Abstract
Objective
The prevalence of type 2 diabetes mellitus (T2DM) and bone metabolism disorders increase with age. Diabetic kidney disease (DKD) is one of the most serious microvascular complications of T2DM, and bone metabolism disorders are closely linked to the occurrence of DKD. The relationship between bone turnover markers(BTMs) and the kidney disease in elderly patients with T2DM remains unclear. Therefore, this study aims to investigate the association between common BTMs and DKD in a large sample of elderly patients. The goal is to provide a basis for early identification of high-risk individuals for DKD among elderly T2DM patients from a bone metabolism perspective.
Methods
In this cross-sectional study, BTMs were collected from a cohort of 2,051 hospitalized Chinese patients. The relationships between 25-hydroxyvitamin D (25-OH-D), β-CrossLaps (β-CTX), osteocalcin (OSTEOC), intact parathyroid hormone (iPTH), and total type I collagen N-terminal propeptide (TP1NP), and DKD, as well as urinary albumin-to-creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) were analyzed using regression analysis and restrictive cubic spline (RCS) curves.
Results
Higher 25-OH-D levels were independently linked to a lower incidence of DKD and decreased UACR. The RCS curves showed a linear association of 25-OH-D and DKD, approaching the L-shape. β-CTX was independently and positively correlated with UACR. There is an independent positive correlation between OSTEOC and UACR and a negative correlation with eGFR. iPTH is independently and positively correlated with DKD incidence and UACR, and negatively correlated with eGFR. Additionally, the RCS curves showed a non-linear association of OSTEOC and iPTH and DKD, approaching the J-shape, and the point of inflection is 10.875 ng/L and 34.15 pg/mL respectively. There is an independent positive correlation between TP1NP and UACR incidence, and a negative correlation with eGFR. Risk estimates significantly increase with higher TP1NP levels in the RCS model.
Conclusion
BTMs are closely associated with kidney disease in elderly patients with T2DM. These discoveries potentially assist clinicians in establishing more preventive measures and targeted treatment strategies for elderly patients with T2DM.
Similar content being viewed by others
Introduction
As the population ages, the proportion of elderly individuals (aged ≥ 60) in China was approximately 17.3% in 2017. By 2050, this percentage is projected to exceed 30%, with more than 20% of the elderly population expected to suffer from diabetes, of which over 95% will be type 2 diabetes mellitus (T2DM) [1]. Chronic hyperglycemia has been observed to reduce osteoblast numbers, impair bone formation, slow bone mineralization, and enhance osteoclast activity, resulting in an imbalance in bone metabolism, particularly in elderly patients [2, 3]. Diabetic kidney disease (DKD) is a prevalent microvascular complication of diabetes mellitus [4]. The presence of DKD significantly complicates the management of diabetes in elderly patients and poses a serious threat to their health and mortality worldwide. Research indicates that bone metabolism disorders may be a risk factor for the development of kidney complications in T2DM [5]. Identifying potential bone metabolism markers related to incident DKD is essential for screening elderly populations with diabetes mellitus who are at high risk for DKD. It also aids in researching the mechanisms of DKD onset and benefits early intervention and correction of risk factors.
Osteoblasts form new bone, while osteoclasts resorb old bone to maintain bone structure integrity. The metabolites produced during this process are known as bone turnover markers (BTMs). Commonly assessed BTMs include 25-hydroxyvitamin D (25-OH-D), β-CrossLaps (β-CTX), osteocalcin (OSTEOC), intact parathyroid hormone (iPTH), and total type I collagen N-terminal propeptide (TP1NP). Previous studies have suggested that these bone metabolic indicators may be involved in the crosstalk between bone, islet, and adipose tissues [6,7,8,9] and may be associated with early renal damage in DKD [10, 11]. However, these findings remain controversial and inconclusive. Only four studies have reported the association between BTMs and the risk of DKD or eGFR and UACR [12,13,14,15]. Two studies showed that OSTEOC, TP1NP, and β-CTX levels negatively correlated with eGFR in diabetes patients (one did not differentiate between type 1 and type 2 disease) [13, 14]. Another study found that UACR was positively associated with OSTEOC, TP1NP, β-CTX and 25-OH-D in T2DM patients [15]. In contrast, one study indicated that serum concentrations of BTMs were not associated with the risks of DKD [12]. Notably, most of these studies are limited by small sample sizes and did not clarify the non-linear relationship between BTMs and DKD. Additionally, there are no studies investigating the relationship between BTMs and DKD in the elderly T2DM population currently.
The relationship between BTMs and the occurrence of kidney disease in elderly patients with T2DM remains unclear. Therefore, this study aims to investigate the association between these five common BTMs and kidney disease in a large sample of elderly patients with T2DM. The goal is to provide a basis for early identification of high-risk individuals for DKD among elderly T2DM patients from a bone metabolism perspective. This approach is beneficial for correcting bone metabolism disorders and, concurrently, slowing the progression of DKD, ultimately contributing to an improved quality of life for elderly individuals with diabetes.
Materials and methods
Study design and participants
A total of 2,987 individuals aged ≥ 60 years with T2DM admitted to the Guang’anmen Hospital from February 2017 to February 2022 were enrolled in this study. The flow chart of the study is shown in Fig. 1. T2DM was diagnosed according to the criteria established by the American Diabetes Association [16]. The exclusion criteria were as follows: (1)lacking BTMs results or medical history, (2)experiencing acute complications of diabetes, bone fractures, acute inflammation or infections, autoimmune diseases, or malignancies, (3)receiving steroid or thyroid hormone treatment, and (4)receiving hemodialysis or peritoneal dialysis treatment. Ultimately, 2,051 participants were included in the analysis. This retrospective study obtained approval from the Medical Ethics Committee of Guang’anmen Hospital, China Academy of Chinese Medical Sciences (2023-187-KY), and strictly adhered to the principles outlined in the Declaration of Helsinki.
Measurements
Information on sex, age, height, weight, duration of diabetes, systolic blood pressure(SBP), diastolic blood pressure(DBP), and medication use was extracted from electronic medical records using standardized questionnaires by the same trained personnel. The medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT-2 inhibitors, and GLP-1 analogues), and ACEI/ARB. Body mass index (BMI) was calculated as body weight (kg) divided by the square of height (m2). Levels of 25-OH-D, β-CTX, OSTEOC, iPTH, and TP1NP were assayed using electrochemiluminescence assays. Fasting plasma glucose (FPG), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), alanine transaminase (ALT), aspartate aminotransferase(AST), alkaline phosphatase (ALP), albumin (ALB), serum calcium, serum phosphorus, serum uric acid, serum creatinine, and hemoglobin were measured using an automated analyzer with standard methods. Urine albumin-to-creatinine ratio (UACR) was calculated from urine albumin and urine creatinine levels. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation designed for individuals of Asian origin. DKD was defined as persistent proteinuria and/or progressive renal insufficiency. In patients without other chronic kidney diseases, those with UACR ≥ 30 mg/g and/or eGFR < 60 mL/min per 1.73 m2 twice after three tests in 3 ~ 6 months were considered to have developed DKD, in accordance with the criteria set by the American Diabetes Association [17].
Statistical analysis
The current analysis was conducted using IBM SPSS Statistics (v 26), R (v 4.4.1), and Zstats (v1.0). Statistical significance was established at a two-sided P-value < 0.05. Continuous variables were presented as means ± standard deviation (SD) or medians ± interquartile range (IQR), while categorical variables were expressed as percentages (%). For the comparison of continuous variables, the nonparametric rank-sum test or Student’s t-test was used, and the Chi-square test was applied for categorical variables. BTMs levels were categorized into quartiles. Regression analysis was performed to identify associations between BTMs and DKD, UACR, and eGFR. The first quartile of BTMs was used as a reference in logistic regression. The associations were evaluated by a crude model 0 with no adjustments, a multivariable model 1 adjusted for age, sex, BMI, and duration of diabetes, and a multivariable model 2 adjusted for age, sex, BMI, duration of diabetes, SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications.and age and family history of diabetes. Data were summarized as odds ratios or beta coefficients with 95% confidence intervals (CIs). The association of BTMs with the incidence of DKD was further evaluated on a continuous scale with restrictive cubic spline (RCS) curves.
Results
The general and sociodemographic characteristics of the study participants are shown in Table 1. The final analysis included 2,051 diabetic participants. Among them, 1,267 participants (61.7%) were diagnosed without DKD (Non-DKD), while 784 participants (38.2%) were diagnosed with DKD. Compared to Non-DKD participants, those with DKD exhibited significantly higher values for age, the number of men, BMI, duration of diabetes, iPTH, FPG, HbA1c, TG, ALP, serum creatinine, serum uric acid, UACR, HbA1c, number of anti-diabetic agents and the number of ACEI/ARB (all P < 0.05). No differences were observed in DBP, β-CTX, TP1NP, TC, LDL, AST, serum phosphorus, or number of anti-osteoporosis drugs between the two groups. However, SBP, 25-OH-D, OSTEOC, HDL, ALT, ALB, hemoglobin, serum calcium, and eGFR were significantly lower in DKD patients compared to those without DKD (all P < 0.05).
We developed several models to evaluate the independent effects of BTMs on DKD, UACR, and eGFR. As presented in Table 2, elevated 25-OH-D levels were associated with a decreased likelihood of DKD, and reduced UACR without any adjustments. After controlling for various confounding variables in model 1 and model 2, the associations between 25-OH-D and the prevalence of DKD, as well as UACR, remained statistically significant. In these three models, β-CTX was positively associated with UACR, elevated OSTEOC levels were associated with increased UACR and reduced eGFR, and iPTH was positively associated with the likelihood of DKD in models 1 and 2, positively associated with UACR in all three models, and negatively associated with eGFR in all three models. TP1NP was positively associated with UACR in all three models and negatively associated with eGFR in models 1 and 2. Multifactor analysis revealed that 25-OH-D is an independent protective factor for DKD, potentially contributing to a decreased UACR, while iPTH is an independent risk factor for DKD, potentially contributing to increased UACR and decreased eGFR. In addition, β-CTX, OSTEOC, iPTH, and TP1NP were independently associated with elevated UACR. OSTEOC and TP1NP were identified as independent risk factors for eGFR.
We evaluated the associations between 25-OH-D quartile levels and DKD, UACR, and eGFR, as shown in Fig. 2. Elevated 25-OH-D quartile levels were significantly associated with a decreased prevalence of DKD and reduced UACR after adjusting for potential confounders. However, no significant associations were observed between 25-OH-D quartile levels and eGFR. Compared to participants in the first quartile of 25-OH-D levels, those in the highest quartile exhibited a significant 68% decrease in the odds of having DKD in model 0. These associations remained significant in both model 1 and model 2. Notably, in modes 1 and 2, the prevalence of DKD among participants in the highest 25-OH-D quartile showed a 66.8% decrease and a 53.1% decrease, respectively, compared to those in the first quartile. Furthermore, our findings revealed that, in these models, as 25-OH-D quartile levels gradually increased, UACR showed a decreasing trend. Compared with the lowest quartile, individuals in the highest quartile exhibited the lowest β for UACR in model 2.
The associations between 25-OH-D quartile levels and DKD, UACR, and eGFR. 0 The model was not adjusted. 1 The model was adjusted for age, sex, BMI, and duration of diabetes. 2 The model was adjusted for model 1and SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications, and the medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT-2 inhibitors, and GLP-1 analogues), and ACEI/ARB. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate
We evaluated the associations between β-CTX quartile levels and DKD, UACR, and eGFR, as shown in Fig. 3. No significant associations were observed between β-CTX quartile levels and the prevalence of DKD or UACR. However, elevated β-CTX quartile levels were found to be significantly associated with decreased eGFR. In these models, as β-CTX quartile levels increased, eGFR showed a decreasing trend after controlling for various confounding variables such as age, sex, BMI, duration of diabetes, SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, hemoglobin, serum calcium, serum phosphorus, serum uric acid and medications. Compared with the lowest quartile, individuals in the highest quartile exhibited the lowest β for eGFR in both model 2 and model 3.
The associations between β-CTX quartile levels and DKD, UACR, and eGFR. 0 The model was not adjusted. 1 The model was adjusted for age, sex, BMI, and duration of diabetes. 2 The model was adjusted for model 1and SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications, and the medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT−2 inhibitors, and GLP−1 analogues), and ACEI/ARB. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate
We evaluated the associations between OSTEOC quartile levels and DKD, UACR, and eGFR, as shown in Fig. 4. No significant associations were observed between OSTEOC quartile levels and the prevalence of DKD. However, elevated OSTEOC quartile levels were found to be significantly associated with increased UACR in models 0 and 1, and decreased eGFR in all three models. In these models, as OSTEOC quartile levels increased, UACR showed an increasing trend, while eGFR showed a decreasing trend. Compared to the lowest quartile, individuals in the highest quartile exhibited the highest β for UACR and lowest β for eGFR in all three models.
The associations between OSTEOC quartile levels and DKD, UACR, and eGFR. 0 The model was not adjusted. 1 The model was adjusted for age, sex, BMI, and duration of diabetes. 2 The model was adjusted for model 1and SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications, and the medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT−2 inhibitors, and GLP−1 analogues), and ACEI/ARB. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate
We evaluated the associations between iPTH quartile levels and DKD, UACR, and eGFR, as shown in Fig. 5. Compared to participants in the first quartile of iPTH levels, those in the highest quartile exhibited a significant 81.5% increase in the odds of having DKD in model 0. However, after adjusting for various varibles, the association between iPTH and the prevalence of DKD was not significant. Furthermore, elevated iPTH quartile levels were found to be significantly associated with a reduced eGFR after adjusting for potential confounders in all three models. Our findings revealed that, as iPTH quartile levels increased, eGFR showed a decreasing trend in all models. Compared to the lowest quartile, individuals in the highest quartile exhibited the lowest β for eGFR in all three models.
The associations between iPTH quartile levels and DKD, UACR, and eGFR. 0 The model was not adjusted. 1 The model was adjusted for age, sex, BMI, and duration of diabetes. 2 The model was adjusted for model 1and SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications, and the medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT−2 inhibitors, and GLP−1 analogues), and ACEI/ARB. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate
We evaluated the associations between TP1NP quartile levels and DKD, UACR, and eGFR, as shown in Fig. 6. No significant associations were observed between TP1NP quartile levels and the prevalence of DKD. However, elevated TP1NP quartile levels were found to be significantly associated with increased UACR and decreased eGFR in all three models. In these models, as TP1NP quartile levels increased, UACR showed an increasing trend, while eGFR showed a decreasing trend. Compared to the lowest quartile, individuals in the highest quartile exhibited the highest β for UACR and the lowest β for eGFR in all models.
The associations between TP1NP quartile levels and DKD, UACR, and eGFR. 0 The model was not adjusted. 1 The model was adjusted for age, sex, BMI, and duration of diabetes. 2 The model was adjusted for model 1and SBP, DBP, FPG, HbA1c, TC, TG, HDL, LDL, ALT, AST, ALP, Hemoglobin, Serum calcium, Serum phosphorus, Serum uric acid and medications, and the medications included anti-osteoporosis drugs (calcium, vitamin D, bisphosphonate, or other drugs), anti-diabetic agents (pioglitazone, SGLT−2 inhibitors, and GLP−1 analogues), and ACEI/ARB. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate
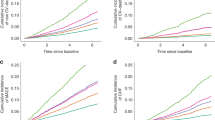
Figure 7 shows that the associations between 25-OH-D and TP1NP levels and the prevalence of DKD were linear in the adjusted RCS model. The risk estimates significantly decreased with increasing 25-OH-D levels, and the association approached the L-shape, while they significantly increased with rising TP1NP levels. β-CTX did not exhibit any independent effects on DKD in the multivariable model. Moreover, the RCS curves showed a non-linear association of OSTEOC and iPTH and DKD, approaching the J-shape, and the point of inflection is 10.875 ng/L and 34.15 pg/mL respectively. The risk estimates markedly increased when OSTEOC levels exceeded 10.875 ng/L and iPTH levels surpassed 34.15 pg/mL.
Adjusted RCS for BTMs and the prevalence of DKD. Adjusted for age, sex, BMI, and duration of diabetes. DKD Diabetic kidney disease, UACR Urine albumin to creatinine ratio, eGFR Estimated glomerular infiltration rate, 25-OH-D 25-hydroxyvitamin D, β-CTX β-CrossLaps, OSTEOC Osteocalcin, iPTH Intact parathyroid hormone, TP1NP Total type I collagen N-terminal propeptide
Discussion
We observed that 25-OH-D levels were significantly lower in patients with DKD compared to those without DKD. Elevated 25-OH-D levels were independently associated with a reduced incidence of DKD and a decrease in UACR. As 25-OH-D levels increased across quartiles, there was a trend of decreasing DKD incidence and UACR. After adjusting for confounding factors, the highest quartile of 25-OH-D demonstrated a significant 53.1% reduction in the prevalence of DKD compared to the first quartile. In the adjusted RCS model, the relationship between 25-OH-D levels and DKD prevalence was linear, approaching the L-shape, with risk estimates markedly decreasing as 25-OH-D levels increased. This suggests that higher levels of 25-OH-D may act as a protective factor against kidney complications in elderly patients with T2DM. These findings are consistent with previous findings [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37], although some studies have reported inconsistent conclusions [38,39,40,41,42,43,44,45]. The discrepancies in these findings may be attributed to differences in the populations studied, methodologies used, and the confounding factors controlled for. By dividing patients into pathological subgroups, it was found that up to 91.5% of patients with DKD were affected by vitamin D deficiency and insufficiency [18]. Vitamin D, a fat-soluble vitamin essential for human health, is catalyzed by the liver into 25-OH-D, which is further converted in the kidneys into biologically active 1,25-dihydroxyvitamin D3. This active form binds to receptors in target tissues, participating in the regulation of calcium and phosphorus metabolism [46,47,48,49,50]. Nakai et al. [52] demonstrated that 25-OH-D partially antagonizes nuclear factor κB activation induced by advanced glycation end products in mouse podocytes [53]. Additionally, the vitamin D analog masalone has been shown to reduce oxidative stress through the Nrf2-Keap1 pathway, thereby delaying the progression of diabetic nephropathy in rats. Vitamin D acts as a potent inhibitor of the renin-angiotensin aldosterone system [54], potentially mitigating glomerulosclerosis and fibrosis [55], regulating apoptosis and autophagy, ameliorating podocyte injury, and maintaining the structure of the glomerular filtration barrier [55, 56]. Lower levels of 25-OH-D are particularly detrimental in the context of renin-angiotensin-aldosterone system activation and hyperfiltration in diabetic mice [57]. Moreover, vitamin D may reduce the expression of transforming growth factor-β and inflammation, maintain vascular homeostasis, improve glucose and lipid metabolism, and enhance antioxidant defense and immune function [57,58,59]. Animal studies have suggested that vitamin D insufficiency may contribute to the pathogenesis of albuminuria [19]. 25-OH-D can decrease proteinuria by suppressing the renin-angiotensin system and TGF-β in mesangial and juxtaglomerular cells, consistent with the findings of this study.
The findings of this study demonstrate that β-CTX is independently and positively correlated with UACR. As quartiles of β-CTX levels increase, there is a trend towards decreasing eGFR. However, β-CTX did not exhibit any independent effects on DKD in the multivariable model using RCS. β-CTX serves as a degradation product of type I collagen, reflecting the biological activity of osteoclasts and indicating the extent of bone resorption [61]. Previous research has highlighted a negative correlation between β-CTX and eGFR in diabetic patients [13, 14], and a positive correlation with UACR [15], which is consistent with the current findings. Nonetheless, the specific mechanism by which β-CTX influences the progression from T2DM to DKD remains unclear and warrants further investigation.
Furthermore, our research reveals an independent positive correlation between OSTEOC and UACR, while it is independently negatively correlated with eGFR. As quartile levels of OSTEOC increase, there is a trend towards increasing UACR and decreasing eGFR. Moreover, the associations between OSTEOC and DKD were non-linear, approaching the J-shape, with risk estimates markedly increasing when OSTEOC levels exceeded 10.875 ng/L. OSTEOC, a specific protein secreted by osteoblasts and composed of 49 amino acids, plays crucial roles in various physiological processes including bone metabolism, energy metabolism, reproduction, and cognition [62]. It reflects the activity status of osteoblasts. OSTEOC has also been implicated in stimulating islet beta cells to release insulin and prompting adipocytes to release adiponectin, thereby enhancing insulin sensitivity [63]. Studies investigating the relationship between OSTEOC and glucose-lipid metabolism have yielded conflicting results, and the underlying mechanisms remain unclear [7, 63,64,65,66,67]. Zhao et al. found a significant positive correlation between UACR and OSTEOC in a cross-sectional study involving 297 T2DM patients [12], consistent with our findings. However, caution is warranted regarding the potential for reverse causality. A prospective cohort study demonstrated that even after adjusting for baseline eGFR and UACR, serum OSTEOC maintains an independent and robust negative correlation with DKD events [69]. In cross-sectional studies, reduced renal function may lead to decreased OSTEOC excretion and consequently higher circulating OSTEOC levels, potentially distorting the exposure-disease relationship.
The findings of this study indicate that iPTH levels are significantly higher in DKD patients compared to those without DKD. iPTH is independently and positively correlated with the incidence of DKD and UACR, while being independently negatively correlated with eGFR. As quartile levels of iPTH increase, there is a downward trend in eGFR. iPTH, a peptide hormone, exerts biological effects by regulating calcium and phosphorus metabolism through actions on target tissues such as bones and kidneys, and it is ultimately cleared by the kidneys. PTH strengthens osteolysis, enhances renal tubular reabsorption of calcium, mobilizes calcium into the bloodstream, and increases blood calcium levels. Previous research has suggested that elevated iPTH levels can act as a uremic toxin, influencing mitochondrial function and contributing to cell death and organ damage [69,70,71]. Our observations reveal a non-linear association between iPTH and DKD, approaching the J-shape, with risk estimates significantly increasing when iPTH levels exceed 34.15 pg/mL. This reflects the dual nature of iPTH, where within a physiological range it exerts beneficial effects, while beyond this range it may have detrimental effects, consistent with previous findings.
Furthermore, our study reveals an independent positive correlation between TP1NP and the incidence of UACR, while being independently negatively correlated with eGFR. As quartile levels of TP1NP increase, there is a trend of increasing UACR and decreasing eGFR. Additionally, the risk estimates markedly increase with rising TP1NP levels. TP1NP is an extension peptide of type I procollagen [72, 73], synthesized and released into circulation by osteoblasts [74, 75]. It serves as a sensitive marker of bone formation [76]. Previous research supports our findings, indicating a negative correlation between TP1NP levels and eGFR in diabetes patients, and a positive association between TP1NP and UACR in T2DM patients. We propose two potential explanations for this association. First, TP1NP may accumulate in the body as eGFR declines, leading to elevated circulating levels [77]. Second, given that bone remodeling is metabolically demanding, disturbances in energy metabolism and microcirculation in T2DM patients may contribute to observed decreases in bone formation markers [78].
The findings suggest BTMs homeostasis may be related to the etiology and pathogenesis of DKD in elder patients with T2DM. These results highlight the potential utility of BTMs as biomarkers for kidney disease, aiding in the identification of individuals at increased risk for T2DM-related renal complications. This has significant clinical implications for managing bone metabolism disorders and kidney complications in elderly patients with diabetes. Therefore, in clinical practice, attention should be given to the dynamic monitoring of BTMs in elderly T2DM patients. Additionally, maintaining optimal BTM levels from an early age may be associated with a reduced future risk of DKD development.
Our study possesses several strengths. Firstly, we conducted a large-scale population study involving hospitalized elderly T2DM patients, ensuring a substantial sample size and comprehensive data collection, which allowed us to assess common confounders. This is the first study to report the association between BTMs and the prevalence of DKD in an elderly cohort. Secondly, we emphasized the nonlinearity in the study, better illustrating the dose-response relationship. Thirdly, we examined BTMs as both continuous and categorical variables to reduce data analysis contingency and enhance the robustness of our results. Nevertheless, this study has certain limitations. Firstly, selection bias could not be avoided in this single-center, hospital-based study. Secondly, detecting BTMs at a single time point only provides a snapshot and does not allow for an understanding of the dynamic changes in BTMs and their association with DKD. Thirdly, all participants were of Han Chinese ethnicity, which may limit the generalizability of the results to other ethnic groups, as bone metabolism and osteoporosis vary among different races. Fourthly, potential confounding factors affecting BTMs levels, such as sun exposure, outdoor exercise, nutritional status, dietary habits, and seasonal variations, were not included in this analysis.
Conclustions
BTMs are closely associated with kidney disease in elderly patients with T2DM. These discoveries potentially assist clinicians in establishing more preventive measures and targeted treatment strategies for elderly patients with T2DM.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chinese Elderly Type 2 Diabetes Prevention and Treatment of Clinical Guidelines Writing Group. [Clinical guidelines for prevention and treatment of type 2 diabetes mellitus in the elderly in China (2022 edition)]. Zhonghua nei ke za zhi. 2022;61(1):12–50. Chinese. Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Society; Geriatric Endocrinology and Metabolism Branch of Chinese Geriatric Health Care Society.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s guide to Prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81.
Rathinavelu S, Guidry-Elizondo C, Banu J. Molecular modulation of osteoblasts and osteoclasts in type 2 diabetes. J Diabetes Res. 2018;2018:6354787.
Zou Y, Zhao L, Zhang J, Wang Y, Wu Y, Ren H, et al. Development and internal validation of machine learning algorithms for end-stage renal disease risk prediction model of people with type 2 diabetes mellitus and diabetic kidney disease. Ren Fail. 2022;44(1):562–70.
Winiarska A, Filipska I, Knysak M, Stompór T. Dietary phosphorus as a marker of Mineral Metabolism and Progression of Diabetic kidney disease. Nutrients. 2021;13(3):789.
Tan A, Gao Y, Yang X, Zhang H, Qin X, Mo L, et al. Low serum osteocalcin level is a potential marker for metabolic syndrome: results from a Chinese male population survey. Metabolism. 2011;60(8):1186–92.
Rui X, Xu B, Su J, Pan C, Zhan C, Su B, et al. Differential pattern for regulating insulin secretion, insulin resistance, and lipid metabolism by osteocalcin in male and female T2DM patients. Med Sci Monit. 2014;20:711–9.
Bador KM, Wee LD, Halim SA, Fadi MF, Santhiran P, Rosli NF, et al. Serum osteocalcin in subjects with metabolic syndrome and central obesity. Diabetes Metab Syndr. 2016 Jan-Mar;10(1 Suppl 1):S42–5.
Chen Y, Zhao Q, Du G, Xu Y. Association between serum osteocalcin and glucose/lipid metabolism in Chinese Han and Uygur populations with type 2 diabetes mellitus in Xinjiang: two cross-sectional studies. Lipids Health Dis. 2017;16(1):139.
Tejwani V, Qian Q. Calcium regulation and bone mineral metabolism in elderly patients with chronic kidney disease. Nutrients. 2013;5(6):1913–36.
Kochanek M, Said A, Lerma EV. Mineral metabolism in chronic kidney disease. Dis Mon. 2015;61(10):425–33.
Zhao X, Zhang XM, Yuan N, Yu XF, Ji LN. Associations of Bone Mineral density and bone metabolism indices with urine albumin to creatinine ratio in Chinese patients with type 2 diabetes. Exp Clin Endocrinol Diabetes. 2019;127(1):50–5.
Zhu X, Zhou Y, Hong S, Xue Y, Cui Y. Correlation between serum bone turnover markers and estimated glomerular filtration rate in Chinese patients with diabetes. Dis Markers. 2021;2021:6731218.
Maghbooli Z, Shabani P, Gorgani-Firuzjaee S, Hossein-Nezhad A. The association between bone turnover markers and microvascular complications of type 2 diabetes. J Diabetes Metab Disord. 2016;15:51.
Hou Y, Hou X, Nie Q, Xia Q, Hu R, Yang X, et al. Association of bone turnover markers with type 2 diabetes Mellitus and Microvascular complications: a matched case-control study. Diabetes Metab Syndr Obes. 2023;16:1177–92.
American Diabetes Association. Standards of Medical Care in Diabetes-2017 abridged for primary care providers. Clin Diabetes. 2017;35(1):5–26.
American Diabetes Association. 11. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S124-S138.
Duan S, Lu F, Wu B, Zhang C, Nie G, Sun L, et al. Association of Serum 25 (OH) vitamin D with chronic kidney Disease Progression in Type 2 diabetes. Front Endocrinol (Lausanne). 2022;13:929598.
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS. 25-Hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis. 2007;50(1):69–77.
Chen X, Wan Z, Geng T, Zhu K, Li R, Lu Q, et al. Vitamin D status, Vitamin D Receptor Polymorphisms, and risk of Microvascular complications among individuals with type 2 diabetes: a prospective study. Diabetes Care. 2023;46(2):270–7.
Zhou T, Shen L, Li Z, Jia J, Xing H, Wang N, et al. Severe 25-Hydroxyvitamin D Deficiency May Predict Poor renal outcomes in patients with Biopsy-Proven Diabetic Nephropathy. Front Endocrinol (Lausanne). 2022;13:871571.
Wang X, Liu X, Zhao J, Chen M, Wang L. Construction of a Nomogram-based prediction model for the risk of Diabetic kidney disease in T2DM. Diabetes Metab Syndr Obes. 2024;17:215–25.
Kim MJ, Frankel AH, Donaldson M, Darch SJ, Pusey CD, Hill PD, et al. Oral cholecalciferol decreases albuminuria and urinary TGF-β1 in patients with type 2 diabetic nephropathy on established renin-angiotensin-aldosterone system inhibition. Kidney Int. 2011;80(8):851–60.
Wan H, Wang Y, Zhang K, Chen Y, Fang S, Zhang W, et al. Associations between vitamin D and microvascular complications in middle-aged and elderly diabetic patients. Endocr Pract. 2019;25(8):809–16.
Liang Q, Hu H, Wu H, Chen X, Wang W, Le Y, et al. A nonlinear relationship between serum 25-Hydroxyvitamin D and urine albumin to creatinine ratio in type 2 diabetes: a cross-sectional study in China. Diabetes Metab Syndr Obes. 2021;14:2581–93.
Hong SH, Kim YB, Choi HS, Jeong TD, Kim JT, Sung YA. Association of Vitamin D Deficiency with Diabetic Nephropathy. Endocrinol Metab (Seoul). 2021;36(1):106–13.
Grammatiki M, Karras S, Kotsa K. The role of vitamin D in the pathogenesis and treatment of diabetes mellitus: a narrative review. Horm (Athens). 2019;18(1):37–48.
Xie S, Huang L, Cao W, Hu Y, Sun H, Cao L, et al. Association between serum 25-hydroxyvitamin D and diabetic kidney disease in Chinese patients with type 2 diabetes. PLoS ONE. 2019;14(4):e0214728.
Peng Y, Li LJ. Serum 25-hydroxyvitamin D level and diabetic nephropathy in patients with type 2 diabetes mellitus. Int Urol Nephrol. 2015;47(6):983–9.
Zhao WJ, Xia XY, Yin J. Relationship of serum vitamin D levels with diabetic microvascular complications in patients with type 2 diabetes mellitus. Chin Med J (Engl). 2021;134(7):814–20.
Ravani P, Malberti F, Tripepi G, Pecchini P, Cutrupi S, Pizzini P, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75(1):88–95.
Agarwal R, Vitamin D. Proteinuria, diabetic nephropathy, and progression of CKD. Clin J Am Soc Nephrol. 2009;4(9):1523–8.
Xiao X, Wang Y, Hou Y, Han F, Ren J, Hu Z. Vitamin D deficiency and related risk factors in patients with diabetic nephropathy. J Int Med Res. 2016;44(3):673–84.
Liyanage P, Lekamwasam S, Weerarathna TP, Liyanage C. Effect of vitamin D therapy on urinary albumin excretion, renal functions, and plasma renin among patients with diabetic nephropathy: a randomized, double-blind clinical trial. J Postgrad Med. 2018 Jan-Mar;64(1):10–5.
Senyigit A. The association between 25-hydroxy vitamin D deficiency and diabetic complications in patients with type 2 diabetes mellitus. Diabetes Metab Syndr. 2019 Mar-Apr;13(2):1381–6.
Ucak S, Sevim E, Ersoy D, Sivritepe R, Basat O, Atay S. Evaluation of the relationship between microalbuminuria and 25-(OH) vitamin D levels in patients with type 2 diabetes mellitus. Aging Male. 2019;22(2):116–20.
Derakhshanian H, Shab-Bidar S, Speakman JR, Nadimi H, Djafarian K. Vitamin D and diabetic nephropathy: a systematic review and meta-analysis. Nutrition. 2015;31(10):1189–94.
Herrmann M, Sullivan DR, Veillard AS, McCorquodale T, Straub IR, Scott R, et al. FIELD study investigators. Serum 25-hydroxyvitamin D: a predictor of macrovascular and microvascular complications in patients with type 2 diabetes. Diabetes Care. 2015;38(3):521–8.
Felício JS, de Rider Britto HA, Cortez PC, de Souza Resende F, de Lemos MN, de Moraes LV, et al. Association between 25(OH)vitamin D, HbA1c and Albuminuria in Diabetes Mellitus: Data from a Population-based study (VIDAMAZON). Front Endocrinol (Lausanne). 2021;12:723502.
Abasheva D, Dolcet-Negre MM, Fernández-Seara MA, Mora-Gutiérrez JM, Orbe J, Escalada FJ, et al. Association between circulating levels of 25-Hydroxyvitamin D3 and Matrix Metalloproteinase-10 (MMP-10) in patients with type 2 diabetes. Nutrients. 2022;14(17):3484.
Joergensen C, Gall MA, Schmedes A, Tarnow L, Parving HH, Rossing P. Vitamin D levels and mortality in type 2 diabetes. Diabetes Care. 2010;33(10):2238–43.
Joergensen C, Hovind P, Schmedes A, Parving HH, Rossing P. Vitamin D levels, microvascular complications, and mortality in type 1 diabetes. Diabetes Care. 2011;34(5):1081–5.
Dall’Agnol A, Brondani LA, Cancelier VDA, Camargo EG, Silveiro SP. Lower serum 25-hydroxyvitamin D levels are associated with impaired glomerular filtration rate in type 2 diabetes patients. Ther Adv Endocrinol Metab. 2020;11:2042018820930904.
Xiao Y, Wei L, Xiong X, Yang M, Sun L. Association between Vitamin D Status and Diabetic complications in patients with type 2 diabetes Mellitus: a cross-sectional study in Hunan China. Front Endocrinol (Lausanne). 2020;11:564738.
Xiong R, Yuan Y, Zhu Z, Wu Y, Ha J, Han X, et al. Micronutrients and Diabetic Retinopathy: evidence from the National Health and Nutrition Examination Survey and a Meta-analysis. Am J Ophthalmol. 2022;238:141–56.
Mohammed A, Marie MA, Abdulazim DO, Hassan M, Shaker O, Ayeldeen G, et al. Serum urate lowering therapy using Allopurinol improves serum 25 Hydroxy vitamin D in Stage 3–5 CKD patients: a pilot study. Nephron. 2021;145(2):133–6.
Schön A, Leifheit-Nestler M, Deppe J, Fischer DC, Bayazit AK, Obrycki L, et al. Active vitamin D is cardioprotective in experimental uraemia but not in children with CKD stages 3–5. Nephrol Dial Transpl. 2021;36(3):442–51.
Caccamo D, Cannata A, Ricca S, Catalano LM, Montalto AF, Alibrandi A, et al. Role of Vitamin-D receptor (VDR) single nucleotide polymorphisms in gestational hypertension development: a case-control study. PLoS ONE. 2020;15(11):e0239407.
Vernia F, Valvano M, Longo S, Cesaro N, Viscido A, Latella G. Vitamin D in Inflammatory Bowel diseases. Mech Action Therapeutic Implications Nutrients. 2022;14(2):269.
de Souza Freitas R, Fratelli CF, de Souza Silva CM, de Lima LR, Stival MM, da Silva ICR, et al. Association of Vitamin D with the TaqI polymorphism of the VDR Gene in Older Women attending the Basic Health Unit of the Federal District, DF (Brazil). J Aging Res. 2020;2020:7145193.
Nakai K, Fujii H, Kono K, Goto S, Kitazawa R, Kitazawa S, et al. Vitamin D activates the Nrf2-Keap1 antioxidant pathway and ameliorates nephropathy in diabetic rats. Am J Hypertens. 2014;27(4):586–95.
Rüster C, Franke S, Reuter S, Mrowka R, Bondeva T, Wolf G. Vitamin D3 partly antagonizes Advanced-Glycation endproducts-Induced NFκB activation in Mouse Podocytes. Nephron. 2016;134(2):105–16.
Alam U, Arul-Devah V, Javed S, Malik RA. Vitamin D and Diabetic complications: true or false prophet? Diabetes Ther. 2016;7(1):11–26.
Lei M, Liu Z, Guo J. The emerging role of vitamin D and Vitamin D Receptor in Diabetic Nephropathy. Biomed Res Int. 2020;2020:4137268.
Hamzawy M, Gouda SAA, Rashid L, Attia Morcos M, Shoukry H, Sharawy N. The cellular selection between apoptosis and autophagy: roles of vitamin D, glucose and immune response in diabetic nephropathy. Endocrine. 2017;58(1):66–80.
Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110(2):229–38.
Tecilazich F, Formenti AM, Giustina A. Role of vitamin D in diabetic retinopathy: pathophysiological and clinical aspects. Rev Endocr Metab Disord. 2021;22(4):715–27.
Grammatiki M, Rapti E, Karras S, Ajjan RA, Kotsa K. Vitamin D and diabetes mellitus: causal or casual association? Rev Endocr Metab Disord. 2017;18(2):227–41.
Lee H, Lee H, Lim Y. Vitamin D3 improves lipophagy-associated renal lipid metabolism and tissue damage in diabetic mice. Nutr Res. 2020;80:55–65.
Iglesias P, Arrieta F, Piñera M, Botella-Carretero JI, Balsa JA, Zamarrón I, et al. Serum concentrations of osteocalcin, procollagen type 1 N-terminal propeptide and beta-CrossLaps in obese subjects with varying degrees of glucose tolerance. Clin Endocrinol (Oxf). 2011;75(2):184–8.
Zhou H, Seibel MJ, Bone. Osteoblasts and global energy metabolism - beyond osteocalcin. Nat Rev Rheumatol. 2017;13(5):261–2.
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, et al. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007;130(3):456–69.
Choudhury AB, Sarkar PD, Sakalley DK, Petkar SB. Role of adiponectin in mediating the association of osteocalcin with insulin resistance and type 2 diabetes: a cross sectional study in pre- and post-menopausal women. Arch Physiol Biochem. 2014;120(2):73–9.
Chen L, Li Q, Yang Z, Ye Z, Huang Y, He M, et al. Osteocalcin, glucose metabolism, lipid profile and chronic low-grade inflammation in middle-aged and elderly Chinese. Diabet Med. 2013;30(3):309–17.
Liu DM, Guo XZ, Tong HJ, Tao B, Sun LH, Zhao HY, et al. Erratum to: Association between osteocalcin and glucose metabolism: a meta-analysis. Osteoporos Int. 2015;26(12):2835–6.
Shu H, Pei Y, Chen K, Lu J. Significant inverse association between serum osteocalcin and incident type 2 diabetes in a middle-aged cohort. Diabetes Metab Res Rev. 2016;32(8):867–74.
Wang Q, Zhang B, Xu Y, Xu H, Zhang N. The relationship between serum osteocalcin concentration and glucose metabolism in patients with type 2 diabetes Mellitus. Int J Endocrinol. 2013;2013:842598.
Ye X, Yu R, Jiang F, Hou X, Wei L, Bao Y, et al. Osteocalcin and risks of Incident Diabetes and Diabetic kidney disease: a 4.6-Year prospective cohort study. Diabetes Care. 2022;45(4):830–6.
Kuriwaka-Kido R, Kido S, Miyatani Y, Ito Y, Kondo T, Omatsu T, et al. Parathyroid hormone (1–34) counteracts the suppression of interleukin-11 expression by glucocorticoid in murine osteoblasts: a possible mechanism for stimulating osteoblast differentiation against glucocorticoid excess. Endocrinology. 2013;154(3):1156–67.
Krikorian A, Shah S, Wasman J. Parathyroid hormone-related protein: an unusual mechanism for hypercalcemia in sarcoidosis. Endocr Pract 2011 Jul-Aug;17(4):e84–6.
Chen T, Wang Y, Hao Z, Hu Y, Li J. Parathyroid hormone and its related peptides in bone metabolism. Biochem Pharmacol. 2021;192:114669.
Nordklint AK, Almdal TP, Vestergaard P, Lundby-Christensen L, Jørgensen NR, Boesgaard TW, et al. Effect of Metformin vs. Placebo in combination with insulin analogues on bone markers P1NP and CTX in patients with type 2 diabetes Mellitus. Calcif Tissue Int. 2020;107(2):160–9.
Takada J, Dinavahi R, Miyauchi A, Hamaya E, Hirama T, Libanati C, et al. Correction to: relationship between P1NP, a biochemical marker of bone turnover, and bone mineral density in patients transitioned from alendronate to romosozumab or teriparatide: a post hoc analysis of the STRUCTURE trial. J Bone Min Metab. 2020;38(4):605.
Zuo CT, Yin DC, Fan HX, Lin M, Meng Z, Xin GW, et al. Study on diagnostic value of P1NP and β-CTX in bone metastasis of patients with breast cancer and the correlation between them. Eur Rev Med Pharmacol Sci. 2019;23(12):5277–84.
Hansen S, Shanbhogue VV, Jørgensen NR, Beck-Nielsen SS. Elevated bone remodeling markers of CTX and P1NP in addition to Sclerostin in patients with X-linked hypophosphatemia: a cross-sectional controlled study. Calcif Tissue Int. 2019;104(6):591–8.
Glendenning P, Chubb SAP, Vasikaran S. Clinical utility of bone turnover markers in the management of common metabolic bone diseases in adults. Clin Chim Acta. 2018;481:161–70.
Hayer MK, Radhakrishnan A, Price AM, Liu B, Baig S, Weston CJ, et al. Defining myocardial abnormalities across the stages of chronic kidney disease: a Cardiac magnetic resonance imaging study. JACC Cardiovasc Imaging. 2020;13(11):2357–67.
Wang H, Zheng X, Zhang Y, Huang J, Zhou W, Li X, et al. The endocrine role of bone: novel functions of bone-derived cytokines. Biochem Pharmacol. 2021;183:114308.
Acknowledgements
The authors thank all the participants in the study and colleagues in the nursing group in their department.
Funding
This project was funded by Beijing Municipal Natural Science Foundation (Grant No.7242255), the Traditional Chinese Medicine Evidence-Based Capacity Building Project(Grant No.60104), the Technology Innovation Project of Major Key Projects at the China Academy of Chinese Medical Sciences (Grant No.C12021A01617),and the High Level Chinese Medical Hospital Promotion Project (Grant No. HLCMHPP2023084).
Author information
Authors and Affiliations
Contributions
Shuwu Wei conceived the study, participated in its design and coordination, analyzed the data and drafted the manuscript. Xinyu Pan recruited patients and collected data. Junping Wei participated in its design and coordination, and was responsible for project administration, and visualization. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The ethics committee has waived the requirement of informed consent for this study. The full name of the Institutional Review Board that waived the informed consent procedure is “Ethical Committee in Guan’anmen Hospital, China Academy of Chinese Medical Sciences” (registration code:2023−187-KY). We confirm that methods were performed in accordance with declaration of Helsinki’s guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wei, S., Pan, X. & Wei, J. Relationship between bone turnover markers and renal disease in elderly patients with type 2 diabetes: a cross-sectional study. BMC Endocr Disord 24, 179 (2024). https://doi.org/10.1186/s12902-024-01698-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01698-y