Abstract
This study evaluated the use of traditional polypropylene mesh, used in hernias repair, as a sling in the treatment of female stress urinary incontinence (SUI). Forty patients diagnosed with SUI underwent transobturator sling fashioned from the ordinary polypropylene mesh (vypro II®). Each lateral end of the tape is secured by a zero prolene suture. The procedure was then done outside-in, and the patients were followed up. The mean operative time was 40–60 min when the procedure was performed alone or accompanied with associated pelvic floor repair. Thirty-five patients (87.5%) were cured, and two patients (5%) significantly improved, but the procedure failed in three patients (7.5%), and the slings were removed because of vaginal erosion. Polypropylene mesh transobturator sling is an easy and cheap method for the treatment of female SUI with a high success rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence is a significant health problem in the developed and the developing countries. Population studies have shown that about 10–35% of all women have urinary incontinence [1]. Stress urinary incontinence (SUI) is the most common type of incontinence. A lot of different techniques are used for the treatment of SUI; slings are the most effective and durable form of treatment [2]. Various tissues and synthetic materials are used for that purpose. The new synthetic materials, replacing the torn fascia, are the basis of the recent development of a multitude of surgical techniques of SUI and other pelvic floor lesions. The tension-free vaginal tape (TVT) procedure has revolutionized the surgery of female SUI, and it is now considered by many surgeons to be the gold-standard surgery for female SUI with excellent long-term efficacy [3]. The TVT procedure, which uses a retropubic route, has been associated with a number of complications resulting from penetrations of the surgical device into pelvic vessels, nerves, and organs [4]. The transobturator tape (TOT) approach was developed for female SUI with the aim of avoiding the risk of urethra and bladder injuries with minimal vaginal dissection within a short period of time [5]. The procedure is now the most popular technique in many worldwide centers with good results. In a developing country like Egypt, the cost of the tape is highly expensive; in this study, we report our early experience in the use of polypropylene mesh as a transobturator sling in the treatment of female SUI.
Materials and methods
From December 2004 to May 2006, 45 patients diagnosed with SUI underwent the procedure with a sling fashioned from the ordinary surgical polypropylene mesh (Vypro II mesh). This mesh is a vicryl-prolene composite (polypropylene-polyglactin 910, violet, undyed, Ethicon, Johnson & Johnson, Summerville, NJ). For all patients, physical examination with cough stress test, urine culture, and sensitivity and preoperative urodynamics examination were performed. The cough stress test is done with full bladder (300 ml measured by ultrasound). The patient is asked to cough and bear down; urine is usually lost in small spurts with each cough. Delayed urine loss, particularly large volume loss or complete bladder emptying occurring after coughing, is suggestive of unstable bladder activity. If the stress incontinence is not demonstrated in a standard lithotomy position, the test should be repeated in the standing position with the patient’s feet comfortably separated at shoulder width. In cases of associated cystocele and/or rectocele, the test is done before and after insertion of a vaginal pack [6]. Cases with a neurogenic bladder or with evident urge incontinence were excluded. If there was a defect in pelvic floor support, it was corrected with an appropriate technique. All subjects received intravenous prophylactic antibiotic therapy at the beginning of surgery (2 g amoxicillin–clavulanic acid).
During induction of anesthesia (spinal or general) and positioning of the patient in the extended lithotomy position (hyperflexion, abduction external rotation of the thigh with the buttocks at the end of the table), the manually designed vaginal sling was prepared. It was designed from polypropylene mesh (Vypro II®, 30 × 20 or 30 × 10 cm) by the following measurement. The sling (Fig. 1) is composed of a central part (6 × 2.5 cm) and two peripheral parts (each is 12 × 2 cm) with a total length of the sling of 30 cm. Each lateral end of the sling was secured by a zero prolene suture.
After fixation of 16-F indwelling urethral catheter, a 2–3 midline anterior vaginal wall incision was performed starting 1 cm proximal to the external urethral meatus and extending proximally to near the bladder neck. The vaginal mucosa was dissected bilaterally at the direction of the ischiopubic ramus. The index finger was introduced into the dissected space to palpate the posterior part of the ischiopubic ramus and the internal obturator muscle. Two small cutaneous incisions were made in the inferior internal part of the obturator foramen at a horizontal plane passing between the external urethral meatus and the clitoris. The TOT needle was inserted through the obturator membrane and guided by the surgeon’s index finger into the vaginal incision. The two ends of the prolene sutures of the sling were inserted through the eye of the tip of the needle and guided back to the obturator incision. The same technique was performed at the other side. The sling was adjusted without any tension, and the excess length was cut off at the obturator incision. Cystocele and/or rectocele were performed before insertion of the sling in combined cases of SUI and pelvic floor lesions. In mild cases of cystocele, the insertion of the sling was enough without the need for cystocele repair. Closure of the vaginal mucosa was performed with interrupted catgut 2/0 followed by the insertion of a vaginal pack. The patient was discharged from the hospital the next day after removal of the vaginal pack, urethral catheter, and spontaneous urination of the patient. Oral ciprofloxacin 500 mg bidaily for 5 days was prescribed for the patients. When the procedure was associated with pelvic lesions surgery, the catheter was left in situ for 2–5 days. When there was a voiding difficulty or complete retention of urine, a program of clean intermittent catheterization (CIC) was started. Other immediate postoperative complications including hematoma and infections were also recorded.
Follow-up evaluation was performed at 1, 3, 6, and 12 months including physical examination, cough test, complete urine analysis, and uroflowmetry with postvoid residual urine volume (PVR) measurement. Postoperative complications were recorded and including urinary retention, voiding difficulty, de novo urgency, recurrent urinary tract infection, vaginal or urethral erosion, and dysparunia. The outcome score of surgical treatment was estimated as follows: the subjective cure = no urine loss during stress, objective cure = no leakage of urine with cough at the bladder capacity of 300 ml, and improvement = significantly fewer leakage episodes during stress than before surgery. All other patients were classified as failures, even if a clear improvement from the preoperative situation has occurred. Comparisons between preoperative and postoperative values were performed with the paired Student’s t test when continuous variables were evaluated, including symptoms, quality of life (QOL), and visual analog scale scores, Q-max. Statistical tests were two-tailed, and p < 0.05 was considered statistically significant. Analyses were performed with the Stat View® statistical software package.
Results
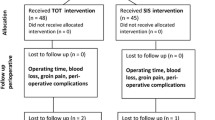
Forty-five female patients were enrolled in this study. Follow-up was lost in five patients, and complete data were available for only 40 patients. The ages of the patients ranged from 28 to 55 years (40.8 ± 7.8). Other patients’ characteristics are shown in Table 1. Pure SUI was found in 27 (67.5%) and mixed incontinence in 13 patients (32.5%). Preoperatively, all patients demonstrated subjective signs of SUI. The cough test with a bladder volume of 300 ml was positive for all patients even in those with accompanied cystocele, after insertion of a vaginal pack. The procedure was performed alone in 28 patients (70%) and was accompanied with cystocele repair in eight patients (20%), rectocele repair in three patients (7.5%) and cystorectocele repair in one patient (2.5%). The mean operative time was 40 (30–50) and 60 min (45–75) when the procedure was performed alone or accompanied with an associated pelvic floor repair, respectively.
Complications of the procedure were controlled. Two cases (5%) of remarkable intraoperative vaginal bleeding (>200 ml blood) were reported and managed; however, there was no need for blood transfusion. Postoperatively, 35 patients (87.5%) resumed normal voiding in the first postoperative day. Early postoperative voiding difficulty, within 1 week, was recorded in five patients (12.5%). Within 2 weeks postoperatively, three patients (7.5%) resumed normal voiding, and only two patients (5%) had persistent voiding difficulty. Cystometrogram of these two patients revealed PVR of 90 and 110 ml with involuntary bladder contractions and Q-max of 5 and 7 ml/s, respectively. Consequently, a program of CIC was scheduled for 1 month for the first patient and one and half month for the second patient. For all patients, there was a significant statistical difference between preoperative and 1-month postoperative Q-max (Table 2). Vaginal infections were recorded in four patients (10%) and properly managed by antibiotics and vaginal hygiene measures. Dysparunia was recorded in six patients (15%); later on, three of them developed vaginal erosion, and slings were removed.
Postoperatively, 10 out of 13 patients (76.9%) with preoperative mixed incontinence significantly improved; the other three patients (23.1%) still had persistent detrusor instability and required anticholinergics. On the other hand, 3 out of 27 patients (11.1%) with preoperative pure SUI developed de novo detrusor instability; with further follow-up, all cases improved within 1 month postoperatively.
With follow-up of 3, 6, and 12 months, there were no changes in the postoperative outcome, and the results seemed to be constant with time. The follow-up was at least 12 months and at a maximum of 24 months (16.7 ± 3.6). According to the protocol of the study, 35 patients (87.5%) were cured, and two patients (5%) significantly improved, but the procedure failed in three patients (7.5%), and the slings were removed because of vaginal erosion. These last three patients with vaginal erosions were presenting with vaginal pain, dysparunia, and purulent vaginal discharge. The mean time of the appearance of vaginal erosion symptoms was 10 months (6, 11, and 13 months). Polymicrobial flora was obtained from vaginal discharge in all patients. Physical examination demonstrated vaginal erosion at the midline beneath the urethra with exposure of the mesh. All the slings were removed surgically with the recurrence of SUI.
Comparisons between preoperative and postoperative SUI symptoms scores showed a statistically significant decrease in the severity of these symptoms after the procedure (Table 2). In addition, there was a significant decrease in postoperative Q-max. Analysis of incontinence severity and the impact of urinary symptoms on QOL using a visual analog scale and the Ditrovie QOL self-questionnaire, respectively, showed a significant decrease in urinary leakage together with significant improvement in QOL (Table 2).
Discussion
SUI is a devastating condition that affects many females. The basic idea of all sling and tape procedures is the placement of a strip, either organic or synthetic material, under the bladder neck and urethra producing urethral support and compression during a sudden increase in the intra-abdominal pressure [7]. Ulmsten and Petros [8] described the procedure of TVT based on a new theory of a urethral closure mechanism in women. The technique is considered as a gold-standard surgery for female SUI with excellent long-term results [3]. The outside-in TOT technique developed by Delorme et al. [5, 9] is an alternative to TVT to avoid the retropubic approach with the potential complication of the bladder, major blood vessel injuries, and voiding dysfunction. However, anatomical and clinical studies [10, 11] demonstrated that bladder, urethral, and vaginal injuries may still occur with the outside-in TOT technique. In 2003, de Leval [12] developed the inside-out TOT technique to avoid the risk of urethral and bladder injuries with a minimal vaginal dissection.
Recent anatomic cadaveric studies indicated that the insertion of inside-out TOT follows a highly reproducible and accurate trajectory minimizing the potential for bladder, urethral, vascular, intestinal, or neurological complications [13, 14]. In 253 patients, with a minimum of 1 year follow-up in 99 patients, this technique was found effective and safe without any case of serious complication [15].
In this study, the number of patients was relatively small, although the number of patients suffering from SUI is high in developing countries. Fewer numbers of these patients are seeking for treatment, as SUI is a social problem and management depends mainly on the QOL and economic status of the patients. In Egypt, the price of the tape is very expensive and cannot be tolerated by many patients. In this study, the traditional polypropylene mesh (Vypro II®), used for hernias repair with successful results, was used and utilized as a material for the transobturator sling. The mesh is characterized by relatively wide pores, which allow the circulation of macrophages, fibroblasts, deposition of collagen, and angiogenesis. The integrated polyglactin in the mesh is absorbed with time, which allows more integration of the tape in the host tissue. Therefore, with this mesh, there is a good healing of the vaginal wound with expected low rates of vaginal and urethral erosion.
Is was very important in this procedure, as for all anti-incontinence surgery, to follow the strict anatomical principles of TOT procedures [5, 15]. The learning curve of the procedure is very short provided that the surgeon is familiar with pelvic and vaginal surgery. During early cases in this study and because of the previous experience with the fascial slings [16, 17], it was easy to shift to transobturator sling without considerable difficulty. In this study, the technique of the transobturator sling has been used for the treatment of SUI in 40 patients. The procedure was done alone in 28 patients (70%) or with concomitant pelvic floor repair in 12 patients (30%). Using the strict criteria for success, the cure rate was recorded in 87.5% and improvement in 5%, but the procedure failed in 7.5% of cases. These results are similar to the results of TOT in other studies (89–91%) [15, 18, 19].
In this study, intraoperative complications such as vaginal bleeding and vaginal wall lacerations were properly managed. The best way to avoid these complications is the dissection in the proper plane and away from the anterior vaginal wall. When laceration occurs, it should be identified intraoperatively so the defect may be sutured promptly, thus minimizing the possibility of subsequent vaginal erosion. At the beginning of this study, intraoperative cystoscopy, used in the first seven cases, showed no bladder injuries. In the postoperative follow-up, no cases of sling-related bladder perforation were found. Based on the anatomical consideration of trajectory of the tape and the experience in the anti-incontinence surgery, cystoscopy may not be necessary when performing TOT. In accordance with other studies, cystoscopy is indicated only in cases of previous extensive pelvic surgery or when needle passage is difficult [15, 18]. However, Minalgia et al. [20] reported bladder perforation in 3 of 61 patients during TOT placement and recommended the routine use of intraoperative cystoscopy in this procedure. It should be noted that all three patients with bladder perforation had undergone previous pelvic surgery and that these complications occurred mainly in conjunction with a large C-shaped TOT needle.
In this study, there was an improvement of the preoperative irritative symptoms in 76.9% of cases by the procedure alone. Most importantly, the procedure improved QOL of the patients. After tape procedure for mixed incontinence, the preoperative irritative symptoms disappeared in 65–75% of the patients [15, 21]. According to the integral theory, this improvement is due to correction of the urethrovesical geometry and subsequently the function [8]. Digital midurethral anchoring under video ultrasound has been proven to restore anatomy and continence. This is an excellent preoperative predictive test for success of a midurethral sling [22]. In a urodynamic study, Petros demonstrated that this test can also relieve urge symptoms in patients with mixed incontinence and even unstable detrusor contractions. This was attributed to prevention of inappropriate activation of the micturition stretch receptors [23].
In this study, early postoperative voiding difficulty was reported in five patients (12.5%); however, only two patients (5%) required CIC. The voiding difficulty was recorded after all sling procedures. The reported rate of voiding difficulty after TOT procedures ranged from 7 to 11% [15, 18]. The cause of such voiding difficulty is usually overcorrection with tight tape. Diagnosis is approached by the clinical picture and urodynamics. The best way for treatment is prevention intraoperatively by no tension placement of the tape. The tape is needed to work only during periods of increased intra-abdominal pressure and not to obstruct the flow of urine during micturition. In this study, there was a significant decrease in Q-max after the procedure as previously reported after TOT procedures [15, 18, 24]. After the procedure, the patient should be instructed to relax the pelvic muscles during micturition, so the obstructing effect of the tape is minimized and the voiding is improved.
In this study, three cases (7.5%) of vaginal erosion were reported. One of them had diabetes mellitus type II with a possibility of repeated infections and subsequent vaginal erosion. The reported rate of vaginal erosion after TOT procedures varies greatly. Waltregny et al. [15] reported 0%, while Domingo et al. [24] reported 13.8% incidence of vaginal erosion after use of nonwoven, nonknitted polypropylene (Uratape™ or Obtape™). In the study of Yamada et al., 13.4% of vaginal erosion was reported after Obtape™ use, while no case was reported after Monarc™ use. The pore size appears to be the most important factor in polypropylene sling safety. A larger pore size allows for ingrowth of macrophages and fibroblasts, collagen deposition, and angiogenesis [25].
In this study, no cases of bladder or urethral injuries were recorded, may be attributed to absence of recurrent cases of SUI or cases with previous history of pelvic or vaginal surgery. In comparison of different techniques of midurethral slings, Silva reported that the short-term efficacy of TOT medurethral slings is comparable with the retropubic slings. In addition, the risk of bladder injury may be the least with inside-out approach [26].
In another study of 390 women who underwent TOT (either outside-in or inside-out) for the treatment of SUI, four lower urinary tract (LUT) injuries (1%), two urethral injuries (0.5%), and two bladder injuries (0.5%) occurred. All LUT injuries occurred in the outside-in group, although this difference did not reach significance. Bladder injuries occurred in women who underwent concomitant vaginal surgery, while urethral injuries occurred in women undergoing secondary procedures. In conclusion, LUT injury is an uncommon complication of the TOT procedures [27]. However, other studies have shown that the risk of obturator nerve and vessel injury is far higher with the inside-out technique. The inside-out TOT trajectory cannot be controlled, and it is subject to wide variability than was originally postulated [28]. In another anatomical study comparing both techniques, the tapes of the inside-out TOT were significantly closer to the obturator canal than those of the outside-in TOT [29]. Lastly, as the course of the dorsal nerve of the clitoris is along the medial aspect of the ischiopubic ramus, the outside-in technique may be safer [30]. Therefore, the outside-in technique should be preferred, even if there is a small possibility of bladder or urethral injury.
Conclusion
In this study, the manually designed transobturator polypropylene mesh sling is an easy, cheap, and cost-effective method for the treatment of female SUI. It is suitable for developing countries. The success rate is high with a few side effects.
Abbreviations
- TVT:
-
tension-free vaginal tape
- SUI:
-
stress urinary incontinence
- TOT:
-
transobturator tape
- QOL:
-
quality of life
- Q-max:
-
maximum flow rate
- CUA:
-
complete urine analysis
- CIC:
-
clean intermittent catheterization
- PVR:
-
postvoid residual urine volume
- LUT:
-
lower urinary tract
References
Milsom I, Ekelund P, Molander U, Arvidsson L, Areskoug B (1993) The influence of age, parity, oral contraception, hysterectomy and menopause on the prevalence of urinary incontinence in women. J Urol 149:1459–1462
Blaivas JG, Jacobs BZ (1991) Pubovaginal fascial sling for the treatment of complicated stress urinary incontinence. J Urol 145:1214–1218
Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U (2001) Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S5–S8
Boustead GB (2002) The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int 89:687–693
DeLorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
Ghoniem GM, Walters F, Lewis V (1994) The value of the vaginal pack test in largecystoceles. J Urol 152:931–934
Jarvis GJ (1994) Surgery for genuine stress incontinence. Br J Obstet Gynaecol 101:371–374
Ulmsten U, Petros P (1995) Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 29:75–82
Delorme E, Droupy S, deTayrac R, Delma V (2004) Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol 45:203–207
Costa P, Grise P, Droupy S, Monneins F, Assenmacher C, Ballanger P, Hermieu JF, Delmas V, Boccon-Gibod L, Ortuno C (2004) Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T.O.T.) Uratape: short term results of a prospective multicentric study. Eur Urol 46:102–106
Hermieu JF, Messas A, Delmas V, Ravery V, Dumonceau O, Boccon-Gibod L (2003) Bladder injury after TVT transobturator. Prog Urol 13:115–117
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Bonnet P, Waltregny D, Reul O, de Leval J (2005) Transobturator vaginal tape inside out for the surgical treatment of female stress urinary incontinence: anatomical considerations. J Urol 173:1223–1228
Reisenauer C, Kirschniak A, Drews U, Wallwiener D (2006) Transobturator vaginal tape inside-out. A minimally invasive treatment of stress urinary incontinence: surgical procedure and anatomical conditions. Eur J Obstet Gynecol Reprod Biol 127:123–129
Waltregny D, Reul O, Mathantu B, Gaspar Y, Bonnet P, de Leval J (2006) Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum followup. J Urol 175:2191–2195
Ghoniem GM, Elgamasy AN, Elsergany R, Kapoor DS (2002) Grades of intrinsic sphincteric deficiency (ISD) associated with female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 13:99–105
Ghoniem G, Elgamasy A (1995) Simplified surgical approach to bladder outlet obstruction following pubovaginal sling. J Urol 154:181–183
Morey AF, Medendorp AR, Noller MW, Mora RV, Shandera KC, Foley JP, Rivera LR, Reyna JA, Terry PJ (2006) Transobturator versus transabdominal mid urethral slings: a multiinstitutional comparison of obstructive voiding complications. J Urol 175:1014–1017
Deval B, Ferchaux J, Berry R, Gambino S, Ciofu C, Rafii A, Haab F (2006) Objective and subjective cure rates after trans-obturator tape (OBTAPE) treatment of female urinary incontinence. Eur Urol 49:373–377
Minaglia S, Ozel B, Klutke C, Ballard C, Klutke J (2004) Bladder injury during transobturator sling. Urology 64:376–377
Tahseen S, Reid PC, Charan P (2007) Short-term complications of the trans-obturator foramen procedure for urinary stress incontinence. J Obstet Gynaecol 27:500–502
Petros PP, Von Konsky B (1999) Anchoring the midurethra restores bladder-neck anatomy and continence. Lancet 354:997–998
Papa Petros PE (1999) Detrusor instability and low compliance may represent different levels of disturbance in peripheral feedback control of the micturition reflex. Neurourol Urodyn 18:81–91
Domingo S, Alama P, Ruiz N, Perales A, Pellicer A (2005) Diagnosis, management and prognosis of vaginal erosion after transobturator suburethral tape procedure using a nonwoven thermally bonded polypropylene mesh. J Urol 173:1627–1630
Yamada BS, Govier FE, Stefanovic KB, Kobashi KC (2006) High rate of vaginal erosions with the mentor Obtape. J Urol 176:651–654
Silva WA (2007) Treatment of stress urinary incontinence—midurethral slings: top-down, bottom-up, “outside-in,” or “inside-out”. Clin Obstet Gynecol 50:362–375
Abdel-Fattah M, Ramsay I, Pringle S (2006) Lower urinary tract injuries after transobturator tape insertion by different routes: a large retrospective study. BJOG 113:1377–1381
Hinoul P, Vanormelingen L, Roovers JP, de Jonge E, Smajda S (2007) Anatomical variability in the trajectory of the inside-out transobturator vaginal tape technique (TVT-O). Int Urogynecol J Pelvic Floor Dysfunct 18:1201–1206
Zahn CM, Siddique S, Hernandez S, Lockrow EG (2007) Anatomic comparison of two transobturator tape procedures. Obstet Gynecol 109:701–706
Achtari C, McKenzie BJ, Hiscock R, Rosamilia A, Schierlitz L, Briggs CA, Dwyer PL (2006) Anatomical study of the obturator foramen and dorsal nerve of the clitoris and their relationship to minimally invasive slings. Int Urogynecol J Pelvic Floor Dysfunct 17:330–334
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elgamasy, A.K.H., Elashry, O.M., Elenin, M.A. et al. The use of polypropylene mesh as a transobturator sling for the treatment of female stress urinary incontinence (early experience with 40 cases). Int Urogynecol J 19, 833–838 (2008). https://doi.org/10.1007/s00192-007-0539-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0539-x