Abstract
Background
Brominated flame retardants (BFRs) are widely utilized to mitigate the flammability of various materials. Previous studies have revealed the impact of BFRs exposure on hormonal disruption and bone metabolism which are closely related to periodontitis. However, it remains unknown the potential relationship between BFRs and periodontitis. This study aimed to explore the association between BFRs exposure and periodontitis in US adults.
Methods
The data analyzed in this study were obtained from the National Health and Nutrition Examination Survey (NHANES) 2009–2014. Twelve serum BFRs were quantified using isotope dilution gas chromatography high-resolution mass spectrometry. Univariable and multivariable logistic regression was employed to evaluate the association between serum BFRs and periodontitis. Bayesian kernel machine regression (BKMR) analyses were utilized to assess the association between mixtures of BFRs and periodontitis.
Results
A total of 3311 eligible participants were included. Serum BFRs (PBDE-47, PBDE-99, and PBDE-154) were significantly associated with periodontitis, and the odds ratios (ORs) and corresponding 95% confidence intervals(CIs) were 1.15(1.01,1.29), 1.10(1.01,1.20), and 1.12(1.01,1.25), respectively. Notably, these three BFRs were also significantly associated with the severity of periodontitis. Additionally, the BKMR model revealed a significant association between the mixture of all twelve BFRs and periodontitis.
Conclusions
This preliminary study suggests a significant association between specific serum BFRs (PBDE-47, PBDE-99, and PBDE-154) and periodontitis and its severity. Further prospective and experimental studies are warranted to validate our findings.
Similar content being viewed by others
Introduction
Periodontitis, a multifactorial chronic inflammatory disease, is widely recognized as one of the most prevalent diseases in humans. A microbial infection of a susceptible host is the primary cause of periodontitis, which leads to the reciprocal interaction between a dysbiotic biofilm and the host immune-inflammatory reactions. Its etiology involves a variety of causative factors, such as genetic predisposition, socio-economic status, level of education, and economic environment, as well as uncontrolled diabetes mellitus and lifestyle choices [1,2,3]. The primary manifestations of this condition encompass the loss of alveolar bone and periodontal tissue support. With a global prevalence ranging from 45 to 50%, periodontitis ranks as the sixth most common human disease [4]. If left untreated, it can lead to tooth loss, impaired masticatory function, compromised nutritional status, and diminished quality of life [3]. Consequently, investigating the risk factors associated with periodontitis is of paramount importance. While recent years have witnessed a surge in research on risk factors related to diet and lifestyle behaviors [5,6,7,8,9], studies exploring the impact of environmental substances in daily life remain scarce [10, 11].
Brominated flame retardants (BFRs), specifically poly brominated diphenyl ethers (PBDEs) and poly brominated biphenyls (PBBs), which account for about 21% of the total production of BFRs [12, 13], are widely used in plastics, electrical equipment, foams, and furniture products to improve their fire resistance [14]. The utilization of flame retardants has witnessed a significant rise due to the implementation of stringent fire safety regulations by numerous countries [15]. Whereas most BFRs lack covalent bonds with the host polymer and readily penetrate into the indoor environment, humans can be widely exposed to BFRs through inhalation of dust and air, dietary intake and dermal contact [16]. Its high solubility in adipose tissue renders it easily assimilated by organisms and progressively accumulated within the food chain. Several studies have shown that BFR has thyrotoxicity, neurotoxicity, and reproductive and developmental toxicity, affecting human health [17,18,19]. Despite certain flame retardants being banned, the persistent nature of these chemicals in certain consumer goods and their ability to accumulate in biological systems imply that humans worldwide will continue to be exposed to them for several decades [13, 20].
Previous studies have indicated that elevated exposure to PBDEs can adversely affect bone metabolism and mineral density [21]. Given that alveolar bone loss is an important feature of periodontitis, these findings suggest a potential link between PBDE exposure and periodontal health. Moreover, BFRs, including PBDEs, are known endocrine disruptors that can alter the levels of sex hormones such as estradiol and testosterone [22]. Since both bone metabolism disorders and hormonal imbalances have been associated with periodontitis [23,24,25], it is plausible to hypothesize a correlation between BFRs exposure and periodontitis. Despite this rationale, the relationship between BFRs and periodontitis has not been examined in prior studies. Therefore, the present study seeks to address this research gap by investigating the association between exposure to individual or mixed BFRs and periodontitis in a nationally representative population using data from the National Health and Nutrition Examination Survey (NHANES). This study will contribute valuable insights into the prevention of periodontitis from the perspective of environmental pollutant exposure.
Methods
Study population
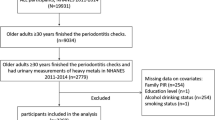
NHANES, a program for evaluating the health and nutritional well-being of both adults and children in the United States, includes a series of cross-sectional nationally representative health examination surveys. In this study, we selected publicly accessible data originating from three distinct cycles of NHANES, namely 2009–2010, 2011–2012, and 2013–2014. These particular cycles were chosen due to their inclusion of comprehensive full-mouth periodontal examinations, with the exception of the third molars. The intricate process employed to identify eligible participants is elucidated in Fig. 1. The inclusion criteria for this study were as follows: (1) participants aged 30 years or older with complete periodontal examination data, and (2) participants with complete serum BFRs examination data. 3357 participants with incomplete periodontal examinations and 72 participants with incomplete serum BFRs data were excluded. The final intersection of periodontal examination data and serum BFRs data, 3311 participants, were included in the subsequent analyses.
BFRs detection
The comprehensive protocols for detecting BFRs can be accessed on the official NHANES website. In summary, serum samples were subjected to processing using a Gilson 215 liquid processor. A total of nine serum BFRs, namely 2, 4, 4´-Tribromodiphenyl ether(PBDE-28), 2, 2´, 4, 4´-Tetrabromodiphenyl ether(PBDE-47), 2, 2´, 3, 4, 4´-Tentabromodiphenyl ether (PBDE-85), 2, 2´, 4, 4´, 5-Pentabromodiphenyl ether (PBDE-99), 2, 2´, 4, 4´, 6-Pentabromodiphenyl ether (PBDE-100), 2, 2´, 4, 4´, 5, 5´-Hexabromodiphenyl ether (PBDE-153), 2, 2´, 4, 4´, 5, 6´-Hexabromodiphenyl ether (PBDE-154), Decabromodiphenyl ether (PBDE-209), 2, 2´, 4, 4´, 5, 5´-Hexabromobiphenyl (PBB-153), were quantified utilizing automated liquid/liquid extraction followed by sample clean-up. Isotope dilution gas chromatography high resolution mass spectrometry (GC/IDHRMS) was subsequently employed to determine the target analytes. The Supplementary Table 1 presents the minimum detection limits for the nine BFRs.
Periodontal examination
The study utilized measurements of probing pocket depth (PPD) and clinical attachment level (CAL) to diagnose periodontitis. Participants were classified into four categories of periodontitis severity based on their PPD and CAL measurements, as well as the CDC/APP definition [26]. Specifically, mild periodontitis was defined as having ≥ 2 interdental sites with AL ≥ 3 mm but < 4 mm, ≥ 2 interdental sites with PD ≥ 4 mm but < 5 mm (not on the same tooth), or one site with PD ≥ 5 mm. Moderate periodontitis was defined as having ≥ 2 interdental sites with AL ≥ 4 mm but < 6 mm, or ≥ 2 interdental sites with PD ≥ 5 mm (not on the same tooth). Severe periodontitis was defined as having ≥ 2 interdental sites with AL ≥ 6 mm (not on the same tooth), and ≥ 1 interdental sites with PD ≥ 5 mm. Participants who did not fall into any of these categories were classified as having no periodontitis [27].
Covariates
The study also took into account potential confounding variables, including age, gender, smoking, daily alcohol consumption, marital status, education, household poverty-to-income ratio (PIR), body mass index (BMI), hypertension, and diabetes. Smoking status was categorized as current smoker, former smoker (participants who do not smoke now but have smoked more than 100 cigarettes in their lifetime), or never smoker, while marital status was categorized as married, never married, or unmarried but with a partner. Educational attainment was grouped into high school and below, college, and college and above. Age, BMI, daily alcohol consumption, and household PIR were analyzed as continuous variables. Hypertension was defined as self-reported use of anti-hypertensive medication or having a measured systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg [28]. Diabetes was defined as self-reported diagnosis or medication use, or having Hemoglobin A1c (HbA1c) ≥ 6.5%, fasting blood glucose ≥ 126 mg/dL, or blood glucose ≥ 200 mg/dL on an oral glucose tolerance test [29].
Data analysis
To account for the intricate survey design employed in the NHANES, appropriate sampling weights were utilized during the analysis of the collected data. Descriptive analyses involved the representation of continuous variables as medians (25th and 75th percentiles) due to their non-normal distribution, while categorical variables were expressed as frequencies (percentages). The general characteristics of participants with and without periodontitis were compared using either the chi-square test (for categorical variables) or the Mann–Whitney U test (for continuous variables). The Mann–Whitney U test was used to compare serum BFRs levels between participants with and without periodontitis, while the Kruskal–Wallis test and the Dunn’s post hoc test from the 'FSA' package were used to compare differences between different severities of periodontitis. Weighted binary logistic regression models were employed to calculate the odds ratios (ORs) and corresponding 95% confidence intervals (CIs) in order to assess the potential association between BFRs and periodontitis. Model 1 represented the unadjusted model, while Model 2 accounted for various confounding factors such as age, sex, smoking, alcohol consumption, education, marital status, household PIR, BMI, hypertension, and diabetes status.
To assess the relationship between BFRs mixtures and periodontitis, the Bayesian kernel machine regression model (BKMR) based on the "bkmr" package were used. This approach took into consideration the potential synergistic, non-additive, and non-linear effects that may arise from multiple environmental exposures. The model included ten covariates, namely age, gender, smoking, alcohol consumption, education, marital status, household PIR, BMI, hypertension, and diabetes status. Missing values of the covariates were imputed using the multiple interpolation method implemented in the "mice" package. After fitting the final model using a Markov chain Monte Carlo (MCMC) sampler for 10,000 iterations, the posterior inclusion probability (PIP) was estimated for each chemical, and exposure-outcome function estimates were generated. Furthermore, an overall mixed-effects analysis was conducted.
In addition, a restricted cubic spline (RCS) was plotted using the "RCS" package to explore the non-linear relationship between BFRs and periodontitis. Participants were categorized into four groups based on the severity of periodontitis (no periodontitis, mild, moderate, and severe), and an unordered polynomial logistic regression model was utilized to investigate the correlation between serum BFRs levels and the severity of periodontitis, considering the unsatisfactory results of parallelism testing.
Mediation analyses were further performed using the “mediation” package to explore the potential mediating roles of sex hormones (including estradiol and testosterone) as well as skull bone mineral density in the relationship between BFRs levels and periodontitis. In the sensitivity analyses, we firstly re-analyzed the relationship between BFRs and periodontitis based on the 2018 new periodontal classification [30]. Moreover, considering that the number of teeth may be a confounding factor influencing the classification of periodontal status, we additionally adjusted the number of missing teeth based on the Model 2. In addition, we also excluded the cancer population to further assess the robustness of the results. All statistical analyses were performed with a significance level of 0.05 using R version 4.2.1.
Results
Table 1 presents an overview of the study population, highlighting various characteristics. Notably, age, alcohol consumption, and household poverty income ratio exhibited statistically significant differences (P < 0.05) between individuals with periodontitis and those without. Conversely, there was no significant difference in BMI between the two groups (P = 0.102). Moreover, categorical variables such as gender, marital status, race, smoking, hypertension, and diabetes demonstrated significant differences between the periodontitis and non-periodontitis groups. In addition, differences in the characteristics of participants with different severities of periodontitis are presented in Supplementary Table 2.
The distribution of nine BFRs is visually represented in Fig. 2 and Supplementary Table 3. Among these BFRs, the serum levels of eight (PBDE-28, PBDE-47, PBDE-85, PBDE-99, PBDE-100, PBDE-154, PBDE-209, and PBB-153) exhibited statistically significant differences between the periodontitis and non-periodontitis groups. Furthermore, the differences in the concentrations of these BFRs among different severities of periodontitis are presented in Supplementary Table 4.
Univariable logistic analyses were conducted to assess the association between serum concentrations of various BFRs and periodontitis. PBDE-28, PBDE-47, PBDE-85, PBDE-99, PBDE-100, PBDE-154, and PBB-153 displayed significant associations with periodontitis (all P < 0.05). After adjusting for potential confounders, PBDE-47 (OR = 1.15, 95%CI: 1.01–1.29), PBDE-99 (OR = 1.10, 95%CI: 1.01–1.20), and PBDE-154 (OR = 1.12, 95%CI: 1.01–1.25) maintained significant associations with periodontitis (Table 2). RCS analysis results, as depicted in Fig. 3, demonstrated a non-linear relationship between serum concentrations of PBDE-47, PBDE-99, PBDE-154, and the odds ratio (OR) for periodontitis (P for non-linear < 0.05).
Figure 4A illustrates the varying degrees of significant correlation among six BFRs (PBDE-28, PBDE-47, PBDE-85, PBDE-99, PBDE-100, and PBDE-154). Additionally, the BKMR model revealed a significant correlation between the mixtures of all nine BFRs and periodontitis (Fig. 4B). Notably, PBDE-154 emerged as the primary contributor to the overall mixture effect (Fig. 4C). Supplementary Table 5 presents the PIP values, indicating the significance of each BFR's association with periodontitis. A PIP value closer to 1 signifies a stronger association. In this regard, PBDE-154 exhibited the highest significance (PIP = 0.979).
When participants were categorized into four groups based on the severity of periodontitis (no periodontitis, mild periodontitis, moderate periodontitis, and severe periodontitis), unordered polynomial logistic regression models revealed significant correlations between three BFRs (PBDE-47, PBDE-99, and PBDE-154) and the severity of periodontitis (Supplementary Table 6). Notably, PBDE-154 exhibited the strongest associations with the severity of periodontitis, with ORs and 95%CIs of 1.22 (1.08, 1.38) for mild periodontitis, 1.12 (1.02, 1.22) for moderate periodontitis, and 1.18 (1.07, 1.31) for severe periodontitis.
Furthermore, we observed that sex hormones partially mediated the relationship between BFRs levels and periodontitis. Specifically, testosterone explained 3.17%, 4.38%, and 4.40% of the relationships involving PBDE47, PBDE99, and PBDE154, respectively, with respect to periodontitis, whereas estradiol mediated 4.27%, 6.08%, and 4.17% of the associations, respectively (Supplementary Fig. 1). We also found a significant mediation role of skull bone mineral density in the relationship between BFR levels and periodontitis (Supplementary Fig. 2). Additionally, to further confirm the robustness of the results, we further performed a series of sensitivity analyses by excluding the cancer population, using the 2018 new periodontal classification, or additionally adjusted the number of missing teeth, respectively. Generally consistent results were yielded and are shown in Supplementary Tables 7–9.
Discussion
In this extensive cross-sectional study utilizing a nationally representative sample, our findings have demonstrated a positive correlation between specific BFRs (PBDE-47, PBDE-99, and PBDE-154) and periodontitis. Furthermore, we have observed a significant relationship between these three BFRs and the severity of periodontitis. The application of the BKMR model has also provided support for a significant association between twelve mixtures of BFRs and periodontitis.
Although there is no direct epidemiological or laboratory evidence to explain the observed association between BFRs and periodontitis, several previous studies have indicated that elevated exposure to BFRs can adversely affect bone metabolism and bone density [21, 31]. In the present study, we observed a significant mediating effect of skull density on the relationship between certain BFRs and periodontitis. Since periodontitis involves the destruction of alveolar bone supporting the teeth, it is plausible that BFRs could accelerate this process by disrupting normal bone turnover mechanisms. Additionally, BFRs have the potential to disrupt the levels of sex hormones in the body by affecting the hypothalamic-pituitary–gonadal axis [22, 32]. Given the role of hormones such as estrogen in modulating immune responses and inflammation [33], it is possible that BFRs could influence the progression of periodontitis by dysregulating these hormonal pathways. These findings provided valuable insights for the underlying mechanism of BFRs and periodontitis, but the specific mechanisms remain to be elucidated through subsequent experimental studies.
Furthermore, our findings highlight the importance of considering mixtures of BFRs when assessing their health impacts. It is important to acknowledge that BFRs are not commonly found in isolation within the environment, and there may exist interactions among them. Employing the BKMR model, this study revealed a positive correlation between mixtures of BFRs and periodontitis. The use of the BKMR model allowed us to explore the combined effects of multiple BFRs on periodontitis risk, providing a more comprehensive understanding of how complex chemical mixtures may interact to influence disease outcomes [34]. This approach is particularly relevant given the ubiquitous presence of multiple BFRs in the environment and their potential for cumulative exposure [35].
The findings from the unordered polynomial logistic regression analysis indicated a positive correlation between BFRs and the severity of periodontitis. Several in vitro studies have provided evidence of BFRs' ability to enhance the production of pro-inflammatory cytokines, including IL-1β, IL-6, and TNF-α [36,37,38]. These inflammatory factors have been previously associated with the pathogenesis of periodontitis [39, 40]. Therefore, it is plausible to suggest that exposure to BFRs with pro-inflammatory properties may contribute to the development of periodontitis by activating a biologically plausible mechanism.
This study possesses several strengths. Firstly, a comprehensive approach was employed to investigate the correlation between individual and mixed BFRs and periodontitis, utilizing a nationally representative large sample. Secondly, this study is the first epidemiological study to explore the relationship between BFRs and periodontitis. Thirdly, the possible mediating effects of sex hormones and skull density on the relationship between BFRs and periodontitis were further investigated. The findings of this study will provide valuable insights for future prospective and mechanistic studies.
Nonetheless, it is crucial to acknowledge the limitations of this study. Firstly, due to its cross-sectional nature, establishing causality is challenging, and only epidemiological associations can be ascertained. Secondly, the possibility of bias arising from residual and unmeasured confounding factors, as well as measurement errors, cannot be entirely ruled out. Nonetheless, the inclusion of E-values (refer to Supplementary Table 10) provides evidence that the observed associations are unlikely to be entirely explained by unmeasured confounders.
Conclusion
This study provides preliminary evidence indicating a positive correlation between specific BFRs (PBDE-47, PBDE-99, and PBDE-154) and periodontitis as well as its severity. These findings offer novel perspectives on the prevention of periodontitis through the lens of environmental exposure and contribute to the development of targeted public health policies aimed at reducing environmental risks and improving oral health outcomes. However, future studies should focus on conducting extensive prospective studies on larger scale samples and exploring the underlying mechanisms to confirm and strengthen our observations.
Availability of data and materials
The data that support the findings of this study are available in NHANES (National Health and Nutrition Examination Survey) at: https://www.cdc.gov/nchs/nhanes/index.htm .
Abbreviations
- BFRs:
-
Brominated flame retardants
- NHANES:
-
National Health and Nutrition Examination Survey
- BKMR:
-
Bayesian kernel machine regression
- ORs:
-
Odds ratios
- CIs:
-
Confidence intervals
- PBDEs:
-
Poly brominated diphenyl ethers
- PBBs:
-
Poly brominated biphenyls
- NCDC:
-
National Centers for Disease Control and Prevention
- PBDE-28:
-
2, 4, 4´-Tribromodiphenyl ether
- PBDE-47:
-
2, 2´, 4, 4´-Tetrabromodiphenyl ether
- PBDE-85:
-
2, 2´, 3, 4, 4´-Tentabromodiphenyl ether
- PBDE-99:
-
2, 2´, 4, 4´, 5-Pentabromodiphenyl ether
- PBDE-100:
-
2, 2´, 4, 4´, 6-Pentabromodiphenyl ether
- PBDE-153:
-
2, 2´, 4, 4´, 5, 5´-Hexabromodiphenyl ether
- PBDE-154:
-
2, 2´, 4, 4´, 5, 6´-Hexabromodiphenyl ether
- PBDE-209:
-
Decabromodiphenyl ether
- PBB-153:
-
2, 2´, 4, 4´, 5, 5´-Hexabromobiphenyl
- GC/IDHRMS:
-
Isotope dilution gas chromatography high resolution mass spectrometry
- PPD:
-
Probing pocket depth
- CAL:
-
Clinical attachment level
- CDC/APP:
-
Centers for Disease Control and Prevention/American Academy of Periodontology
- PIR:
-
Poverty-to-income ratio
- BMI:
-
Body mass index
- HbA1c:
-
Hemoglobin A1c
- MCMC:
-
Markov chain Monte Carlo
- PIP:
-
Posterior inclusion probability
- RCS:
-
Restricted cubic spline
References
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45(Suppl 20):S162-s170.
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS: Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. Journal of clinical periodontology 2020, 47 Suppl 22(Suppl 22):4–60.
Chapple IL, Bouchard P, Cagetti MG, Campus G, Carra MC, Cocco F, Nibali L, Hujoel P, Laine ML, Lingstrom P, et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44(Suppl 18):S39-s51.
Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 2014;93(11):1045–53.
Wright DM, McKenna G, Nugent A, Winning L, Linden GJ, Woodside JV. Association between diet and periodontitis: a cross-sectional study of 10,000 NHANES participants. Am J Clin Nutr. 2020;112(6):1485–91.
Leite FRM, Nascimento GG, Scheutz F, Lopez R. Effect of Smoking on Periodontitis: A Systematic Review and Meta-regression. Am J Prev Med. 2018;54(6):831–41.
Wu Y, Qiu Y, Wu Y, Deng Q, Yu Y, Yang H, Chen Q, He B, Yan F, Li Y, et al. Association between plasma trans fatty acids and chronic periodontitis: Results from a nationally representative cross-sectional survey. J Periodontol. 2023;94(8):976–85.
Chen Q, Ge R, Wu Y, Wu Y, Yang H, Yu Y, Deng Q, Qiu Y, He B, Yan F, et al. The associations of coffee consumption, coffee types, and caffeine metabolites with periodontitis: Results from NHANES 2009–2014. J Periodontol. 2024;95(8):778–88.
Wu Y, He B, Chen Q, Yu R, Wu Y, Yang H, Yu Y, Yan F, Li Y, Chen F. Association between Mediterranean diet and periodontitis among US adults: The mediating roles of obesity indicators. J Periodontal Res. 2023;59(1):32–41.
Wu Y, Yang H, Jin W, Wu Y, Yu Y, Chen Q, He B, Yan F, Li Y, Chen F. Association between polycyclic aromatic hydrocarbons and periodontitis: Results from a large population-based study. J Clin Periodontol. 2023;51(4):441–51.
Wu Y, Qiu Y, Wu Y, Li H, Yang H, Deng Q, He B, Yan F, Li Y, Chen F. Association of per- and polyfluoroalkyl substances (PFAS) with periodontitis: the mediating role of sex hormones. BMC Oral Health. 2024;24(1):243.
Han L, Wang Q. Associations of brominated flame retardants exposure with chronic obstructive pulmonary disease: A US population-based cross-sectional analysis. Front Public Health. 2023;11:1138811.
Feiteiro J, Mariana M, Cairrao E. Health toxicity effects of brominated flame retardants: From environmental to human exposure. Environ Pollut. 2021;285: 117475.
Sousa S, Maia ML, Pestana D, Teixeira D, Angelo-Dias M, Martins C, Borrego LM, Delerue-Matos C, Calhau C, Fernandes Domingues V, et al. Brominated flame retardants effect in MCF-7 cells: Impact on vitamin D pathway. J Steroid Biochem Mol Biol. 2022;219:106079.
de Wit CA, Herzke D, Vorkamp K. Brominated flame retardants in the Arctic environment–trends and new candidates. Sci Total Environ. 2010;408(15):2885–918.
Zuiderveen EAR, Slootweg JC, de Boer J. Novel brominated flame retardants - A review of their occurrence in indoor air, dust, consumer goods and food. Chemosphere. 2020;255: 126816.
Costa LG, de Laat R, Tagliaferri S, Pellacani C. A mechanistic view of polybrominated diphenyl ether (PBDE) developmental neurotoxicity. Toxicol Lett. 2014;230(2):282–94.
Wu Z, He C, Han W, Song J, Li H, Zhang Y, Jing X, Wu W. Exposure pathways, levels and toxicity of polybrominated diphenyl ethers in humans: A review. Environ Res. 2020;187: 109531.
Sarkar D, Singh SK. Inhibition of testicular steroidogenesis and impaired differentiation of Sertoli cells in peripubertal mice offspring following maternal exposure to BDE-209 during lactation suppress germ cell proliferation. Toxicol Lett. 2018;290:83–96.
Zota AR, Mitro SD, Robinson JF, Hamilton EG, Park JS, Parry E, Zoeller RT, Woodruff TJ. Polybrominated diphenyl ethers (PBDEs) and hydroxylated PBDE metabolites (OH-PBDEs) in maternal and fetal tissues, and associations with fetal cytochrome P450 gene expression. Environ Int. 2018;112:269–78.
Plourde SP, Moreau R, Letcher RJ, Verreault J: Is the bone tissue of ring-billed gulls breeding in a pollution hotspot in the St. Lawrence River, Canada, impacted by halogenated flame retardant exposure? Chemosphere 2013, 93(10):2333–2340.
Plunk EC, Richards SM. Endocrine-Disrupting Air Pollutants and Their Effects on the Hypothalamus-Pituitary-Gonadal Axis. Int J Mol Sci. 2020;21(23):9191.
Yu B, Wang CY: Osteoporosis and periodontal diseases – An update on their association and mechanistic links. Periodontology 2000 2022, 89(1):99–113.
Su X, Jin K, Zhou X, Zhang Z, Zhang C, Li Y, Yang M, Huang X, Xu S, Wei Q, et al. The association between sex hormones and periodontitis among American adults: A cross-sectional study. Front Endocrinol. 2023;14:1125819.
Penoni DC, Fidalgo TKS, Torres SR, Varela VM, Masterson D, Leão ATT, Maia LC. Bone Density and Clinical Periodontal Attachment in Postmenopausal Women: A Systematic Review and Meta-Analysis. J Dent Res. 2017;96(3):261–9.
Holtfreter B, Albandar JM, Dietrich T, Dye BA, Eaton KA, Eke PI, Papapanou PN, Kocher T. Joint EUUSAPEWG: Standards for reporting chronic periodontitis prevalence and severity in epidemiologic studies: Proposed standards from the Joint EU/USA Periodontal Epidemiology Working Group. J Clin Periodontol. 2015;42(5):407–12.
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the Case Definitions for Population-Based Surveillance of Periodontitis. J Periodontol. 2012;83(12):1449–54.
Li C, Shang S. Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014). Int J Environ Res Public Health. 2021;18(15):7867.
McClure ST, Schlechter H, Oh S, White K, Wu B, Pilla SJ, Maruthur NM, Yeh HC, Miller ER, Appel LJ. Dietary intake of adults with and without diabetes: results from NHANES 2013–2016. BMJ Open Diabetes Res Care. 2020;8(1): e001681.
Botelho J, Machado V, Proença L, Mendes JJ. The 2018 periodontitis case definition improves accuracy performance of full-mouth partial diagnostic protocols. Sci Rep. 2020;10(1):7093.
Bai T, Li X, Zhang H, Yang W, Lv C, Du X, Xu S, Zhao A, Xi Y. The association between brominated flame retardants exposure with bone mineral density in US adults: A cross-sectional study of the national health and nutrition examination survey (NHANES) 2005–2014. Environ Res. 2024;251(Pt 1): 118580.
Johnson PI, Stapleton HM, Mukherjee B, Hauser R, Meeker JD. Associations between brominated flame retardants in house dust and hormone levels in men. Sci Total Environ. 2013;445–446:177–84.
Straub RH. The complex role of estrogens in inflammation. Endocr Rev. 2007;28(5):521–74.
Bobb JF, Valeri L, Claus Henn B, Christiani DC, Wright RO, Mazumdar M, Godleski JJ, Coull BA. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics (Oxford, England). 2015;16(3):493–508.
Gouesse RJ, Plante I. Environmental Exposure to Brominated Flame Retardants: Unraveling Endocrine and Mammary Gland Effects That May Increase Disease Risk. Toxicological sciences : an official journal of the Society of Toxicology. 2022;186(2):190–207.
Wang X, Wei L, Zhu J, He B, Kong B, Xue Z, Jin X, Fu Z. Environmentally relevant doses of tetrabromobisphenol A (TBBPA) cause immunotoxicity in murine macrophages. Chemosphere. 2019;236: 124413.
Yasmin S, Whalen M. Flame retardants, hexabromocyclododecane (HCBD) and tetrabromobisphenol a (TBBPA), alter secretion of tumor necrosis factor alpha (TNFalpha) from human immune cells. Arch Toxicol. 2018;92(4):1483–94.
Anisuzzaman S, Whalen MM. Tetrabromobisphenol A and hexabromocyclododecane alter secretion of IL-1beta from human immune cells. J Immunotoxicol. 2016;13(3):403–16.
Deo V, Bhongade ML: Pathogenesis of periodontitis: role of cytokines in host response. Dent Today 2010, 29(9):60–62, 64–66; quiz 68–69.
Liukkonen J, Gursoy UK, Pussinen PJ, Suominen AL, Kononen E. Salivary Concentrations of Interleukin (IL)-1beta, IL-17A, and IL-23 Vary in Relation to Periodontal Status. J Periodontol. 2016;87(12):1484–91.
Acknowledgements
We appreciate the support of all authors and funding for this article.
Funding
This research is supported by the Jiangsu Health Commission Scientific Research Project (No. H2019033), and High-level Talents research Start-up Project of Fujian Medical University, Fujian, China (No. XRCZX2018001).
Author information
Authors and Affiliations
Contributions
Fa Chen and Yanfen Li were involved in the conceptualization and design of the study. Yanhong Pan and Qiansi Chen were responsible for drafting the manuscript and making substantial revisions. Yiming Yu and Qiansi Chen were involved in conducting statistical analyses. Zilin Liu, Bingqin Xie, Yu Huang and Han Yang were responsible for creating figures and tables. Baochang He and Fuhua Yan were involved in data collection and interpretation. All authors were involved in the critical revision of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The NCHS Research Ethics Review Board reviewed and approved NHANES, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pan, Y., Chen, Q., Yu, Y. et al. Association between brominated flame retardants (BFRs) and periodontitis: Results from a large population-based study. BMC Oral Health 24, 1025 (2024). https://doi.org/10.1186/s12903-024-04796-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04796-4