Abstract
Introduction and hypothesis
The aim of this study is to describe the use of ordinary polypropylene mesh and our modified helical passers through a transobturator vaginal tape inside-out technique (TVT-O) as a low-cost alternative to available commercial kits in the treatment of stress urinary incontinence (SUI) with evaluation of its long-term safety and efficacy. This is important in developing countries due to limited health care resources.
Methods
Tailored (11 × 1.5 cm) polypropylene tape was inserted in 59 women from June 2006 to June 2009 at the Urology Department, Cairo University Hospitals as an open prospective study. SUI was diagnosed by positive cough stress test (CST) and abdominal leak point pressure (ALPP). Patients with post-void residual urine (PVRU) > 100 ml, bladder capacity < 300 ml, or neurological lesions were excluded. The Stress and Urge Incontinence and Quality of Life Questionnaire (SUIQQ), urodynamic parameters, and other variables were compared pre- versus postoperatively with paired t, Wilcoxon signed rank, McNemar, or chi-square tests.
Results
The mean age was 47.47 ± 8.52 years. Twenty-one (35.6 %) patients had intrinsic sphincter deficiency (ISD). The mean operative time was 21.22 ± 4.26 min (15–30). Procedures for prolapse were done in four (6 %) patients. Complications were vaginal discharge (6 %), dyspareunia (1 %), groin pain (20 %), urinary tract infection (3 %), obstructive symptoms (1 %), accidental cut of polypropylene suture (1 %) and felt subcutaneous polypropylene sutures (3 %). We had no cases of erosions or de novo urgency. SUIQQ indices improved significantly, while urodynamic parameters showed no significant difference postoperatively. Of the patients, 54 (91 %) were cured and 3 (5 %) improved, while failure was detected in 2 (3 %) patients.
Conclusions
Our technique is safe with excellent 5-year results. It should be considered as a low-cost alternative to available commercial kits in the treatment of SUI mainly for public health systems with few financial resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The tension-free vaginal tape (TVT) for the surgical correction of female stress urinary incontinence (SUI) was first described in 1996 by Ulmsten et al. [1]. Different complications were reported as a consequence of the passage of the needles through the retropubic space including bladder perforation, hematoma, bowel perforation, and vascular and nerve lesions [2]. Subsequently, transobturator tapes [outside-in (TOT) and inside-out (TVT-O)] were developed in order to perform less invasive surgical procedures with fewer complications [3, 4]. Although these surgical techniques have a satisfactory outcome, they require special needles or passers and prefabricated slings. Their cost is too high to be afforded by most patients in many parts of the world.
Therefore, we describe a new procedure based on the surgical principles of TVT-O using a tailored ordinary polypropylene mesh with evaluation of its long-term safety and efficacy as a low-cost alternative to the available commercial kits in the treatment of female SUI.
Patients and methods
The polypropylene tape was inserted in 59 women using the TVT-O technique in the period from June 2006 to June 2009 at the Urology Department, Cairo University Hospitals as an open prospective study (Fig. 1).
Women complaining of SUI (involuntary loss of urine on effort or physical exertion, or on sneezing or coughing) were evaluated by the cough stress test (CST) and abdominal leak point pressure (ALPP). Associated urgency (a sudden compelling desire to pass urine which is difficult to defer), urgency urinary incontinence (UUI) (involuntary loss of urine associated with urgency), intrinsic sphincter deficiency (ISD), or previous surgeries were not a contraindication (provided that UUI is not the predominant component). Informed consent was received from all patients after approval of the study by the local Ethics Committee.
Preoperative evaluation included complete urogynecological history and examination. Severity of symptoms and quality of life (QOL) were evaluated according to the Stress and Urge Incontinence and Quality of Life Questionnaire (SUIQQ) [5]. The questionnaire consists of QOL index (0–16 score), SUI index (0–12 score), and UUI index (0–8 score). Positive urinary cultures were treated with specific antibiotics before any intervention. Abdominal and pelvic ultrasound (US) was done to evaluate the kidneys and the bladder and to exclude the presence of any post-void residual urine (PVRU). Free flowmetry was performed. Filling cystometry was done for each patient to assess the maximum cystometric capacity, compliance, presence of detrusor overactivity (DO), any leakage, and ALPP. Pressure flow study was done to assess the maximum flow rate (Qmax), the detrusor pressure at maximum flow rate (PdetQmax), and any PVRU. We compared these parameters with postoperative findings.
Patients with PVRU >100 ml, bladder capacity <300 ml, impaired bladder compliance, neurological lesions, or urogenital prolapse more than grade 2 (according to the Baden and Walker classification) were excluded. Patients with symptomatic prolapse were included but additional repair was done.
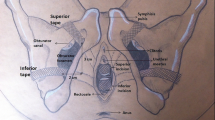
Specifically designed surgical instruments
We modified the helical passers that were originally designed by de Leval [3]. They are pairs of stainless steel instruments, specific for the left and right sides, comprising a spirally shaped section and a handle. The spiral section comprises an open circular segment having a 3-cm radius terminated by two linear segments with a blunt tapered distal end. The passer is fenestrated at the tip, which allows the insertion of polypropylene sutures that were attached intraoperatively to both ends of the polypropylene mesh strip. On a horizontal plane perpendicular to the handle’s axis, the gap between the extremities of the spiral section is 2 cm. Our modified helical passers have the advantage of being resterilizable. They can be reused decreasing the treatment expenses (Fig. 2).
Preparation of the polypropylene mesh
A strip of about 11 cm in length and 1.5 cm in width was manually tailored from the commercially available 11×6 cm nonabsorbable monofilament polypropylene mesh (Prolene®, Polypropylene Mesh, Ethicon Ltd, Bracknell, UK) (the same mesh used in herniorrhaphy). Each end of the 11×1.5 cm polypropylene tape was anchored with a zero polypropylene suture in a figure-of-eight fashion. The polypropylene suture was then inserted into the “eye” at the end of the passer.
Surgical technique
The repair was done under spinal anesthesia in the lithotomy position with thighs in hyperflexion (120°). During induction of anesthesia and positioning of the patient, the polypropylene sling was prepared. Antibiotic prophylaxis with 1 g of third-generation cephalosporin was administered before the procedure. The bladder was emptied by a Foley catheter. Submucosal saline injection was done (hydrodissection) to elevate the vaginal mucosa easing the dissection. The technique was done similar to that originally described by de Leval [3]. When the pointed tip of the passer appeared at the skin exit points (or alternatively, the skin was incised over the pointed tip of the passer), the polypropylene sutures were extracted from the passer (Fig. 3). The passer was then removed by a backward rotational movement. The same technique was applied to the other side. Cystourethroscopy was done to rule out any injury produced by helical passers. The tape was then aligned midway between the urethral meatus and bladder neck and adjusted by simultaneous pulling on the polypropylene sutures on both sides without twisting the tape. Tension was controlled by passing a clamp between the tape and the urethra. The polypropylene sutures attached to both ends of the tape were fixed to the deep fascia on both sides at the exit points using a French eye needle without exerting any tension on the tape (Fig. 3). The anterior vaginal wall was closed by interrupted absorbable 3-0 sutures. A vaginal pack soaked with povidone-iodine (Betadine) was used for 12 h. Then, it was removed together with the urethral catheter. Patients were discharged if they had no PVRU in the postoperative US following removal of the urethral catheter. In cases associated with prolapse surgery, a bladder catheter was maintained to the second postoperative day. Fluoroquinolones and metronidazole were prescribed postoperatively in addition to a vaginal douche. Follow-up was done every 2 weeks during the first month, then every 6 months. Administration of the SUIQQ and urodynamic study were done 5 years postoperatively to assess the long-term outcome.
Extraction and fixation of polypropylene sutures at the skin exit points. a The pointed tip of the helical passer appeared at the skin exit points. b The polypropylene sutures attached to both ends of the tape are extracted from the passer. c After alignment and adjustment of the tape, the polypropylene sutures are passed through the French eye needle. d The polypropylene sutures are fixed to the deep fascia on both sides at the exit points using a French eye needle without exerting any tension on the tape
Finally, patients were categorized as cured if no SUI occurred, subjectively (absence of complaint of leakage) and objectively (absence of leakage on CST and urodynamics). The patients were considered improved if SUI was still present but to a milder degree than preoperatively, subjectively (improved SUIQQ) and objectively [marked increase in the activity that induced urine leakage than it was preoperatively (ALPP)]. Failure was documented if SUI was still the same or worse than before surgery (worse SUIQQ or ALPP).
All statistical calculations were done using the computer program Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows. Comparison of quantitative variables between baseline and the 5-year follow-up was done with the paired t test (if normally distributed) or with the Wilcoxon signed rank test (if not normally distributed). Comparison of dichotomous variables was done with the McNemar test. Comparison of categorical data between the study groups was done using the chi-square (χ2) test. A probability value (p value) <0.05 was considered statistically significant.
Results
The mean follow-up was 61.67 ± 7.39 months (Fig. 1). The perioperative data are presented in Table 1. Postoperative vaginal discharge was found in four (6 %) cases. Treatment was given in the form of oral antibiotics, local metronidazole, and local antiseptics. The polypropylene sutures had been cut accidentally in one (1 %) patient during an attempt to pull the sutures outside the helical passer after its passage through the skin at the thigh folds. Withdrawal of the passer and reinsertion of new sutures into the end of the tape and reintroduction of the passer into the obturator canal again was then mandatory at this side. This prolonged the total operative time. Twelve (20 %) patients complained directly after the procedure that they had pain or discomfort in the thigh folds and groin. This symptom was controlled in all cases by non-opioid analgesics. The groin pain persisted for a few days in most patients and disappeared completely within 4 weeks in all patients. The polypropylene sutures were felt subcutaneously in two (3 %) patients with mild discomfort. We had no cases of postoperative urinary retention, erosions, or mesh exposure. One (1 %) patient had obstructive urinary symptoms that persisted for a few days. Other complications included dyspareunia (1 %) and urinary tract infection (UTI, 3 %) (Table 1).
Of the patients, 54 (91 %) were cured and 3 (5 %) improved, while failure was detected in 2 (3 %) patients. The present study showed no statistically significant difference in the outcome according to the presence or absence of ISD (p =0.457) (Table 2). There was no significant difference in the outcome between patients without prolapse versus patients with associated prolapse (all types) (p =0.405) or patients with associated cystocele (p =0.510) (Table 2). Associated prolapse repair was done for four patients. These four patients had no DO pre- or postoperatively. Two of these patients had preoperative urgency which was cured postoperatively.
The postoperative SUI, UUI, and QOL indices were improved significantly (Table 3). Comparison between pre- and postoperative maximum cystometric capacity, compliance, Qmax, PdetQmax, and free Qmax showed no significant difference (Table 4). The pre- and postoperative PVRU were negligible.
No postoperative de novo urgency or de novo UUI were reported. Urgency decreased from 23 (39 %) patients preoperatively to 7 (11 %) patients postoperatively (p <0.001). UUI decreased from 19 (32 %) patients preoperatively to 7 (11 %) patients postoperatively (p <0.001). UUI improved on anticholinergics in four of the seven patients with persistent postoperative UUI. Four (6 %) patients had DO preoperatively. The involuntary contractions were mild and did not exceed 20 cmH2O. They complained of urgency and UUI. Postoperatively, DO disappeared in three patients and persisted in the last patient (Table 4).
The cost of our tailored mesh was about US$10. This is lower than the cost of the commercially available TVT-O by 50 times (according to local prices).
Discussion
The cost-effectiveness of the commercially available kits for the treatment of female SUI has been questioned [6–9]. Many surgeons tried to overcome this cost by tailoring off-the-shelf polypropylene mesh and inserting it as a midurethral sling [6–9]. The safety and efficacy of surgeon-tailored polypropylene mesh have been proven when used as TOT [8]. The present study may be the first one that evaluates the use of ordinary polypropylene mesh using TVT-O. This reduces the material cost from US$500 to about US$10, which is very important in developing countries due to limited health care resources. Our modified helical passers have the advantage of being resterilizable. They can be reused decreasing the treatment expenses.
Chen and colleagues reported TVT-O using 1 × 15 cm tailored polypropylene mesh (Gynemesh) and modified helical needles in 80 patients with 1-year follow-up [9]. The mean age was 65 years (older than the present study by 17 years), while the mean vaginal deliveries was two times. No patient had associated prolapse, a previous anti-incontinence surgery, or prolapse repair. They excluded patients with mixed symptoms of SUI and UUI, urgency, or dysuria. They did not report the number of patients with ISD as they did not use urodynamics in the diagnostic workup. The mean operative time was 15 min (range 6–22). Of the 80 patients, 75 (93.8 %) were cured and 5 (6.2 %) were improved; no failure occurred. Three (3.8 %) patients showed urinary retention. Recatheterization was performed for 48 h. Groin pain was reported by 15 (18.8 %) patients. Pain was not reported by any patient 1 month postoperatively [9]. Although we did not exclude patients with prolapse or previous surgery or patients with mixed UI or ISD, we had comparable results using the ordinary mesh. Our operative time is more by 6–7 min when compared to this study or other studies using the ordinary TOT or TVT-O techniques. The increased operative time in our technique is due to bilateral fixation of the suspension sutures into the deep fascia and covering these nonabsorbable sutures with subcutaneous tissue. Moreover, we used cystoscopy to evaluate this new technique. Although cystoscopy is mandatory in special conditions such as presence of associated prolapse or previous surgery, it can be omitted in most straightforward cases. In the present study, there was no significant difference in the outcome as regards associated prolapse and previous anti-incontinence surgery. We used the CST and urodynamic parameters such as ALPP for objective assessment, while the SUIQQ was used as a subjective parameter.
Latthe and colleagues reviewed the randomized controlled trials (RCT) that compared TVT-O (five RCT) or TOT (six RCTs) versus TVT. The number of patients in TVT-O groups in these studies ranged from 27 to 131 with a follow-up period mostly around 1 year. Some studies excluded patients with prolapse or previous failed surgery. The reported complications were vaginal erosions (2/188 patients, 1.06 %), groin and thigh pain (25/159 patients, 15.7 %), de novo urgency (13/71 patients, 18.3 %), retention and voiding difficulties (12/215 patients, 5.58 %), and bladder perforation (0/291). The cure rate ranged from 85.7 to 95.4 %. The reported means for operative time ranged from 16 to 29 min [10].
Our results were nearly similar to these studies with 91 % cure, 5 % improvement, and 3 % failure. However, the results may have been improved by the relatively younger age of patients in the present study. Although we did not exclude patients with previous failed anti-incontinence surgery, we had only three patients (5 %) in the present study and another four patients (4 %) with associated prolapse repair. On the other hand, we had no cases complicated by erosion or mesh exposure, vaginal or bladder perforations, de novo urgency, or de novo UUI. Other complications were nearly comparable (groin pain, UTI). We had other mild complications related to our modified technique. The figure-of-eight polypropylene sutures at the end of the tape had been cut accidentally in one patient. This prolonged the total operative time. The polypropylene sutures were felt subcutaneously in another two patients with mild discomfort.
Zullo and colleagues compared TVT (35 patients) vs TVT-O (37 patients). At the 12-month follow-up of the TVT-O group, 33 (89 %) patients were successfully treated (CST during urodynamics). As regards urodynamic parameters, no statistically significant differences were found from baseline to the 12-month follow-up in the maximum cystometric capacity and PdetQmax, while the mean Qmax showed a significant reduction from 26.6 ± 5.5 to 22.4 ± 3.8 ml/s [11]. In the present study, we had no significant difference between pre- and postoperative urodynamic parameters.
We had significant improvement in urgency, UUI, and DO postoperatively. No postoperative de novo urgency or de novo UUI were reported. A meta-analysis was performed by Jain and colleagues to evaluate the effectiveness of midurethral slings in women with mixed incontinence. The overall cure of urgency and the UUI component was 30–85 %. The cure rate of SUI varied from 85 to 97 % [12]. There are several theories to explain the cure of UUI following midurethral slings. With a weak urethral sphincter, the urine may enter the proximal urethra due to its funneling during any increase in intra-abdominal pressure. This produces sensory stimulation and reflex bladder contraction [13]. After midurethral slings, the reflex urgency is avoided as the urine is prevented from entering into the posterior urethra during rise of intra-abdominal pressure [14]. Papa Petros demonstrated also that midurethral slings can relieve urge symptoms and even unstable detrusor contractions due to prevention of inappropriate activation of the micturition stretch receptors [15].
Some studies have used the maximum urethral closure pressure (MUCP) to identify patients with ISD [16, 17]. Sand et al. reported a 54 % failure rate after surgical repair of SUI in patients with a low MUCP compared with 18 % in those with a normal MUCP [17]. ISD was evaluated on the basis of ALPP by other authors [18]. McGuire et al. denied that MUCP had any predictive value for ISD and demonstrated that 75 % of patients with type III incontinence had a low ALPP at videourodynamic study. ALPP <60 cmH2O was associated with patients with high-grade incontinence without any patient with type I incontinence [18]. Pajoncini and colleagues analyzed the urodynamic features of ISD in 92 patients. The patients were divided into two categories: 50 patients affected by pure ISD as they had severe SUI and no urethral mobility and 42 patients suffering from marked urethral hypermobility without ISD as they had mild SUI. The ALPP was found below the cutoff value (≤60 cmH2O) in 70 % of ISD patients, whereas the MUCP below 30 cmH2O in 50 % of ISD patients [19]. In the present study, we diagnosed ISD on the basis of ALPP. Bai and colleagues compared the treatment outcomes of TVT for ISD (cases with ALPP <60 cmH2O or MUCP <20 cmH2O) and non-ISD patients. No significant difference was found in the cure rate at the 12-month follow-up. They concluded that TVT is effective for both ISD and non-ISD patients [20]. In the present study, there was no significant difference in the cure rate as regards ISD.
Our study has some limitations, mainly because of lack of a control group, so our results were compared with other published papers on TVT-O. The number of patients was limited in some subgroups. However, the strengths of this study include that it is a prospective long-term study with SUI, UUI, and QOL assessment using validated standardized questionnaires and objective evaluation using the urodynamic parameters for the severity of incontinence and the presence of ISD, any associated DO, and the occurrence of any degree of obstruction. Despite reporting excellent long-term results in the present study, further controlled studies including a larger number of patients are needed.
Conclusions
Our technique is a safe surgical procedure with excellent 5-year results. Our resterilizable modified helical passers and the cheap ordinary polypropylene mesh should be considered as a low-cost alternative to available commercial kits in the treatment of female SUI, mainly for public health systems with few financial resources. The presence of ISD or associated prolapse did not influence the success rate. No postoperative erosion, mesh exposure, or de novo urgency were reported. However, controlled studies of TVT-O with a larger number of patients are needed to confirm our results.
Abbreviations
- ALPP:
-
Abdominal leak point pressure
- CST:
-
Cough stress test
- DO:
-
Detrusor overactivity
- ISD:
-
Intrinsic sphincter deficiency
- MUCP:
-
Maximum urethral closure pressure
- Pdet Qmax :
-
Detrusor pressure at maximum flow rate
- PVRU:
-
Post-void residual urine
- Qmax :
-
Maximum flow rate
- QOL:
-
Quality of life
- SUI:
-
Stress urinary incontinence
- SUIQQ:
-
Stress and Urge Incontinence and Quality of Life Questionnaire
- TOT:
-
Transobturator vaginal tape outside-in
- TVT:
-
Tension-free vaginal tape
- TVT-O:
-
Transobturator vaginal tape inside-out
- US:
-
Abdominal and pelvic ultrasound
- UUI:
-
Urgency urinary incontinence
- RCT:
-
Randomized controlled trial
References
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7(2):81–85
Boustead GB (2002) The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int 89(7):687–693
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress incontinence in women. Prog Urol 11(6):1306–1313
Kulseng-Hanssen S, Borstad E (2003) The development of a questionnaire to measure the severity of symptoms and the quality of life before and after surgery for stress incontinence. BJOG 110(11):983–988
Patel BN, Smith JJ, Badlani GH (2009) Minimizing the cost of surgical correction of stress urinary incontinence and prolapse. Urology 74(4):762–764
Shah DK, Paul EM, Amukele S, Eisenberg ER, Badlani GH (2003) Broad based tension-free synthetic sling for stress urinary incontinence: 5-year outcome. J Urol 170(3):849–851
Elgamasy AK, Elashry OM, Elenin MA, Eltatawy HH, Elsharaby MD (2008) The use of polypropylene mesh as a transobturator sling for the treatment of female stress urinary incontinence (early experience with 40 cases). Int Urogynecol J Pelvic Floor Dysfunct 19(6):833–838
Chen X, Li H, Fan B, Yang X, Tong X (2009) An inexpensive modified transobturator vaginal tape inside-out procedure for the surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1365–1368
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114(5):522–531
Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, Basile S, Muzii L, Angioli R, Panici PB (2007) One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol 51(5):1376–1382
Jain P, Jirschele K, Botros SM, Latthe PM (2011) Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J 22(8):923–932
Bump RC, Norton PA, Zinner NR, Yalcin I, Duloxetine Urinary Incontinence Study Group (2003) Mixed urinary incontinence symptoms: urodynamic findings, incontinence severity, and treatment response. Obstet Gynecol 102:76–83
Minassian VA, Stewart WF, Hirsch AG (2008) Why do stress and urge incontinence co-occur much more often than expected? Int Urogynecol J Pelvic Floor Dysfunct 19:1429–1440
Papa Petros PE (1999) Detrusor instability and low compliance may represent different levels of disturbance in peripheral feedback control of the micturition reflex. Neurourol Urodyn 18:81–91
Koonings PP, Bergman A, Ballard CA (1990) Low urethral pressure and stress urinary incontinence in women: risk factor for failed retropubic surgical procedure. Urology 36(3):245–248
Sand PK, Bowen LW, Panganiban R, Ostergard DR (1987) The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol 69(3 Pt 1):399–402
McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, Gormley EA (1993) Clinical assessment of urethral sphincter function. J Urol 150(5 Pt 1):1452–1454
Pajoncini C, Costantini E, Guercini F, Bini V, Porena M (2003) Clinical and urodynamic features of intrinsic sphincter deficiency. Neurourol Urodyn 22(4):264–268
Bai SW, Jung YH, Jeon MJ, da Jung J, Kim SK, Kim JW (2007) Treatment outcome of tension-free vaginal tape in stress urinary incontinence: comparison of intrinsic sphincter deficiency and nonintrinsic sphincter deficiency patients. Int Urogynecol J Pelvic Floor Dysfunct 18(12):1431–1434
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
ElSheemy, M.S., Elsergany, R. & ElShenoufy, A. Low-cost transobturator vaginal tape inside-out procedure for the treatment of female stress urinary incontinence using ordinary polypropylene mesh. Int Urogynecol J 26, 577–584 (2015). https://doi.org/10.1007/s00192-014-2552-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2552-1