Abstract
Background
The increasing trend in childhood obesity needs to be closely monitored and intervened due to long-term health issues such as metabolic syndrome, cardiovascular diseases, hypertension, and type 2 diabetes. We aimed to determine and compare the cut-off values for the visceral adiposity index (VAI), triglyceride-glucose index (TyG), and HOMA-IR for predicting metabolic syndrome (MetS).
Methods
This population-based cross-sectional study was conducted in May 2019 in Samsun, Turkey. The study included 169 children with obesity aged 9 and 10 years. After anthropometric and clinical evaluation, fasting blood samples were collected from the children. The areas under the curve of the visceral adiposity index, triglyceride-glucose index, and HOMA-IR were compared by receiver-operating-characteristic (ROC) analysis in predicting the MetS.
Results
The total prevalence of MetS was 21.3% in children with obesity, and it was two times higher in girls than in boys. The mean values of TyG and VAI were significantly different in those who have and have not MetS in both genders. However, the HOMA-IR index was higher only in girls with MetS and did not differ in boys by having MetS. The VAI and the TyG index both had statistically significant cut-off values in both sexes and a larger ROC area than the HOMA-IR index in predicting MetS.
Conclusions
The VAI and TyG index are effective indicators in assessing the MetS risk in children with obesity. Both indexes can be considered useful tools in pediatric research and the evaluation of interventions. However, the HOMA-IR index formula needs to be developed taking into account age, gender, and ethnicity.
Similar content being viewed by others
Introduction
Obesity is a global health problem for children and adolescents due to the many morbid consequences it is associated with, and the increasing trend in childhood obesity needs to be closely monitored and intervened [1, 2]. Childhood obesity causes many short and long-term health issues such as metabolic syndrome (MetS), cardiovascular diseases, hypertension, type 2 diabetes, fatty liver, orthopedic difficulties, and decreased self-confidence [3, 4]. While MetS increases Type 2 diabetes risk through dysregulated cellular metabolism leading to insulin resistance, it also contributes to cardiovascular disease risk due to increased blood pressure, free fatty acids, triglycerides, and decreased HDL cholesterol levels. For these reasons, MetS is considered an indicator of future type 2 diabetes in children [5]. MetS, whose prevalence is increased by obesity, can persist into adulthood, and follow-up studies have shown that 50–80% of children with obesity become obese adults with a high risk of developing the aforementioned morbidities [6]. While the exact prevalence of pediatric MetS is unknown because of the wide range of physical and hormonal changes according to age and sex during childhood and adolescence [7], pediatric MetS is considered an important target for potential interventions to reduce the burden of cardiometabolic diseases [5]. Detecting MetS in children can provide an opportunity for early intervention to prevent CVD in adults [6]. However, calculating the risk of MetS requires various measurements such as waist circumference, triglyceride, HDL cholesterol, fasting glucose, and systolic and diastolic blood pressure levels [8]. Besides, lack of consensus on the limit value of the biochemical parameters used in calculating the risk of MetS in children, and missing national and/or international assessment systems for diagnosing MetS in children makes it difficult to use these indices [9].
As in adults, early detection of insulin resistance (IR) in children is important to prevent the development of cardiometabolic diseases such as Type 2 Diabetes Mellitus, metabolic syndrome, and coronary heart disease. The Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) index, which has high sensitivity and specificity, has been shown to be more useful in estimating the risk of insulin resistance, instead of more invasive, complex, and expensive direct tests such as pancreatic suppression test and hyperinsulinemic-euglycemic glucose clamp technique[10]. HOMA-IR is an approved method for evaluating insulin resistance using fasting glucose and insulin levels and is widely used in clinical practice [11].
Visceral adiposity index (VAI) which is used to calculate cardiometabolic risk by anthropometric measurements and blood lipid parameters is a useful tool for detecting MetS in children and adolescents [12,13,14,15]. Recently, the use of the triglyceride glucose (TyG) index, a product of fasting glucose and triglyceride and a useful predictor of cardiometabolic risk factors in childhood and adolescence has also increased [16,17,18,19], because, they are more easily accessible assessment tools both at the outpatient clinics and at the community level, and are low cost [20]. Although VAI and TyG have proven to be useful in determining the risk of cardiometabolic disease in the adult population, few studies have been conducted on children with obesity. Therefore, we aimed to establish the cut-off points of the VAI, the TyG index, and the HOMA-IR index for the diagnosis of MetS in obese Turkish children, and to determine which of these indices will provide a more accurate approach to diagnosis.
Methods
Study design
To determine the prevalence of childhood obesity, we conducted a cross-sectional study on 9786 children representing all public and private primary school students between October and November 2016, in Samsun, Turkey [21]. This representative sample was selected from 70,660 students in 388 primary schools by multistage and stratified random sampling method by residency (rural/urban), school type (public/private), grade (I-IV), and gender. Classes with less than ten students were not included in the sample selection. The prevalence of obesity was found 10.5% (1030 children). While 403 of these children were first and second-grade students, 627 were third and fourth-grade students. We planned the current cross-sectional study to gather new data on the development of metabolic syndrome in children with obesity. However, the preparation of the project, sourcing and obtaining the approval of the ethics committee took two years, and those 627 students in the third and fourth grades had already graduated by then. In our country, especially in rural, students usually change their schools and leave their provinces or districts when they start secondary school, which makes it extremely hard to reach them again. For this reason, the students to be followed were limited to the 403 first and second-grade students who participated in the prior study. In addition, the lack of consensus on the definition of MetS in children under 9 years of age was another limiting factor in the selection of the study group [20].
Sampling
We tried to reach the parents of 403 children by phone or e-mail based on information extracted from the records of the initial study in April and May 2019. Nineteen children had been lost during the follow-up period. The remaining students were invited to the family health center for re-examination. Children who were diagnosed with obesity in the previous study and whose BMI value is above two standard deviations according to the WHO's age and sex-specific BMI table were included in the study. Children who lost weight and were no longer obese (n = 14), and those who were medicating for obesity or for another metabolic disease (such as neurologic, respiratory, or cardiovascular disease) (n = 15) were excluded. We used the formula n = Nxt2xpxq/d2x(N − 1) + t2xpxq to determine the minimum sample size [22]. In the formula;
n = The minimum number of individuals to be sampled,
N = The number of individuals in the target group from which the sample will be taken (355),
p = Prevalence of the investigated event (MetS prevalence 30% in Turkish obese children),
q = 1-prevalence (70%),
t = The theoretical value found according to the “t” table at 5% significance level (1.96),
d = The accepted sampling error (0.05).
The minimum sample size was found n = (355)x(1.96)2x(0.30 × 0.70)/(0.05)2x(355–1) + (1.96)2x(0.3 × 0.7) = 169.
Since taking a blood sample is an invasive method and is frightening for the pediatric age group, we preferred to limit the number of participants to a minimum sample size. The current study group was selected from the list of children with obesity by a systematic sampling method.
Anthropometrics and clinical assessment
For anthropometric measurements, children were dressed in light underwear and bare feet or in socks. The waist circumference (WC) measurements were taken at the umbilical level. The student's height and weight were measured using a stadiometer with a sensitivity of ± 0.1 cm (SECA Ltd, Medical Scales and Measurement Systems, Birmingham, United Kingdom) and a calibrated weighing instrument with a sensitivity of ± 0·1 kg (Seca Mess und Wiegetechnik, Germany), respectively. The height and weight were measured twice, and the averages were recorded. The BMI was calculated by the Quetelet equation (weight / height2). According to the WHO BMI chart, the children who had a BMI score above two standard deviations for age and sex were defined as obese [23]. Systolic (SBP) and diastolic blood pressures (DBP) were measured twice at five-minute intervals with the ERKA sphygmomanometer, and their average was recorded as mm Hg. Being a blood pressure higher than 130/85 mm Hg was accepted as hypertension [24].
Biochemical analyses and definitions
The fasting blood samples of the children were collected between 08:00 and 09:00 h. The levels of total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglyceride (TG), and fasting blood glucose (FBG) were measured. Biochemical measurements of fasting blood samples were studied with the COBAS 8000 c-702 (Roche) auto analyzer device using colorimetric kits.
Insulin resistance was calculated according to the Homeostasis Model Assessment insulin resistance (HOMA-IR) index. HOMA-IR was obtained with the formula fasting glucose (mmol/L) X fasting insulin (IU/ml) / 405. HOMA-IR values above 3.54 were identified as insulin resistance [10]. The TyG index was calculated using the following formula: ln [fasting triglycerides (mg/dl) × fasting plasma glucose (mg/dL)/2] [25]. The VAI were calculated both for men and women separately according to the following Equations [13]:
According to the International Diabetes Federation’s criteria, the presence of at least two of the following criteria accompanying central obesity was considered MetS: Triglyceride level of ≥ 150 mg/dL, HDL cholesterol level of < 40 mg/dL, fasting glucose level equal to or higher than 100 mg/dL, systolic blood pressure of higher than 130 mm Hg, or diastolic blood pressure of equal to or higher than 85 mm Hg, or receiving antihypertensive treatment [9].
Statistical analysis
Statistical analysis was performed by SPSS version 22·0 (IBM Corporation, Armonk, NY, USA) package program. The conformity of continuous variables to normal distribution was determined by the Shapiro Wilk test. Quantitative data were presented with arithmetic mean and standard deviation, and qualitative data were presented in numbers and percentages. The Chi-square test was used to compare categorical variables. While non-normally distributed data were compared using the Mann Whitney U test, the Student’s t-test was used to compare normally distributed quantitative data. The sensitivity, specificity, and cut-off points of the VAI and the TyG were examined using receiver-operating characteristic (ROC) curve analyses. We assessed the overall performance of each index for predicting the MetS by computing the area under the curve (AUC). We determined the best cut-off points as the point on the curve where both sensitivity and specificity were the highest. In statistical analysis, p˂0.05 was accepted as the limit value of significance.
Results
The mean age of the 169 students with obesity was 10·2 ± 0·5 years, and 85 (50·3%) of them were girls. While the anthropometric parameters were no different except waist circumference according to gender, biochemical parameters were higher in girls than in boys, except HDL (Table 1). The total prevalence of MetS was 21.3% in children with obesity, and it was two times higher in girls than in boys. The TyG index was similar in both genders (p = 0.376).
HOMA-IR, TyG, and VAI were higher both in boys and girls with MetS than in those without (Table 2). However, HOMA-IR was statistically different in girls only.
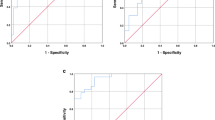
The abilities of the triglyceride-glucose index, visceral adiposity index, and HOMA-IR index for predicting the MetS were evaluated by ROC curve analysis for boys and girls, and the results were presented in Figs. 1 and 2, respectively.
The cut-off points of the TyG, the VAI, and the HOMA-IR index with the best balance between sensitivity and specificity for MetS and the area under the curve (AUC) were presented in Table 3. Cut-off values of all three indices were found to be higher in girls than in boys. The AUC values of both TyG and VAI index cut-off points were significantly higher than the AUC value of the HOMA-IR cut-off value in both sexes (p < 0.01).
Discussion
Cardiometabolic disorders are important public health problems due to their negative effects on disease burden and healthcare costs. For this reason, many studies have been conducted on cardiometabolic risk factors and early detection criteria in children and adolescents as well as adults [4]. VAI and TyG index are valuable tools to identify MetS and estimate cardiometabolic risk factors in children and adolescents with obesity because both have higher values in children with obesity, and are advantageous as an easy tool for detecting MetS [20, 26]. In addition, many researchers have declared that the association of VAI with metabolic diseases in adults is stronger than with traditional anthropometric indicators of adiposity, and its strength in children and adolescents continues to be investigated [12, 15, 26].
Studies conducted in different countries reported that the cut-off points calculated for VAI in predicting the MetS in children ranged from 1.30–6.15 (AUC: 85%-77%) in boys, and 1.78–4.95 (AUC: 89%-76%) in girls [12, 15, 16, 26]. Our study was conducted on Turkish children with obesity in a more limited age group, and the cut-off points we obtained for VAI were found higher than in the aforementioned studies. The presence of a hypersensitive hypothalamic–pituitary–adrenal axis in children with obesity in the prepubertal-pubertal period negatively affects the hormonal balance. The balance between the lipogenic effect of cortisol and insulin, which are hormones effective on body fat distribution, and the lipolytic effect of sex steroids and growth hormones can be disrupted, especially in children with obesity [27]. The differences between sexes are related to the differences in the amount and location of visceral fat accumulation, as well as hormones [28]. The reason for the high VAI cut-off points and the lower sensitivity/specificity values determined in our study may be due to the selection of the sample from the age group close to the pubertal period, as well as the differences in the distribution of adipose tissue in children with obesity. In a systematic review, it has been reported that the distribution of visceral adipose tissue in children and adolescents is associated with factors such as genetics, ethnicity, gender, age, developmental level, and puberty [29]. Therefore, these factors should be considered when evaluating predictors of cardiometabolic risk. For the measurement of waist circumference, which is also a predictor for the MetS, it is recommended to use percentiles specific to ethnic origin, in addition to age and gender [30]. The main factor that makes VAI an important predictor is that it is an indicator of early cardiometabolic risk when the metabolic syndrome does not show clinical signs yet. Having better performance of VAI in predicting the MetS has been explained by the association of VAI with three main components of the MetS criteria, WC, TG, and HDL, and adiponectin and insulin resistance, which are cytokines associated with high levels of inflammation [27].
However, there are some studies in the literature, suggesting that the TyG index is a better indicator than the VAI in adults [31,32,33]. The TyG index is associated with insulin resistance and dyslipidemia and has been recommended as a good indicator of the presence of cardiometabolic risk factors, particularly insulin sensitivity [11, 18, 34, 35]. Besides, it has been reported that the TyG index has a high sensitivity for MetS in children and adolescents with obesity [11, 19, 36]. Similar to our result, Brito et al. [20] reported in a systematic review that in the ROC curve analyses performed to predict the cardiometabolic risk factors, the TyG index threshold values ranged from 4.65 to 8.66, and the cut-off point in girls was higher than in boys. Similarly, it was stated that the cut-off points ranged between 8.52–8.74 (AUC: 84%- 90%) while the sensitivity (82%-92%) and specificity (82%-91%) values were high in another study also [36]. Although we obtained lower sensitivity and specificity values compared to these studies, their cut-off points are consistent with our cut-off points for both genders. It has been stated that the difference between the cut-off points may be originated from age, gender, ethnicity, pubertal level, diet, and the TyG index formula used. [7, 18, 20, 35, 37]. We consider that the main reason for reporting different cut-off points for TyG is the difference in the TyG index formula used. Because, when the TyG index is calculated according to the original formula (Ln [fasting triglycerides (mg/dL) x fasting glucose (mg/dL) /2]) results in close to eight, while the following formula gives a result in close to four: Ln [fasting triglycerides (mg/dL) x fasting glucose (mg/dL)]/2. Unfortunately, the studies that have correctly computed and reported the TyG index using the original formula are limited.
Although there is an increasing number of studies detecting IR and related metabolic abnormalities in children, the HOMA-IR threshold value has not been determined for metabolic syndrome, but a positive correlation of HOMA-IR scores with BMI has been demonstrated [25]. In a systematic review, it was reported that the cut-off points of HOMA-IR in children and adolescents for predicting the MetS ranged from 2.30 to 3.59, and the sensitivity and specificity of these values were 59%-89% and 62%-87%, respectively [10]. In a study conducted on obese Turkish adolescents, the cut-off point for HOMA-IR was determined 2.62 in boys (AUC = 0.710; sensitivity = 80·4%; specificity = 47·4%), and 2.66 in girls (AUC = 0.673; sensitivity = 81.8%; specificity = 40.6%) [11]. The cut-off points of HOMA-IR were approximately twice as high in our study, but lower sensitivity and higher specificity were determined. These different findings indicate the existence of other factors other than ethnicity or nutritional culture. For example, the mean age of our study group is lower than those of many other study groups. It could not be shown clearly there is a correlation between visceral adiposity and inflammation markers, and insulin sensitivity in the pediatric age group, and the genetic factors have a greater role in emerging metabolic risk [38]. However, it was also noteworthy that a significant cut-off point for HOMA-IR has been found only in girls. Previous research has shown that adipose tissue produces adipokines that play a key role in the development and progression of insulin resistance and plays an important role in energy regulation through endocrine, paracrine and autocrine signals [39]. Therefore, it is hypothesized that adipokines have a possible link between obesity and other risk components of metabolic syndrome. An increase in adiponectin plasma concentration decreases insulin resistance, while leptin leads to the development of insulin resistance [40]. In studies conducted on people with obesity, serum leptin / adiponectin levels were found to be significantly higher in women than in men [41, 42]. Ather et al. [43] drew attention to a positive correlation between leptin and overweight in adolescent girls, and a negative correlation with adiponectin, besides to higher leptin levels in children with metabolic syndrome. In addition, it was shown that age and sex were significantly associated with MetS, and MetS prevalence generally increased with age in children [8]. All these findings explain why HOMA-IR levels and cut-off values for MetS are different in boys and girls with obesity.
Another disadvantage of HOMA-IR is its limited usage due to cost, requiring standardization for insulin, a labile hormone [19, 34]. It was shown that the difference in insulin sensitivity in children with obesity between the sexes is due to phenotypic characteristics, that there may be a gene responsible for it, and that girls have higher insulin resistance [44]. A study conducted in the Turkish population found that the FTO rs1421085 variant was associated with the risk of obesity only in women [45]. All these findings show that longitudinal and genetic studies are still needed to ensure standardization of HOMA-IR's cut-off points according to age, sex, ethnicity, and obesity status and to confirm its clinical benefit.
In contrast, the VAI and the TyG index both had significant cut-off values in both sexes, and their AUC values were larger than that of HOMA-IR. The TyG index has been proposed as a good indicator of insulin sensitivity, as it has been found significantly associated with glucose metabolism rates in many populations [11, 18, 34, 35]. In addition, some studies have suggested that TyG is a better indicator than VAI also in adults. [32, 46]. Nevertheless, it should be taken into account that in studies that indicate that VAI or Tyg is a superior predictor, the male/female ratio of participants may have affected the results.
There were some limitations to our study. First, although euglycemic hyperinsulinemic clamp technique is the gold standard method, we used the HOMA-IR to determine insulin resistance, as the former is a time-consuming, expensive, and invasive method. Second, the participants were limited to children aged 9–10 years in Samsun province, therefore the results may not be generalizable to other populations. Besides the cross-sectional study design, having not assessed the children's diet and physical activity were also other limitations.
Conclusion
Based on our results, the VAI had the highest area under the curve in boys, while TyG had the highest AUC in girls, suggesting both are more useful predictors than the HOMA-IR to determine for MetS risk. We determined that the VAI and the TyG index are effective indicators in the light of significant results obtained by ROC analysis in assessing the MetS risk in children with obesity. Both indexes can be considered useful tools in pediatric research and the evaluation of interventions. However, the HOMA-IR index formula needs to be developed taking into account age, gender, and ethnicity. For this purpose, it is thought that there is a need for cohort studies to be conducted in different populations and age groups.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BP:
-
Blood pressure
- CVD:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- FBG:
-
Fasting blood glucose
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostasis Model Assessment Insulin Resistance
- IFG:
-
Impaired fasting glucose
- LDL:
-
Low-density lipoprotein
- MetS:
-
Metabolic syndrome
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TyG:
-
Triglyceride-glucose index
- VAI:
-
Visceral adiposity index
- WC:
-
Waist circumference
References
Sanyaolu A, Okorie C, Qi X, Locke J, Rehman S. Childhood and adolescent obesity in the United States: A public health concern. Glob Pediatr Health. 2019;6:2333794X19891305.
Motlagh ME, Qorbani M, Rafiemanzelat AM, Taheri M, Aminaee T, Shafiee G, et al. Prevalence of cardiometabolic risk factors in a nationally representative sample of Iranian children and adolescents: the CASPIAN-V Study. J Cardiovasc Thorac Res. 2018;10(2):76–82.
Morales Camacho WJ, Molina Díaz JM, Plata Ortiz S, Plata Ortiz JE, Morales Camacho MA, Calderón BP. Childhood obesity: Aetiology, comorbidities, and treatment. Diabetes Metab Res Rev. 2019;35(8):e3203.
Weihe P, Weihrauch-Blüher S. Metabolic syndrome in children and adolescents: diagnostic criteria, therapeutic options and perspectives. Curr Obes Rep. 2019;8(4):472–9.
Lepe A, de Kroon ML, de Winter AF, Reijneveld SA. Alternative pediatric metabolic syndrome definitions impact prevalence estimates and socioeconomic gradients. Pediatr Res. 2021;90(3):694–700.
Leis R, de Lamas C, de Castro M-J, Picáns R, Gil-Campos M, Couce ML. Effects of nutritional education interventions on metabolic risk in children and adolescents: a systematic review of controlled trials. Nutrients. 2019;12(1):31.
Kim JW, Park SH, Kim Y, Im M, Han H-S. The cutoff values of indirect indices for measuring insulin resistance for metabolic syndrome in Korean children and adolescents. Ann Pediatr Endocrinol Metab. 2016;21(3):143.
Zhu Y, Zheng H, Zou Z, Jing J, Ma Y, Wang H, et al. Metabolic syndrome and related factors in Chinese children and adolescents: analysis from a Chinese national study. J Atheroscler Thromb. 2020;27(6):534–44.
DeBoer MD. Assessing and managing the metabolic syndrome in children and adolescents. Nutrients. 2019;11(8):1788.
Arellano-Ruiz P, Garcia-Hermoso A, Cavero-Redondo I, Pozuelo-Carrascosa D, Martinez-Vizcaino V, Solera-Martinez M. Homeostasis Model Assessment cut-off points related to metabolic syndrome in children and adolescents: a systematic review and meta-analysis. Eur J Pediatr. 2019;178(12):1813–22.
Çin NNA, Yardımcı H, Koç N, Uçaktürk SA, Ok MA. Triglycerides/high-density lipoprotein cholesterol is a predictor similar to the triglyceride–glucose index for the diagnosis of metabolic syndrome using International Diabetes Federation criteria of insulin resistance in obese adolescents: a cross-sectional study. J Pediatr Endocrinol Metab. 2020;33(6):777–84.
Vizzuso S, Del Torto A, Dilillo D, Calcaterra V, Di Profio E, Leone A, et al. Visceral adiposity index (VAI) in children and adolescents with obesity: no association with daily energy intake but promising tool to identify metabolic syndrome (MetS). Nutrients. 2021;13(2):413.
Lin I-T, Lee M-Y, Wang C-W, Wu D-W, Chen S-C. Gender differences in the relationships among metabolic syndrome and various obesity-related indices with nonalcoholic fatty liver disease in a Taiwanese population. Int J Environ Res Public Health. 2021;18(3):857.
Calcaterra V, Verduci E, Schneider L, Cena H, De Silvestri A, Vizzuso S, et al. Sex-specific differences in the relationship between insulin resistance and adiposity indexes in children and adolescents with obesity. Children. 2021;8(6):449.
Dong Y, Bai L, Cai R, Zhou J, Ding W. Visceral adiposity index performed better than traditional adiposity indicators in predicting unhealthy metabolic phenotype among Chinese children and adolescents. Sci Rep. 2021;11(1):1–8.
Dikaiakou E, Vlachopapadopoulou EA, Paschou SA, Athanasouli F, Panagiotopoulos Ι, Kafetzi M, et al. Τriglycerides-glucose (TyG) index is a sensitive marker of insulin resistance in Greek children and adolescents. Endocrine. 2020;70(1):58–64.
García AG, Treviño MVU, Sánchez DCV, Aguilar CA. Diagnostic accuracy of triglyceride/glucose and triglyceride/HDL index as predictors for insulin resistance in children with and without obesity. Diabetes Metab Syndr. 2019;13(4):2329–34.
Moon S, Park J-S, Ahn Y. The cut-off values of triglycerides and glucose index for metabolic syndrome in American and Korean adolescents. J Korean Med Sci. 2017;32(3):427–33.
Yoon JS, Shim YS, Lee HS, Hwang IT, Hwang JS. A population-based study of TyG index distribution and its relationship to cardiometabolic risk factors in children and adolescents. Sci Rep. 2021;11(1):1–9.
Brito ADMd, Hermsdorff HHM, Filgueiras MDS, Suhett LG, Vieira-Ribeiro SA, Franceschini SdCC, et al. Predictive capacity of triglyceride-glucose (TyG) index for insulin resistance and cardiometabolic risk in children and adolescents: a systematic review. Crit Rev Food Sci Nutr. 2021;61(16):2783–92.
Arslan HN, Dundar C, Terzi Ö. Prevalence of overweight and obesity among school children and parents: a cross-sectional study. Rural Remote Health. 2021;21(4):6773.
Baş T. How to Prepare a Questioner? (in Turkish). Ankara: Seçkin Publishing; 2001.
Organization WH. The double burden of malnutrition: priority actions on ending childhood obesity. 2020.
Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 2018;172(6):557–65.
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA. Triglyceride–glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the Vascular-Metabolic CUN cohort. Prev Med. 2016;86:99–105.
Ejtahed H-S, Kelishadi R, Hasani-Ranjbar S, Angoorani P, Motlagh ME, Shafiee G, et al. Discriminatory ability of visceral adiposity index as an indicator for modeling cardio-metabolic risk factors in pediatric population: the CASPIAN-V study. J Cardiovasc Thoracic Res. 2019;11(4):280.
Amato MC, Giordano C. Visceral adiposity index: an indicator of adipose tissue dysfunction. Int J Endocrinol. 2014;2014:730827.
Bredella MA. Sex differences in body composition. In: Mauvais-Jarvis, F. (eds). Sex and gender factors affecting metabolic homeostasis, diabetes and obesity. Advances in Experimental Medicine and Biology. Cham: Springer; 2017;1043:9–27. https://doi.org/10.1007/978-3-319-70178-3_2.
Negrea MO, Neamtu B, Dobrotă I, Sofariu CR, Crisan RM, Ciprian BI, et al. Causative mechanisms of childhood and adolescent obesity leading to adult cardiometabolic disease: a literature review. Appl Sci. 2021;11(23):11565.
Wang HH, Lee DK, Liu M, Portincasa P, Wang DQ-H. Novel insights into the pathogenesis and management of the metabolic syndrome. Pediatr Gastroenterol Hepatol Nutr. 2020;23(3):189.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13(1):1–10.
Huang R, Cheng Z, Jin X, Yu X, Yu J, Guo Y, et al. Usefulness of four surrogate indexes of insulin resistance in middle-aged population in Hefei, China. Ann Med. 2022;54(1):622–32.
Mazidi M, Kengne A-P, Katsiki N, Mikhailidis DP, Banach M. Lipid accumulation product and triglycerides/glucose index are useful predictors of insulin resistance. J Diabetes Complications. 2018;32(3):266–70.
Raimi TH, Dele-Ojo BF, Dada SA, Fadare JO, Ajayi DD, Ajayi EA, et al. Triglyceride-glucose index and related parameters predicted metabolic syndrome in Nigerians. Metab Syndr Relat Disord. 2021;19(2):76–82.
Sánchez-Escudero V, Lacalle CG, Vergaz AG, Mateo LR, Cabrero AM. The triglyceride/glucose index as an insulin resistance marker in the pediatric population and its relation to eating habits and physical activity. Endocrinol Diabetes Nutr (Engl Ed). 2021;68(5):296–303.
Lee J, Lee YA, Lee SY, Shin CH, Kim JH. Comparison of Lipid-Derived Markers for Metabolic Syndrome in Youth: Triglyceride/HDL Cholesterol Ratio, Triglyceride-Glucose Index, and non-HDL Cholesterol. Tohoku J Exp Med. 2022;256(1):53–62.
Angoorani P, Heshmat R, Ejtahed H-S, Motlagh ME, Ziaodini H, Taheri M, et al. Validity of triglyceride–glucose index as an indicator for metabolic syndrome in children and adolescents: the CASPIAN-V study. Eat Weight Disord. 2018;23(6):877–83.
Hagman E, Besor O, Hershkop K, Santoro N, Pierpont B, Mata M, et al. Relation of the degree of obesity in childhood to adipose tissue insulin resistance. Acta Diabetol. 2019;56(2):219–26.
Kumari R, Kumar S, Kant R. An update on metabolic syndrome: Metabolic risk markers and adipokines in the development of metabolic syndrome. Diabetes Metab Syndr. 2019;13(4):2409–17.
Campos RMdS, Masquio DCL, Corgosinho FC, Carvalho-Ferreira JP, Molin Netto BD, Clemente APG, et al. Relationship between adiponectin and leptin on osteocalcin in obese adolescents during weight loss therapy. Arch Endocrinol Metab. 2018;62(3):275–84.
Selthofer-Relatić K, Radić R, Stupin A, Šišljagić V, Bošnjak I, Bulj N, et al. Leptin/adiponectin ratio in overweight patients–gender differences. Diab Vasc Dis Res. 2018;15(3):260–2.
Bharath LP, Choi WW, Cho JM, Skobodzinski AA, Wong A, Sweeney TE, et al. Combined resistance and aerobic exercise training reduces insulin resistance and central adiposity in adolescent girls who are obese: randomized clinical trial. Eur J Appl Physiol. 2018;118(8):1653–60.
Ather U, Shirwany TAK, Imran I, Saleem M, Gul F, Saleem A, et al. Relationship of serum leptin level with chronological age and body mass index in adolescent girls. Ann King Edward Med Univ. 2018;24(2):728–34.
González-Herrera L, Zavala-Castro J, Ayala-Cáceres C, Pérez-Mendoza G, López-González MJ, Pinto-Escalante D, et al. Genetic variation of FTO: rs1421085 T> C, rs8057044 G> A, rs9939609 T> A, and copy number (CNV) in Mexican Mayan school-aged children with obesity/overweight and with normal weight. Am J Hum Biol. 2019;31(1):e23192.
Guclu-Geyik F, Onat A, Yuzbasıogulları AB, Coban N, Can G, Lehtimäki T, et al. Risk of obesity and metabolic syndrome associated with FTO gene variants discloses clinically relevant gender difference among Turks. Mol Biol Rep. 2016;43(6):485–94.
Pérez-Castro E, Godínez-Jaimes F, Vázquez-Medina MU, Ocharan-Hernández ME, Vargas-De-León C. Derivation and validation of sex-specific continuous metabolic syndrome scores for the Mexican adult population. Sci Rep. 2022;12(1):1–11.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CD: Conceptualization (lead); writing – original draft (lead); statistical analysis (lead); writing – review and editing (equal). OT: writing – original draft (supporting); writing – review and editing (equal); statistical analysis. HNA: Writing – original draft (supporting); statistical analysis; writing – review, and editing (equal). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was completed in accordance with the Declaration of Helsinki as revised in 2013. Participants and their guardians were informed about the study, and informed consent was obtained from all children and their legal guardians. The Clinical Research Ethics Committee of Ondokuz Mayis University (KAEK: 2018/1936) approved the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dundar, C., Terzi, O. & Arslan, H.N. Comparison of the ability of HOMA-IR, VAI, and TyG indexes to predict metabolic syndrome in children with obesity: a cross-sectional study. BMC Pediatr 23, 74 (2023). https://doi.org/10.1186/s12887-023-03892-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-03892-8