Abstract
Adjuvant treatment based on fluoropyrimidines (FL) improves the prognosis of stage II/III colorectal cancer (CRC). Validated predictive/prognostic biomarkers would spare therapy-related morbidity in patients with a good prognosis. We compared the impact of a set of 22 FL-related polymorphisms with the prognosis of two cohorts of CRC patients treated with adjuvant FL with or without OXA, including a total of 262 cases. 5,10-Methylentetrahydrofolate reductase (MTHFR) MTHFR-1298 A>C (rs1801131) polymorphism had a concordant effect: MTHFR-rs1801131-1298CC genotype carriers had a worse disease free survival (DFS) in both the cohorts. In the pooled population MTHFR-rs1801131-1298CC carriers had also a worse overall survival. We computed a clinical score related to DFS including MTHFR-rs1801131, tumor stage, sex and tumor location, where rs1801131 is the most detrimental factor (hazard ratio=5.3, 95% confidence interval=2.2–12.9; P-value=0.0006). MTHFR-rs1801131 is a prognostic factor that could be used as an additional criteria for the choice of the proper adjuvant regimen in stage II/III colorectal cancer patients.
Similar content being viewed by others
Introduction
In patients with completely resected colorectal cancer (CRC), an adjuvant treatment with fluoropyrimidines (FL) (i.e., 5-fluorouracil/folinic acid or capecitabine) improves the outcome of stage II/III cancer patients.1,2 The addition of oxaliplatin (OXA) to FL further reduced patient mortality, with longer disease free survival (DFS) in a significant percentage of patients.3, 4, 5, 6, 7 The addition of OXA to FL regimens is burdened by a higher incidence of acute toxicity including the hematological toxicity, and the peripheral OXA-related neuropathy. In particular, the latter may persist after OXA discontinuation.8,9
A careful evaluation of the real benefit for the CRC patients of either a FL or a FL+OXA adjuvant treatment is required. The pathologic tumor stage is today the most reliable factor for the prediction of CRC prognosis and treatment outcome. However, a considerable stage-independent variability has been reported10 and more effective predictive/prognostic factors are needed to optimize CRC stage II/III management.
Host genetic characteristics have been considered as biomarkers of CRC outcome after a FL-based treatment.11 Interesting data regard polymorphisms in genes with a key role in the FL therapeutic action. Thymidylate synthase (TS) is the key enzyme in the mechanism of action of FL. The enzymes involved in folate metabolism and transport, as 5,10-methylentetrahydrofolate reductase (MTHFR), dihydrofolate reductase (DHFR), folylpolyglutamate synthetase (FPGS), glutamyl hydrolase (GGH), reduced folate carrier (RFC, encoded by SLC19A1) and cellular transporters (PCFT, ABCC1 and ABCC2) also play a relevant role determining the intracellular concentration of reduced folates whose availability is a required condition for FL activity. The inhibition of TS is increased by the presence of high intracellular concentration of 5,10-methylene-tetrahydrofolate that is in turn regulated by the activity of MTHFR. Polymorphisms of genes encoding these enzymes have been proposed to have a role in the clinical response to FL with still controversial results.12, 13, 14
At our knowledge, there are no available validated genetic markers to select CRC patients who could benefit from adjuvant FL-based treatment.
The aim of this study was to evaluate the impact of a set of FL-related polymorphisms on DFS in two distinct cohorts of patients treated with FL with or without OXA. This study was expected to provide the clinicians with validated biomarkers of patients clinical outcome.
Materials and methods
Patients and study design
This study included two cohorts of stage II-III CRC patients resected with curative intent. The main study endpoint was DFS. The Ethical Committee of each participating institution approved the research protocol, and all patients signed a written informed consent for biospecimens collection. All the patients had histologically confirmed stage II-III CRC; radiologically confirmed absence of distant metastases, age ⩾18 years; performance status (World Health Organization) 0–2; normal bone marrow, renal and liver function; Caucasian ethnicity. Patients follow-up was truncated at 5 years. Patients recruited after October 2007 were excluded for inadequate follow up (<5 years).
Fluorpyrimidines and oxaliplatin association cohort (FL+OXA)
This cohort includes 150 cases and is based on a previous prospective multi-institution study,11 143 cases were from the previous study, and 7 patients were enrolled after the previous study conclusion. The patients underwent radical surgery between November 2003 and October 2007, and were treated with FOLFOX4 as previously reported.11
Fluoropyrimidines cohort (FL)
This cohort includes an independent collection of samples from 112 CRC cases undergoing radical surgery between May 1995 and October 2007, and subsequently treated with adjuvant FL-alone at University Hospital of Florence or Istituto Oncologico Veneto of Padova, Italy. Patients received 5-fluorouracil/folinic acid according to the IMPACT investigators,1 or capecitabine according to Twelves et al.2
Follow-up monitoring
All the patients underwent the standard follow-up protocol for stage II/III surgically resected CRC patients, consisting in physical examination with routine blood tests, pulmonary X-ray and abdominal ultra-sonography or computed tomography. Patients were assessed every three months during the treatment, every 6 months within the first 3 years, and then yearly.
Selection of candidate polymorphisms and genotyping assay
Genomic DNA was extracted from peripheral blood or normal colonic mucosa from CRC patients. Genotyping was performed blinded to clinical data, and positive and negative controls were included.
Genetic variants in folate cycle and transcellular transport pathways were selected (www.pharmgkb.org). We have selected a panel of 22 polymorphisms in 9 genes involved in the cellular transport and folate cycle pathways (ABCC1, ABCC2, MTHFR, DHFR, SLC19A1, GGH, FPGS, PCFT and TYMS). More detail on genes, variants, pathways, minor allele frequency and assays are listed in Supplementary Table SI1.
Detailed pyrosequencing genotyping protocols performed on PSQ96MA (Biotage, Uppsala, Sweden) are available upon request. Pre-designed or custom TaqMan® single-nucleotide polymorphism genotyping assays, purchased from Applied Biosystems (Foster City, CA, USA) (www.appliedbiosystems.com), were performed on ABI 7900HT (AB Applied Biosystems), according to the manufacturer instructions. TYMS polymorphisms were analysed as previously published.15
Statistical analysis
The effect of gene polymorphisms on DFS or overall survival (OS) was assessed through hazard ratios (HR) and corresponding 95% confidence intervals, estimated by COX proportional hazard model. HRs were adjusted for gender, age, primary tumor site, tumor node metastasis stage and FL-dose density. OXA administration was added as a co-variate only in the pooled analysis. Dominant, recessive and additive genetic models were considered; the best-fitting model was selected according to Wald X2-test. A P<0.05 (two-sided) was adopted as significance threshold. P-values were not corrected for multiple testing to avoid false negative results. To lower the chance of false positive discoveries, only concordant effects (same effect, same genetic model) in the two cohorts were considered significant. Survival analysis was computed by Kaplan–Meier method, and log-rank test was used to test the differences between groups.
Results
Patient characteristics
The demographic and clinical characteristics of the two cohorts are summarized in Table 1. Patients were well balanced for sex, age and primary tumor location. Median follow-up was longer for patients in the FL-alone cohort. The stage at diagnosis was significantly different between the two cohorts (P<0.0001) with an higher percentage of stage III in the FL+OXA cohort. The majority of the patients in FL+OXA cohort were derived from a previous study11 based on FOLFOX4 administration and therefore treated with 5-fluorouracil (P=0.0405).
When stratified by stage, patients treated with the association regimen presented a longer DFS, according to the literature data3 (stage II patients HR=0.65, 95% CI 0.11–3.74, P=0.6248; stage III patients HR=0.65, 95% CI 0.38–1.13, P=0.1268). The difference did not reach statistical significance probably because of the low number of events in the different strata.
Association of genetic polymorphisms with disease free survival in each cohort
We assessed the association of the polymorphisms with DFS in each cohort by a multivariate analysis (Table 2). In FL-alone cohort, three polymorphisms (MTHFR-rs1801131, ABCC2-rs3740066 and SLC19A1-rs1051266) were associated with an increased risk of recurrence. In FL+OXA cohort, two polymorphisms (MTHFR-rs1801131 and ABCC2-rs3740066) increased the risk of tumor recurrence, whereas three polymorphisms (MTHFR-rs1801133, ABCC2-rs20020401 and SLC19A1-rs1051266) were related to decreased risk of recurrence. A concordant effect of MTHFR-rs1801131 on DFS in the two cohorts was highlighted, according to a recessive genetic model (Table 2). We thus considered MTHFR-rs1801131 a significant marker of patients DFS.
For ABCC2-rs3740066 polymorphism we found the same effect in the two cohorts of patients but according to different genetic models (dominant for FL cohort, and recessive for FL+OXA). Although this effect was not considered concordant according to the study criteria (same effect, same genetic model), when applying the additive genetic model to the polymorphism, we observed that in both groups of patients, each variant ABCC2-rs3740066 allele increased of 1.52 the risk of recurrence even if this effect was not significant (P=0.0966 for FL and 0.0597 for FL+OXA).
Pooled analysis on MTHFR-rs1801131 for disease free and overall survival
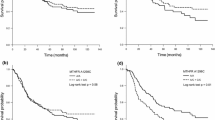
Considering the concordant effect of the MTHFR-rs1801131 polymorphism in the two cohorts, we performed a pooled analysis of the combined dataset, to increase the statistical power. MTHFR-rs1801131 polymorphism was related to lower recurrence risk in MTHFR-rs1801131-1298AA+AC patients than in MTHFR-rs1801131-1298CC patients (HR=2.57, 95% CI 1.28–5.17) and to longer DFS (Log-Rank P-value=0.0029). Wild-type MTHFR-rs1801131-1298AA and heterozygous MTHFR-rs1801131-1298AC patients had also lower risk of death (HR=2.01, 95%CI 0.85–4.75) and longer OS than MTHFR-rs1801131-1298CC patients in a multivariate model (Log-Rank P-value=0.0350) (Figure 1).
Pooled multivariate analysis (262 patients included) of disease free survival (a) and overall survival (b) of colorectal cancer patients undergoing fluoropyrimidines-based chemotherapy according to MTHFR-rs1801131 polymorphism. FL, fluoropyrimidines.
A subgroup analysis in the pooled population showed a negative prognostic value of MTHFR-rs1801131-1298CC genotype on DFS for male patients, below 65 years of age, with a colon primary tumor location. MTHFR-rs1801131 had a significant detrimental effect on OS of patients younger than 65 years and with colon as primary tumor site (Figure 2).
Association between MTHFR-rs1801131 genetic polymorphism and disease free survival or overall survival, according to a recessive genetic model, in separate strata of selected covariates using the pooled population of patients (262 patients included). HRs were estimated for MTHFR-rs1801131-1298CC versus MTHFR-rs1801131-1298 AC+AA according to a multivariate Cox proportional hazard model. Hazard ratios in stage II cancers is not accountable because none of the patients with stage II cancer presented a MTHFR-rs1801131–1298CC genotype. CI, confidence intervals; HR, harzard ratios.
A significant interaction was found between tumor stage and MTHFR-rs1801131 in the pooled population. One-hundred seventy-two patients out of 240 (72%) with MTHFR-rs1801131-1298AA+AC had a stage III disease versus 18 out of 18 (100%) with MTHFR-rs1801131-1298CC genotype (P-value=0.0046). No variant MTHFR-rs1801131-1298CC genotype carrier was found among stage II patients.
Risk model for disease free survival in the pooled population
In our study, male sex (vs female), colon primary tumor site (vs rectum), and tumor stage III (vs stage II) were non-genetic negative prognostic factors for DFS by multivariate analysis (age higher than 65 years was not associated with DFS).
We compared the negative prognostic effect of carrying 0–3 of these factors with the effect of carrying the genetic negative prognostic factor MTHFR-rs1801131-1298CC genotype (Figure 3). Each additional negative prognostic factor (0–3) significantly increased the risk of disease recurrence in the pooled group of patients. Carrying a MTHFR-rs1801131-1298CC genotype is the worse prognostic factor conferring, independently from the other non-genetic factors, the highest risk of disease recurrence (HR=5.3, 95% CI 2.2–12.9; Log-rank P-value=0.0006).
Disease free survival of colorectal cancer patients undergoing fluoropyrimidines-based chemotherapy (pooled group of patients, 262 patients included) according to an increasing number of risk factors (gender, tumor site and stage) and MTHFR-rs1801131 polymorphism.
Considering the significant interaction reported between MTHFR-rs1801131 polymorphism and tumor stage, we evaluated the advantage on DFS of using OXA in addition to FL, only in stage III patients, stratified by MTHFR genotype. Even if the results were nonsignificant because of the low number of events in the single strata, we observed an advantage of using OXA in patients with at least one MTHFR-rs1801131-1298A allele (102 treated with FL-alone, and 138 with FL+OXA) (HR=0.65, 95%C.I. 0.35–1.18, P=0.1524). The DFS curves of patients with MTHFR-rs1801131-1298CC genotype (8 treated with FL-alone, and 10 with FL+OXA) were super-imposable in presence or absence of OXA (Supplementary Figure SI1).
Discussion
This pharmacogenetic study compares the effect of a set of host polymorphisms on DFS in two independent cohorts of CRC patients treated with adjuvant FL with or without OXA. We found a concordant prognostic effect of MTHFR-rs1801131 polymorphism on DFS demonstrating, for the first time, that it is independent from the addition of OXA to a FL regimen. MTHFR-rs1801131 represents a risk factor for disease recurrence (lower DFS) according to a recessive model in both the cohorts. In the pooled set of patients a detrimental effect of MTHFR-rs1801131 on OS was observed, with a worse prognosis in patients carrying the MTHFR-rs1801131-1298CC genotype. When defining a multi-parametric score of DFS we found that MTHFR-rs1801131 was more effective than the cancer stage in predicting the clinical outcome of the patients.
Several authors reported a detrimental effect of MTHFR-rs1801131 on CRC patients prognosis, consistent with our results. The polymorphism was associated to worse survival in metastatic CRC patients16, 17, 18 and in patients with a localized disease.19,20 The patients were mainly treated with FL-based regimens, but a negative prognostic effect of MTHFR-rs1801131 has been reported also in untreated patients.20 Conversely, Capitain et al.,21 reported a positive effect on metastatic CRC patients survival of MTHFR-rs1801131, but only if combined with other polymorphisms in the folate pathway. Other studies failed to evidence any association between MTHFR-rs1801131 and FL-treated CRC patients survival.22, 23, 24, 25 Summarizing, despite the large number of studies conducted up to date, the clinical impact of MTHFR-rs1801131 is still controversial.
In vitro, the variant MTHFR-rs1801131 allele, encoding for a mutant protein (Glu429Ala), was associated with decreased enzymatic activity26 and higher FL cytotoxicity.27
We would expect that patients carrying MTHFR-rs1801131 polymorphism present higher intracellular level of 5,10-MTHF and are therefore more sensitive to FL treatment. However, the complexity of the tumor response phenotype in vivo could lead to opposite, unexpected results, as those reported by us and others.16,26
The influence of MTHFR genotype on patient DFS could be related to the impact of MTHFR function on DNA methylation patterns. It has been previously demonstrated that a deficient MTHFR activity is associated with a reduced level of global DNA methylation in peripheral blood leukocytes.19 CpG islands methylation in the gene promoters was related to specific CRC phenotypes with differential sensitivity to FL treatment.28,29 In addition, previous studies30 reported that MTHFR-rs1801133, and to a lesser extent MTHFR-rs1801131, polymorphisms are inversely related to the development of microsatellite instable (MSI) CRC.31 MSI tumors development is related to a defective mis-match repair mechanism, because of either gene mutations or silencing by promoter hyper-methylation. Patients with MTHFR-rs1801131-1298CC genotype could be more sensitive to FL-based therapies and present a worse prognosis as in our study, since less prone to develop an MSI tumor.32,33 The effect of MTHFR-rs1801131 on the risk to develop an MSI-CRC was previously related to an optimal folate intake.31 We do not have nutritional data on our patients, but we observed a stronger effect of the polymorphism on the DFS and OS of younger patients (age<65 years) (Figure 2), presumably presenting more adequate dietary folate intake.
Two previous studies reported a major detrimental effect of MTHFR-rs1801131 polymorphism on OS of female CRC patients.17,18 We observed only a slightly increased effect of the polymorphism on OS in female patients, that is basically sex-independent in our patients (Figure 2).
MTHFR-rs1801131 genotype was associated to cancer tumor node metastasis stage at diagnosis in our study. This observation could imply a differential carcinogenesis related to this polymorphism. This is consistent with recent findings of an association between the same MTHFR-rs1801131 polymorphism and the risk of CRC,34 possibly linked to the effect of the polymorphism on DNA synthesis and methylation. In addition, the paper by Negandhi et al.,20 reported a detrimental effect of MTHFR-rs1801131 on CRC patients OS independently from FL administration, highlighting a possible prognostic effect of the single-nucleotide polymorphism, unrelated to the chemotherapeutic treatment. We do not have, in our study, a group of untreated patients to compare the effect of the polymorphism on patients outcome in absence of any chemotherapeutic treatment, therefore this observation will need further investigation.
We performed also an exploratory analysis to verify the impact of MTHFR-rs1801131 polymorphism on the treatment outcome when patients were given the combination regimen instead of FL-alone (Supplementary Figure SI1). Despite the low number of patients in the homozygous variant group (n=18), it seems that no benefit was derived by MTHFR-rs1801131-1298CC patients when treated with the association regimen. Patients with MTHFR-rs1801131-1298AC or MTHFR-rs1801131-1298AA genotypes, presented a trend for improved DFS if treated with the combination regimen. This finding is partially at odds with the study by Boige et al.,23 performed on metastatic CRC patients, that suggested that the positive effect on tumor response of OXA addition to a FL treatment, increases with the number of MTHFR-rs1801131 variant alleles. However, chemotherapy could interact differently with the host genetic environment to produce a tumor response in patients with nonmetastatic patients, as in our study, and it is not possible to directly compare the obtained results. Before hypothesizing a stage-specific effect further investigation is needed.
Some polymorphisms in SLC19A1 (rs1051266), ABCC2 (rs3740066 and rs20020401) and MTHFR (rs1801133) resulted associated to DFS with a nonconcordant effect in the two cohorts. This finding could support a regimen-specific (FL-alone or FL+OXA) impact of these polymorphisms. However, we do not have adequate information to provide insights of this possible interaction. Moreover, the limited number of patients in each cohort weakens the probability of a population specific effect. From a statistical point of view, to find the same association with a concordant effect in two independent cohorts of patients lowers the chance of false positive discoveries. Nonconcordant associations should, in our opinion, be considered as exploratory and should be further validated to exclude they are false positive. However, a specific attention should be spent for ABCC2-rs3740066 that presents the same significant effect in the two cohorts of cases, although according to different genetic models (dominant or recessive). When considering the additive genetic model we observed that in both groups of patients each variant ABCC2-rs3740066 allele increases of 1.52 the risk of recurrence. This trend highlights that, even if the heterozygous genotype seems to contribute differentially to the recurrence risk according to the different therapeutic scheme (FL or FL+OXA), the effect of the variant ABCC2-rs3740066 allele could be considered concordant in the two populations. ABCC2-rs3740066 is a synonymous single-nucleotide polymorphism that has been reported to lower the ABCC2 protein expression in vitro35 and has been related to the clinical outcome of cancer patients.36, 37, 38 We have previously demonstrated a significant effect of this polymorphism in increasing the risk to develop severe neurological toxicity in the FL+OXA group of patients,11 consistently with a phenotypic effect of the single-nucleotide polymorphism. We could hypothesize that an effect of ABCC2 in modulating the intracellular folate levels, could interfere with the efficacy of FL treatment. However, because of the role of ABC transporters in the modulation of cancer chemiosensibility based on several indirect effects on cellular homeostasis and apoptotic control39 we can not exclude a prognostic effect of the marker independent from the used chemotherapeutic treatment.
Some relevant variants for patients outcome, as tumor stage at diagnosis and OXA administration are dishomogeneous between the two cohorts of patients. This strengthens the value of the discovery of a concordant effect for MTHFR-rs1801131 polymorphism. However, it limits the possibility to interpret the nonconcordant effect of other polymorphisms, as pointed out above. To overcome a possible difference in the duration of the treatment in the two groups we adjusted the multivariate DFS and OS analyses also for FL-dose density. The knowledge of the tumor MSI status would have been useful to better interpret our results. Unfortunately, we do not have such information since MSI is not routinely evaluated.
In conclusion, this study validates in two different retrospective cohorts a detrimental role of MTHFR-rs1801131 polymorphism on the DFS and OS of CRC patients treated with adjuvant FL-based regimen. These results support the implementation of a clinical pharmacogenetic study to prospectively use MTHFR-rs1801131 to direct post-operative chemotherapy in stage II/III CRC patients. Patients carrying the unfavorable MTHFR-rs1801131 genotype should be allowed to undergo a chemotherapy regimen other than the standard ones (i.e., a fluoropyrimidine with or without OXA). An intensified chemotherapy regimen including also drugs with different mechanisms of action (e.g., irinotecan) could be investigated in this setting of patients with unfavorable prognosis.
References
International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. Lancet 1995; 345: 939–944.
Twelves C, Wong A, Nowacki MP, Abt M, Burris H III, Carrato A et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005; 352: 2696–2704.
Andre T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009; 27: 3109–3116.
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011; 29: 1465–1471.
Moertel CG, Fleming TR, Macdonald JS, Haller DG, Laurie JA, Tangen CM et al. Intergroup study of fluorouracil plus levamisole as adjuvant therapy for stage II/Dukes' B2 colon cancer. J Clin Oncol 1995; 13: 2936–2943.
O'Connor ES, Greenblatt DY, LoConte NK, Gangnon RE, Liou JI, Heise CP et al. Adjuvant chemotherapy for stage II colon cancer with poor prognostic features. J Clin Oncol 2011; 29: 3381–3388.
Tournigand C, Andre T, Bonnetain F, Chibaudel B, Lledo G, Hickish T et al. Adjuvant therapy with fluorouracil and oxaliplatin in stage II and elderly patients (between ages 70 and 75 years) with colon cancer: subgroup analyses of the Multicenter International Study of Oxaliplatin, Fluorouracil, and Leucovorin in the Adjuvant Treatment of Colon Cancer trial. J Clin Oncol 2012; 30: 3353–3360.
Andre T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004; 350: 2343–2351.
Schmoll HJ, Cartwright T, Tabernero J, Nowacki MP, Figer A, Maroun J et al. Phase III trial of capecitabine plus oxaliplatin as adjuvant therapy for stage III colon cancer: a planned safety analysis in 1,864 patients. J Clin Oncol 2007; 25: 102–109.
Puppa G, Sonzogni A, Colombari R, Pelosi G . TNM staging system of colorectal carcinoma: a critical appraisal of challenging issues. Arch Pathol Lab Med 2010; 134: 837–852.
Cecchin E, D'Andrea M, Lonardi S, Zanusso C, Pella N, Errante D et al. A prospective validation pharmacogenomic study in the adjuvant setting of colorectal cancer patients treated with the 5-fluorouracil/leucovorin/oxaliplatin (FOLFOX4) regimen. Pharmacogenomics J 2013; 13: 403–409.
Toffoli G, Cecchin E . Uridine diphosphoglucuronosyl transferase and methylenetetrahydrofolate reductase polymorphisms as genomic predictors of toxicity and response to irinotecan-, antifolate- and fluoropyrimidine-based chemotherapy. J Chemother 2004; 16: 31–35.
Toffoli G, De Mattia E . Pharmacogenetic relevance of MTHFR polymorphisms. Pharmacogenomics 2008; 9: 1195–1206.
Vignoli M, Nobili S, Napoli C, Putignano AL, Morganti M, Papi L et al. Thymidylate synthase expression and genotype have no major impact on the clinical outcome of colorectal cancer patients treated with 5-fluorouracil. Pharmacol Res 2011; 64: 242–248.
Ulrich CM, Bigler J, Bostick R, Fosdick L, Potter JD . Thymidylate synthase promoter polymorphism, interaction with folate intake, and risk of colorectal adenomas. Cancer Res 2002; 62: 3361–3364.
Etienne MC, Formento JL, Chazal M, Francoual M, Magne N, Formento P et al. Methylenetetrahydrofolate reductase gene polymorphisms and response to fluorouracil-based treatment in advanced colorectal cancer patients. Pharmacogenetics 2004; 14: 785–792.
Pare L, Salazar J, del Rio E, Baiget M, Altes A, Marcuello E et al. Methylenetetrahydrofolate reductase gene polymorphisms: genomic predictors of clinical response to fluoropyrimidine-based chemotherapy in females. J Clin Oncol 2008; 26: 3468–3469.
Zhang W, Press OA, Haiman CA, Yang DY, Gordon MA, Fazzone W et al. Association of methylenetetrahydrofolate reductase gene polymorphisms and sex-specific survival in patients with metastatic colon cancer. J Clin Oncol 2007; 25: 3726–3731.
Fernandez-Peralta AM, Daimiel L, Nejda N, Iglesias D, Medina A, Gonzalez-Aguilera JJ . Association of polymorphisms MTHFR C677T and A1298C with risk of colorectal cancer, genetic and epigenetic characteristic of tumors, and response to chemotherapy. Int J Colorectal Dis 2010; 25: 141–151.
Negandhi AA, Hyde A, Dicks E, Pollett W, Younghusband BH, Parfrey P et al. MTHFR Glu429Ala and ERCC5 His46His polymorphisms are associated with prognosis in colorectal cancer patients: analysis of Two independent cohorts from Newfoundland. PLoS One 2013; 8: e61469.
Capitain O, Boisdron-Celle M, Poirier AL, Abadie-Lacourtoisie S, Morel A, Gamelin E . The influence of fluorouracil outcome parameters on tolerance and efficacy in patients with advanced colorectal cancer. Pharmacogenomics J 2008; 8: 256–267.
Afzal S, Jensen SA, Vainer B, Vogel U, Matsen JP, Sorensen JB et al. MTHFR polymorphisms and 5-FU-based adjuvant chemotherapy in colorectal cancer. Ann Oncol 2009; 20: 1660–1666.
Boige V, Mendiboure J, Pignon JP, Loriot MA, Castaing M, Barrois M et al. Pharmacogenetic assessment of toxicity and outcome in patients with metastatic colorectal cancer treated with LV5FU2, FOLFOX, and FOLFIRI: FFCD 2000-05. J Clin Oncol 2010; 28: 2556–2564.
Lee KH, Chang HJ, Han SW, Oh DY, Im SA, Bang YJ et al. Pharmacogenetic analysis of adjuvant FOLFOX for Korean patients with colon cancer. Cancer Chemother Pharmacol 2013; 71: 843–851.
Zhu L, Wang F, Hu F, Wang Y, Li D, Dong X et al. Association between MTHFR polymorphisms and overall survival of colorectal cancer patients in Northeast China. Med Oncol 2013; 30: 467.
van der Put NM, Gabreels F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 1998; 62: 1044–1051.
Etienne MC, Ilc K, Formento JL, Laurent-Puig P, Formento P, Cheradame S et al. Thymidylate synthase and methylenetetrahydrofolate reductase gene polymorphisms: relationships with 5-fluorouracil sensitivity. Br J Cancer 2004; 90: 526–534.
Noguchi T, Tanimoto K, Shimokuni T, Ukon K, Tsujimoto H, Fukushima M et al. Aberrant methylation of DPYD promoter, DPYD expression, and cellular sensitivity to 5-fluorouracil in cancer cells. Clin Cancer Res 2004; 10: 7100–7107.
Van Rijnsoever M, Elsaleh H, Joseph D, McCaul K, Iacopetta B . CpG island methylator phenotype is an independent predictor of survival benefit from 5-fluorouracil in stage III colorectal cancer. Clin Cancer Res 2003; 9: 2898–2903.
Toffoli G, Gafa R, Russo A, Lanza G, Dolcetti R, Sartor F et al. Methylenetetrahydrofolate reductase 677 C—>T polymorphism and risk of proximal colon cancer in north Italy. Clin Cancer Res 2003; 9: 743–748.
Eaton AM, Sandler R, Carethers JM, Millikan RC, Galanko J, Keku TO . 5,10-methylenetetrahydrofolate reductase 677 and 1298 polymorphisms, folate intake, and microsatellite instability in colon cancer. Cancer Epidemiol Biomarkers Prev 2005; 14: 2023–2029.
Liang JT, Huang KC, Lai HS, Lee PH, Cheng YM, Hsu HC et al. High-frequency microsatellite instability predicts better chemosensitivity to high-dose 5-fluorouracil plus leucovorin chemotherapy for stage IV sporadic colorectal cancer after palliative bowel resection. Int J Cancer 2002; 101: 519–525.
Watanabe T, Wu TT, Catalano PJ, Ueki T, Satriano R, Haller DG et al. Molecular predictors of survival after adjuvant chemotherapy for colon cancer. N Engl J Med 2001; 344: 1196–1206.
Ge H, Zheng X, Zhao E, Sheng X, Lu S, Cheng S et al. Letter to the editor: a meta-analyses of association between polymorphism of MTHFR A1298C and colorectal cancer risk. Int J Colorectal Dis 2012; 27: 1387–8.
Itoda M, Saito Y, Soyama A, Saeki M, Murayama N, Ishida S et al. Polymorphisms in the ABCC2 (cMOAT/MRP2) gene found in 72 established cell lines derived from Japanese individuals: an association between single nucleotide polymorphisms in the 5'-untranslated region and exon 28. Drug Metab Dispo 2002; 30: 363–364.
Han JY, Lim HS, Park YH, Lee SY, Lee JS . Integrated pharmacogenetic prediction of irinotecan pharmacokinetics and toxicity in patients with advanced non-small cell lung cancer. Lung Cancer 2009; 63: 115–120.
Han JY, Lim HS, Yoo YK, Shin ES, Park YH, Lee SY et al. Associations of ABCB1, ABCC2, and ABCG2 polymorphisms with irinotecan-pharmacokinetics and clinical outcome in patients with advanced non-small cell lung cancer. Cancer 2007; 110: 138–147.
Sharifi MJ, Bahoush G, Zaker F, Ansari S, Rafsanjani KA, Sharafi H . Association of -24CT, 1249GA, and 3972CT ABCC2 gene polymorphisms with methotrexate serum levels and toxic side effects in children with acute lymphoblastic leukemia. Pediatr Hematol Oncol 2014; 31: 169–177.
Huang Y, Sadee W . Membrane transporters and channels in chemoresistance and -sensitivity of tumor cells. Cancer Lett 2006; 239: 168–182.
Acknowledgements
This work was supported by the ‘Associazione ABO per l’Applicazione delle Biotecnologie in Oncologia’ to GT; the ‘Associazione Italiana per la Ricerca sul Cancro (AIRC) (Special Program Molecular Clinical Oncology, 5 × 1000, (No. 12214)) to GT; the European Research Council (Programme ‘ideas’, Proposal No 269051’) to GT; the Italian Ministry of Education MIUR (FIRB prot. RBAP11ETKA) to GT; Ente Cassa di Risparmio di Firenze to EM; Associazione Giacomo Onlus, Castiglioncello to EM; and Gruppo Oncologico Chirurgico Cooperativo Italiano, Florence to EM.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Rights and permissions
About this article
Cite this article
Cecchin, E., Perrone, G., Nobili, S. et al. MTHFR-1298 A>C (rs1801131) is a predictor of survival in two cohorts of stage II/III colorectal cancer patients treated with adjuvant fluoropyrimidine chemotherapy with or without oxaliplatin. Pharmacogenomics J 15, 219–225 (2015). https://doi.org/10.1038/tpj.2014.64
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2014.64
- Springer Nature Limited
This article is cited by
-
Influence of FPGS, ABCC4, SLC29A1, and MTHFR genes on the pharmacogenomics of fluoropyrimidines in patients with gastrointestinal cancer from the Brazilian Amazon
Cancer Chemotherapy and Pharmacology (2021)
-
Polymorphisms of MTHFR C677T and A1298C associated with survival in patients with colorectal cancer treated with 5-fluorouracil-based chemotherapy
International Journal of Clinical Oncology (2017)
-
Influences of ERCC1, ERCC2, XRCC1, GSTP1, GSTT1, and MTHFR polymorphisms on clinical outcomes in gastric cancer patients treated with EOF chemotherapy
Tumor Biology (2016)