Abstract
Background
Pancreatic head cancer patients who undergo pancreatoduodenectomy (PD) often experience disease recurrence, frequently associated with a positive margin status (R1). Total mesopancreas excision (TMpE) has emerged as a potential approach to increase surgical radicality and minimize locoregional recurrence. However, its effectiveness and safety remain under evaluation.
Methods
We conducted a systematic review and meta-analysis to synthesize current evidence on TMpE outcomes. A systematic search of MEDLINE, EMBASE, Cochrane, and Web of Science databases was conducted up to March 2024 to identify studies comparing TMpE with standard pancreatoduodenectomy (sPD). The risk ratio (RR) or mean difference (MD) was pooled using a random effects model.
Results
From 452 studies identified, 9 studies with a total of 738 patients were included, with 361 (49%) undergoing TMpE. TMpE significantly improved the R0 resection rate (RR 1.24; 95% CI 1.11–1.38; P < 0.05), reduced blood loss (MD -143.70 ml; 95% CI -247.92, -39.49; P < 0.05), and increased lymph node harvest (MD 7.27 nodes; 95% CI 4.81, 9.73; P < 0.05). No significant differences were observed in hospital stay, postoperative complications, or mortality between TMpE and sPD. TMpE also significantly reduced overall recurrence (RR 0.53; 95% CI 0.35–0.81; P < 0.05) and local recurrence (RR 0.39; 95% CI 0.24–0.63; P < 0.05). Additionally, the risk of pancreatic fistula was lower in the TMpE group (RR 0.66; 95% CI 0.52–0.85; P < 0.05).
Conclusion
Total mesopancreas excision significantly increases the R0 resection rate and reduces locoregional recurrence while maintaining an acceptable safety profile when compared with standard pancreatoduodenectomy. Further prospective randomized studies are warranted to determine the optimal surgical approach for total mesopancreatic resection.
Similar content being viewed by others
Introduction
Pancreatic cancer is the seventh leading cause of cancer death worldwide, accounting for almost as many deaths annually as new cases, and its increasing incidence is attributed to rising risk factors such as obesity, diabetes, and alcohol consumption [1,2,3]. Currently, surgery is the cornerstone and curative option for treating pancreatic adenocarcinoma (PDAC), aiming for margin-negative resection (R0) [4,5,6]. However, even patients undergoing curative treatment exhibit high recurrence rates ranging from 59.7 to 91.1%, which has been associated with a positive margin status (R1) [7, 8]. Since its initial description in the early 20th century, pancreatoduodenectomy (PD), the standard surgical approach for treating PDAC located in the head of the pancreas, has undergone numerous modifications to improve oncological outcomes [9,10,11,12]. Although advancements in surgical techniques and the development of minimally invasive approaches have been made, achieving R0 resection remains limited to less than 50% of patients with PDAC [13]. Furthermore, aggressive extended resection aimed at improving resectability and radicality (R0 resection rates) has shown no survival benefits in clinical trials, encompassing paraaortic lymph node dissection and superior mesenteric artery (SMA) nerve plexus dissection for PDAC in the pancreatic head [14, 15].
Within this context, total mesopancreas excision (TMpE), coupled with circumferential lymphadenectomy, has emerged as a potential approach to minimize R1 resection and locoregional recurrence [16,17,18]. The mesopancreas, alternatively referred to as the “pancreatic head plexus”, “retroportal lamina” or “mesopancreatoduodenum”, encompasses retropancreatic tissue, including adipose tissue, peripheral nerves and plexuses, and vascular structures, constituting a controversial and debated anatomical entity [19,20,21]. The mesopancreatic resection margin, yielding the retroperitoneal, uncinate, posterior, and portal vein groove margins, has been identified as the primary site for R1 resection due to neoplastic invasion of neurovascular and lymphatic tissues [22,23,24,25]. Therefore, total mesopancreatic excision (“en bloc mesopancreatic resection”) has been suggested to increase the clearance of peripancreatic retroperitoneal tissue, improving oncological outcomes [26, 27].
Currently, there is limited evidence regarding the effectiveness and safety of total mesopancreatic excision (TMpE), compounded by a lack of randomized controlled trials. Therefore, we conducted a systematic review and meta-analysis to comprehensively assess the oncological outcomes associated with TMpE and to determine whether increased radicality is accompanied by manageable postoperative complications.
Materials and methods
This systematic review and meta-analysis were performed in accordance with the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines [28]. The protocol for this review was registered in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42024551679).
Search strategy and selection criteria
A systematic digital search was conducted across the MEDLINE, EMBASE, Cochrane (CENTRAL) and Web of Science databases up to March 2023. The search utilized terms related to mesopancreatic excision: “MesoPancreatoduodenum” OR “Mesopancreatoduodenum” OR “Mesopancreas” OR “Retroportal lamina” OR “Retropancreatic lamina” OR “Mesopancreatic excision” OR “Mesopancreas excision” OR “pancreatic head plexus”. The references from all included studies and previous systematic reviews were also searched manually for any additional studies. Two investigators (L.F. and J.S.) independently reviewed the titles and abstracts for eligibility and discussed them with a senior investigator in case of disagreement. The full text, supplementary material, online appendices, and reference lists of each eligible study were examined to confirm adherence to the inclusion criteria and to identify any additional relevant studies. Any disagreements were resolved through discussion with other reviewers to achieve consensus.
The inclusion criteria in this systematic review were restricted to studies that met all the following eligibility criteria: (1) were randomized trials or nonrandomized cohorts; (2) compared total mesopancreatic excision (“en bloc resection”) with sPD; and (3) enrolled patients with PDAC who underwent pancreatoduodenectomy (Whipple procedure). In addition, studies were included only if they reported any of the clinical outcomes of interest. We excluded studies with (1) no control group; (2) case reports, literature reviews, editorials, comments, or letters; or (3) available only in the abstract format.
Data extraction and quality assessment
A comprehensive data extraction process was implemented, covering the number of patients, median age, body mass index (BMI), ASA score, mesopancreatic definition, and surgical technique. The oncological outcomes were the achievement of R0 margins, number of lymph nodes harvested (LNH), locoregional recurrence, and disease-free survival (DFS). Surgical outcomes included procedure duration and length of hospitalization. Postoperative pancreatic fistula (POPF) was defined according to the International Study Group on Pancreatic Fistula [29], and adverse events were classified using the Clavien‒Dindo grading system [30].
The Newcastle‒Ottawa Scale [31] (NOS) was used in this meta-analysis to evaluate the quality of nonrandomized trials. This scale includes Representativeness of the Exposed Cohort, Selection of the Non-Exposed Cohort, Ascertainment of Exposure, Outcome Not Present at Start, Assessment of Outcome, Adequate Follow-Up Length, and Adequacy of Follow-Up. Scores were classified as follows: 7–9 indicated a low risk of bias, 4–6 indicated a moderate risk, and scores below 4 indicated a high risk of bias.
Statistical analysis and data synthesis
The risk ratios (RRs) with 95% confidence intervals (CIs) were pooled using a random-effects model to compare treatment effects for categorical endpoints. Pooled mean differences (MDs) were employed to synthesize data regarding continuous endpoints. The Cochran Q test and I2 statistics were used to assess heterogeneity; P values less than 0.10 and I2 > 25% were considered significant for heterogeneity [32]. When necessary, means were estimated from medians and interquartile intervals with the method described by Luo et al. [33]. A leave-one-out sensitivity analysis was performed to evaluate the influence of individual studies on the overall results of the meta-analysis [34]. Furthermore, the extracted data from the studies were systematically organized into data tables and graphics and were critically reviewed. Review Manager 5.4 (Cochrane Centre, The Cochrane Collaboration, Denmark) and R-studio were used for statistical analysis. Publication bias was investigated by funnel plot analysis of point estimates according to study weights. Egger’s test was used to assess funnel plot asymmetry by performing a linear regression of the log risk ratio against the inverse standard error [35].
Results
Baseline characteristics of cohorts evaluating TMpE
We identified 452 studies through a database search strategy. After excluding duplicates and unrelated studies, 149 studies were fully evaluated. Overall, 738 patients were included from 9 studies, 361 (49%) of whom underwent mesopancreatic resection. The characteristics of the included studies are detailed in Table 1. Overlapping cohorts were identified between Kawabata 2012 and Kawabata 2016 [22, 38], as well as between Quero 2020 and Quero 2021 [36, 37], and a sensitivity analysis encompassing those with longer follow-up periods was performed. The study designs ranged from two studies with propensity score matching [36, 37] but overlapping populations, one prospective cohort study [26] and six retrospective studies [22, 38,39,40,41, 42]; Table 2.
Baseline characteristics, including median age, number of patients and sex, were presented proportionally between TMpE and control group across all studies (Table 1). No neoadjuvant therapy was reported for any patient. Furthermore, studies that described the tumor size (mm) and of ASA Score presented similar values for patients undergoing TMpE and sPD. Nevertheless, some studies had a subtle disproportion between treatment groups regarding TNM staging, as a higher proportion of TNM stage II patients in the control group in Kawabata et al. [38], and a higher number of stage III patients in Kawabata et al. [22]; (Table S2). These subtle baseline differences could contribute to observed heterogeneity in the outcomes. Mesopancreas definition presented similar aspects across studies, encompassing blood vessels, lymphogenic structures, nerve fibers and locoregional lymph nodes posterior to pancreas (Table S2; Fig. 1).
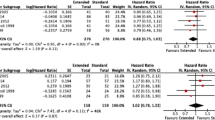
Surgical and oncological outcomes related to TMpE compared to those related to standard PD
The R0 resection rate was significantly greater in the TMpE group than in the standard pancreatoduodenectomy (sPD) group (RR 1.24; 95% CI 1.11–1.38; P < 0.05; Fig. 2A). The mean difference in blood loss was significantly lower in the TMpE group than in the sPD group (MD -143.70 ml; 95% CI -247.92, -39.49; P < 0.05). The average number of lymph nodes harvested was significantly greater in the TMpE group (MD 7.27 nodes; 95% CI 4.81, 9.73; P < 0.05; Fig. 2C). No significant differences were detected between the groups for hospital stay (MD -6.13 days; 95% CI -12.28, 0.03; P = 0.05), postoperative complications (RR 1.07; 95% CI 0.86–1.33; P = 0.55), or postoperative mortality (RR 0.64; 95% CI 0.23–1.82; P = 0.40). There was no significant difference in the reoperation rate between the two groups (RR 0.74; 95% CI 0.29–1.90; P = 0.40) or in the operative time (MD -6.86 min; 95% CI 0.29.69, 15.97; P = 0.56)
Forest plots comparing TMpE with standard PD regarding the R0 resection rate, local recurrence rate and number of lymph nodes harvested. Forest plots of the risk ratios of (a) R0 resection, (b) local recurrence, and (c) number of lymph nodes harvested. Squares are the effect sizes of the individual studies; diamonds are the summarized effect sizes; horizontal lines are the upper and lower borders of the 95% confidence intervals; p values > 0.05 are considered to indicate statistical significance
Forest plots comparing TMpE with standard PD regarding B/C pancreatic fistula, delayed gastric emptying and postoperative diarrhea. Forest plots of the risk ratios of (A) B/C pancreatic fistula, (B) delayed gastric emptying and (C) postoperative diarrhea. Squares are the effect sizes of the individual studies; diamonds are the summarized effect sizes; horizontal lines are the upper and lower borders of the 95% confidence intervals; p values > 0.05 are considered to indicate statistical significance
The recurrence and local recurrence rates were significantly lower in the TMpE group than in the sPD group (RR 0.53; 95% CI 0.35–0.81; P < 0.05, Fig. 2B) and (RR 0.39; 95% CI 0.24–0.63; P < 0.05), respectively. No significant difference was observed in the administration of adjuvant chemotherapy between the groups analyzed (RR 1.18; 95% CI 0.83–1.86; P = 0.36). The exclusion of studies with overlapping cohorts yielded consistent findings, with the risk of R0 resection remaining significantly elevated (RR 1.21; 95% CI 1.08–1.36; P < 0.05). A sensitivity analysis removing studies with overlapping populations for the outcomes of recurrence rate and local recurrence also demonstrated consistent results (supplementary files).
Safety of TMpE compared to sPD
The risk of pancreatic fistula was significantly lower in the TMpE group than in the sPD group (RR 0.66; 95% CI 0.52–0.85; P < 0.05). There were no significant differences between the groups for the risk of complications classified as Clavien‒Dindo ≥ III (RR 0.82; 95% CI 0.56–1.19; P = 0.29), delayed gastric emptying (RR 0.64; 95% CI 0.40–1.04; P = 0.07, Fig. 3B) or diarrhea (RR 1.59; 95% CI 0.95–2.66; P = 0.08, Fig. 3C). Sensitivity analysis, employing the leave-one-out approach, revealed minimal fluctuations in risk ratios (RRs) upon exclusion of individual studies. For instance, in the pooled results regarding pancreatic fistula, the RR ranged only from 0.63 to 0.69 across exclusions, with consistently low heterogeneity observed. Furthermore, a sensitivity analysis that removed studies with overlapping populations demonstrated results consistent with the main findings for pancreatic fistula outcome (RR 0.63; 95% CI 0.47–0.84; P < 0.05).
Quality assessment and publication bias
The funnel plot exhibited a symmetrical distribution of studies, with comparable weights converging toward the pooled treatment effect size as study sizes increased. Due to the limited number of studies available for comparison, Egger’s test was not applicable. Evaluation using the Newcastle‒Ottawa assessment revealed that most studies demonstrated a low risk of bias. Nonetheless, some studies exhibited moderate bias, primarily attributed to the absence of statements regarding patient follow-up and inadequate reporting of essential baseline patient characteristics.
Discussion
In this systematic review and pooled analysis of 9 studies, we evaluated the efficacy and safety of total mesopancreatic excision in pancreatoduodenectomy. The key findings of our comprehensive analysis were as follows: (1) TMpE was associated with a greater rate of R0 resection and lymph node harvesting than was standard PD; (2) patients who underwent TMpE experienced a lower rate of locoregional recurrence, suggesting improved oncological outcomes; (3) the duration of surgery was similar between TMpE and sPD; and (4) TMpE was linked to a decreased risk of pancreatic fistula, and there were no significant differences in postoperative delayed gastric emptying between the groups. These findings suggest the efficacy of TMpE in achieving better oncological control while maintaining an adequate safety profile.
The term ‘resection of mesopancreas’ was first introduced by Gockel et al. as an analogy to the mesorectum and the technique of total mesorectal excision, which is known to increase local control after rectal cancer resection [18, 43, 44]. Positioned adjacent to major vascular structures such as the SMA, the mesopancreas harbors a critical neurovascular plexus and lymph nodes involved in the spread of pancreatic cancer [21, 45–47] Initial case series evaluating the results of TMpE revealed an R0 resection rate exceeding 60%, with mesopancreatic tumor invasion identified in the majority of cases [24, 26, 48].
In a propensity score-matched (PSM) study, Quero et al. compared 60 sPD patients to 60 PD patients with TMpE, which yielded more harvested lymph nodes (19.8 ± 7.6 vs. 10.1 ± 5.1; p < 0.01), less local tumor recurrence (26.8% vs. 55.5%; p = 0.002), and better disease-free survival (22.3% vs. 14.8%; p = 0.04) with mesopancreatic excision [36]. Interestingly, in this PSM analysis TMpE was associated with a concomitant reduction of local (p = 0.002) and distant (p = 0.03) recurrence, while distant metastasis as the only site of recurrence were similar between groups. These findings are consistent with those of Aimoto et al. and Kawabata et al. [38, 40]. Our meta-analysis revealed a similar benefit of TMpE in terms of local recurrence and harvested lymph nodes.
Different surgical techniques have been evaluated to achieve surgical radicality and mesopancreatic resection [49]. Inoue et al. classified mesopancreatic dissection in PD patients into four levels. Level I is a standard approach without lymphadenectomy and is suitable for treating less aggressive pathologies, while level II involves ‘en bloc’ mesopancreas excision, lymphadenectomy, and soft tissue removal, which are suitable for treating tumors distant from the SMA and patients with compromised status. Level III entails removal of the nerve plexus around the pancreas head and hemicircumferential removal of the right and posterior nerve plexus around the SMA, while for tumors abutting the SMA up to 180° or more, extended level 3 involves complete circumferential removal of the periarterial plexus to ensure horizontal margins [42, 50]. Notably, the integration of these advancements in surgical techniques with minimally invasive approaches and robotic surgery has significantly contributed to improving outcomes in mesopancreatic resection, enhancing radicality and safety [51,52,53]. A prospective study evaluating the surgical feasibility of robotic TMpE revealed an increased R0 rate with level III resection compared with that with level II or I resection (93.8% vs. 72.2%, p < 0.001) and decreased blood loss compared with that with open level III PD [54].
The ‘triangle operation’ approach was further explored for the excision of the mesopancreas, defining its anatomical boundaries as an inverted triangle with the apex at the origins of the celiac trunk (CT), hepatic artery, and SMA and the base at the posterior face of the superior mesenteric vein and portal vein [24, 55]. Another option that has been commonly adopted is the artery-first approach, which involves early control and dissection at the SMA margin at the initial stage of resection to identify arterial tumor infiltration, assess resectability, promote adequate clearance of the SMA, perform radical lymphadenectomy, and minimize bleeding by ligation of the inferior pancreaticoduodenal artery (IPDA) [56,57,58]. In fact, the optimal mesopancreatic excision surgical technique remains under evaluation. Mahmoud et al. conducted a study comparing the artery-first approach with the conventional ‘triangle operation’ for TMpE and concluded that both methods presented comparable operative times, blood loss and postoperative morbidity [59]. Furthermore, some studies have evaluated the incorporation of the Cattell-Braasch-Valdoni maneuver (intestinal derotation) to facilitate mesopancreatic resection, which seems to simplify the procedure anatomy and reduce the operative time [60,61,62]. Currently, there is an ongoing randomized controlled trial (MAPLE-PD trial) in which a mesenteric artery-first approach is compared with conventional TMpE [63].
Resectability is a crucial consideration in pancreatic surgery, but it must be balanced with surgical safety [50]. Mesopancreatic excision has been associated with an acceptable rate of pancreatic fistula, a critical complication of PD [26, 29, 64]. In the prospective cohort conducted by Xu et al., the rate of POPF was 30.2% in patients who underwent sPD, while the rate of POPF in patients who underwent TMpE was 25.9%. Our pooled results indicate a decreased risk of this complication with TMpE. These findings could be attributed to improved vascular resection with TMpE, which has been previously associated as a protective factor for POPF in meta-analysis [65, 66]. However, TMpE is associated with increased postoperative diarrhea in some studies, likely due to neuronal damage, and with a greater incidence in patients undergoing level III mesopancreatic excision [16, 54]. Severe or intractable diarrhea is a major postoperative concern in PD patients and is a possible cause of adjuvant chemotherapy failure, which is an important prognostic factor [67,68,69]. Notably, most patients who undergo TMpE have diarrhea controlled with antidiarrheal opioids, and studies have suggested that preemptive antidiarrheals effectively prevent intractable diarrhea [70]. Despite the risk of postoperative diarrhea, aggressive dissection of the nerve plexus may be justified for achieving optimal oncological outcomes. Furthermore, the TMpE technique did not increase the risk of perioperative bleeding, operative mortality, or hospitalization time.
Although our review provides valuable insights into the efficacy and safety of TMpE, it is important to acknowledge certain limitations. The heterogeneity among the included studies, such as variations in patient populations and surgical techniques, may have influenced the pooled results. To address this variability, a leave-one-out analysis was conducted to explore the impact of individual studies on pooled estimates. Additionally, the retrospective nature of the studies and the potential of selection bias should be considered in the interpretation. Furthermore, the limited availability of long-term follow-up data restricts the ability to assess the durability of oncological outcomes. The strengths of this review include the use of a systematic approach and the inclusion of a diverse range of studies to capture the available evidence. By synthesizing data from multiple studies, we were able to offer valuable insights into the comparative efficacy and safety of TMpE versus sPD. Furthermore, our review highlights the potential benefits of TMpE in achieving improved oncological outcomes, such as higher rates of R0 resection and lower locoregional recurrence rates, while also addressing the associated risks. Overall, these findings provide valuable guidance for surgeons in decision-making regarding surgical radicality in pancreatic cancer management, but further prospective randomized studies are warranted to determine the optimal surgical approach.
Conclusion
Total mesopancreas excision significantly increases the R0 resection rate and reduces locoregional recurrence while maintaining an acceptable safety profile when compared with standard pancreatoduodenectomy. Further prospective randomized studies are warranted to determine the optimal surgical approach for total mesopancreatic resection.
Data availability
No datasets were generated or analysed during the current study.
References
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, et al. Global burden of 5 major types of gastrointestinal Cancer. Gastroenterology. 2020;159(1):335–e34915.
He R, Jiang W, Wang C, Li X, Zhou W. Global burden of pancreatic cancer attributable to metabolic risks from 1990 to 2019, with projections of mortality to 2030. BMC Public Health. 2024;24(1):456.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Conroy T, Pfeiffer P, Vilgrain V, Lamarca A, Seufferlein T, O’Reilly EM, et al. Pancreatic cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34(11):987–1002.
Okusaka T, Nakamura M, Yoshida M, Kitano M, Ito Y, Mizuno N, et al. Clinical practice guidelines for pancreatic Cancer 2022 from the Japan Pancreas Society: a synopsis. Int J Clin Oncol. 2023;28(4):493–511.
Springfeld C, Ferrone CR, Katz MHG, Philip PA, Hong TS, Hackert T, et al. Neoadjuvant therapy for pancreatic cancer. Nat Rev Clin Oncol. 2023;20(5):318–37.
Groot VP, Rezaee N, Wu W, Cameron JL, Fishman EK, Hruban RH, et al. Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg. 2018;267(5):936–45.
Tanaka M, Mihaljevic AL, Probst P, Heckler M, Klaiber U, Heger U, et al. Meta-analysis of recurrence pattern after resection for pancreatic cancer. Br J Surg. 2019;106(12):1590–601.
Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB. 2011;13(6):377–84.
Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, et al. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 2012;152(3):S56–63.
Whipple AO, Parsons WB, Mullins CR, TEEATMENT OF CARCINOMA OF THE AMPULLA OF VATER. Ann Surg. 1935;102(4):763–79.
Des S. L. Pancreatectomy et specialement de la pancreatectomie cephalique. Rev Chir. 1908;37:335–85.
Augustinus S, Schafrat PJM, Janssen BV, Bonsing BA, Brosens LAA, Busch OR, et al. Nationwide impact of centralization, Neoadjuvant Therapy, minimally invasive surgery, and standardized Pathology reporting on R0 resection and overall survival in Pancreatoduodenectomy for pancreatic Cancer. Ann Surg Oncol. 2023;30(8):5051–60.
Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, et al. A prospective randomized controlled study comparing outcomes of Standard Resection and Extended Resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic Head Cancer. Ann Surg. 2014;259(4):656–64.
Nimura Y, Nagino M, Takao S, Takada T, Miyazaki K, Kawarada Y, et al. Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepato-Biliary-Pancreat Sci. 2012;19(3):230–41.
Fernandes EDSM, Strobel O, Girão C, Moraes-Junior JMA, Torres OJM. What do surgeons need to know about the mesopancreas. Langenbecks Arch Surg. 2021;406(8):2621–32.
Peparini N, Mesopancreas. A boundless structure, namely the rationale for dissection of the paraaortic area in pancreaticoduodenectomy for pancreatic head carcinoma. World J Gastroenterol WJG. 2015;21(10):2865–70.
Gockel I, Domeyer M, Wolloscheck T, Konerding MA, Junginger T. Resection of the mesopancreas (RMP): a new surgical classification of a known anatomical space. World J Surg Oncol. 2007;5:44.
Peparini N, Chirletti P. Mesopancreas: a boundless structure, namely R1 risk in pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2013;39(12):1303–8.
Chowdappa R, Challa VR. Mesopancreas in Pancreatic Cancer: where do we stand – review of literature. Indian J Surg Oncol. 2015;6(1):69–74.
Yi SQ, Nagakawa Y, Ren K, Dai YD, Zhang M, Chen JF, et al. The mesopancreas and pancreatic head plexus: morphological, developmental, and clinical perspectives. Surg Radiol Anat. 2020;42(12):1501–8.
Kawabata Y, Tanaka T, Ishikawa N, Hayashi H, Tajima Y. Modified total meso-pancreatoduodenum excision with pancreaticoduodenectomy as a mesopancreatic plane surgery in borderline resectable pancreatic cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2016;42(5):698–705.
Ramia JM, De-la-Plaza R, Manuel-Vazquez A, Lopez-Marcano A, Morales R. Systematic review of the mesopancreas: concept and clinical implications. Clin Transl Oncol off Publ Fed Span Oncol Soc Natl Cancer Inst Mex. 2018;20(11):1385–91.
Adham M, Singhirunnusorn J. Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2012;38(4):340–5.
Kalisvaart M, Broadhurst D, Marcon F, Pande R, Schlegel A, Sutcliffe R, et al. Recurrence patterns of pancreatic cancer after pancreatoduodenectomy: systematic review and a single-centre retrospective study. HPB. 2020;22(9):1240–9.
Xu J, Tian X, Chen Y, Ma Y, Liu C, Tian L, et al. Total mesopancreas excision for the treatment of pancreatic head cancer. J Cancer. 2017;8(17):3575–84.
Gaedcke J, Gunawan B, Grade M, Szöke R, Liersch T, Becker H, et al. The mesopancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg. 2010;395(4):451–8.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161(3):584–91.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Ottawa Hospital Research Institute [Internet]. [cited 2024 May 24]. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–805.
Willis BH, Riley RD. Measuring the statistical validity of summary meta-analysis and meta-regression results for use in clinical practice. Stat Med. 2017;36(21):3283–301.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Quero G, Fiorillo C, Menghi R, Cina C, Galiandro F, Longo F, et al. Total mesopancreas excision for periampullary malignancy: a single-center propensity score-matched comparison of long-term outcomes. Langenbecks Arch Surg. 2020;405(3):303–12.
Quero G, Fiorillo C, De Sio D, Laterza V, Menghi R, Cina C, et al. The role of mesopancreas excision for ampullary carcinomas: a single center propensity-score matched analysis. HPB. 2021;23(10):1557–64.
Kawabata Y, Tanaka T, Nishi T, Monma H, Yano S, Tajima Y. Appraisal of a total meso-pancreatoduodenum excision with pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2012;38(7):574–9.
Shrestha S, Dahal R, Maharjan N, Kandel B, Lakhey PJ. Perioperative outcomes of systematic mesopancreas dissection for pancreatic and Periampullary Carcinoma at a Tertiary Referral Center from a low Middle-Income Country. Cureus. 2023;15(7):e42461.
Aimoto T, Mizutani S, Kawano Y, Matsushita A, Yamashita N, Suzuki H, et al. Left posterior approach pancreaticoduodenectomy with total mesopancreas excision and circumferential lymphadenectomy around the superior mesenteric artery for pancreatic head carcinoma. J Nippon Med Sch Nippon Ika Daigaku Zasshi. 2013;80(6):438–45.
Du F, Wang X, Lin H, Zhao X. Pancreaticoduodenectomy with arterial Approach of Total Mesenteric Resection of the pancreas for pancreatic Head Cancer. Gastroenterol Res. 2019;12(5):256–62.
Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, et al. Pancreatoduodenectomy with systematic mesopancreas Dissection using a supracolic anterior artery-first Approach. Ann Surg. 2015;262(6):1092–101.
Peparini N, Caronna R, Chirletti P. The ‘meso’ of the rectum and the ‘meso’ of the pancreas: similar terms but distinct concepts in surgical oncology. Hepatobiliary Pancreat Dis Int HBPD INT. 2015;14(5):548–51.
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet Lond Engl. 2009;373(9666):821–8.
Cees DB. The Mesopancreas Dissection - A New Surgical Paradigm: An Anatomical Reflection of Surgical and Prognostic Importance? 2015.
Borghi F, Gattolin A, Garbossa D, Bogliatto F, Garavoglia M, Levi AC. Embryologic bases of extended radical resection in pancreatic cancer. Arch Surg Chic Ill 1960. 1998;133(3):297–301.
Strobel O, Neoptolemos J, Jäger D, Büchler MW. Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol. 2019;16(1):11–26.
Moldovan SC, Moldovan AM, Dumitraæcu T, Andrei S, Popescu I. The advantages of retropancreatic vascular dissection for pancreatic head cancer with portal/superior mesenteric vein invasion: posterior approach pancreatico-duodenectomy technique and the mesopancreas theory. Chir Buchar Rom. 1990. 2012;107(5):571–8.
Hank T, Leonhardt CS, Klaiber U, Strobel O. Intraoperative strategies and techniques to achieve surgical radicality in pancreatic cancer. Eur Surg. 2024;56(3):86–92.
Inoue Y, Saiura A, Oba A, Kawakatsu S, Ono Y, Sato T, et al. Optimal extent of Superior Mesenteric Artery Dissection during Pancreaticoduodenectomy for Pancreatic Cancer: Balancing Surgical and Oncological Safety. J Gastrointest Surg off J Soc Surg Aliment Tract. 2019;23(7):1373–83.
Ielpo B, d’Addetta MV, Anselmo A, Rosso E, de Blasi V, Sanchez-Velazquez P, et al. Levels of robotic mesopancreas Dissection according to malignancy and vascular anatomy: what surgeons need to know. Ann Surg Oncol. 2024;31(3):1916–8.
Machado MA, Mattos BV, Lobo Filho MM, Makdissi F. Mesopancreas Excision and Triangle Operation during Robotic Pancreatoduodenectomy. Ann Surg Oncol. 2021;28(13):8330–4.
Bhandare MS, Varty GP, Chaudhari VA, Shrikhande SV. Robotic pancreaticoduodenectomy with ‘SMA-First Approach (posterior and right medial)’ and ‘Triangle Operation’. Ann Surg Oncol. 2024;31(6):4112.
Shyr BU, Shyr BS, Chen SC, Shyr YM, Wang SE. Mesopancreas level 3 dissection in robotic pancreaticoduodenectomy. Surgery. 2021;169(2):362–8.
Hackert T, Strobel O, Michalski CW, Mihaljevic AL, Mehrabi A, Müller-Stich B, et al. The TRIANGLE operation - radical surgery after neoadjuvant treatment for advanced pancreatic cancer: a single arm observational study. HPB. 2017;19(11):1001–7.
Wang X, Luo Q, Li S, Wu Y, Zhen T, Zhu F, et al. A comparative study of the ‘superior mesenteric artery first’ approach versus the conventional approach in short-term and long-term outcomes in patients with pancreatic ductal adenocarcinoma undergoing laparoscopic pancreaticoduodenectomy. Surg Endosc. 2023;37(12):9326–38.
Ironside N, Barreto SG, Loveday B, Shrikhande SV, Windsor JA, Pandanaboyana S. Meta-analysis of an artery-first approach versus standard pancreatoduodenectomy on perioperative outcomes and survival. Br J Surg. 2018;105(6):628–36.
Weitz J, Rahbari N, Koch M, Büchler MW. The ‘artery first’ approach for resection of pancreatic head cancer. J Am Coll Surg. 2010;210(2):e1–4.
Mahmoud MA, Reyad HA, Korany M. Comparative study between artery-first approach and classic approach in pancreatoduodenectomy with mesopancreas dissection. Egypt J Surg. 2021;40(3):959.
Sugiyama M, Suzuki Y, Nakazato T, Yokoyama M, Kogure M, Abe N, et al. Intestinal derotation procedure for facilitating pancreatoduodenectomy. Surgery. 2016;159(5):1325–32.
Akita M, Maeda E, Nishimura T, Abe K, Kozuki A, Yokoyama K, et al. Anatomical change of SMV branches after the Cattell Braasch maneuver facilitates safe resection around the uncinated process in pancreatoduodenectomy. BMC Surg. 2021;21(1):341.
Akita M, Yamasaki N, Miyake T, Mimura K, Maeda E, Nishimura T, et al. Cattell-Braasch maneuver facilitates the artery-first approach and complete excision of the mesopancreas for pancreatoduodenectomy. J Surg Oncol. 2020;121(7):1126–31.
Hirono S, Kawai M, Okada K ichi, Fujii T, Sho M, Satoi S et al. MAPLE-PD trial (Mesenteric Approach vs. Conventional Approach for Pancreatic Cancer during Pancreaticoduodenectomy): study protocol for a multicenter randomized controlled trial of 354 patients with pancreatic ductal adenocarcinoma. Trials. 2018;19(1):613.
Nguyen TK, Nguyen HH, Luong TH, Dang KK, Le VD, Tran DD, et al. Pancreaticoduodenectomy with superior mesenteric artery first-approach combined total meso-pancreas excision for periampullary malignancies: a high-volume single-center experience with short-term outcomes. Ann Hepato-Biliary-Pancreat Surg. 2024;28(1):59–69.
Zhang B, Yuan Q, Li S et al. Risk factors of clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy: A systematic review and meta-analysis. Medicine (Baltimore). 2022;101(26):e29757. Published 2022 Jul 1. https://doi.org/10.1097/MD.0000000000029757
Kamarajah SK, Bundred JR, Lin A, et al. Systematic review and meta-analysis of factors associated with post-operative pancreatic fistula following pancreatoduodenectomy. ANZ J Surg. 2021;91(5):810–21. https://doi.org/10.1111/ans.16408.
Kimura W. Strategies for the treatment of invasive ductal carcinoma of the pancreas and how to achieve zero mortality for pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg. 2008;15(3):270–7.
Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet Lond Engl. 2016;388(10041):248–57.
Yamada S, Satoi S, Takami H, Yamamoto T, Yoshioka I, Sonohara F, et al. Multicenter randomized phase II trial of prophylactic right-half dissection of superior mesenteric artery nerve plexus in pancreatoduodenectomy for pancreatic head cancer. Ann Gastroenterol Surg. 2021;5(1):111–8.
Kuroki N, Ono Y, Sato T, Inoue Y, Oba A, Ito H, et al. Long-term outcome of patients with postoperative refractory diarrhea after tailored nerve plexus dissection around the major visceral arteries during pancreatoduodenectomy for pancreatic Cancer. World J Surg. 2022;46(5):1172–82.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
L.F.L.S. and M.B.O. contributed to the study concepts. The study design was developed by L.F.L.S. and J.S.A.M. Data acquisition was performed by L.F.C.A., L.H.P., and L.F.L.S. Quality control of data and algorithms was ensured by L.H.P. and L.F.C.A. Data analysis and interpretation were conducted by L.F.C.A. and L.F.L.S. L.F.C.A. also carried out the statistical analysis. Manuscript preparation was undertaken by L.F.L.S., L.F.C.A., J.S.A.M., and M.S.A. Manuscript editing was performed by L.F.L.S., M.B.O., R.O.A., and J.R. Finally, M.S.A., M.B.O., R.O.A., and J.R. reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable as this study is a systematic review and meta-analysis of previously published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
da Silva, L.F.L., Belotto, M., de Almeida, L.F.C. et al. Radicality and safety of total mesopancreatic excision in pancreatoduodenectomy: a systematic review and meta-analysis. World J Surg Onc 22, 217 (2024). https://doi.org/10.1186/s12957-024-03495-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-024-03495-2