Abstract
Background
Stress urinary incontinence (SUI) is a common social problem that affect about 4–35% of adult women adult. There are multiple surgical options for treatment of SUI but midurethral slings are the most effective and durable form of treatment. In this study, transobturator vaginal sling (TOT-VS, Elgamasy technique) was used to overcome the unique risks associated with synthetic mesh placement, as well as the higher rate of voiding dysfunction and harvest site complications associated with pubovaginal sling placement.
Objective
To assess the short-term outcome of transobturator vaginal wall sling (TOT-VS) for the treatment of SUI.
Materials and Methods
This is a prospective study included 20 females who underwent TOT-VS placement for SUI from January 2021 to March 2022 at Tanta Urology Department–Tanta University Hospitals. Two-parallel longitudinal vaginal mucosal incisions were performed 2 cm below the bladder neck, and 6 × 2 cm graft was harvested from the anterior vaginal wall, with a prolene suture on each side and fixed around the urethra via the transobturator rout. Patients were followed in the outpatient clinic after one week, two weeks, 3, 6 months and one year postoperatively. Outcomes were measured subjectively by the Bristol Female Lower Urinary Tract Symptoms (B-FLUTS) score comparing preoperative and postoperative scores and objectively by cough stress test.
Results
The median age of patients was 42 years, and the median BMI was 30.0 kg/m2. The technique was performed, and the patient was discharged the next day after surgery. Mean operative time was 50.5 ± 9 min. All patients completed B-FLUTS at the last follow-up. Compared to preoperative scores, all patients showed significant improvement in all domains. Nineteen cases (95%) showed negative cough stress test 6 months postoperatively, and none of them suffered from severe (Clavien III-V) complications or required reoperation to release the sling. The procedure was failed in one case (5%). At one-year follow-up, no recurrence of SUI was recorded in any case.
Conclusion
In the treatment of female stress urinary incontinence, transobturator vaginal wall slings can be a viable, autologous and cost-effective option with excellent short-term outcome, no recurrence, short operative periods, minor complications and short hospital stays.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.1 Introduction
Stress urinary incontinence (SUI) is the involuntary leakage of urine on exertion, or sneezing or coughing which is a common social problem with high prevalence as it affects between 4 and 35% of the adult women with higher rates in older women [1].
There are a multiple options for the treatments of SUI but the most durable and effective method is midurethral slings [2]. There are of two types of slings, synthetic mesh and autologous sling that commonly harvested from rectus fascia, fascia lata and vaginal mucosa. In the last twenty years, the synthetic midurethral sling (MUS) has been considered the gold standard surgical treatment for index SUI patients after failure of conservative treatments [3, 4].
Recently, after the initial Food and Drug Administration notification on mesh use in pelvic surgery, many healthcare providers and patients shift to the non-mesh alternatives in SUI surgery in spite of the proven safety and efficacy of MUS by SUFU/AUGS and AUA guidelines [5].
The autologous sling, obtained from the fascia lata, was first described in the 1930s, while the first use of rectus fascia sling was in the 1940s [6]. A fifty years later, Raz et al. first described the vaginal wall slings with reports of a 94.4% success rate at 4 years [7, 8].
Although the autologous pubovaginal sling is a surgical option for management of SUI [9, 10], it is associated with a risk of postoperative voiding dysfunction which also notable with synthetic sling placement via the retropubic approach. This complication is less frequent with the transobturator approach [11].
In this study, TOT-VS (Elgamasy technique) was used to eliminate the unique risks associated with synthetic mesh placement, as well as the higher rate of voiding dysfunction and harvest site complications associated with pubovaginal sling placement. In this pilot study, the short-term outcomes of patients who underwent TOT-VS were evaluated.
2 Materials and methods
Approval by the ethical committee review board (Approval code: 34,724/6/21) was done, and written consents were obtained from every participant. This study was conducted according to the principles expressed in the Declaration of Helsinki.
In this prospective study, the outcomes of 20 female SUI patients who underwent TOT-VS placement for management of bothersome symptomatic SUI from January 2021 to March 2022 in Tanta Urology Department—Tanta University Hospitals were evaluated.
Our objective is to assess the short-term outcome of transobturator vaginal wall sling (TOT-VS) for the treatment of female stress urinary incontinence.
Inclusion criteria included female patients with SUI and clinically positive cough stress test. Also, female patients with mixed urinary incontinence with predominant stress component were included. Exclusion criteria included patients with history of failed previous anti-incontinence surgery, mixed urinary incontinence with prominent urge component, repeated transvaginal surgeries or massive complicated pelvic surgeries and cases with high post-voiding residual urine volume or presence of underactive detrusor, cases of grade 3 pelvic organ prolapse and presence of active urinary tract infection. Also, cases of previous pelvic irradiation and bleeding disorders were excluded.
Patients were assessed preoperatively with a history and physical examination, urinalysis, urine culture, 24-hour urinary bad test, ultrasound measurements of post-void residuals, uroflowmetry, the Bristol Female Lower Urinary Tract Symptoms (B-FLUTS) score filled by the aid of the physician and urodynamic evaluation in case of mixed urinary incontinence. All female SUI patients agreed to proceed with TOT-VS following discussion of their available treatment options. All procedures were performed by a single surgeon.
Steps as seen in the Additional file 1: video (Elgamasy technique):
Link:
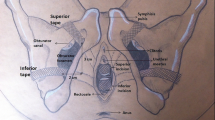
Under spinal anesthesia, the patient was placed in the lithotomy position with external rotation of legs, draped as usual, and the Foley’s catheter 16 Fr. was inserted. We placed a vaginal retractor or four traction vaginal sutures and then used saline mixed with adrenaline to hydro-dissect the anterior vaginal mucosa. Two-parallel longitudinal vaginal mucosal incisions were performed 2 cm below the bladder neck (about 6 cm long and 2 cm wide). A combination of blunt and sharp dissections was used to separate the vaginal graft completely (Fig. 1). Dissection was then carried out bilaterally toward the inferior pubic rami.
The graft was deflated and prepared by making multiple longitudinal incisions in the mucosal surface followed by two prolene suspension sutures (No 1) at both lateral edges (Fig. 2). During the procedure, two stab incisions (2 cm) were made in the thigh at the level of clitoris, and a curved C-shaped trocar was passed twice (with 2 cm away between the upper and lower border of the thigh incision) through each obturator foramen under finger guidance and the prolene sutures of the vaginal graft were guided by the needle from the vagina back to the thigh. The graft was fixed to the periurethral tissue (with the smooth side of the graft over the urethra and the vaginal mucosal side outside) the by 4/0 vicryl sutures in order to prevent it from rolling around the urethra (Fig. 3). Tying of the prolene sutures at both sides was done without tension (with an instrument was placed between the urethra and the graft to prevent overcorrection). In the presence of cystocele and/or rectocele, repair was done in the usual way. Finally, closure of the vaginal incision and insertion of a vaginal pack were done. Perioperative complications were evaluated using the Clavien-Dindo classification.
At postoperative day 1, the urethral catheter and vaginal pack were removed, and the patient was discharged after ensuring normal voiding with insignificant post-voiding residual (PVR). In the outpatient clinic, patients were followed up after one week, two weeks, three, 6 months and one year. Urine analysis was routinely performed with each visit. The first visit involves the assessment of the vaginal incision and PVR by ultrasound, while in the second visit check the vaginal incision healing. Our last visit involved a subjective evaluation of the outcome based on B-FLUTS filled by the aid of the physician as well as an objective evaluation based on the cough stress test and uroflowmetry test.
2.1 Statistical analysis
All the statistical analyses were carried out with the Statistical Package for Social Sciences software (SPSS version 21). All statistical tests were two-sided, with a p-value < 0.05 considered statistically significant.
3 Results
During the timeframe of the study, 20 patients underwent TOT-VS placement for SUI. Patients median age was 42.0 (39.0–50.75) years old with a median body mass index of 30.0 kg/m2 (25.0–33.0) as shown in Table 1. We had 3 cases with medical history of diabetes mellitus, 2 cases with hypertension and 4 cases had both diabetes and hypertension as shown in Table 1. The mean parity of the included patients was 3.8 ± 1.37 as shown in Table 1. The median preoperative uroflow was 24 ml/sec as shown in Table 2. Notably, all cases were performed for symptomatic stress urinary incontinence, as verified on office cough stress test, number of daily used pad, and 24-h pad test with 14 cases with stress incontinence and 6 cases with mixed urinary incontinence with prominent stress component as shown in Table 1. For the filling, voiding, incontinence, sexual, and quality-of-life components of the preoperative Bristol FLUTS, the respective medians were 3.5, 1, 12, 1 and 16.5 as shown in Table 3.
Isolated sling placement was performed in 8 (40%) cases, Concomitant procedures included anterior and/or posterior colporrhaphy (n = 12), The median operative times were 42 and 47.5 min when TOT-VS was performed alone or with POP repair, respectively, as shown in Table 4. No complications were encountered during the procedure. Any patient with active UTI was excluded preoperatively, none of our patients had positive culture in the preoperative assessment, and none of our cases presented by any symptoms of UTI postoperatively. All patients had normal urine analysis during the regular follow-up.
At the last follow-up appointment, all of the cases completed B-FLUTS and underwent uroflowmetry.
Regarding B-FLUTS score, there was significant improvement in all symptom and bother scores from baseline preoperative levels, including the filling (p = < 0.001), voiding (p = 0.046), incontinence (p = < 0.001), sexual (p = 0.012) and quality of life (p = < 0.001) subscores as shown in Table 3, with no significant difference between the pre- and postoperative Q-max (p = 0.080) as shown in Table 2; none of our cases continued to use pad except in one case (Table 5). All cases of SUI with cystocele and/or rectocele cured with no recurrence for either incontinence or pelvic floor prolapse (Table 6).
With regard to complications from vaginal wall sling placement, no patients required sling release for postoperative voiding dysfunction. Three patients had leg pain and responded well to the medical treatment. Likewise, no patients suffered severe (Clavien III-V) postoperative complications. At the end of the study (one-year follow-up, Table 7), 19 patients (95%) remained continent and only one patient (5%) had positive cough test and considered failure.
4 Discussion
Urinary incontinence (UI) affects women of all ages and races. The most commonly reported type of UI is stress urinary incontinence (SUI), which occurs when exert effort, sneeze, or cough. In spite of the fact that all subtypes of UI are a significant burden for individuals and healthcare systems, SUI is the most amenable to surgical correction [12].
Over the years, surgery to resolve this problem has become less invasive, and a variety of options are available. Among all of these options, mid‐urethral sling operations (either synthetic or autologous) are commonly undertaken to try and cure stress urinary incontinence [5, 9].
Autologous fascial slings, particularly the pubovaginal, had been the gold standard for the treatment of SUI for many decades, and they are the godfather of medurethral sling [13]. The synthetic mid-urethral sling became the gold standard treatment for SUI after its introduction. However, in July 2011, the FDA warned against the use of synthetic mesh in transvaginal pelvic organ prolapse repair due to reported complications [14]. Despite FDA notifications not including mesh used to treat stress urinary incontinence, this warning forces many patients and healthcare providers for renaissance of autologous slings [15].
Although an autologous pubovaginal sling is an option for the management of SUI, it may cause postoperative voiding dysfunction [9, 10]. This is notable with synthetic sling placement via the retropubic approach. With the transobturator approach, this complication is less common [16].
By using the transobturator vaginal wall sling as part of this study, we avoided the inherent risks associated with synthetic mesh placement [17, 18]. In addition, we eliminated the increased risk of voiding dysfunction and harvest site complications associated with pubovaginal sling placement [10].
Various technique modifications have been made to the vaginal wall sling since its introduction by Raz et al. in 1989, all of these techniques use the retropubic approach [9]. Recently, autologous transobturator rectus fascial mid-urethral sling appeared safe and successful in the short-term follow-up [19]. However, no one before used the transobturator approach (in the current study) for the vaginal sling.
The vaginal wall sling and pubovaginal rectus sling were compared by Kaplan et al. in 1996. It was found that both techniques have comparable efficacy and the vaginal sling group had a short operative time, decreased persistent urges postoperatively, and shorter hospital stays and catheterizations [20].
In this study, twenty consecutive women followed up for one year found excellent results with TOT-VS placement. All cases had no postoperative voiding dysfunction necessitating sling release with no major (Clavien III-V) complications. By assessing short-term outcomes, we augment our initial series that suggested technical feasibility.
In this study, the median age was 42.0 years old and the median body mass index was 30.0 kg/m2. A total of thirteen cases of stress incontinence were operated on, as well as seven cases of mixed urinary incontinence with a prominent stress component. Eight of our cases required isolated sling placement. Concomitant procedures including anterior and/or posterior colporrhaphy were done in 12 cases. The median operative time was 47.5 min. When the procedure was done alone, the median operative time was 42 min. No complications were encountered during the procedure. We did not find any difference between isolated sling placement with or without POP repair except in the operative time which was longer if POP repair was done. Another study with a big number of cases is needed to clarify this point.
Although the median operative time was 47.5 min, it is still short compared to the operative times of the traditional pubovaginal sling which are usually over one hour as most literature mentions [21, 22].
There was a significant improvement in all subscores of the Bristol FLUTS from preoperative baseline levels, which subjectively supports our new technique. A successful outcome is also implied by the fact that all cough tests were negative in 19 patients (95%) at one-year follow-up.
Our objective and subjective success rates were comparable to Raz et al., and they first introduced the use of vaginal wall slings in the treatment of 160 patients with either urethral hypermobility or intrinsic sphincter deficiency. Despite the fact that their results showed 7% for de novo urge incontinence and 9% for urge incontinence [7, 8], in the current study, these problems were not encountered. Even in mixed urinary incontinence, none of the patients required any additional postoperative medical treatment, may be due to the small number of the patients in the current study.
In terms of postoperative voiding dysfunction, we have not encountered any cases with acute urine retention or sling release. There was no significant difference between the pre- and postoperative flow rates. The transobturator approach used in this new technique has been shown to be the reason for avoiding this problem.
The vaginal wall sling is an autologous one with no cost and also provides a shorter hospital stay and no harvest site complications compared to standard pubovaginal slings [23], with all cases in the present study discharged after 24 h.
In this study, no complications were recorded except three cases of groin pain and were responded well to the medical treatment; this in contrary to cases of synthetic med urethral TOT sling, the pain was severe and not responding to any medication and the only solution was the unavoidable difficult removal of the tape [17, 18]. In this study, the pain is less as the prolene sutures are traversing the thigh muscles and tied in the subcutaneous area over the muscle; however, in classic TOT the synthetic tape is wider and making more injury, inflammation, fibrosis and subsequently more pain to the patient.
To our knowledge, this is the first study that used the transobturator approach in suspension of the vaginal wall sling, and we use this technique due to many advantages which mentioned before.
This study has limitations due to the fact that it was conducted at a single center and one single surgeon. Another limitation, the procedure is difficult in relatively narrow vagina; however, it is easy in cases of concomitant cystocele with redundant vaginal mucosa. Additionally, the study had a small sample size and a short follow-up period. A future study should incorporate long-term follow-ups and a large sample size in order to make further conclusions. In addition, another studies are needed to evaluate multiple parameters such as cases with concomitant POP, cases of pure SUI versus MUI, postoperative denovo urgency, and postoperative obstructive symptoms.
5 Conclusion
In the treatment of female stress urinary incontinence, transobturator vaginal wall sling can be a viable, autologous and cost-effective option with excellent short-term outcome, less recurrence, short operative periods and short hospital stays.
Availability of data and materials
Not applicable.
Abbreviations
- SUI:
-
Stress urinary incontinence
- TOT-VS:
-
Transobturator vaginal wall sling
- B-FLUTS:
-
Bristol Female Lower Urinary Tract Symptoms
- MUS:
-
Midurethral sling
- PVR:
-
Post-voiding residual
- UI:
-
Urinary incontinence
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
References
KM Luber 2004 The definition, prevalence, and risk factors for stress urinary incontinence Rev Urol 6 Suppl 3 S3
G Ghoniem J Hammett 2015 Female pelvic medicine and reconstructive surgery practice patterns: IUGA member survey Int Urogynecol J 26 10 1489 1494
CR Chapple F Cruz X Deffieux AL Milani S Arlandis W Artibani 2017 Consensus statement of the European Urology Association and the European Urogynaecological Association on the use of implanted materials for treating pelvic organ prolapse and stress urinary incontinence Eur Urol 72 3 424 431
A Elgamasy O Elashry MA Elenin H Eltatawy M Elsharaby 2008 The use of polypropylene mesh as a transobturator sling for the treatment of female stress urinary incontinence (early experience with 40 cases) Int Urogynecol J Pelvic Floor Dysfunct 19 6 833 838
RR Dmochowski JM Blaivas EA Gormley S Juma MM Karram DJ Lightner 2010 Update of AUA guideline on the surgical management of female stress urinary incontinence J Urol 183 5 1906 1914
AH Aldridge 1942 Transplantation of fascia for relief of urinary stress incontinence Am J Obstet Gynecol 44 3 398 411
S Raz AL Siegel JL Short JA Synder 1989 Vaginal wall sling The J urol 141 1 43 46
S Juma NA Little S Raz 1992 Vaginal wall sling: four years later Urology 39 5 424 428
A Elgamasy T Jameel M Redwan 2017 Use of modified fascial pubovaginal sling for the treatment of stress urinary incontinence: up to 20 years follow up J Urol 197 4S Supply e523
G Ghoniem A Shaaban 1994 Sub-urethral slings for treatment of stress urinary incontinence Int Urogyn J 5 228 239
BJ Linder DS Elliott 2016 Autologous transobturator urethral sling placement for female stress urinary incontinence: short-term outcomes Urology 93 55 59
WS Reynolds RR Dmochowski DF Penson 2011 Epidemiology of stress urinary incontinence in women Curr Urol Rep 12 5 370 376
D Taha B Wadie 2015 Pubovaginal sling, the godfather of midurethral slins that remained so J of Acute disease 4 2 91 96
J Geelen Van P Dwyer 2013 Where to for pelvic organ prolapse treatment after the FDA pronouncements? Int Urogynecol J 24 5 707 718
G Ghoniem D Rizk 2018 Renaissanace of the autologous pubovaginal sling Int Urogynecol J 29 177 178
EJ Stanford MFR Paraiso 2008 A comprehensive review of suburethral sling procedure complications J Minim Invasive Gynecol 15 2 132 145
J Laufer S Scasso V Bentancor 2019 Autologous transobturator sling as an alternativetherapy for stress urinary incontinence Int J Gynaecol Obstet 145 3 300 305
JR Miklos O Chinthakanan RD Moore DR Karp GM Nogueiras GW Davila 2016 Indications and complications associated with the removal of 506 pieces of vaginal mesh used in pelvic floor reconstruction: a multicenter study Surg Technol Int 26 29 185 189
P Vasudeva V Tyagi N Kumar 2021 ″Mesh free″ autologous transobturator mid urethral sling placement for predominant stress urinary incontinence: a pilot study Neurourol Urodyn 40 2 659 665
SA Kaplan AE Te GP Young A Andrade MA Cabelin EF Ikeguchi 2000 Prospective analysis of 373 consecutive women with stress urinary incontinence treated with a vaginal wall sling: the Columbia-Cornell University experience J Urol 164 5 1623 1627
Ö Bayrak D Osborn WS Reynolds RR Dmochowski 2014 Pubovaginal sling materials and their outcomes Turkish journal of urology 40 4 233
SL Brown FE Govier 2000 Cadaveric versus autologous fascia lata for the pubovaginal sling: surgical outcome and patient satisfaction J Urol 164 5 1633 1637
DG Wong S Kim A Christie T Rawlings G Lemack P Zimmern 2020 Cost analysis of vaginal anti-incontinence procedures at a tertiary care center Urology 141 50 54
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
The author designed the study, collected the data, performed the analysis, and wrote the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the local ethical committee (Approval code: 34724/6/21Tanta University, Egypt) before the start of this study. The study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards Informed consent: The procedures with its possible complications were discussed with all patients, and informed consent was obtained from the subjects of this study before the beginning of the procedures. Patients’ confidentiality was regarded and maintained along this study.
Particular special issue
Female urology.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
*Accepted and presented (Video V 009) at European Association of Urology meeting, Milan Italy March 10-13, 2023. AM23-3935.
Supplementary Information
Additional file 1. Conclusion.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Elgamasy, A.K. Transobturator vaginal wall sling (Elgamasy technique) for the treatment of female stress urinary incontinence: a pilot study. Afr J Urol 30, 23 (2024). https://doi.org/10.1186/s12301-024-00421-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-024-00421-6