Abstract
Purpose
Ethnic diversity of genetic polymorphism can result in individual differences in the efficacy and toxicity of cancer chemotherapy.
Methods
We analyzed 20 germline polymorphisms in 10 genes (TS, MTHFR, ERCC1, XPD, XRCC1, ABCC2, AGXT, GSTP1, GSTT1 and GSTM1) from prospectively enrolled 292 Korean patients treated with adjuvant oxaliplatin plus leucovorin plus 5-fluorouracil (FOLFOX) for colon cancer.
Results
In contrast to previous studies in Caucasians, neutropenia (grade 3–4, 60.5 %) was frequently observed, whereas only 16.4 % experienced grade 2 or more sensory neuropathy. Neutropenia was more frequent in MTHFR 677TT [adjusted odds ratio (OR) 2.32, 95 % confidence interval (CI) 1.19–4.55] and ERCC1 19007TT (adjusted OR 4.58, 95 % CI 1.20–17.40) genotypes. Patients harboring XRCC1 23885GG experienced less grade 2–4 neuropathy [adjusted OR 0.52, 95 % CI 0.27–0.99]. MTHFR 677TT (p = 0.002) and XRCC1 23885GG (p = 0.146) genotypes were also more prevalent in Koreans compared to Caucasians. TS ‘low’ genotype (adjusted HR 1.83, 95 % CI 1.003–3.34) was significantly related to shorter disease-free survival. Overall survival was not significantly different according to the polymorphisms.
Conclusions
Polymorphisms in MTHFR, XRCC1 and TS are related to toxicities and disease-free survival in patients with colon cancer. The ethnic differences in frequencies of genotypes may explain the ethnic difference in toxicity profile following adjuvant FOLFOX chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer has a worldwide incidence of 1 million cases annually and claims the lives of half a million people every year [13]. In Korea, colorectal cancer is the fourth most common cancer and the incidence is rapidly increasing [30]. Adjuvant chemotherapy with oxaliplatin, 5-fluorouracil (5-FU) and leucovorin (FOLFOX) has become the standard of care for patients with resected stage III and high-risk stage II colon cancer [2, 4]. However, 5-FU and oxaliplatin toxicity, such as peripheral neuropathy and neutropenia, is frequent and often severe. Defining the associations between genetic polymorphisms and patient outcomes may help to individualize and optimize adjuvant chemotherapy [6, 8].
Ethnic diversity in drug response or toxicity is becoming increasingly recognized. For example, both response rate and adverse events, such as severe diarrhea, were significantly higher in white patients than in black patients [25]. On the other hand, East Asians, including Koreans, were more susceptible to neutropenia from chemotherapy agents than the Western population, and genetic polymorphism could explain these ethnic differences of effectiveness and toxicity of chemotherapy [24]. Thus, pharmacoethnic studies investigating the differences in frequency of genetic single nucleotide polymorphisms (SNPs) between ethnic groups and the clinical implications are practically important.
SNPs in genes encoding key enzymes for the metabolism of 5-FU and oxaliplatin that might alter the gene’s expression or activity of the protein have been reported. Thymidylate synthase (TS) is the target enzyme of 5-FU [9], and common polymorphisms of the gene have been associated with altered TS expression [21, 23]. Methylenetetrahydrofolate reductase (MTHFR) is an important enzyme in the folate pathway, and two common SNPs were shown to reduce the activity of MTHFR [27, 29].
Resistance to oxaliplatin has been attributed to enhanced repair of DNA damage through the nucleotide excision repair (NER) pathway [28], including the excision repair cross-complementing group 1 (ERCC1) and the xeroderma pigmentosum group D (XPD) products, and the base-excision repair (BER) pathway including X-ray repair cross-complementing group 1 (XRCC1) [16]. Moreover, response to oxaliplatin may depend on detoxification pathways, including the glutathione S-transferase (GST) family of isoenzymes, GSTP1, GSTT1 and GSTM1 [26]. Alanine glyoxylate aminotransferase (AGXT) is involved in oxalate metabolism, detoxifying glyoxylate, and harbors two SNPs [11]. The adenosine binding-cassette transporter C2 (ABCC2) gene codes for multidrug resistance protein 2, an ATP-binding-cassette transporter involved in the excretion of oxaliplatin and other xenobiotica. SNPs in ABCC2 (−24C > T and 3972C > T) have been reported [10].
We examined 20 polymorphisms within ten genes from a prospective multicenter cohort study of patients treated with adjuvant FOLFOX chemotherapy, which was conducted in Korea. The studied genes are those involved in the DNA-repair complex or in the metabolism and detoxification of 5-FU and oxaliplatin. Associations between genotypes and toxicity of the chemotherapy were investigated. We also investigated possible ethnic differences in allelic frequencies between Western and Asian (Korean) patients.
Materials and methods
Patients
Patients older than 18 years with resected stage III or high-risk stage II colon cancer were enrolled. Patients with cancer of the recto-sigmoid junction were also eligible. High risk was defined as follows: a T4 tumor, poor histological grade, lymphovascular involvement, bowel obstruction, localized perforation, involvement of surgical margins or fewer than 12 nodes analyzed. Patients with severe renal disorder, history of disabling peripheral neuropathy, investigational agents within 30 days, bone marrow suppression or those who were pregnant or breastfeeding were excluded. Patients were enrolled from six Korean centers between August 2006 and December 2008. The study protocol was reviewed and approved by the institutional review board of participating centers. Written informed consent was obtained from all the patients.
Treatment and evaluations
Twelve cycles of adjuvant FOLFOX were administered. Each cycle consisted of oxaliplatin (85 mg/m2) on day 1, and folinic acid (200 mg/m2) and a bolus of 5-FU (400 mg/m2), followed by a 22-h infusion of 5-FU (600 mg/m2) on days 1 and 2; the cycle was repeated every 2 weeks.
Adverse events were graded according to National Cancer Institute common terminology criteria for adverse events (NCI-CTCAE version 3.0). Dose reductions were based on the worst adverse event observed during the previous cycle. The dose of oxaliplatin was reduced to 75 mg/m2, 5-FU bolus to 300 mg/m2 and 5-FU infusion to 500 mg/m2 in the event of grade 3/4 hematologic toxicity, grade 4 diarrhea/stomatitis or other grade 3 toxicities. In instances of peripheral sensory neuropathy, oxaliplatin was reduced to 75 mg/m2 for grade 1 toxicity that persisted between cycles, grade 2 toxicity for at least 7 days or grade 3 for up to 7 days. The next cycle of FOLFOX was permitted after recovery from all toxicities less than grade 1. Oxaliplatin was discontinued in cases of persistent painful paresthesias or functional impairment.
Patients were assessed before the initiation of chemotherapy and every 2 weeks during treatment. Computed tomography was repeated every three cycles during the chemotherapy period.
Genotyping
Genomic DNA was extracted from peripheral blood using QIAmp DNA blood kits (Qiagen, Valencia, CA, USA), and each polymorphism was analyzed using PCR-restriction fragment length polymorphism methods or SNaPshot assay (ABI PRISM SNaPshot Multiplex kit, Foster City, CA, USA). The primer sequences and the restriction enzymes used are specified in Supplementary Table 1.
The SNaPshot assay was used for AGXT and ABCC2 polymorphisms. Analysis was carried out using Genemapper software (version 4.0, Applied Biosystems, Carlsbad, CA, USA).
Two polymorphisms in the enhancer region of TS gene (the 28-bp variable number tandem repeat [VNTR] in the 5′ UTR (double repeat [2R] or triple repeat [3R]) of a 28-bp sequence and the G > C substitution in the second repeat of the 3R allele (3RG > 3RC) were evaluated and patients were grouped based on the expected TS expression level (‘high,’ 2R/3G,3C/3G,3G/3G; ‘low,’ 2R/2R,2R/3C,3C/3C) [14].
Ethnic SNP database
To investigate possible ethnic differences, we compared our allele and genotype frequency data with those selected from publicly available sources based on the International HapMap Project (http://hapmap.org/). The CEU (Centre d’Etude du Polymorphisme; Utah residents with northern and western European ancestry) population was defined as Western. Japanese in Tokyo (JPT) and Han Chinese in Beijing (CHB) were defined as Asians. Because the frequency data for TS (28-bp repeat in enhancer region, 6-bp deletion in 3′ UTR), AGXT 154C > T, GSTT1 (null genotype) and GSTM1 (null genotype) were lacking, ethnic frequencies of each polymorphisms were selected from previously published studies [11, 12, 22, 31].
Statistical analyses
Before assessing clinical associations, genotype frequencies were checked for agreement with those expected under Hardy–Weinberg equilibrium (HWE) (http://www.oege.org/software/hwe-mr-calc.shtml). Pearson’s χ 2 test and Fisher’s exact test were used as appropriate. Kaplan–Meier curves and log-rank tests were used for survival analysis, and multiple risk factors were analyzed using Cox proportional hazards model. Logistic regression was used for identifying factors jointly associated with risk of toxicity. Two-sided p values <0.05 were considered statically significant. The p values were presented without any correction for multiple comparisons. Genotypes were grouped after trying to seek the most significant association with phenotypes. Statistical analyses were performed with SPSS software for Window, version 17.0 (SPSS, Chicago, IL, USA).
Results
Patient characteristics
A total of 292 Korean patients (183 men and 109 women) from six hospitals in Korea were included and analyzed (median age, 59 years). Two hundred and fifty-two patients (86.3 %) received 12 complete cycles. The cause of early discontinuation was relapsed during treatment in 7, treatment toxicities in 11 (including peripheral neuropathy in 3, hypersensitivity for oxaliplatin in 3, neutropenia in 3 and others in 2), patient’s refusal or loss of follow-up in 14 patients and others in 8. Thirty patients (9.7 %) were found to have recurrent colon cancer after 15 months of follow-up. The characteristics of patients are presented in Table 1. After median 49.4 months of follow-up, there were 58 (19.9 %) relapses and 19 (6.5 %) deaths.
Toxicity and safety of chemotherapy
Regarding hematologic toxicity, 175 patients experienced severe neutropenia: 123 (42.5 %) grade 3 and 52 (18.0 %) grade 4. Grade 3/4 thrombocytopenia was present in 12 (4.2 %) patients.
Sensory neuropathy was experienced by 257 patients (88.0 %), but only 46 patients (15.8 %) had grade 2 neuropathy and five (1.7 %) patients had grade 3 (Table 2). As for non-hematologic toxicity, 16 patients (5.7 %) had grade 3/4 diarrhea and 4 patients (1.4 %) had an allergy to oxaliplatin.
Genotypes
All SNPs analyzed showed no deviation from the HWE except GSTP1 313A > G, which was excluded from further analysis. The frequency data of all studied genotypes are listed in Supplementary Table 2.
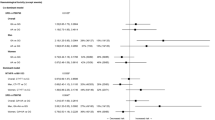
Significant differences in allele frequencies of 13 SNPs were observed between CEU and the present study, but only 3 SNPs were significantly different between CHB/JPT and the present study (Supplementary Table 3). It is also noteworthy that all patients in the present study, except a single patient with C/T, had the AGXT 154C/C genotype, which is different from the western population [11]. Representative genotypes of inter-ethnic difference are presented in Fig. 1. More detailed genotype frequency data are presented in the Supplementary Figures.
Representative genotypes of inter-ethnic difference. The allele and genotype frequency data of the present study were compared with those selected from publicly available sources based on the International HapMap Project (http://hapmap.org/). Utah residents with northern and western European ancestry (CEU) were defined as Europids. Japanese in Tokyo (JPT) and Han Chinese in Beijing (CHB) were defined as Asians. Because the frequency data for AGXT 154C > T were lacking, the ethnic frequency of the polymorphism in Europids was selected from a previously published study [11, 12, 22, 31]
Association between genotypes and toxicities
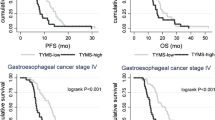
The MTHFR 677TT genotype was associated with higher risk for grade 3/4 neutropenia than MTHFR 677CC and CT (72.6 vs. 57.1 %, p = 0.027, Fig. 2a). ERCC1 19007TT carriers were at significantly higher risk compared with ERCC1 19007TC and CC carriers (85.0 vs. 58.6 %, p = 0.020, Fig. 2b). Using clinical factors such as cycles of chemotherapy delivered, sex, age, body surface area of the patient, stage of the tumor and Eastern Cooperative Oncology Group (ECOG) performance status as covariates, logistic regression also confirmed that development of grade 3–4 neutropenia was significantly associated with MTHFR 677TT (adjusted odds ratio 2.32, 95 % CI 1.19–4.55, p = 0.014) and ERCC1 19007TT carriers (adjusted odds ratio 4.58, 95 % CI 1.20–17.40, p = 0.026).
Associations between polymorphisms and toxicities (neutropenia and neuropathy). a MTHFR 677C > T polymorphism and neutropenia. Frequencies of grade 3–4 neutropenia according to the genotype and p value from χ 2 tests are presented. b ERCC1 19007T > C polymorphism and neutropenia. Frequencies of grade 3–4 neutropenia according to the genotype and p value from χ 2 tests are presented. c XRCC1 G23885A polymorphism and sensory neuropathy. Frequencies of grade 2 or higher neuropathy according to the genotype and p value from χ 2 tests are presented. d Time to the onset of grade 2–4 neuropathy. Time to the onset of grade 2 or higher neuropathy differs significantly according to XRCC1 G23885A genotypes (p = 0.041). Patients with GG genotype suffered from less neuropathy, and the onset of neuropathy was later
ABCC2 genotypes consisting of two variants were related to the appearance of grade 3/4 thrombocytopenia. ABCC2 −24CC polymorphism was associated with grade 3/4 thrombocytopenia than ABCC2 −24C/T and T/T polymorphisms [5.6 % (9 out of 160 patients with CC) vs. 0.8 % (1 out of 124 with CT or TT), respectively. p = 0.047].
Grade 2–4 sensory neuropathy was significantly associated with XRCC1 genotypes. Patients harboring the XRCC1 23885GG experienced less grade 2–4 neuropathy (12.9 vs. 21.7 %, p = 0.050, Fig. 2c). The association was also found in logistic regression using clinical factors as covariates (adjusted odds ratio 0.52, 95 % confidence interval 0.27–0.99, p = 0.046). Moreover, time to the onset of grade 2–4 neuropathy differed significantly according to XRCC1 G23885A genotypes (Fig. 2d, p = 0.041). Cox proportional hazards model, using sex, age, stage, ECOG performance status and cumulative dose of oxaliplatin as covariates also revealed that the onset of grade 2–4 neuropathy was later in patients harboring XRCC1 23885GG (adjusted hazard ratio (HR) 0.56, 95 % CI 0.32–0.99) compared to AA/AG.
Ethnic difference in genotype frequencies of genes related to toxicities
MTHFR 677TT homozygotes, associated with higher risk for grade 3/4 neutropenia, were more frequently found in Korean patients (21.2 %) than in western patients (8.2 %) (Supplementary Table 3; Fig. 1).
XRCC1 23885GG carriers, associated with less sensory neuropathy, were also more frequent in Korean (47.6 %) than in western people (38.4 %, p = 0.15).
All Korean patients in the present study had the AGXT 154C/C allele, which was associated with lower risk of neurotoxicity in a previous study, except one patient with the C/T allele [11]. Due to the homogeneity in genetic composition of the patients, association analysis of AGXT polymorphisms and neuropathy could not be performed in the present study.
Disease-free survival and overall survival according to the genetic and clinical characteristics
DFS for 98 patients with TS ‘low’ genotype was shorter than DFS for 194 patients with ‘high’ (3-year DFS, 75.6 vs. 84.8 %, p = 0.133, Fig. 3). The differences of DFS according to these genetic characteristics were significant also in the multivariable analysis (adjusted HR 1.71, 95 % CI 1.002–2.920, Table 3).
Patients who experienced grade 2–4 neuropathy had significantly longer DFS than who did not (3-year DFS, 92.1 vs. 79.5 %, p = 0.046). However, neither grade 3–4 neutropenia nor thrombocytopenia was related to DFS.
Overall survival did not differ according to the genotypes, due to the small number of events.
Discussion
The present study is the largest pharmacogenetic study of patients treated with adjuvant FOLFOX. In a previous study of 166 patients with metastatic disease treated with FOLFOX, SNPs of ERCC1 and XPD were associated with progression-free survival [23], but pharmacogenetics of adjuvant FOLFOX has not been widely studied. As expected, symptoms of clinically significant toxicity, such as neuropathy and neutropenia, were associated with SNPs in the genes encoding enzymes involved in drug metabolism in our study. Moreover, ethnic differences in toxicity profiles were found between the data obtained from Asian patients and that obtained from a western population.
Hematologic toxicities, including neutropenia (grade 3–4, 60.5 %) and thrombocytopenia (grade 3–4, 3.5 %) were more frequent in the present study of East-Asian (Korean) patients. The incidence of grade 3/4 neutropenia and thrombocytopenia was 41.1 and 1.7 %, respectively, in the MOSAIC study [2], and 32.6 and 3.4 % in NSABP C-08 [1]. In contrast, peripheral sensory neuropathy, which is well known as the most common adverse effect with oxaliplatin-based treatments, was less common in the present study. Only 16.4 % of the patients experienced clinically significant (grade 2 or higher) neurotoxicity. In the NSABP C-08, sensory neuropathy of grade ≥2 was reported in 43.7 % of patients. Our data are similar to those in the previous report in Asian patients, which showed grade 2–4 neuropathy in 27.7 % and grade 3–4 neutropenia in 52.2 % [17]. Taken together, there are clear ethnic differences in the toxicity profiles of FOLFOX chemotherapy. Moreover, it has been reported that Asian patients experience more cytopenia, especially severe neutropenia, from the dose of chemotherapy used in Western population, and dose reduction was frequently required in many studies [24].
MTHFR 677C > T changes Ala to Val in the catalytic domain, and the enzyme activity is reduced in TT-homozygous patients [19]. Therefore, it is conceivable that patients with MTHFR 677TT experience more toxicity symptoms, such as neutropenia. Moreover, MTHFR 677TT homozygotes were more frequently found in Korean patients (21.2 %) than in western patients (8.2 %). The frequencies of MTHFR C677T genotypes were statistically significant (p = 0.002). The higher incidence of neutropenia in Asian patients could partly be explained by this genotype. Neutropenia was also associated with ERCC1 T19007C polymorphism. ERCC1 19007TT carriers were more likely to experience significant neutropenia. This polymorphism at codon 118 (Asn118Asn) is a synonymous SNP, and may be associated with a reduced mRNA levels and subsequently a decreased ERCC1 protein, but the functional significance is not yet fully known [18].
Patients with the XRCC1 23885GG genotype experienced less neuropathy (grade 2 or more). Moreover, the onset of neuropathy was significantly late in patients with XRCC1 23885GG (Fig. 2d). The XRCC1 protein is important for BER and single-strand break repair pathway. The enzymatic activity of XRCC1 is reduced with the G23885A polymorphism [20]. Thus, patients with this polymorphism are theoretically prone to more toxicity from platinum therapy, as shown in the present study. Moreover, XRCC1 G23885A polymorphism is more frequently found in western people. The lower incidence of neuropathy (grade 2 or more) than determined from the western data could be associated with differences in this genotype.
The mechanism of oxaliplatin-induced neurotoxicity remains unclear, but the accumulation of heavy metals (i.e., platinum) has been thought to cause the neuronal damage. Gamelin et al. [11] have proposed another mechanism where oxalate synthesis pathway could be associated with platinum-drug neurotoxicity. A minor haplotype of the AGXT gene, which is implicated in the oxalate pathway, was able to predict both acute and chronic neurotoxicity [11]. The frequencies of the two SNPs (AGXT P11L and I340 M) are significantly different between the Gamelin et al. study and the present study. All patients in the present study had the AGXT 154C/C allele, except one patient with the C/T allele. As patients with the AGXT minor allele were considered to be at a higher risk of neurotoxicity, the lower incidence of neuropathy is in line with the less frequency of the AGXT polymorphism in our Asian patients.
The distribution of genetic polymorphisms of Korean patients was different from that of the Western population (Supplementary Table 3). The frequencies of 14 out of the 20 polymorphisms studied differed significantly from the western data as retrieved from the HapMap database or previously published reports [11, 12, 22, 31]. In contrast, the differences were small between Korean patients and the Japanese and Chinese populations. East Asians, including Koreans, could be considered as a distinct ethnic group, and further tailoring of the dosage and schedule of chemotherapy might be warranted [24]. Our findings of inter-ethnic diversity in SNPs could aid in understanding the genetic composition of the populations and discovering optimized chemotherapy.
Polymorphisms in genes encoding enzymes related to drug metabolism, including MTHFR, ERCC1 and XRCC1, have been studied, but the result has been contradictory and inconclusive [3, 5, 23]. We find significant associations in the present study in Korean patients treated with adjuvant FOLFOX, and further validation in both Caucasians and Asians in a prospective pharmacogenetic study might be warranted. Pharmacogenetics-based individualized therapy could improve patients’ tolerability of chemotherapy and treatment outcome.
Patients with TS ‘low’ genotype had shorter DFS than those with TS ‘high,’ and the differences of DFS was significant in the multivariable analysis after adjustment for clinical factors. TS ‘low’ (adjusted HR 1.71, 95 % CI 1.002–2.920, Table 3) was significantly related to shorter disease-free survival in the present study. This is in line with previous reports on colorectal cancers treated with post-operative adjuvant 5-FU treatment [7, 15], where outcomes of TS ‘low’ tumors were worse than ‘high’ tumors. These results are contradictory to the concept that TS ‘low’ tumors are more responsive to TS inhibitors such as 5-FU [22]. In the adjuvant setting, at least, TS ‘low’ phenotype indicates worse outcome, which could be the result of aggressive biology of these tumors or detrimental effect of adjuvant 5-FU therapy. As 5-FU is the backbone of chemotherapy for colorectal cancers, these warrants further research efforts to avoid unnecessary or even potentially harmful treatment.
In summary, neutropenia from FOLFOX chemotherapy was associated with MTHFR and ERCC1 genotypes. Neuropathy was associated with XRCC1 genotypes. Ethnic differences in genetic polymorphisms were associated with different toxicity profiles between our Korean patients and a western population. Also, TS ‘low’ genotype was related to shorter disease-free survival. Pharmacoethnic study of genetic polymorphisms could help to optimize and individualize chemotherapy for colon cancer.
References
Allegra CJ, Yothers G, O’Connell MJ, Sharif S, Colangelo LH, Lopa SH, Petrelli NJ, Goldberg RM, Atkins JN, Seay TE, Fehrenbacher L, O’Reilly S, Chu L, Azar CA, Wolmark N (2009) Initial safety report of NSABP C-08: a randomized phase III study of modified FOLFOX6 with or without bevacizumab for the adjuvant treatment of patients with stage II or III colon cancer. J Clin Oncol 27:3385–3390
Andre T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan P, Bridgewater J (2004) Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350:2343
Boige V, Mendiboure J, Pignon JP, Loriot MA, Castaing M, Barrois M, Malka D, Tregouet DA, Bouche O, Le Corre D, Miran I, Mulot C, Ducreux M, Beaune P, Laurent-Puig P (2010) Pharmacogenetic assessment of toxicity and outcome in patients with metastatic colorectal cancer treated with LV5FU2, FOLFOX, and FOLFIRI: FFCD 2000–05. J Clin Oncol 28:2556–2564
Bosch TM (2008) Pharmacogenomics of drug-metabolizing enzymes and drug transporters in chemotherapy. Methods Mol Biol 448:63–76
Chua W, Goldstein D, Lee CK, Dhillon H, Michael M, Mitchell P, Clarke SJ, Iacopetta B (2009) Molecular markers of response and toxicity to FOLFOX chemotherapy in metastatic colorectal cancer. Br J Cancer 101:998–1004
De Gramont A, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, Bonetti A, Clingan P, Lorenzato C, Andre T (2007) Oxaliplatin/5FU/LV in adjuvant colon cancer: updated efficacy results of the MOSAIC trial, including survival, with a median follow-up of six years. J Clin Oncol 25:4007
Edler D, Glimelius B, Hallstrom M, Jakobsen A, Johnston PG, Magnusson I, Ragnhammar P, Blomgren H (2002) Thymidylate synthase expression in colorectal cancer: a prognostic and predictive marker of benefit from adjuvant fluorouracil-based chemotherapy. J Clin Oncol 20:1721–1728
Evans WE, McLeod HL (2003) Pharmacogenomics–drug disposition, drug targets, and side effects. N Engl J Med 348:538–549
Fernandez-Contreras ME, Sanchez-Prudencio S, Sanchez-Hernandez JJ, Garcia de Paredes ML, Gisbert JP, Roda-Navarro P, Gamallo C (2006) Thymidylate synthase expression pattern, expression level and single nucleotide polymorphism are predictors for disease-free survival in patients of colorectal cancer treated with 5-fluorouracil. Int J Oncol 28:1303–1310
Funke S, Brenner H, Chang-Claude J (2008) Pharmacogenetics in colorectal cancer: a systematic review. Pharmacogenomics 9:1079–1099
Gamelin L, Capitain O, Morel A, Dumont A, Traore S, le Anne B, Gilles S, Boisdron-Celle M, Gamelin E (2007) Predictive factors of oxaliplatin neurotoxicity: the involvement of the oxalate outcome pathway. Clin Cancer Res 13:6359–6368
Huang K, Sandler RS, Millikan RC, Schroeder JC, North KE, Hu J (2006) GSTM1 and GSTT1 polymorphisms, cigarette smoking, and risk of colon cancer: a population-based case-control study in North Carolina (United States). Cancer Causes Control 17:385–394
Jemal A, Murray T, Ward E, Samuels A, Tiwari R, Ghafoor A, Feuer E, Thun M (2005) Cancer statistics, 2005. CA Cancer J Clin 55:10
Kawakami K, Watanabe G (2003) Identification and functional analysis of single nucleotide polymorphism in the tandem repeat sequence of thymidylate synthase gene. Cancer Res 63:6004–6007
Kornmann M, Schwabe W, Sander S, Kron M, Strater J, Polat S, Kettner E, Weiser HF, Baumann W, Schramm H, Hausler P, Ott K, Behnke D, Staib L, Beger HG, Link KH (2003) Thymidylate synthase and dihydropyrimidine dehydrogenase mRNA expression levels: predictors for survival in colorectal cancer patients receiving adjuvant 5-fluorouracil. Clin Cancer Res 9:4116–4124
Kweekel DM, Gelderblom H, Guchelaar HJ (2005) Pharmacology of oxaliplatin and the use of pharmacogenomics to individualize therapy. Cancer Treat Rev 31:90–105
P-H LEE, Y-S PARK, J-F JI, Y-T FU, Ratanatharathorn V (2009) Safety and tolerability of FOLFOX4 in the adjuvant treatment of colon cancer in Asian patients: the MASCOT study. Asia-Pacific J Clin Oncol 5:101–110
Li Y, Gu S, Wu Q, Fu X, Mao Y, Huang Y, Xie Y (2007) No association of ERCC1 C8092A and T19007C polymorphisms to cancer risk: a meta-analysis. Eur J Hum Genet 15:967–973
Little J, Sharp L, Duthie S, Narayanan S (2003) Colon cancer and genetic variation in folate metabolism: the clinical bottom line. J Nutr 133:3758S–3766S
Lunn RM, Langlois RG, Hsieh LL, Thompson CL, Bell DA (1999) XRCC1 polymorphisms: effects on aflatoxin B1-DNA adducts and glycophorin A variant frequency. Cancer Res 59:2557–2561
Lurje G, Manegold PC, Ning Y, Pohl A, Zhang W, Lenz HJ (2009) Thymidylate synthase gene variations: predictive and prognostic markers. Mol Cancer Ther 8:1000–1007
Lurje G, Zhang W, Yang D, Groshen S, Hendifar AE, Husain H, Nagashima F, Chang HM, Fazzone W, Ladner RD, Pohl A, Ning Y, Iqbal S, El-Khoueiry A, Lenz HJ (2008) Thymidylate synthase haplotype is associated with tumor recurrence in stage II and stage III colon cancer. Pharmacogenet Genomics 18:161–168
Morganti M, Ciantelli M, Giglioni B, Putignano AL, Nobili S, Papi L, Landini I, Napoli C, Valanzano R, Cianchi F, Boddi V, Tonelli F, Cortesini C, Mazzei T, Genuardi M, Mini E (2005) Relationships between promoter polymorphisms in the thymidylate synthase gene and mRNA levels in colorectal cancers. Eur J Cancer 41:2176–2183
O’Donnell PH, Dolan ME (2009) Cancer pharmacoethnicity: ethnic differences in susceptibility to the effects of chemotherapy. Clin Cancer Res 15:4806–4814
Sanoff HK, Sargent DJ, Green EM, McLeod HL, Goldberg RM (2009) Racial differences in advanced colorectal cancer outcomes and pharmacogenetics: a subgroup analysis of a large randomized clinical trial. J Clin Oncol 27:4109–4115
Stoehlmacher J, Park DJ, Zhang W, Groshen S, Tsao-Wei DD, Yu MC, Lenz HJ (2002) Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J Natl Cancer Inst 94:936–942
van der Put NM, Gabreels F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK, van den Heuvel LP, Blom HJ (1998) A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 62:1044–1051
Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4:307–320
Weisberg I, Tran P, Christensen B, Sibani S, Rozen R (1998) A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Metab 64:169–172
Won Y, Sung J, Jung K, Kong H, Park S, Shin H, Park E, Ahn Y, Hwang I, Lee D (2009) Nationwide cancer incidence in Korea, 2003–2005. Cancer Res Treat 41:122–131
Zhuo X, Cai L, Xiang Z, Li Q, Zhang X (2009) GSTM1 and GSTT1 polymorphisms and nasopharyngeal cancer risk: an evidence-based meta-analysis. J Exp Clin Cancer Res 28:46
Acknowledgments
This research was supported by Priority Research Centers Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009-0093820) and by Future-based Technology Development Program (Nano Fields) through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012-0001033).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
280_2013_2075_MOESM1_ESM.tif
Supplementary Figure 1 Inter-ethnic difference of genotype frequency. The allele and genotype frequency data of the present study were compared with those selected from publicly available sources based on International HapMap Project (http://hapmap.org/). Utah residents with northern and western European ancestry (CEU) were defined as Europids. Japanese in Tokyo (JPT) and Han Chinese in Beijing (CHB) were defined as Asians. Because the frequency data for TS (28-bp repeat in enhancer region, 6-bp deletion in 3′ UTR), AGXT 154C > T, GSTT1 (null genotype) and GSTM1 (null genotype) were lacking, ethnic frequencies of each polymorphisms were selected from previously published studies (TIFF 19173 kb).
Rights and permissions
About this article
Cite this article
Lee, KH., Chang, H.J., Han, SW. et al. Pharmacogenetic analysis of adjuvant FOLFOX for Korean patients with colon cancer. Cancer Chemother Pharmacol 71, 843–851 (2013). https://doi.org/10.1007/s00280-013-2075-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2075-3