Abstract
Background
Cement mantle penetration and the cement–bone interface strength were critical to a successful primary total knee arthroplasty (TKA). It remained unclear whether decreased blood and fat in the cancellous bone achieved with the use of a tourniquet increases tibial cement mantle penetration in different zones on AP and lateral view in TKA according to criteria defined by the Knee Society Scoring System (KSS). The purpose of this study was to determine whether tourniquet use influences tibial cement mantle penetration in different zones on AP and lateral view in TKA according to KSS.
Methods
We conducted a meta-analysis to identify studies involving the impact of tourniquet use and no tourniquet use on tibial bone cement penetration in primary TKA in electronic databases, including Web of Science, Embase, PubMed, Cochrane Controlled Trials Register, Cochrane Library, Highwire, CBM, VIP, Wanfang database, up to January 2021. Finally, we identified 1231 patients (1231 knees) assessed in twelve studies.
Results
Tourniquet use increases the cumulative cement mantle penetration (P < 0.00001), mean cement mantle penetration (P = 0.004), and cement mantle in zone 3(P < 0.0001) on AP view. However, there were no significant differences in cement mantle in zone 1(P = 0.5), zone 2(P =0 .54), zone 4(P = 0.07) on AP view, and zone 1(P = 0.32), zone 2(P = 0.38) on lateral view between two groups. There were also no significant differences in length of surgery(P = 0.7), change in hemoglobin(P = 0.4), transfusion rates(P = 0.47), and complications such as muscular calf vein thrombosis(P = 0.21), superficial infection (P = 0.72), and deep vein thrombosis (P = 0.66) between two groups.
Conclusion
The application of a tourniquet increases the thickness of the tibial bone cement penetration—the increase in the thickness of bone cement penetration mainly located in zone 3 on the anteroposterior (AP) view.
Similar content being viewed by others
Background
Cement mantle penetration and the strength of the cement–bone interface are critical to a successful primary TKA. Because bone cement has no adhesive properties, adequate penetration is vital to achieve component stability by mechanical interlock with bony trabecular spaces [1,2,3,4]. Increased cement mantle thickness has also been shown to confer increased implant survival and stability [1, 5, 6]. One of the factors that can easily affect the cementation during TKA is a tourniquet during surgery [7]. The potential benefit of tourniquet use was to aid in preparing the bone surface for cementation by reducing the blood and fat in the field and offers better visualization due to bloodless field, which would facilitate cementing quality [8]. Some literature found tourniquet use will increase the bone cement penetration [7, 9,10,11,12]. However, some studies suggest that tourniquet use does not affect cement mantle penetration [13,14,15,16,17]. There is no consensus and evidence-based medicine of tourniquet use on bone cement mantle penetration, especially bone cement mantle penetration in a different zone. Therefore, in this meta-analysis, our specific purpose was to determine whether tourniquet use influences tibial cement mantle penetration in different zones on AP and lateral view in TKA based on the Knee Society scoring system (KSS) [18].
Methods
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement, we strictly followed the PRISMA (preferred reporting items for systematic review and meta-analysis) guidelines to conduct this analysis [19].
Search strategy
We conducted a meta-analysis to identify studies involving the impact of tourniquet use and no tourniquet use on tibial bone cement penetration in primary TKA in electronic databases, including PubMed, Web of Science, Embase, Cochrane, Controlled Trials Register, Cochrane Library, Highwire, CBM, VIP, CNKI, Wanfang database, up to January 2021. The keywords used were “total knee arthroplasty,” “total knee replacement,” “tourniquet,” “bone cement mantle,” penetration,” in conjunction with Boolean operators “AND” or “OR.” We used the Review Manager Software was to perform the meta-analysis.
Inclusion criteria
This review includes randomized controlled trials (RCTs) and non-randomized studies of interventions (NRSI) with a control group that comparing the impact of tourniquet use and no tourniquet use on tibial bone cement penetration in primary TKA. The included studies should meet the following inclusion criteria: (1) The TKA procedure was performed for the first time. (2) The impact of tourniquet use on tibial bone cement penetration was involved. (3) The comparator was the impact of no tourniquet use on tibial bone cement penetration in the original comparative study. (4) At least one of the following indexes was reported: the thickness of cement mantle penetration on the tibia, surgery duration, change in hemoglobin, transfusion rates, and complications such as muscular calf vein thrombosis (MCVT), superficial infection, and deep vein thrombosis (DVT). We also excluded (1) studies of TKA revision and (2) unclear or incomplete sample data were available.
Data extraction process
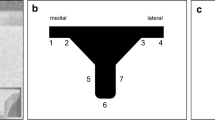
All RCTs and NORIs comparing the impact of tourniquet use and no tourniquet use on tibial bone cement penetration with primary TKA were identified and included from the search strategy. Two researchers independently reviewed titles and abstracts to assess study eligibility against the predefined criteria and independently extracted the available data from each study. Disagreements on inclusion of studies and data extractions were discussed and a consensus reached. Data were extracted based on the following: (1) research features (i.e., authors, type of study and year of publication), (2) population information (i.e., gender, body mass index (BMI), (3) intervention (i.e., tourniquet pressure, tourniquet time, the brand of bone cement, cementing technique, drainage). The primary outcome measure was the thickness of cement mantle penetration on the tibia, including different zones on AP and lateral view in TKA based on the Knee Society scoring system(KSS). Tibial anteroposterior (AP) zones 1, 2, 3, and 4 (Fig. 1) represent the medial and lateral inferior surfaces of the tibial baseplate, respectively. Tibial lateral zones 1 and 2 (Fig. 1) represent the anterior and posterior distal surfaces of the tibial baseplate, respectively. For zones in both the AP and lateral tibial views, cement penetration was measured at the one-third, two-third, or one-half marks. The cumulative cement penetration depth was calculated and expressed as the sum of all measurement. Cement depth was measured utilizing the measurement tool in the picture archiving and communication system (PACS). Secondary outcomes were surgery time duration, change in hemoglobin, transfusion rates, and complications such as MCVT, superficial infection, and DVT.
Assessment of studies
The two authors (C.J.S and X.Y.) independently assessed the risk of bias and quality of studies using the Cochrane Risk of Bias tool for randomized studies and the nine-star Newcastle-Ottawa scale (NOS) for NRSIs [20, 21]. Two researchers independently evaluated the studies, and disagreements were resolved through discussions with a third author or consensus. For this review, studies scoring ≤ 4 stars or at high risk of bias on Cochrane Risk of Bias tool were defined as being of low quality.
Statistical analysis
A random-effects model was used due to expected methodological heterogeneity among studies in relation to differences in cementing technique, tourniquet pressure, tourniquet time, and bone cement brand. In each study, we commonly used the odds ratio (OR) and relevant 95% confidence interval (CI) to measure dichotomous variables such as rates of transfusion and complications such as muscular calf vein thrombosis, superficial infection, and deep vein thrombosis. Given that the outcome is rare, OR was supposed to approximate RR (relative risk) based on Cornfield's rare disease outcome assumption [22]. The mean difference (MD) was used to assess continuous outcomes such as cement mantle penetration, length of surgery, and hemoglobin change with a 95% confidence interval (CI). Statistical algorithms were used to estimate the standard deviation for those studies that provided only continuous variables for means and range [23]. Meta-analysis was undertaken using Review Manager (version 5.3 for MAC, the Cochrane Collaboration, the Nordic Cochrane Centre, and Copenhagen, 2014). We considered the results as a statistically significant difference if p values were less than 0.05.
Results
Search results
The literature search strategy and selection process are shown in Fig. 2. Finally, eleven publications from 2014 to 2021 were included in our meta-analysis. Two hundred thirty-five relevant citations were identified from the databases according to the literature search strategy described earlier. After deleting 180 duplicates, we obtained 55 studies. Based on screening titles and abstracts of the 55 remaining articles, 38 irrelevant clinical studies were excluded. By reading the 17 full-text articles, we excluded another 5 articles for the following reasons: none-compare groups and no useful outcome data. The remaining 12 articles were deemed appropriate. Finally, we identified 1231 patients (1231 knees) assessed in (8 RCTs [7, 10, 13,14,15, 17, 22, 24] and 4 NRSIs [9, 11, 12, 16])
The search results and selection procedure. Two hundred thirty-five relevant citations were identified from the databases according to the literature search strategy described earlier. After deleting 180 duplicates, we obtained 55 studies. Based on screening titles and abstracts of the 55 remaining articles, 38 irrelevant clinical studies were excluded. By reading the 17 full-text articles, we excluded another 5 articles. Finally, we identified 1231 patients assessed in 12 articles
Study characteristics and quality
The characteristics of the 12 included studies are given in Tables 1 and 2. All included articles were published in English and Chinese between the years 2014 and 2021.
Risk of bias assessment
The methodological quality of the involved NRSIs ranged from seven to eight (Table 3). The risk of bias summary and risk of bias graph for RCTs are shown in Figs. 3 and 4. As a result, the overall quality of all included studies was considered adequate.
Cumulative thickness of cumulative cement mantle penetration
Five studies assessed the thickness of cumulative cement mantle penetration. The meta-analysis results showed a significant difference in cumulative thickness of cumulative cement mantle penetration between the tourniquet use group and no tourniquet use group (MD 2.09, 95% CI 1.64 to 2.54, P < 0.00001, I2 = 88%, Fig. 5). The results indicated that tourniquet use could increase the cumulative thickness of cement mantle penetration compared with the no tourniquet use group.
A forest plot diagram showing cumulative cement mantle penetration. Five studies assessed the thickness of cumulative cement mantle penetration. The meta-analysis results showed a significant difference in cumulative thickness of cumulative cement mantle penetration between the tourniquet use group and no tourniquet use group (MD 2.09, 95% CI 1.64 to 2.54, P < 0.00001, I2 = 88%)
Mean thickness of cement mantle penetration
Four studies reported the mean cement mantle penetration. The results showed significant difference in mean thickness of cement mantle penetration between the 2 groups (MD 0.1, 95% CI 0.03 to 0.17, P = 0.004, I2 = 0%; Fig. 6). The results indicated that compared with the no tourniquet use group, the tourniquet use could increase the mean thickness of cement mantle penetration.
The thickness of cement mantle penetration in different zones on AP and lateral view
Five studies reported the cement mantle penetration in zone 1 on AP view. The results showed no significant difference in cement mantle penetration in zone 1 on AP view between the 2 groups (MD 0.15, 95% CI - 0.28 to 0.57, P = 0.5, I2 = 96%, Fig. 7). Three studies reported the cement mantle penetration in zone 2 on AP view. The results showed no significant difference in Cement mantle penetration in zone 2 on AP view between the 2 groups (MD - 0.11, 95% CI - 0.47 to 0.25, P = 0.54, I2 = 85%, Fig. 7). Three studies reported the cement mantle penetration in zone 3 on AP view. The results showed significant difference in thickness of cement mantle penetration in zone 3 on AP view between the 2 groups (MD 0.23, 95% CI 0.12 to 0.34, P < 0.0001, I2 = 0%, Fig. 7). Five studies reported the cement mantle penetration in zone 4 on AP view. The results showed no significant difference in cement mantle penetration in zone 4 on AP view between the 2 groups (MD 0.29, 95% CI - 0.03 to 0.6, P = 0.07, I2 = 90%, Fig. 7). Five studies reported the cement mantle penetration in zone 1 on lateral view. The results showed no significant difference in cement mantle penetration in zone 1 on lateral view between the 2 groups (MD 0.18, 95% CI - 0.18 to 0.54, P = 0.32, I2 = 93%, Fig. 7). Five studies reported the cement mantle penetration in zone 2 on lateral view. The results showed no significant difference in cement mantle penetration in zone 2 on lateral view between the 2 groups (MD 0.18, 95% CI - 0.22 to 0.57, P = 0.38, I2 = 94%, Fig. 7).
A forest plot diagram showing cement mantle penetration in different zones on AP and lateral view. Five studies reported the cement mantle penetration in zone 1 on AP view. The results showed no significant difference in cement mantle penetration in zone 1 on AP view between the 2 groups (MD 0.15, 95% CI - 0.28 to 0.57, P = 0.5, I2 = 96%). Three studies reported the cement mantle penetration in zone 2 on AP view. The results showed no significant difference in cement mantle penetration in zone 2 on AP view between the 2 groups (MD - 0.11, 95% CI - 0.47 to 0.25, P = 0.54, I2 = 85%). Three studies reported the cement mantle penetration in zone 3 on AP view. The results showed significant difference in thickness of cement mantle penetration in zone 3 on AP view between the 2 groups (MD 0.23, 95% CI 0.12 to 0.34, P < 0.0001, I2 = 0%). Five studies reported the cement mantle penetration in zone 4 on AP view. The results showed no significant difference in cement mantle penetration in zone 4 on AP view between the 2 groups (MD 0.29, 95% CI - 0.03 to 0.6, P = 0.07, I2 = 90%). Five studies reported the cement mantle penetration in zone 1 on lateral view. The results showed no significant difference in cement mantle penetration in zone 1 on lateral view between the 2 groups (MD 0.18, 95% CI - 0.18 to 0.54, P = 0.32, I2 = 93%). Five studies reported the cement mantle penetration in zone 2 on lateral view. The results showed no significant difference in cement mantle penetration in zone 2 on lateral view between the 2 groups (MD 0.18, 95% CI - 0.22 to 0.57, P = 0.38, I2 = 94%)
Duration of surgery time
Four studies reported the length of surgery time. The results showed no significant difference in duration of surgery time between the two groups (MD - 1.4, 95% CI - 8.58 to 5.78, P = 0.70, I2 = 79%; Fig. 8)
Change in hemoglobin
Three studies reported the change in hemoglobin. The results showed no significant difference in change in hemoglobin between the two groups (MD - 0.58, 95% CI - 1.95 to 0.79, P = 0.4, I2 = 98%; Fig. 9)
Blood transfusion rate
Three studies reported the blood transfusion rate. The results showed no significant difference in blood transfusion rate between the two groups (OR 0.6, 95% CI 0.15 to 2.43, P = 0.47, I2 = 64%; Fig. 10)
Complications
Two studies reported the rate of MCVT. The results showed no significant difference in rate of MCVT between the 2 groups (OR 0.12, 95% CI - 0.07 to 0.3, P = 0.21, I2 = 65%; Fig. 11). Two studies reported the rate of superficial infection. The results showed no significant difference in the rate of superficial infection between the two groups (OR 0.01, 95% CI - 0.03 to 0.04, P = 0.71, I2 = 0%; Fig. 11). Two studies reported the rate of DVT. The results showed no significant difference in the rate of superficial infection between the two groups (OR 0.01, 95% CI - 0.03 to 0.05, P = 0.66, I2 = 0%; Fig. 11).
A forest plot diagram showing complications. Two studies reported the rate of MCVT. The results showed no significant difference in rate of MCVT between the 2 groups (OR 0.12, 95% CI - 0.07 to 0.3, P = 0.21, I2 = 65%). Two studies reported the rate of superficial infection. The results showed no significant difference in rate of superficial infection between the 2 groups (OR 0.01, 95% CI - 0.03 to 0.04, P = 0.71, I2 = 0%). Two studies reported the rate of DVT. The results showed no significant difference in rate of superficial infection between the 2 groups (OR 0.01, 95% CI - 0.03 to 0.05, P = 0.66, I2 = 0%)
Discussion
To the best of our knowledge, our study is the first meta-analysis to identify the tibial bone cement penetration in different zones on AP and lateral view according to the KSS with and without tourniquet application in primary TKA. There was only one meta-analysis identify the tibial bone cement penetration in TKA. However, they did not evaluate tibial cement mantle penetration in different zones on AP and lateral view. Our meta-analysis of 12 studied that evaluated a total of 1231 TKAs shows that the use of tourniquet increased the tibial cement mantle thickness in primary TKA. The increase of tibial cement mantle is mainly located in zone 3 on AP view. However, there no increase of tibial cement mantle in other zones, including zone 1, zone 2, zone 4 on AP view, and zone 1, zone 2 on the lateral view. There were also no significant differences in surgery time duration, change in hemoglobin, transfusion rates, and complications such as MCVT, superficial infection, and DVT between the two groups.
It is well known that increased initial fixation strength of the tibial component is an essential factor influencing the implant's continued function. Aseptic loosening is a devastating complication that usually occurs at the bone–cement interface [23]. Therefore, Increased cement penetration thickness is of paramount importance in creating an ideal cement–bone bond, determining the strength of the implant against shearing forces [6, 25, 26], and has also been shown to confer improved implant stability and survival [1, 5, 6]. Several studies [7, 13, 27, 28] have suggested that the optimal thickness of cement penetration is 3 to 4 mm for maximal cement–bone interface fixation. There are many factors that will improve the cement penetration such as uniform bone density with sufficient drill-hole interdigitation, reduced intraoperative bleeding [29,30,31], pulsed lavage [32,33,34,35], absence of sclerosis [33, 36], bone debris in cancellous bone [35, 37, 38], and blood at the cement–bone interface [32]. Some studies have found that tourniquet use leads to increased cement penetration [7, 39]. One potential advantage of using a tourniquet in cemented TKR is increased bone cement penetration due to decreased cancellous bone bleeding or clot debris during cementing [7]. Another advantage is that the tourniquet application offers better visualization due to the bloodless field, which would facilitate cementing quality [8]. Using a tourniquet can significantly decrease intraoperative blood loss and operation time but do not significantly decrease the rate of transfusion or DVT in TKA [40].
The result showing that the use of a tourniquet increases the tibial cement mantle thickness was consistent with the outcome of a previous meta-analysis [41]. However, in the previous study, they did not evaluate tibial cement mantle penetration in different zones on AP and lateral view. In our research, we found the increase of tibial cement mantle mainly located in zone 3 on AP view, and there was no increase of tibial cement mantle in other zones including zone 1, zone 2, zone 4 on AP view and zone 1, zone 2 on the lateral view. An explanation for the increase of the tibial cement mantle mainly located in zone 3 on AP view may be that zone 3 of the tibial cement mantle happens to be the most stressed area when the prosthesis is placed.
Hemoglobin change level and transfusion rate have been recognized as the most objective indicators of actual blood loss. In our study, there are no differences in hemoglobin change level and transfusion rate between the two groups, which was consistent with the outcome of the previous meta-analysis [40]. Tourniquet use may decrease intraoperative blood loss. However, Tourniquet release can result in ongoing bleeding from cut cancellous bone [42], blood extravasated into the knee joint and adjacent soft tissues [43], or blood loss from hemolysis [44].
A tourniquet will provide surgeons with a bloodless surgery field to facilitate the clear identification of anatomical structures with less electrocoagulation and wound irrigation during surgery, which might help shorten the operation time. However, our result showed tourniquet use did not reduce the duration of surgery time in our meta-analysis.
One of the more significant clinical concerns regarding tourniquet use is its association with thromboembolism. No significant difference was found between groups regarding the rate of IMVT and DVT in our study, which was consistent with Jawhar’s meta-analysis [45]. However, the complication of venous thrombosis is the secondary outcome, the number of included studies comparing venous thrombosis between two groups is little, although several studies have investigated the incidence of venous thrombosis using the tourniquet [46,47,48,49,50]. The evidence is mixed because of heterogeneous study groups, designs, and confounding factors like time of surgery making it difficult to compare.
Although we evaluated the impact of tourniquet on tibial bone cement penetration in different zones, we should know it is also very important to have a proper distribution of the cement through the porosity of the bone. Too much thickness of the mantle may imply danger to the bone as it goes deeper and increases necrosis risk. It is true and known from all the authors that bloodless field is better for the cementing time, so tourniquet should be applied in the cementing technique to get a proper interlocking mechanism of this tool. Neither this mechanism nor the thickness of the mantle allows a good fixation of the tibial baseplate.
Limitations
The current meta-analysis has several limitations: first, there is a high heterogeneity because of differences in cementing technique, tourniquet pressure, time of tourniquet use, and the brand of bone cement. This heterogeneity may influence the reliability of results. So, we used a random-effects model for all analyses. Second, the depth of cement mantle was assessed in the simple post-op X-ray; many factors could affect the outcomes and the analysis of the thickness of the mantle. Third, only the cement mantle of the tibial component was analyzed. It is difficult to assess the femoral component cement mantle thickness on a lateral fluoroscopic radiograph because of the medial and lateral condyles’ overlay. However, as both tibia and femur were prepared and cemented simultaneously in a similar fashion intraoperatively, analysis of the tibial component alone is sufficient. Third, there are no worldwide uniform guidelines for performing total knee arthroplasty. Different surgical techniques (such as the selection of approach, anesthesia methods, patellar resurfacing, and type of prosthesis) were used in the individual studies. Lastly, although it has been shown that increased cement mantle thickness improved implant stability, our study only evaluates cement mantle thickness and does not assess the association of the thickness with long-term TKA implant survivorship or longevity. Further studies assessing the association of this thickness with long-term outcomes are necessary.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CIs:
-
Confidence intervals
- RCTs:
-
Randomized controlled trials
- NRSIs:
-
Non-randomized studies of interventions
- RR:
-
Risk ratio
- OR:
-
Odds ratio
- VMD:
-
Weighted mean difference
- TKA:
-
Total knee arthroplasty
- BMI:
-
Body mass index
- MCVT:
-
Muscular calf vein thrombosis
- DVT:
-
Deep vein thrombosis
References
Bert JM, McShane M. Is it necessary to cement the tibial stem in cemented total knee arthroplasty? Clin Orthop Relat Res. 1998;356:73–8. https://doi.org/10.1097/00003086-199811000-00012.
Cawley DT, Kelly N, McGarry JP, Shannon FJ. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J. 2013;95-b(3):295–300.
Hofmann AA, Goldberg TD, Tanner AM, Cook TM. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty. 2006;21(3):353–7. https://doi.org/10.1016/j.arth.2005.06.012.
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13.
Peters CL, Craig MA, Mohr RA, Bachus KN. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res. 2003;409:158–68. https://doi.org/10.1097/01.blo.0000058638.94987.20.
Walker PS, Soudry M, Ewald FC, McVickar H. Control of cement penetration in total knee arthroplasty. Clin Orthop Relat Res. 1984;185:155–64.
Pfitzner T, von Roth P, Voerkelius N, Mayr H, Perka C, Hube R. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):96–101. https://doi.org/10.1007/s00167-014-3341-6.
Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1121–30. https://doi.org/10.1007/s00167-010-1342-7.
Gao P, Li H, Bai Z, Zhang P. Effect of not using tourniquet during TKA on early prosthesis stability and knee function. Chin J Bone Joint Injury. 2019;34(12):1294–6.
Touzopoulos P, Ververidis A, Mpogiatzis C, Chatzigiannakis A, Drosos GI. The use of tourniquet may influence the cement mantle thickness under the tibial implant during total knee arthroplasty. Eur J Orthop Surg Traumatol. 2019;29(4):869–75. https://doi.org/10.1007/s00590-019-02369-8.
Gapinski ZA, Yee EJ, Kraus KR, Deckard ER, Meneghini RM. The effect of tourniquet use and sterile carbon dioxide gas bone preparation on cement penetration in primary total knee arthroplasty. J Arthroplasty. 2019;34(8):1634–9. https://doi.org/10.1016/j.arth.2019.03.050.
Hegde V, Bracey DN, Johnson RM, Dennis DA, Jennings JM. Tourniquet use improves cement penetration and reduces radiolucent line progression at 5 years after total knee arthroplasty. J Arthroplasty. 2021;36(1):48–75.
Jawhar A, Stetzelberger V, Kollowa K, Obertacke U. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2071–81. https://doi.org/10.1007/s00167-018-5330-7.
Ozkunt O, Sariyilmaz K, Gemalmaz HC, Dikici F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: a prospective randomized study of 3 methods. Medicine (Baltimore). 2018;97(4):e9668. https://doi.org/10.1097/MD.0000000000009668.
Vertullo CJ, Nagarajan M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg (Hong Kong). 2017;25(1):2309499016684323.
Herndon CL, Grosso MJ, Sarpong NO, Shah RP, Geller JA, Cooper HJ. Tibial cement mantle thickness is not affected by tourniquetless total knee arthroplasty when performed with tranexamic acid. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1526–31. https://doi.org/10.1007/s00167-019-05559-3.
Xie X, Yue C, Huang Z, Kang P, Zhou Z, Yang J, Shen B, Pei F. Total knee arthroplasty with or without tourniquet:a randomized controlled trial. Orthop J China. 2017;25(17):1572–6.
Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. https://doi.org/10.1016/j.ijsu.2010.02.007.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Zhou J, Dou W, Oouyang H, Chu W. The effect of not using tourniquet in total knee arthroplasty. Chin Rural Med. 2018;25(23):10–11+13.
Maistrelli GL, Antonelli L, Fornasier V, Mahomed N. Cement penetration with pulsed lavage versus syringe irrigation in total knee arthroplasty. Clin Orthop Relat Res. 1995;312:261–5.
Yang J, Wei L, Zhang J, Huang X. The efect of the tourniquet on cement mantle thicknes in total kne arthroplasty. Chongqing Med. 2017;46(06):782–5.
Janssen D, Mann KA, Verdonschot N. Micro-mechanical modeling of the cement-bone interface: the effect of friction, morphology and material properties on the micromechanical response. J Biomech. 2008;41(15):3158–63. https://doi.org/10.1016/j.jbiomech.2008.08.020.
Schlegel UJ, Bishop NE, Püschel K, Morlock MM, Nagel K. Comparison of different cement application techniques for tibial component fixation in TKA. Int Orthop. 2015;39(1):47–54. https://doi.org/10.1007/s00264-014-2468-x.
Ejaz A, Laursen AC, Jakobsen T, Rasmussen S, Nielsen PT, Laursen MB. Absence of a tourniquet does not affect fixation of cemented TKA: a randomized RSA study of 70 patients. J Arthroplasty. 2015;30(12):2128–32. https://doi.org/10.1016/j.arth.2015.05.058.
Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S, Nielsen PT. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85(4):422–6. https://doi.org/10.3109/17453674.2014.931197.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5. https://doi.org/10.2106/00004623-200704000-00012.
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–8. https://doi.org/10.1097/00003086-200111000-00041.
Molt M, Harsten A, Toksvig-Larsen S. The effect of tourniquet use on fixation quality in cemented total knee arthroplasty a prospective randomized clinical controlled RSA trial. Knee. 2014;21(2):396–401. https://doi.org/10.1016/j.knee.2013.10.008.
Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013;95(5):385–92. https://doi.org/10.2106/JBJS.L.00206.
Kheir MM, Ziemba-Davis M, Dilley JE, Hood MJ Jr, Meneghini RM. Tourniquetless total knee arthroplasty with modern perioperative protocols decreases pain and opioid consumption in women. J Arthroplasty. 2018;33(11):3455–9. https://doi.org/10.1016/j.arth.2018.06.038.
Baumann CA, Baumann JR, Bozynski CC, Stoker AM, Stannard JP, Cook JL. Comparison of techniques for preimplantation treatment of osteochondral allograft bone. J Knee Surg. 2019;32(1):97–104. https://doi.org/10.1055/s-0038-1636834.
Meyer MA, McCarthy MA, Gitelis ME, Poland SG, Urita A, Chubinskaya S, Yanke AB, Cole BJ. Effectiveness of lavage techniques in removing immunogenic elements from osteochondral allografts. Cartilage. 2017;8(4):369–73. https://doi.org/10.1177/1947603516681132.
Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE. Does tourniquet use in tka affect recovery of lower extremity strength and function? A randomized trial. Clin Orthop Relat Res. 2016;474(1):69–77. https://doi.org/10.1007/s11999-015-4393-8.
Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR. Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty. 2015;30(12):2311–4. https://doi.org/10.1016/j.arth.2015.05.049.
Majkowski RS, Bannister GC, Miles AW. The effect of bleeding on the cement-bone interface. An experimental study. Clin Orthop Relat Res. 1994;299:293–7.
Zhang W, Liu A, Hu D, Tan Y, Al-Aidaros M, Pan Z. Effects of the timing of tourniquet release in cemented total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2014;9(1):125–35. https://doi.org/10.1186/s13018-014-0125-0.
Cai DF, Fan QH, Zhong HH, Peng S, Song H. The effects of tourniquet use on blood loss in primary total knee arthroplasty for patients with osteoarthritis: a meta-analysis. J Orthop Surg Res. 2019;14(1):348–56. https://doi.org/10.1186/s13018-019-1422-4.
Lu C, Song M, Chen J, Li C, Lin W, Ye G, Wu G, Li A, Cai Y, Wu H, Liu W, Xu X. Does tourniquet use affect the periprosthetic bone cement penetration in total knee arthroplasty? A meta-analysis. J Orthop Surg Res. 2020;15(1):602–8. https://doi.org/10.1186/s13018-020-02106-6.
Zan P, Li G. Releasing of tourniquet before wound closure or not in total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty. 2015;30(7):1154. https://doi.org/10.1016/j.arth.2015.01.048.
Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID. Blood loss with knee joint replacement. J R Coll Surg Edinb. 1981;26(5):295–7.
Pattison E, Protheroe K, Pringle RM, Kennedy AC, Dick WC. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis. 1973;32(6):582–4. https://doi.org/10.1136/ard.32.6.582.
Jawhar A, Skeirek D, Stetzelberger V, Obertacke U. Influence of the tourniquet on pain and function in total knee arthroplasty: a systematic review and meta-analysis. Z Orthop Unfall. 2020;158(6):630–40. https://doi.org/10.1055/a-0983-3808.
Jiang FZ, Zhong HM, Hong YC, Zhao GF. Use of a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Sci. 2015;20(1):110–23. https://doi.org/10.1007/s00776-014-0664-6.
Mori N, Kimura S, Onodera T, Iwasaki N, Nakagawa I, Masuda T. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: a prospective, randomized study. Knee. 2016;23(5):887–9. https://doi.org/10.1016/j.knee.2016.02.007.
Tie K, Hu D, Qi Y, Wang H, Chen L. Effects of tourniquet release on total knee arthroplasty. Orthopedics. 2016;39(4):e642–50. https://doi.org/10.3928/01477447-20160606-03.
Wang K, Ni S, Li Z, Zhong Q, Li R, Li H, Ke Y, Lin J. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2849–57. https://doi.org/10.1007/s00167-015-3964-2.
Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. Timing of tourniquet release in total knee arthroplasty: a meta-analysis. Medicine (Baltimore). 2017;96(17):e6786. https://doi.org/10.1097/MD.0000000000006786.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Changjiao Sun, Xu Cai, and Yonggang Zhou: conceptualization and data curation; formal analysis, roles/writing—original draft; writing—review and editing. Xin Yang, Qi Ma, and Yu Peng: data collection, investigation, and methodology. Xiaofei Zhang: resources and software. Xu Cai and Yanggang Zhou: (co-corresponding author): supervised the whole study. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, C., Yang, X., Zhang, X. et al. The impact of tourniquet on tibial bone cement penetration in different zones in primary total knee arthroplasty: a meta-analysis. J Orthop Surg Res 16, 198 (2021). https://doi.org/10.1186/s13018-021-02345-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02345-1