report of the 17th nationwide follow-up survey of primary liver cancer in Japan. Hepatol Res. 2007;37:676–91.
Bridgewater J, Galle PR, Khan SA, et.al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–89.
Mavros MN, Economopoulos KP, Alexiou VG, et al. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014;149:565–74.
Ribero D, Pinna AD, Guglielmi A, et al. Italian Intrahepatic Cholangiocarcinoma Study Group. Surgical approach for long-term survival of patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis of 434 patients. Arch Surg. 2012;147:1107–13.
Farges O, Fuks D, Boleslawski E, et al. Influence of surgical margins on outcome in patients with intrahepatic cholangiocarcinoma: a multicenter study by the AFC-IHCC-2009 study group. Ann Surg. 2011;254:824–30.
de Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011;29:3140–5.
Jiang W, Zeng ZC, Tang ZY, Fan J, et al. A prognostic scoring system based on clinical features of intrahepatic cholangiocarcinoma: the Fudan score. Ann Oncol. 2011;22:1644–52.
Roayaie S, Guarrera JV, Ye MQ, et al. Aggressive surgical treatment of intrahepatic cholangiocarcinoma: predictors of outcomes. J Am Coll Surg. 1998;187:365–72.
Maithel SK, Gamblin TC, Kamel I, et al. Multidisciplinary approaches to intrahepatic cholangiocarcinoma. Cancer. 2013;119:3929–42.
Miura JT, Johnston FM, Tsai S, et al. Chemotherapy for surgically resected intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2015;22:3716–23.
Wang Y, Li J, Xia Y, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013;31:1188–95.
Hyder O, Marques H, Pulitano C, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma an Eastern and Western experience. JAMA Surg. 2014;149:432–8.
Grobmyer SR, Wang L, Gonen M, et al. Perihepatic lymph node assessment in patients undergoing partial hepatectomy for malignancy. Ann Surg. 2006;244:260–4.
Okabayashi T, Yamamoto J, Kosuge T, et al. A new staging system for mass-forming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Cancer. 2001;92(9):2374–83.
Marrero JA. Biomarkers in cholangiocarcinoma. Clin Liver Dis. 2014;3:101–3.
Okamura Y, Sugiura T, Ito T, et al. Neutrophil to lymphocyte ratio as an indicator of the malignant behaviour of hepatocellular carcinoma. Br J Surg. 2016;103:891–8.
Mano Y, Shirabe K, Yamashita Y, et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg. 2013;258:301–5.
Malik HZ, Prasad KR, Halazun KJ, et al. Preoperative prognostic score for predicting survival after hepatic resection for colorectal liver metastases. Ann Surg. 2007;246:806–14.
Saito H, Noji T, Okamura K, et al. A new prognostic scoring system using factors available preoperatively to predict survival after operative resection of perihilar cholangiocarcinoma. Surgery. 2016;159:842–51.
Lin G, Liu Y, Li S, et al. Elevated neutrophil-to-lymphocyte ratio is an independent poor prognostic factor in patients with intrahepatic cholangiocarcinoma. Oncotarget. 2016. doi:10.18632/oncotarget.7680.
Chen Q, Yang LX, Li XD, et al. The elevated preoperative neutrophil-to-lymphocyte ratio predicts poor prognosis in intrahepatic cholangiocarcinoma patients undergoing hepatectomy. Tumour Biol. 2015;36:5283–9.
Gomez D, Morris-Stiff G, Toogood GJ, et al. Impact of systemic inflammation on outcome following resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2008;97:513–8.
Chen Q, Dai Z, Yin D, et al. Negative impact of preoperative platelet-lymphocyte ratio on outcome after hepatic resection for intrahepatic cholangiocarcinoma. Medicine (Baltimore). 2015;94:e574. doi:10.1097/MD.0000000000000574.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–4.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;40:205–13.
Yoh T, Hatano E, Nishio T, et al. Significant improvement in outcomes of patients with intrahepatic cholangiocarcinoma after surgery. World J Surg. 2016;40:2229–36.
Yoh T, Hatano E, Yamanaka K, et al. Is surgical resection justified for advanced intrahepatic cholangiocarcinoma? Liver Cancer. 2016;5:280–9.
Strasberg SM, Phillips C. Use and dissemination of the Brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013;257:377–82.
Bergquist JR, Ivanics T, Storlie CB, et al. Implications of CA19-9 elevation for survival, staging, and treatment sequencing in intrahepatic cholangiocarcinoma: a national cohort analysis. J Surg Oncol. 2016. doi:10.1002/jso.24381.
Nozoe T, Ninomiya M, Maeda T, et al. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surg Today. 2010;40:440–3.
Forrest LM, McMillan DC, McArdle CS, et al. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003;89:1028–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURES
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yoh, T., Seo, S., Hatano, E. et al. A Novel Biomarker-Based Preoperative Prognostic Grading System for Predicting Survival After Surgery for Intrahepatic Cholangiocarcinoma. Ann Surg Oncol 24, 1351–1357 (2017). https://doi.org/10.1245/s10434-016-5708-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5708-z