Abstract
Background
Physical and psychological distress may occur in patients facing an onco-haematological diagnosis and undergoing complex therapies such as intensive chemotherapy, stem cell transplantation, and immunotherapy. Studies have shown the need for incorporating different therapeutic modalities to respond to patients’ physical and psychosocial needs.
Aims
The purpose of this study was to evaluate the effectiveness of music therapy treatment on mood, anxiety, depression, and physical discomfort in hospitalized onco-haematological patients.
Methods
Forty patients were included in this music therapy study from November 2021 to May 2023. Treatment consisted of individual weekly music therapy sessions. Participants completed the following evaluation instruments before and after the intervention: the Hospital Anxiety and Depression Scale (HADS), Profile of Mood States—Short Form A-Version (POMS-A), and European Organization for Research and Treatment of Cancer-Quality of Life Core Questionnaire-30 (EORTC QLQ-C30). A three-item numerical rating scale (NRS) for anxiety, sadness, and physical discomfort was administered at the beginning and end of each session (pre-/postsession).
Results
Differences (p < 0.05) were shown in NRS scores for anxiety, sadness, and physical discomfort before and after the music therapy sessions. Quality of life (QoL) was affected in almost all items, and patients could be anxious at a nonclinical level, but they were clinically depressed. EORTC QLQ-C30 scores for insomnia and pain related to the hospitalization process got worse after discharge.
Conclusions
The interim results of our study showed that music therapy sessions can positively change emotional distress and improve the mood of haematological patients after every session. Despite the difficulties and limitations of this study, this preliminary report contributes to a greater understanding of the potential benefits of music therapy in hospitalized onco-haematological patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Music has been applied in the medical-health context since ancient times, and the study and application of music as a therapeutic resource have evolved based on the beliefs and customs in each era. Interest in the application of music therapy in the medical field has been growing since the 1980s. This is a consequence of the satisfactory results of various studies and investigations. The number of scientific studies on the effects of music in medical treatment continues to grow, offering valuable insights to health care professionals and exciting implications for future research and clinical applications. This discipline has shown its beneficial effects in different fields of health, one of which is oncology [1, 2].
The application and efficacy of music therapy in the oncological context have been specifically studied and analysed during the last 30 years. Munro and Mount first described the application of music therapy in cancer patients in 1978 [3]. Since then, different studies have contributed to the knowledge and dissemination of the role of music therapy in this context, a fact that has helped to create a space and a function for music therapy in the field of oncology and psycho-oncology. Authors such as O'Callaghan and Hiscock [4] use the term "oncological music therapy" to refer to music therapy interventions aimed at cancer patients of all ages, with different cancer prognoses and at different times of the disease. Magill [5] describes integrative music therapy, a specialty of music therapy that is considered within integrative oncology programs and that is applied to treat multiple symptoms such as pain, mood disorders and aspects of communication. Music can improve pain and symptoms such as fear, anxiety, depression, frustration, and loneliness. Music therapy reduces the effects of noxious stimuli while improving the mood and producing feelings of comfort and a sense of control [6].
The literature has increasingly shown the importance of nonpharmacological and complementary therapies to control pain and other symptoms related to chronic diseases. Two meta-analyses carried out in the context of music therapy in medicine reported significant results for variables such as nausea, vomiting, mood, pain, and well-being [2, 7]. Different programs have shown how oncological music therapy is an effective complementary and therapeutic intervention offering a multimodal and comprehensive approach that makes it possible to care for a patient's physiological and psychosocial needs.
Some studies have been carried out in the context of onco-haematology. They have shown the efficacy of music therapy in improving both the physical and psychosocial well-being of bone marrow transplant patients. Among the reported benefits after participating in music therapy sessions, the reduction of anxiety, distress, and fatigue can be highlighted, as well as the increase in states of relaxation and well-being and the improvement of mood [8,9,10,11,12,13,14,15,16,17].
Music therapy interventions thus have an exciting influence on mood and can, in turn, improve quality of life. Mood and quality of life are two variables that have been the subject of interest in oncology music therapy over the years. Unfortunately, although studies exist in this field, the number of published studies with subjects with an onco-haematological diagnosis who are undergoing complex therapies (intensive chemotherapy, stem cell transplantation, immunotherapy, and palliative care) still needs to be increased.
We aimed to determine whether music therapy positively impacts mood disturbances during hospitalization in patients with haematological malignancies.
Methods
We performed a prospective study (IIBSP-MUS-2020–137) of adult patients (≥ 18 years old) who were admitted to the haematology unit to evaluate the effect of music therapy. Patients had to be diagnosed with haematological cancer and be able to actively participate in and follow a music therapy session. Exclusion criteria were an uncontrolled psychiatric disorder and moderate or severe hearing impairment. Patients with psychological support from a psycho-oncologist were allowed to participate.
Music therapy sessions, questionnaires, and mood assessments
Sessions
Weekly music therapy sessions were planned. Patients received at least one and up to six sessions during hospitalization, depending on their needs and length of hospitalization. The duration of each session ranged from 15 to 60 min and was based on the patient's musical preferences. Adherence was sometimes limited by physical discomfort and by gastrointestinal and mucosal toxicity associated with chemotherapy. Based on the results of previous studies, different therapeutic strategies were designed to improve the patient's mood and facilitate the expression of emotions and ventilation of feelings. Singing, lyric analysis, and composition were used to channel verbal and nonverbal emotions and feelings. In contrast, music-assisted relaxation was used to promote relaxation states and distract patients from their worries. The following 2 techniques were applied accompanied by both live or recorded music, according to patient preferences: Progressive Relaxation (a technique that focuses on one part of the body at a time, without creating muscular tension, and with the goal of releasing any tension on that part); and Visualization (a technique that focuses attention on expands on pleasant and calming images). Music listening and instrument playing were used to promote social interaction.
Questionnaires and design
Six baseline questionnaires (pretreatment) were completed as follows:
-
Demographic Information Form (completed by the patient)
-
Clinical Information Form (completed by the physician)
-
Musical Preferences and Previous Musical Experience Questionnaire (completed by the patient)
-
Hospital Anxiety and Depression Scale (HADS) (completed by the patient)
-
Shortened Profile of Mood States questionnaire (POMS-A, Spanish version) (completed by the patient)
-
European Organization for Research and Treatment of Cancer-Quality of Life Core Questionnaire-30 (EORTC QLQ-C30) (completed by the patient)
The following were completed before and after each music therapy session:
-
Numerical Rating Scale (NRS) for Anxiety, Sadness, and Physical Discomfort (completed by the patient)
-
Music Therapy Behaviour Observation Form (completed by the music therapist)
The following were completed before discharge (posttreatment 1).
-
Music Therapy Program Satisfaction Questionnaire (MTPSQ) (completed by the patient)
-
HADS, POMS, and EORTC QLQ-C30 (completed by the patient)
The following were completed during the outpatient visit 2 weeks after discharge (posttreatment 2).
-
HADS, POMS, and EORTC QLQ-C30 (completed by the patient)
Questionnaire parameters
The Musical Preferences and Previous Musical Experience Questionnaire collects data on patients' favourite songs, artists, musical instruments, musical styles, and the types of music and musical instruments they disliked. This questionnaire also asks about previous musical experience, band participation, or instruments played.
The HADS [18] comprises seven questions that evaluate anxiety and seven questions that evaluate depressive mood. Normal scores range between 0 and 7; risk scores range from 8–10, and scores equal to or higher than 11 are considered to indicate pathology.
The Shortened POMS-A [19] consists of a 15-item, five-point adjective rating scale in which participants rate how they are feeling at the current moment or during the past week (scores range from (0) “not at all” to (4) “extremely”). This self-report inventory includes four negative affect scales (the Tension, Depression, Anger, and Fatigue scales) and one positive affect scale (the Vigour scale). Subscale scores are summed to determine the total mood disturbance score (TMS), for which higher scores indicate greater mood disturbances.
The European Organization for Research and Treatment of Cancer-Quality of Life Core Questionnaire-30, EORTC QLQ-C30 [20, 21] is a questionnaire used to assess the quality of life of cancer patients, and it is a typical test used in the music therapy field. It includes five multi-item scales of functioning (physical, role, social, emotional, and cognitive functioning), a Global Health Scale, and a Scale of Symptoms and Problems. Twenty-eight of the 30 items are measured by a four-point Likert-type scale (1 = not at all, 2 = a little bit, 3 = quite a bit, 4 = very much), and the two remaining items, which address global physical health and global quality of life, are measured by a seven-point scale. The time frame focuses on the previous week. The raw scores for all multi and single-item scales are linearly transformed to 0-to-100 scales, with '100' reflecting the highest functioning or highest symptomatology. Our population included different types of haematological patients, and we considered it more appropriate to compare them with an "all cancer patients” referral sample [20].
At the end of the program, patients anonymously completed the Music Therapy Program Satisfaction Questionnaire (MTPSQ), designed ad hoc for this study, to provide information about their personal experiences in the music therapy program.
Statistical analysis
We used frequencies and dispersion statistics to describe the study population and scale values. To analyse differences before and after music therapy sessions using the NRS for Anxiety, Sadness, and Physical Discomfort, we performed a two-tailed nonparametric paired sample test (Wilcoxon's signed rank test). We also used an unpaired two-sample t test to compare patients’ EORTC QLQ-C30 scores with those of the referral population. We performed a power analysis with an effect size of 1 and alpha error of 0.05 to determine which parameters could be compared with a power of detection ≥ 80%. Due to the sample size (the number of patient questionnaires), the only questionnaires that could be compared were the NRS (first, second, and third sessions), POMS-A (baseline and after discharge), and HADS (baseline and after discharge). The results of the other questionnaires (EORTC-Q30, POMS predischarge, and HADS predischarge) could not be compared due to the size of the sample and the risk of losing power to detect differences. Despite this, we will report the results.
We used GraphPad Prism Version 9.5.1; RStudio 2022.07.0. We used the statistical graphical user interface EZR [22], PROscorer, and the QoLMiss package [23, 24].
Results
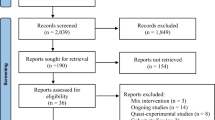
We present the preliminary results of the first 40 patients included in the study from November 2021 to May 2023 (see Fig. 1. Consort flowsheet participants). All participants gave their informed consent.
The patients' characteristics are summarized in Table 1. Three patients were taking anxiolytics (alprazolam), and one of them was also taking an antidepressant (citalopram). Two patients received psychological support.
Adherence to the protocol
Despite offering the study to all potential participants, only 15% agreed to participate. We perceived that adult patients did not fully understand the concept of music therapy and that they preferred not to experience disturbances that could break their equilibrium. The NRS for Anxiety, Sadness, and Physical Discomfort before and after each music therapy session was completed by ≈100% of the participants. However, the HADS, POMS-A, and EORTC QLQ-C30 questionnaires were mainly completed at baseline. Less than half of the patients with more than one music therapy session completed questionnaires before discharge and in the outpatient setting.
The study was conducted as described in Fig. 2.
Numerical rating scale (NRS) for anxiety, sadness and physical discomfort
The NRS is a continuous scale with a total score up to 10 points. The distribution of the samples was not normal (Shapiro‒Wilk test). Wilcoxon's signed rank test showed differences (p < 0.05) in the anxiety, sadness, and physical discomfort scores before and after the music therapy sessions. The positive effect of music therapy was similar after the first, second, and third sessions. In general, the reduction in symptoms was ≥ 50%. The results are summarized in Table 2. The effect was consistent for every music therapy session. To analyse whether there was a tendency over time, we performed a Friedman test, and we did not find any tendency.
POMS and HADS
Thirty-three patients completed the POMS-A at baseline [25]. The mean value for anger was 1.00 (SD 2.26), that for fatigue was 4.0 (SD 3.17), that for vigour was 5.0 (SD 2.78), that for tension was 3.0 (SD 2.18), and that for depressed mood was 2.0 (SD 2.69). The mean POMS-A total mood disturbance score was 21.0 (SD 9.31).
Seven patients completed the POMS-A predischarge. The mean value for anger was 2.00 (SD 3.25), that for fatigue was 6.0 (SD 3.34), that for vigour was 5.0 (SD 2.37), that for tension was 3.0 (SD 2.58), and that for depressed mood was 2.0 (SD 2.24). The mean POMS-A total mood disturbance score was 23.0 (SD 10.5).
Fifteen patients completed the POMS-A 2 weeks after discharge. The mean value for anger was 4.00 (SD 2.34), that for fatigue was 3.0 (SD 3.02), that for vigour was 5.0 (SD 2.63), that for tension was 3.0 (SD 2.64), and that for depressed mood was 3.0 (SD 2.87). The mean POMS-A total mood disturbance score was 23.0 (SD 8.9).
The maximal expected score for the POMS-A was 60 (with 0 indicating no mood disturbance, 30 indicating a moderate mood disturbance, and 60 indicating an extreme mood disturbance).
With these results, we can conclude that there is a tendency towards moderate mood disorder in these patients.
Thirty-four patients completed the HADS questionnaire at baseline [18]. This revealed a mean score of 7 (SD 2.30) for anxiety and 13.2 (SD 1.92) for depression.
Eight patients completed the HADS questionnaire predischarge. This revealed a mean score of 8 (SD 3.31) for anxiety and 14.5 (SD 3.59) for depression.
Fifteen patients completed the HADS questionnaire two weeks after discharge. This revealed a mean score of 8 (SD 2.95) for anxiety and 13.0 (SD 2.85) for depression.
In summary, patients provided risk scores for anxiety predischarge and two weeks after discharge, and there were pathological scores across all times for depression.
To determine the presence of differences between POMS-A, HADS anxiety, and HADS depression scores at baseline and two weeks after discharge, we performed Wilcoxon's signed rank test, and we did not find any differences (see Fig. 3). We did not include predischarge questionnaires because the number of completed questionnaires was not enough to make comparisons.
EORTC QLQ-C30 questionnaire
The results of the EORTC QLQ-C30 in our study population are summarized in Table 3.
We performed a Wilcoxon's signed rank test between baseline and postdischarge scores, and we found a significant increase in pain and insomnia scores after discharge (p < 0.05).
We also compared the baseline EORTC QLQ-C30 (n = 33) with the "all cancer patients" referral population (see Table 4).
For the functioning scale and global QOL scores, our population had impaired functioning compared with the referral population, except for emotional functioning. For the symptom scales, our patients had higher scores, indicating a higher symptom burden.
Music therapy program satisfaction questionnaire (MTPSQ)
Fifteen patients completed the MTPSQ before discharge.
With regard to the patients’ general mood perceptions within the music therapy sessions, the results showed a mean score of 2.5 (based on a Likert scale ranging from 0 to 3) (see Fig. 4).
This questionnaire permitted us to explore other aspects that may have contributed to elevating the patients’ moods, since they deal with different strategies and resources that may help in emotional self-regulation. Communicating and interacting with music therapists, family caregivers, and staff was considered the best strategy during the music therapy sessions, with a mean score of 2.6. The expression of emotions and feelings, distractions and relaxation activities were perceived as a favourable strategy, with a mean score of 2.4. Speaking about one’s illness was an important issue addressed during the sessions that might have also led to facilitating emotional expression and ventilation, with a mean score of 2.1.
Based on patient ratings, we can affirm that the participants perceived this program as useful, with a mean score of 2.66 (0 = not at all; 1 = a little; 2 = enough; 3 = a lot).
Finally, it is important to state that almost all of the participants would recommend this program to other patients; a mean score of 2.93 was obtained for this item.
Discussion
Our study was designed to answer two main research questions: (a) what are the possible changes in the moods, anxiety, depression, and quality of life of hospitalized haematological cancer patients after music therapy (pre-/posttreatment), and (b) what are the possible changes during each 15/60-min music therapy session (pre-/postsession) in the perceived anxiety, sadness and physical discomfort of haematological cancer patients?
The main difference between our study and previous reports is that it includes hospitalized patients only, a complex population (the majority isolated), and our intervention is adapted to each patient with a particular clinical condition.
Here, we present the first preliminary results of the study, which reflect a complex population with diminished QoL and clinically relevant mood disorders.
Less than 20% of the patients agreed to participate. This avoidance might reflect the difficulties and insecurities that these patients were experiencing during the particular clinical episode.
It is even possible that the patients who agreed to participate were those with a better status; this is worrying since the patients who did not participate were not receiving any psychological help. Therefore, it is imperative to actively implement psychological support for this population.
This study compared the effect of music therapy on patients’ mood from pre- to post-session based on three parameters (anxiety, sadness, and physical discomfort) that changed significantly. We demonstrated that music therapy was effective in reducing patients’ emotional and physical discomfort during the sessions, helping to alleviate anxiety, sadness, and physical discomfort every time it was delivered.
As clinicians are directly involved in therapeutically treating and supporting these patients, we consider it relevant to determine the number or type of interventions that could be combined with music therapy to achieve better control of symptoms in the future. This is a matter of frequency and would depend on the ability to adapt music therapy sessions to the clinical scenario. Treatment adherence to music therapy and continuous attendance to following sessions of this group matches with attendance rates of other studies with patients who are in active oncologic treatment, where participants have lower attendance rates or even abandon programs due to health complications, deterioration of symptoms, and physical limitations, as well as referral to intensive care unit or even death. Many music therapy studies in oncology have based the intervention on merely one or two sessions, and few offer a continuity of more sessions.
Achieving the ideal music therapy dosage might also impact the global perception of all supportive therapies that could improve mental health. It is essential to show that these interventions are relevant to patients experiencing the oncological process with tangible results. The knowledge that music therapy is effective will help improve adherence and inspire others to participate in music therapy programs. The participants' satisfaction was high, and no participants reported adverse effects.
We are very aware that the improvement of QoL is linked to the restoration of health; in our case, this would be the resolution of the oncological process. That is why we were not surprised that we could not improve QoL with music therapy during hospitalization, even less so in a short time.
However, if music therapy (and other supportive interventions) is maintained over time, particularly in outpatient settings, QoL could be improved. The objective is to accompany the patient and make the process more bearable, even in an end-of-life situation.
This study has several limitations. We are reporting our first data, which represents an intent-to-treat population. This study included a heterogeneous population, but it perfectly reflected the reality of more severely compromised haematological patients, and with this first analysis, we were able to establish the future direction we must take.
Conclusions
This study indicated that music therapy can positively change emotional distress and improve the moods of haematological patients. Despite the difficulties and limitations of this study, the authors hope this paper contributes to a greater understanding of the potential benefits of music therapy in this population.
Availability of data and materials
Data are available on request only due to ethical & legal reasons.
Abbreviations
- EORTC QLQ-C30:
-
European Organization for Research and Treatment of Cancer-Quality of Life Core Questionnaire-30
- HADS:
-
Hospital Anxiety and Depression Scale
- MTPSQ:
-
Music Therapy Program Satisfaction Questionnaire
- NRS:
-
Numerical Rating Scale
- POMS-A:
-
Shortened Profile of Mood States questionnaire
- QoL:
-
Quality of life
- SD:
-
Standard deviation
- TMD:
-
Total mood disturbance score
References
Martí-Augé P, Mercadal-Brotons M, Solé-Resano C. La musicoterapia en oncología. Gac Mex Oncol. 2015;14:346–52.
Bradt J, Dileo C, Myers-Coffman K, Biondo J. Music interventions for improving psychological and physical outcomes in people with cancer. Cochrane Database Syst Rev. 2021;10:CD006911.
Munro S, Mount B. Music therapy in palliative care. Can Med Assoc J. 1978;119:1029–34.
O’Callaghan C, Hiscock R. Interpretive subgroup analysis extends modified grounded theory research findings in oncologic music therapy. J Music Ther. 2007;44:256–81.
Magill L. Role of music therapy in integrative oncology. J Soc Integr Oncol. 2006;4:79–81.
Aldridge D. Music therapy research and practice in medicine: from out of the silence. London: Jessica Kingsley; 1996.
Augé PM, Mercadal-Brotons M. Musicoterapia en medicina: aplicaciones prácticas. Barcelona: Editorial Médica JIMS; 2010.
Cassileth BR, Vickers AJ, Magill LA. Music therapy for mood disturbance during hospitalization for autologous stem cell transplantation: a randomized controlled trial. Cancer. 2003;98:2723–9.
Dóro CA, Neto JZ, Cunha R, Dóro MP. Music therapy improves the mood of patients undergoing hematopoietic stem cells transplantation (controlled randomized study). Support Care Cancer. 2017;25:1013–8.
Bates D, Bolwell B, Majhail NS, Rybicki L, Yurch M, Abounader D, et al. Music therapy for symptom management after autologous stem cell transplantation: results from a randomized study. Biol Blood Marrow Transplant. 2017;23:1567–72.
Ratcliff CG, Prinsloo S, Richardson M, Baynham-Fletcher L, Lee R, Chaoul A, et al. Music therapy for patients who have undergone hematopoietic stem cell transplant. Evid Based Complement Alternat Med. 2014;2014:742941.
Reimnitz L, Silverman M. Perceived mechanisms targeting cancer-related fatigue, song choice rationale, and song function: an interpretivist study of patient-preferred live music with adult oncology patients on a blood and marrow transplant unit. Psychol Music. 2021;49:1401–14.
Andersen D, Sarah EP, Michael JS. Immediate effects of music therapy on fatigue in hospitalized patients on a bone marrow transplant unit: a pilot study. Korean J Music Ther. 2012;14:47–64.
Fredenburg HA, Silverman MJ. Effects of music therapy on positive and negative affect and pain with hospitalized patients recovering from a blood and marrow transplant: a randomized effectiveness study. Arts Psychother. 2014;41:174–80.
Geyik G, Doğan S, Ozbek H, Atayoglu AT. The effect of music therapy on the physical and mental parameters of cancer patients during hematopoietic stem cell transplantation. Perspect Psychiatr Care. 2021;57:558–64.
Humprey H. Current practices in music therapy with bone marrow and organ transplant recipients. 2016. https://uknowledge.uky.edu/music_etds/65. Accessed 28 Dec 2022.
Ruiz A. Intervención musicoterapéutica en pacientes oncohematológicos sometidos a trasplante autólogo: aplicación del modelo helen bonny de imagen guiada y música (BMGIM). 2018. https://digitum.um.es/digitum/handle/10201/56295. Accessed 28 Dec 2022.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Fuentes Y, García-Merita M, Melià J, Balaguer Y. Formas paralelas de la adaptación valenciana del pefil de estados de ánimo (POMS). In: IV congreso de evaluación psicológica, 21–24 de septiembre. Santiago de Compostela, Spain; 1994.
Scott NW, Fayers P, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, et al. EORTC QLQ-C30 reference values manual. Brussels, Belgium: EORTC Quality of Life Group; 2008.
Michalos AC. European organization for research and treatment of cancer core quality of life questionnaire. In: Michalos AC, editors. Encyclopedia of quality of life and well-being research. Dordrecht: Springer Netherlands; 2014. p. 2014.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Baser R. CRAN-package PROscorer. In The R project for Statistical Computing https://cran.r-project.org/web/packages/PROscorer/index.html. Accessed 14 Jan 2023.
Bhattacharjee A. Scales score calculation from quality of life data. 2022. In The R project for Statistical Computing. https://cran.r-project.org/package=QoLMiss. Accessed 14 Jan 2023.
Andrade E, Arce C, de Francisco C, Torrado J, Garrido J. Versión breve en español del cuestionario POMS para deportistas adultos y población general. Rev Psicol Deporte. 2013;22:95–102.
Acknowledgements
We want to acknowledge all volunteers who helped start the crowd-founding program to cover the budget of this study, especially Paola Grommes, Laia Cendros, Noemí Gutierrez, Lucia Breton, Fernanda Aleman, and David Grau.
Funding
The study was supported by donations.
Author information
Authors and Affiliations
Contributions
Patricia, Iria, and Silvana worked in conceptualization, data curation; formal analysis; funding acquisition; investigation; methodology. Silvana was involved in project administration; resources; supervision, and validation. Patricia and Silvana worked on writing and reviewing the final draft. Irene, Joel, Mariona, Melissa, and Cristina worked on the investigation. Jorge collaborated in funding acquisition.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of our institution (CEIm—Fundació de Gestió Sanitaria Hospital de la Santa. Creu i Sant Pau)approved the study. All eligible patients gave their informed consent to participate and to register their clinical and demographic information. Some patients were allowed to record audio and videos. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martí, P., Fontanals, I., Funtané, J. et al. Preliminary results of the effect of music therapy treatment on anxiety, sadness, physical discomfort, mood, and quality of life in hospitalized onco-haematological patients. BMC Psychol 11, 425 (2023). https://doi.org/10.1186/s40359-023-01459-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-023-01459-x