Abstract
Previous research has demonstrated a critical link between maternal mental health and infant development. However, there is limited understanding of the role of autonomic regulation in postpartum maternal mental health and infant outcomes. In the current study, we tested 76 mother-infant dyads from diverse socioeconomic backgrounds when infants were 3-months of age. We recorded simultaneous ECG from dyads while baseline EEG was collected from the infant; ECG heart rate variability (HRV) and EEG theta-beta ratio and alpha asymmetry were calculated. Dyadic physiological synchrony was also analyzed to better understand the role of autonomic co-regulation. Results demonstrated that lower maternal HRV was associated with higher self-reported maternal depression and anxiety. Additionally, mothers with lower HRV had infants with lower HRV. Maternal HRV was also associated with higher infant theta-beta ratios, but not alpha asymmetry. Exploratory analyses suggested that for mother-infant dyads with greater physiological synchrony, higher maternal HRV predicted increased infant theta-beta ratio via infant HRV. These findings support a model in which maternal mental health may influence infant neurophysiology via alterations in autonomic stress regulation and dyadic physiological co-regulation.
Similar content being viewed by others
Introduction
The prevalence of postpartum mental health concerns among new mothers is on a disconcerting rise1. This is especially concerning as maternal mental health in the perinatal period is known to shape the infant-caregiver relationship and consequent child development2,3,4. However, previous research in this domain have primarily used self-reported measures of psychological distress. Self-report measures are prone to bias, resulting in both over and underreporting of symptoms and offer limited mechanistic insight. While self-report measures of maternal mental health are considered the gold-standard in research, there are notable drawbacks of this approach. Namely, widely used self-reported perinatal mental health measures demonstrate poor cross-cultural validity5, which raises concerns about the accuracy of these measures for diverse sociocultural populations. Thus, research evaluating objective measures that could offer more accurate assessments of depression and anxiety among new mothers is warranted. To better understand the biological mechanisms underlying individual differences in maternal mental health, physiological indices of maternal emotion regulation can be evaluated. Specifically, by examining the maternal stress physiology system, we can gain insights into how maternal psychological distress can influence infant outcomes. Research in this domain is imperative for advancing our understanding of the interplay between maternal well-being and child development.
Heart rate variability (HRV), a measure of the intervals between heartbeats, is a candidate marker of physiological stress regulation that could help elucidate the relation between maternal mental health and infant outcomes. Heart rate variability (HRV) is commonly used to characterize the fast-acting autonomic nervous system (ANS). The ANS comprises two branches: the sympathetic (SNS) and parasympathetic (PNS) branches, representing the “fight-flight-freeze” and “rest and restore” stress systems, respectively. Although the precise physiological mechanisms contributing to heart rate variability (HRV) are still being explored, literature suggests that HRV reflects the balance between sympathetic and parasympathetic nervous system activity and can be used to index physiological stress regulation, more broadly6,7,8.
Past research proposes that HRV approximates the capacity for adaptive regulation of autonomic response to perceived threats and exert top-down cognitive control across the lifespan9,10. Specifically, higher HRV is associated with greater adaptive autonomic regulation and lower HRV is associated with more maladaptive responses to stress. For example, individuals with lower HRV are shown to be less effective at regulating incoming negative emotional stimuli relative to individuals with higher HRV11. Critically, HRV is not a fixed construct but demonstrates individual-level fluctuations, both improvements and disruptions12. Neurobiologically, it has been proposed that HRV is linked with the functional activation of neuroanatomical structures responsible for the detection of threat and safety12,13. Thus, individuals who demonstrate consistent maladaptive threat awareness may also show lower HRV, indicative of heightened reactivity and inadequate recovery of the stress response. Continually elevated states of perceived stress can result in wear and tear on both physical and psychological well-being, impacting overall health and mood14,15.
Maternal heart rate variability (mHRV) has predominantly been evaluated during the prenatal period16,17. Studies in this domain have underscored the importance of mHRV in characterizing cardiorespiratory features of maternal health, with findings suggesting its predictive value for conditions like preeclampsia and other prenatal complications18,19,20. Notably, lower prenatal mHRV scores have been associated with increased prevalence of anxiety disorders during late pregnancy17. Despite these insights, a significant gap exists in the literature regarding the replication of these findings in the postnatal period. Existing studies measuring mHRV within stress-induced contexts, such as the Still-Face paradigm, have revealed associations between mHRV responsiveness and symptoms of depression and anxiety21,22,23. However, there is a lack of research evaluating mHRV at baseline, without any experimental emotion induction. Such studies are necessary to characterize ANS function independent of external stressors, given the documented links between baseline mHRV and prenatal mental health outcomes. The postpartum period is marked by significant physiological and emotional fluctuations as mothers adapt to childbirth and child-rearing25,26,27. Thus, the postpartum period is a critical phase for characterizing biological markers of effective stress regulation systems during this critical phase.
From a psychobiological perspective, assessing caregivers’ physiological stress regulation is crucial as caregivers play an important role in shaping their child’s own stress regulation system development25,28,29,30. Infants are born with immature stress response systems, and thus rely on caregivers for stress regulation24. This co-regulation can occur through behavioral (e.g., soothing) or covert physiological means (e.g., heart-rate synchrony)31,32. When caregivers struggle to manage their own physiological stress, it can lead to atypical patterns of autonomic stress regulation in their infants33,34,35,36. This is because the developing infant ANS and brain are highly receptive to cues from caregivers26,33,37,38. Indeed, research has shown that mHRV changes can regulate infants’ HRV in real-time during maternal breathing exercises39. Consequently, the varied stress cues provided by caregivers may induce changes in the infant’s physiology, including variability (HRV and neural activity29,40.
Two candidate neural markers of infant cognitive and emotion regulation measured using EEG are theta-beta ratio and frontal alpha asymmetry, respectively. Theta-beta ratio is a relative EEG power metric that indicates the abundance of lower frequency power relative to high frequency power. It is believed to reflect the maturation of cortical-subcortical networks that support emerging attentional control processes41,42. Indeed, research has found that higher theta-beta ratios (indicating more relative theta power) at 10 months is predictive of differences in cognitive control over one year later43. Additionally, relative EEG power metrics are sensitive to variations in environmental input. Studies have shown that infants of higher stressed mothers exhibit higher relative theta power compared to higher frequency power44,45. Relatedly, infant frontal alpha asymmetry has been predictive of later emotion regulation abilities in childhood46,47,48 and has been suggested as a potential mechanism explaining intergenerational transmission of depression49,50,51.
The current study leverages unique triadic data collected through concurrent recordings of maternal and infant ECG and infant EEG (N = 76) at 3-months of age. Our study objectives were threefold. Firstly, we examined the associations between mHRV and self-reported experiences of depression, anxiety, and stress. Secondly, we investigated how individual differences in average mHRV levels correlated with infant stress physiology and neural function. Lastly, in an exploratory analysis we examined dyadic physiological synchrony between infant and maternal HRV as a moderator and mediator of associations between mHRV and infant neurophysiology. To incorporate and consolidate diversity in HRV calculations, we employed factor analysis to derive a composite mHRV factor score, encompassing frequency, and non-linear quantifications of heart rate activity. We chose a factor analysis approach primarily due to our theoretical assumption that the latent factor of autonomic regulation underlies observed HRV variables. Similar approaches have been adopted in studies linking HRV to cognition and mood in healthy adults52. This factor score incorporated high-frequency (HF) band power, low-frequency (LF) to HF power ratio, and a non-linear HRV measure, namely DFA Alpha 1, to assess the complexity and irregularity of heart rate dynamics. We hypothesized that lower mHRV would be associated with higher maternal reports of depression, anxiety, and perceived stress. We also hypothesized that higher mHRV would be concurrently associated with higher infant HRV, lower infant theta-beta ratios, and lower infant frontal alpha asymmetry.
Results
Heart rate variability (HRV) factor score
Using confirmatory factor analysis (CFA), we computed a single latent factor score for heart rate variability (HRV) using high-frequency (HF) band power, low-frequency to HF power (LFHF) ratios, and DFA Alpha 1. The decision to estimate a single factor score was justified by the significant correlations observed among HRV variables across different domains, see Table 1. The primary purpose of the CFA was twofold: (1) to estimate a robust latent measure of maternal autonomic regulation and (2) to enhance the measurement specificity of a mHRV score by reducing measurement error.
Maternal HRV (mHRV), anxiety, depression, and perceived stress
For our primary research question, we evaluated associations among mHRV and maternal depression, anxiety, and perceived stress (Table 2). Results demonstrated a significant negative association between mHRV scores with maternal depression and anxiety. There was a trend-level negative association between mHRV scores with maternal perceived stress (See Fig. 1). In other words, mothers with lower mHRV reported significantly higher rates of depression and anxiety. Maternal age, income-to-needs ratio, maternal education, and resting HR were included as covariates but did not show a significant effect. State anxiety was positively associated with all mental health outcomes.
Maternal HRV (mHRV), infant HRV (iHRV), and infant neural markers
Next, we evaluated associations between mHRV scores with infant physiological and neural outcomes. We included infant age, sex, and maternal self-reported mental health using a factor score of the previously evaluated anxiety, depression, and perceived stress (See Table 3). Results demonstrated a significant positive association of mHRV with infant HRV (iHRV) and a significant negative association with infant theta-beta ratio values (See Fig. 2). In other words, for mothers with lower HRV, their infants also showed lower HRV and greater theta power relative to beta power. There were no significant associations with frontal alpha asymmetry. There were also no significant effects of the included covariates in our regression models.
Exploratory dyadic physiological synchrony analysis
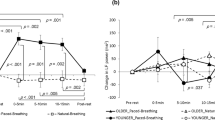
We conducted an exploratory analysis to investigate if the coordination of mother-infant HRV may moderate the relationship between mHRV and infant neurophysiology. To calculate physiological synchrony, we applied 0-lag cross-correlations within each dyad between 30-s HF HRV epochs, to estimate synchrony in respiratory sinus arrythmia (RSA)29,53. We then replicated the infant outcome regressions above but included a main effect term of physiological synchrony and an interaction term of physiological synchrony X mHRV (See full table of results in SI). With iHRV modeled as the dependent variable, there was a main effect of physiological synchrony (β = 0.26, p = 0.02) and an interaction effect of physiological synchrony X mHRV on iHRV (β = 0.25, p = 0.02). Analysis of simple slopes indicated that the positive association between average mHRV and iHRV was amplified among individuals with greater physiological synchrony (mean + 1 SD: β = 0.51, p = 0.001) relative to those with little to no physiological synchrony (mean − 1 SD: β = 0.01, p > 0.05; See Fig. 3a). Further, when the interaction term was added to the model, the R-squared increased from 0.15 to 0.28, suggesting that an additional 13% of the variance in infant HRV was explained by the physiological synchrony main effect and interaction terms. There were no main or interaction effects of physiological synchrony on infant EEG outcomes.
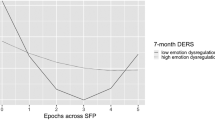
In a secondary exploratory analysis, our aim was to evaluate a theoretical pathway in which physiological synchrony regulates iHRV, consequently influencing infant neural activity. Specifically, we tested moderated mediation to evaluate if iHRV (conditional upon physiological synchrony) mediated the relationship between mHRV and theta-beta ratio. Our analysis revealed that the interactive effects between iHRV and physiological synchrony played a mediating role in the association between mHRV and the theta-beta ratio (β = − 0.06, CI [− 0.26, − 0.003]; see Fig. 3b). Notably, the mediating role of iHRV was heightened among dyads exhibiting greater positive physiological synchrony (mean + 1 SD: β = − 0.13, CI [− 0.52, − 0.01]), compared to those with lower synchrony (mean − 1 SD: β = − 0.050, CI [− 0.003, − 0.00]).
Discussion
There is a pressing need to comprehensively understand the physiological underpinnings of maternal mental health during the perinatal period and its impact on infant development. In this study, we investigated maternal heart rate variability (mHRV) in relation to maternal mental health and evaluated associations between mHRV and infant neurophysiological outcomes at 3 months of age using concurrently recorded dyadic HRV and infant EEG. We present novel evidence of an association between an mHRV factor score and maternal self-reports of depression and anxiety symptoms. Additionally, we established an association between mHRV and infant neurophysiology. Finally, we found that dyadic physiological synchrony may amplify the link between mHRV and infant neural function through infant HRV. These findings reinforce mounting evidence highlighting the crucial role of caregiver well-being in infant development35,45,54,55,56 and provide empirical support for a pathway by which caregivers may influence their infant through physiological co-regulation.
The first aim of this study was to evaluate whether a factor score of mHRV, which accounted for shared variance across multiple measures of HRV, was associated with maternal mental health. Controlling for socioeconomic factors and situational anxiety, we found that higher mHRV was correlated with lower levels of depression and anxiety, but not perceived stress. Given that HRV is thought to reflect adaptive autonomic nervous system regulation, caregivers who are physiologically equipped to manage stress in their environment may be less likely to experience psychological distress12,57. Specifically, it has been posited that stronger ANS regulation may buffer an individual’s likelihood of developing mental health conditions such as depression and anxiety58,59. Further, the null association between mHRV and perceived stress is consistent with previous research that has demonstrated a disconnect between physiological stress and perceived stress60. In general, this finding adds to a growing body of literature linking physiological stress with mental health20,57,61,62. These findings are aligned with research by Kimmel and colleagues demonstrating that lower prenatal HRV scores were associated with increased prevalence of anxiety disorders during late pregancy17. Similarly, these findings also support past research demonstrating differences between HRV reactivity and regulation during caregiver-infant interactions based on symptoms of anxiety and depression21,29. Our findings expand upon the existing literature by linking maternal HRV with normative variation in postpartum mental health experiences within a community sample of mothers.
Prior research has established that maternal psychological distress can interfere with the caregiver-infant relationship and subsequent child development 36,63,64,65. However, relatively little research has looked at the caregiver’s physiological states as a predictor of infant neural and physiological function45,66,67. We found a positive relation between mHRV and infant HRV (iHRV), such that mothers with lower group average mHRV were more likely to have infants with lower group average iHRV. Given that infant and caregiver ECG was recorded simultaneously, we explored the possibility that the between-person associations in HRV were modulated by real-time physiological linkage occurring while the infant was seated on the caregiver’s lap. We found that physiological synchrony within dyads moderated the association between mHRV and iHRV across dyads. In other words, mothers with low mHRV were more likely to have infants with correspondingly low HRV if they exhibited high physiological synchrony, and vice versa for high mHRV. These findings suggest that physiological co-regulation may underlie the positive correlation observed between average mHRV levels and average iHRV levels across individuals, aligning with prior dyadic physiological synchrony literature29,39,68,69,70,71,72. This finding is particularly notable considering that infants were positioned on their mothers’ laps during concurrent recording of dyadic ECG, suggesting evidence of real-time physiological co-regulation potentially facilitated by physical touch73,74. These findings are aligned with prior dyadic synchrony literature demonstrating that experimental manipulation of maternal HRV shows moment-to-moment regulation effects of infant HRV during physical touch39. Moreover, we found evidence of a main effect of physiological synchrony on iHRV, suggesting that greater synchrony is predictive of higher iHRV. This finding may be explained by research suggesting that physiological synchrony captures a critical aspect of the caregiver-infant dynamic, which may drive infant physiological regulation in and of itself29,75.
Our results also demonstrate that higher mHRV scores were correlated with lower infant theta-beta ratios. Mothers who showed greater ANS regulation tended to have infants with increased high-frequency oscillations and lower low-frequency oscillations. Lower theta-beta ratios are neural signatures associated with increased top-down regulation and have been linked to increased attentional control43. Thus, these findings would suggest that children of caregivers with a more regulated physiological stress profile tend to showcase a pattern of neural function associated with greater cognitive control or regulation. Interestingly our regression models linking mHRV to iHRV and theta-beta ratio remained significant after controlling for a host of potentially confounding covariates including maternal mental health. This would suggest that above and beyond perceived psychological experiences, there is utility in measuring caregiver physiological functioning to better understand how caregivers regulate their infant in ways that could affect early trajectories of development16,17. There were no significant associations between mHRV and infant frontal alpha asymmetry. This could possibly be explained by the ontogenetic development of brain specialization that underpins observed differences in alpha asymmetry76. Infant brain hemispheres remains relatively unspecialized for the first months of life, particularly in the frontal cortex as this region of the brain follows as more protracted developmental course77. Indeed, clearer evidence of cortical specialization emerges around 6-months of age, which may lead to more distinct individual differences in alpha asymmetry emerging at this time50,78.
Interestingly, results did not demonstrate any significant interaction effects between mHRV and physiological synchrony on either infant neural outcome, suggesting that mHRV may not be regulating infant EEG directly via synchrony. This finding led us to conduct an exploratory path analysis evaluating indirect effects of mHRV on theta-beta ratio via the interaction of iHRV and dyadic physiological synchrony. Tests of indirect effects revealed that the association between mHRV and infant theta-beta ratio was mediated by iHRV, conditional upon level of physiological synchrony. To elaborate, for mother-infant dyads with high physiological synchrony, iHRV significantly mediated the relation between mHRV to infant neural function. This could suggest that mothers regulate infant HRV via physiological synchrony, and in turn, infant HRV modulates neural function22,79. Taken together, these findings provide preliminary evidence for a pathway through which maternal autonomic regulation may influence infant neural activity via co-regulation of infant’s autonomic nervous system.
Several limitations warrant careful consideration in the context of this study. First, our sample size is relatively modest. To strengthen the robustness of our findings, particularly the more complex moderated mediation analysis, future research should aim to replicate these results with a larger dataset. Furthermore, due to the cross-sectional and observational nature of this investigation, it is crucial to acknowledge that causal directionality cannot be inferred. To address these limitations, future research should also measure contingent associations to explore the interplay between changes in concurrent mHRV and dynamic shifts in maternal mood and emotion. This line of inquiry could provide deeper insights into the intricate relationship between autonomic balance and maternal experiences and behaviors. Additional research is also needed to explore the potential mediating role of infant autonomic function in regulating neural activity. While these questions were not within the scope of present study, future endeavors are warranted to gain a deeper understanding of the interplay between maternal and infant neurophysiology. Lastly, future studies should aim to utilize longitudinal data to advance the field’s understanding of how individual differences in maternal autonomic regulation may have enduring impacts on infant development.
The current study sought to investigate maternal autonomic functioning at three months postpartum, an important phase characterized by rapid biopsychosocial changes within caregiver-infant dyads. Our findings provide novel evidence in support of resting maternal heart rate variability as a robust indicator of caregiver mental health. Results also showed that higher maternal heart rate variability corresponded to infant neural EEG profiles associated with heightened attentional control. Moreover, analyses of dyadic physiological synchrony offer evidence for a pathway by which maternal autonomic regulation could impact infant neurophysiology activity through the co-regulation of the infant’s autonomic nervous system function. Together, our findings emphasize the importance of assessing the biological underpinnings of caregiver stress during the postnatal period. This knowledge could facilitate the early identification of caregivers in need of additional support due to mental health concerns, highlighting the potential significance of this research in clinical practice.
Methods
Participants
Infants and their mothers were recruited through diverse channels, including community events, family services, healthcare providers, and flyers distributed at local businesses in the New York metropolitan area. These participants were originally enrolled in a larger longitudinal study conducted between May 2018 and December 2019. To be eligible for the present study, participants were excluded if their child was born before 36 weeks gestation, if they had multiple births, or if the child had a developmental disorder. We recruited 104 participants into the study, however, data loss occurred at various stages of the data collection and processing, resulting in a usable sample size of N = 76 (See Table 4).
Detailed demographic information for the participants can be found in Table 5. The study was conducted in accordance with the principles outlined in the Declaration of Helsinki, and written informed consent was obtained from a parent or legal guardian before any assessments or data collection occurred. All research procedures were approved by the New York University Institutional Review Board (IRB).
Protocol
Families visited the lab when their infant was approximately 3 months of age. During the visit, ECG was recorded from mother and infant while EEG was simultaneously recorded from the infant. Mothers also completed responses to socio-demographic and mental health questionnaires.
Measures
Family and household characteristics
Questionnaires collected information on demographic factors such as maternal and infant age, race, and ethnicity. Additionally, caregivers provided details regarding their highest level of education completed and the annual household income. To assess the socioeconomic status of the families, the income-to-needs ratio (ITN) was calculated by dividing the total household income by the federal poverty line that corresponds to the number of adults and children in the household.
Maternal mental health
We collected surveys of maternal depression, anxiety, and stress to capture mothers perceived mental health states. Maternal depression was measured using the Edinburgh Postnatal Depression Scale108 and maternal anxiety was measured using the State-Trait Anxiety Inventory109. The Edinburgh Postnatal Depression Scale (EPDS) consists of ten items that capture various aspects of mood and emotional well-being. Each item is scored on a four-point Likert scale with higher scores indicating a higher level of depressive symptoms (Cronbach’s alpha range between 0.73 and 0.87). The State-Trait Anxiety Inventory (STAI) assesses two aspects of anxiety: state anxiety and trait anxiety. The state anxiety domain measures in-the-moment experiences of temporary anxiety while the trait anxiety domain measures chronic trait-like experiences of anxiety. Item responses are scored on a four-point Likert scale with higher scores indicating greater anxiety (Cronbach’s alpha range between 0.86–0.95). For the current analysis we used the STAI trait anxiety total score as a primary outcome. State anxiety was included as a covariate to control for any contextual experiences of temporarily heighted anxiety during experimental testing. Maternal perceived stress was measured using the Perceived Stress Scale (PSS; Cohen et al.110). The PSS is a 14-item questionnaire that asks the respondent to report on their levels of experienced stress in situations during the past month. The perceived stress score was the summed score across all items (Cronbach’s alpha > 0.70).
Confirmatory factor analysis (CFA) was used to derive a composite factor score of maternal mental health for use in all infant outcome models. The factor analysis used the total score from the EPDS, STAI trait, and PSS. All variables significantly loaded (p < 0.001) on the fully saturated CFA model, indicating strong associations. Fit indices suggest excellent fit. (CFI = 1.0, TLI = 1.0, Chi-square = 172.21 p = 0.00, RMSEA = 0.00 [90% CI 0.00–0.00], SRMR = 0.00).
EEG data acquisition & processing
Resting EEG data were acquired while infants watched a video of engaging, non-social stimuli (e.g., bubbles, spinning wheel) while seated on their caregivers’ laps. The recording room was dimly lit and an experimenter was nearby to soothe the infant with bubbles or a toy if the infant became too fussy. Infants provided between 42 and 600 s (M = 406, SD = 142) of baseline data. EEG was recorded using a 64-channel HydroCel Geodesic Sensory Net (Electrical Geodesic, Inc., Eugene, OR) and amplifier (Electrical Geodesic, Inc., Eugene, OR; EB NEURO S.p.A., Firenze, Italy). Electrode impedances were kept below 100 KΩ and the sampling rate was recorded at 1000 Hz.
All EEG files were processed in batch using an electroencephalography automated processing platform (BEAPP) software to ensure standardization in data processing and cleaning across all files (See Fig. 5)80. Continuous resting EEG files were converted from NetStation format to Matlab format. Data preprocessing was carried out using the Harvard Automated Processing Pipeline for EEG (HAPPE V.1), an automated preprocessing pipeline designed for infant EEG data81. First, a 1 Hz high-pass and 100 Hz low-pass filter was applied to each EEG recording. Second, the data, which was originally sampled at 1000 Hz was resampled with interpolation to 250 Hz, following guidelines for further HAPPE processing. The third step involved artifact removal and included CleanLine’s multitaper approach to removing 60 Hz electrical noise, bad channel rejection, and wavelet-enhanced ICA for artifact rejection with automated component rejection through the Multiple Artifact Rejection Algorithm82 in EEGLAB. A subset of spatially distributed electrodes was selected for analysis with MARA: E2, E3, E5, E9, E10, E11, E12, E13, E14, E18, E20, E24, E25, E28, E30, E31, E35, E39, E40, E42, E44, E48, E50, E52, E57, E58, E59, E60 (NetStation Geodesic 64- Channel Net). Bad channels that were initially rejected were repopulated using spherical interpolation to reduce bias in re-referencing and the signal was mean detrended. Finally, each EEG file underwent segmentation into 2-s windows, with each segment subsequently evaluated for residual artifacts. On average, 24 segments were rejected per file (SD = 10, range = 0–48). Segment rejection thresholds were determined according to HAPPE’s automated rejection criteria81, which uses amplitude thresholding and assessment of segment likelihood using joint probability calculations. EEG power decomposition was accomplished using Fast Fourier transformation using a multitaper windowing (3 windows) to decompose power into 2-s segments for each channel.
We calculated power in low and high discrete frequency bands, specifically spectral power was computed for Theta (4–6 Hz), Alpha (6–9 Hz), and Beta (13–20 Hz). Relative power at each channel was computed by summing the power within each frequency band, averaging across all segments, and then dividing by the total power spectrum (2–50 Hz). Two measures of infant neural activity were calculated. First, we computed the theta-beta ratio using whole brain electrodes (See Fig. 4A) to obtain a neural measure indicating the higher abundance of EEG frequencies compared to lower frequencies by dividing relative beta by relative theta. An increased proportion of slow wave (theta) oscillations relative to fast wave oscillations (beta) has shown associations with reduced attentional control during infancy 83,84,85. Furthermore, higher theta-beta ratios during infancy are predictive of lower cognitive control later in childhood43,86,87. We also calculated frontal alpha asymmetry to derive a neural marker of emotion regulation by subtracting log-transformed right frontal hemisphere power values from left frontal hemisphere power values (See Fig. 4B)50,88. Alpha asymmetry during infancy has been correlated with emotion regulation development56.
ECG data acquisition & processing
Dyadic ECG data was collected while infants were seated on their mother’s laps during infant EEG acquisition using a Physio16 (EGI) device (See Fig. 5). Mothers and infants provided an average of 200 + /- 72 s of resting ECG data (min = 23 s, max = 385 s). Data were edited and processed using the software QRSTool89 to remove artifacts and identify heartbeats. R-R intervals were extracted from the processed ECG data. We calculated 3 different indices of heart rate variability that have been associated with autonomic nervous system (ANS) activity6,90. All HRV features were calculated with pyHRV91, a reliable Python signal processing toolbox. Seconds of provided ECG data were not significantly correlated with any of the HRV variables (p’s > 0.21).
Within the frequency domain of the ECG signal, we calculated high-frequency power (HF) and the ratio of low-frequency to high-frequency power (LF/HF) to evaluate the degree to which heart rate is distributed across frequencies92,93. To calculate frequency domain metrics, the RR signal is transformed using fast Fourier transformation to estimate the signal’s power spectral density (PSD) using Welch’s method. Absolute (sum of power) and log-transformed power was estimated within LF (0.04–0.15 Hz) and HF (0.15–0.40 Hz) discrete frequency bands for mothers and LF (0.04–0.24 Hz) and HF (0.24–1.04 Hz) for infants39,92,94,95. HF power was normalized to the entire power spectrum to correct for skew in the distribution. The LF/HF ratio is calculated by dividing the total absolute power of the LF band by the total absolute power of the HF band and multiplying by 100.
Finally, non-linear quantitative approaches were used to capture the aperiodic dynamics of HRV activity96. DFA alpha 1, a scaling exponent, was computed through the following steps:
(1) Integration of the total time series signal; (2) Division of the integrated signal into segments of equal length; (3) Subtraction of a linear least square regression line within each segment to detrend the data; (4) Application of Root-Mean-Square fluctuation analysis to each detrended segment; (5) Repetition of the analysis using varying segment sizes to capture the relationship between fluctuation and time scale For DFA alpha 1, segments ranging from 4 to 16 heartbeats were analyzed (see Fig. 6); (6) Generation of a logarithmic plot to examine this relationship; (7) Fitting a linear regression line to the log–log plot to obtain DFA alpha 1, where the slope represents the scaling exponent. DFA alpha 1 allows us to extract correlations between successive RR intervals over different time scales, offering insights into the underlying physiological mechanisms and regulatory dynamics of the cardiovascular system. Short-term DFA correlations reflect the activity of the baroreceptor reflex97. The baroreceptor reflex is a physiological mechanism that helps regulate blood pressure. In response to changes in blood pressure, the baroreceptor reflex mediates a coordinated response through the ANS. Activation of the baroreceptor reflex leads to inhibition of the sympathetic nervous system and activation of the parasympathetic nervous system.
Using confirmatory factor analysis (CFA), we computed a single latent factor score for heart rate variability (HRV) using the four indices. To assess the goodness of fit of the CFA model, we employed several fit indices, namely the Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Standardized Root Mean Square Residual (SRMR), and Tucker-Lewis Index (TLI). These indices provided valuable information about the adequacy of the model in representing the observed data. All CFA analyses were performed using the Lavaan package in R98. Findings indicated that all indicator variables loaded significantly on the HRV factor score (p < 0.001), providing support for the validity of the factor structure. The model fit statistics indicated good fit to the data (CFI = 1.00, TLI = 1.00, Chi-square = 186.00 p = 0.00, RMSEA = 0.000 [90% CI: 0.00–0.00]; SRMR = 0.000). These results confirm that the four HRV indices were meaningfully associated with the latent HRV factor score. The excellent fit of the model and the significant factor loadings suggest that the HRV factor score provides a comprehensive representation of maternal HRV, encompassing different domains of measurement. We replicated the CFA model using infant HRV indices and found a similar outcome. All indices loaded significantly on the latent HRV factor score and the model fit statistics indicated excellent fit to the data (CFI = 1.00, TLI = 1.00, Chi-square = 230.38 p = 0.00, RMSEA = 0.000 [90% CI: 0.00–0.00]; SRMR = 0.000).
Dyadic physiological synchrony analysis
To compute a metric for dyadic physiological synchrony, we calculated HF HRV on 30-s epochs of mother-infant IBI data using the same established pipeline and parameters utilized for the HRV factor score. We chose to calculate HF HRV for the synchrony analysis as HF HRV is associated with Respiratory Sinus Arrhythmia (RSA), which is commonly studied in the context of dyadic physiological synchrony in existing literature68,69,99,100. Physiological synchrony between maternal and infant HRV was assessed for each dyad by computing 0-lag cross-correlations on linearly detrended IBI epochs101 to investigate concurrent changes in parent-infant ANS activity. Only dyads with at least 2 min of usable ECG data were included in the synchrony analysis (5 dyads were removed for having less than 2 min of ECG). Cross-correlations were computed using the tseries package in R102. The cross-correlation coefficient for each dyad was subsequently utilized as an independent variable in subsequent analysis. Thus, positive cross-correlation coefficients reflect synchrony, whereas coefficients that are 0 or negative reflect a lack of synchrony. Moreover, we refer to higher and lower synchrony values relative to sample averages, where high is + 1 SD above the sample average and low is − 1 SD below the sample average (Supplementary Table 1).
Data analysis
The overall aim of our analysis is to evaluate the relationship between maternal heart rate variability (HRV) with maternal mental health and infant neurophysiological activity. Our analysis involved several statistical techniques to explore these associations and address our research questions. First, we conducted Pearson correlations to explore the relations between all numeric maternal HRV variables and both maternal and infant outcomes. This analysis allowed us to assess the strength and direction of the correlations between the variables of interest. Next, we constructed multiple regression models to address our primary research questions regarding the relationship between maternal HRV with mental health and infant neurophysiological function at 3 months of age. In the first set of regression models, we included maternal depression, trait anxiety, and perceived stress as dependent variables, while maternal HRV was included as the independent variable. Additionally, we included income-to-needs, maternal age, and maternal resting heart rate (HR), and situational state anxiety as covariates to account for their potential influence. Situational state anxiety was included as a covariate in our first set of models to account for potential short-term experiences of heightened anxiety resulting from testing within an unfamiliar laboratory environment, which could influence HRV readings103. In the second set of regression models, we examined the association between maternal HRV factor score with infant HRV factor score and two infant neural outcomes: theta-beta ratio and alpha asymmetry. In the exploratory physiological synchrony analysis, we employed tests of statistical moderation using grand-mean centered mHRV and synchrony scores to compute the interaction term. Significant interactions were probed at one standard deviation below (lower physiological synchrony) and above (higher physiological synchrony) the mean104. Maternal reported mental health factor scores, maternal resting HR, infant age, and gestational age were included as covariates in all models. Maternal resting HR was included as a covariate in our regression models given the high covariance between HRV and resting HR16. Statistical mediation tests employed bootstrapping with 5000 samples to generate bias-corrected confidence intervals for indirect effects105. To increase model parsimony and reduce overfitting, non-significant covariates were removed from the final path analysis.
We screened all regression models for influential outlier data points by examining studentized residuals using the outlierTest function from the car package in R106. Outliers were identified using a threshold of 3, and the Bonferroni correction method was applied to adjust for multiple comparisons. Only one outlier was identified when maternal anxiety was modeled. This individual was removed from the final model. Full information maximum likelihood (FIML) was used to account for missing data in all analyses, as FIML produces unbiased parameter estimates. All mHRV p-values reported were adjusted for multiple comparisons (3 p-values per family of test) using Benjamini–Hochberg procedure for false discovery rate (FDR) correction107. All models were run in the R environment.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Pearson, R. M. et al. Prevalence of prenatal depression symptoms among 2 generations of pregnant mothers: the Avon longitudinal study of parents and children. JAMA Netw. Open 1, e180725 (2018).
Riva Crugnola, C. et al. Mother-infant emotion regulation at three months: The role of maternal anxiety, depression and parenting stress. Psychopathology 49, 285–294 (2016).
Hakanen, H. et al. How maternal pre- and postnatal symptoms of depression and anxiety affect early mother-infant interaction?. J. Affect. Disord. 257, 83–90 (2019).
Slomian, J., Honvo, G., Emonts, P., Reginster, J.-Y. & Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Womens. Health 15, 1745506519844044 (2019).
Chan, A. W., Reid, C., Skeffington, P. & Marriott, R. A systematic review of EPDS cultural suitability with Indigenous mothers: A global perspective. Arch. Womens. Ment. Health 24, 353–365 (2021).
Rajendra Acharya, U., Paul Joseph, K., Kannathal, N., Lim, C. M. & Suri, J. S. Heart rate variability: A review. Med. Biol. Eng. Comput. 44, 1031–1051 (2006).
Heiss, S., Vaschillo, B., Vaschillo, E. G., Timko, C. A. & Hormes, J. M. Heart rate variability as a biobehavioral marker of diverse psychopathologies: A review and argument for an “ideal range”. Neurosci. Biobehav. Rev. 121, 144–155 (2021).
Appelhans, B. M. & Luecken, L. J. Heart rate variability as an index of regulated emotional responding. Rev. Gen. Psychol. 10, 229–240 (2006).
Porges, S. W. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology 32, 301–318 (1995).
Thayer, J. F. & Lane, R. D. A model of neurovisceral integration in emotion regulation and dysregulation. J. Affect. Disord. 61, 201–216 (2000).
Krypotos, A.-M., Jahfari, S., van Ast, V. A., Kindt, M. & Forstmann, B. U. Individual differences in heart rate variability predict the degree of slowing during response inhibition and initiation in the presence of emotional stimuli. Front. Psychol. 2, 278 (2011).
Thayer, J. F., Ahs, F., Fredrikson, M., Sollers, J. J. 3rd. & Wager, T. D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 36, 747–756 (2012).
Benarroch, E. E. The central autonomic network: Functional organization, dysfunction, and perspective. Mayo Clin. Proc. 68, 988–1001 (1993).
McEwen, B. S. & Gianaros, P. J. Stress- and allostasis-induced brain plasticity. Annu. Rev. Med. 62, 431–445 (2011).
McEwen, B. S. Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 840, 33–44 (1998).
Bester, M. et al. Characterizing the effect of demographics, cardiorespiratory factors, and inter-subject variation on maternal heart rate variability in pregnancy with statistical modeling: A retrospective observational analysis. Sci. Rep. 12, 19305 (2022).
Kimmel, M. C. et al. Heart rate variability in late pregnancy: Exploration of distinctive patterns in relation to maternal mental health. Transl. Psychiatry 11, 286 (2021).
Garg, P. et al. Sequential analysis of heart rate variability, blood pressure variability and baroreflex sensitivity in healthy pregnancy. Clin. Auton. Res. 30, 433–439 (2020).
Eneroth-Grimfors, E., Westgren, M., Ericson, M., Ihrman-Sandahl, C. & Lindblad, L. E. Autonomic cardiovascular control in normal and pre-eclamptic pregnancy. Acta Obstet. Gynecol. Scand. 73, 680–684 (1994).
Moors, S. et al. Heart rate variability in hypertensive pregnancy disorders: A systematic review. Pregnancy Hypertens. 20, 56–68 (2020).
Oppenheimer, J. E., Measelle, J. R., Laurent, H. K. & Ablow, J. C. Mothers’ vagal regulation during the still-face paradigm: Normative reactivity and impact of depression symptoms. Infant Behav. Dev. 36, 255–267 (2013).
Smith, C. G. et al. Anxious parents show higher physiological synchrony with their infants. Psychol. Med. 52, 3040–3050 (2022).
Ham, J. & Tronick, E. Infant resilience to the stress of the still-face: Infant and maternal psychophysiology are related. Ann. N. Y. Acad. Sci. 1094, 297–302 (2006).
Gunnar, M. R. & Donzella, B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 27, 199–220 (2002).
Bush, N. R. et al. Effects of pre- and postnatal maternal stress on infant temperament and autonomic nervous system reactivity and regulation in a diverse, low-income population. Dev. Psychopathol. 29, 1553–1571 (2017).
Feldman, R. Sensitive periods in human social development: New insights from research on oxytocin, synchrony, and high-risk parenting. Dev. Psychopathol. 27, 369–395 (2015).
Braren, S. H. et al. Maternal psychological stress moderates diurnal cortisol linkage in expectant fathers and mothers during late pregnancy. Psychoneuroendocrinology 111, 104474 (2020).
Blair, C. & Raver, C. C. Individual development and evolution: Experiential canalization of self-regulation. Dev. Psychol. 48, 647–657 (2012).
Ham, J. & Tronick, E. Relational psychophysiology: Lessons from mother-infant physiology research on dyadically expanded states of consciousness. Psychother. Res. 19, 619–632 (2009).
Wass, S. V. et al. Parents mimic and influence their infant’s autonomic state through dynamic affective state matching. Curr. Biol. 29, 2415-2422.e4 (2019).
Calkins, S. D., Perry, N. B. & Dollar, J. M. A biopsychosocial model of self-regulation in infancy. In Child Psychology: A Handbook of Contemporary Issues: Third Edition 3–20 (Taylor and Francis Inc., 2016).
Feldman, R. The neurobiology of mammalian parenting and the biosocial context of human caregiving. Horm. Behav. 77, 3–17 (2016).
Nazzari, S., Fearon, P., Rice, F., Molteni, M. & Frigerio, A. Maternal caregiving moderates the impact of antenatal maternal cortisol on infant stress regulation. J. Child Psychol. Psychiatry 63, 871–880 (2022).
Gunnar, M. R. Social regulation of stress in early child development. In Blackwell Handbook of Early Childhood Development vol. 663, 106–125 (2006).
Calkins, S. D. Caregiving as coregulation: Psychobiological processes and child functioning. In Biosocial Foundations of Family Processes (eds Booth, A. et al.) 49–59 (Springer New York, 2011).
Tronick, E., Mueller, I., DiCorcia, J., Hunter, R. & Snidman, N. A caretaker acute stress paradigm: Effects on behavior and physiology of caretaker and infant. Dev. Psychobiol. 63, 237–246 (2021).
Gabard-Durnam, L. & McLaughlin, K. A. Sensitive periods in human development: Charting a course for the future. Curr. Opin. Behav. Sci. 36, 120–128 (2020).
Hensch, T. K. Critical period plasticity in local cortical circuits. Nat. Rev. Neurosci. 6, 877–888 (2005).
Suga, A., Uraguchi, M., Tange, A., Ishikawa, H. & Ohira, H. Cardiac interaction between mother and infant: enhancement of heart rate variability. Sci. Rep. 9, 20019 (2019).
DePasquale, C. E. A systematic review of caregiver-child physiological synchrony across systems: Associations with behavior and child functioning. Dev. Psychopathol. 32, 1754–1777 (2020).
Chen, J., Xiao, Y., Xu, B. & Zhang, D. The developmental trajectory of task-related frontal EEG theta/beta ratio in childhood. Dev. Cogn. Neurosci. 60, 101233 (2023).
Anderson, A. J. & Perone, S. Developmental change in the resting state electroencephalogram: Insights into cognition and the brain. Brain Cogn. 126, 40–52 (2018).
Begum-Ali, J. et al. Altered theta-beta ratio in infancy associates with family history of ADHD and later ADHD-relevant temperamental traits. J. Child Psychol. Psychiatry 63, 1057–1067 (2022).
Troller-Renfree, S. V. et al. Associations between maternal stress and infant resting brain activity among families residing in poverty in the U.S. Biol. Psychol. 108683 (2023).
Brandes-Aitken, A., Pini, N., Weatherhead, M. & Brito, N. H. Maternal hair cortisol predicts periodic and aperiodic infant frontal EEG activity longitudinally across infancy. Dev. Psychobiol. 65, e22393 (2023).
Goldstein, B. L. et al. Positive and negative emotionality at age 3 predicts change in frontal EEG asymmetry across early childhood. J. Abnorm. Child Psychol. 47, 209–219 (2019).
Smith, C. L., Diaz, A., Day, K. L. & Bell, M. A. Infant frontal electroencephalogram asymmetry and negative emotional reactivity as predictors of toddlerhood effortful control. J. Exp. Child Psychol. 142, 262–273 (2016).
Gartstein, M. A., Hancock, G. R., Potapova, N. V., Calkins, S. D. & Bell, M. A. Modeling development of frontal electroencephalogram (EEG) asymmetry: Sex differences and links with temperament. Dev. Sci. 23, e12891 (2020).
Hill, K. E. et al. Intergenerational transmission of frontal alpha asymmetry among mother-infant dyads. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 5, 420–428 (2020).
Brooker, R. J., Canen, M. J., Davidson, R. J. & Hill Goldsmith, H. Short- and long-term stability of alpha asymmetry in infants: Baseline and affective measures. Psychophysiology 54, 1100–1109 (2017).
Mulligan, D. J., Palopoli, A. C., van den Heuvel, M. I., Thomason, M. E. & Trentacosta, C. J. Frontal alpha asymmetry in response to stressor moderates the relation between parenting hassles and child externalizing problems. Front. Neurosci. 16, 917300 (2022).
Young, H. & Benton, D. We should be using nonlinear indices when relating heart-rate dynamics to cognition and mood. Sci. Rep. 5, 16619 (2015).
Abney, D. H., daSilva, E. B., Lewis, G. F. & Bertenthal, B. I. A method for measuring dynamic respiratory sinus arrhythmia (RSA) in infants and mothers. Infant Behav. Dev. 63, 101569 (2021).
Pierce, L. J. et al. Association of perceived maternal stress during the perinatal period with electroencephalography patterns in 2-month-old infants. JAMA Pediatr. 173, 561–570 (2019).
Brandes-Aitken, A. et al. Within-person changes in basal cortisol and caregiving modulate executive attention across infancy. Dev. Psychopathol. 1–14 (2021).
Hane, A. A. & Fox, N. A. Ordinary variations in maternal caregiving influence human infants’ stress reactivity. Psychol. Sci. 17, 550–556 (2006).
Friedman, B. H. & Thayer, J. F. Autonomic balance revisited: Panic anxiety and heart rate variability. J. Psychosom. Res. 44, 133–151 (1998).
Miller, J. G. et al. Heart rate variability moderates the effects of COVID-19-related stress and family adversity on emotional problems in adolescents: Testing models of differential susceptibility and diathesis stress. Dev. Psychopathol. 34, 1–12 (2021).
Schiweck, C., Piette, D., Berckmans, D., Claes, S. & Vrieze, E. Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychol. Med. 49, 200–211 (2019).
Kogler, L. et al. Psychosocial versus physiological stress—Meta-analyses on deactivations and activations of the neural correlates of stress reactions. Neuroimage 119, 235–251 (2015).
Agorastos, A. et al. Vagal effects of endocrine HPA axis challenges on resting autonomic activity assessed by heart rate variability measures in healthy humans. Psychoneuroendocrinology 102, 196–203 (2019).
McCraty, R. & Shaffer, F. Heart rate variability: New perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Glob. Adv. Health Med. 4, 46–61 (2015).
Calkins, S. D. & Hill, A. Caregiver influences on emerging emotion regulation. In Handbook of Emotion Regulation vol. 229248, 229–248 (2007).
Gunnar, M. R. & Cheatham, C. L. Brain and behavior interface: Stress and the developing brain. Infant Ment. Health J. 24, 195–211 (2003).
Blair, C. Stress and the development of executive functions. In 37th Minnesota Symposium on Child Psychology: Developing Cognitive Control Processes: Mechanisms, Implications, and Interventions 145–180 (Wiley Online Library, 2014).
St John, A. M., Kao, K., Liederman, J., Grieve, P. G. & Tarullo, A. R. Maternal cortisol slope at 6 months predicts infant cortisol slope and EEG power at 12 months. Dev. Psychobiol. 59, 787–801 (2017).
Troller-Renfree, S. V. et al. Infants of mothers with higher physiological stress show alterations in brain function. Dev. Sci. e12976 (2020).
Abney, D. H., daSilva, E. B. & Bertenthal, B. I. Associations between infant-mother physiological synchrony and 4- and 6-month-old infants’ emotion regulation. Dev. Psychobiol. 63, e22161 (2021).
Busuito, A., Quigley, K. M., Moore, G. A., Voegtline, K. M. & DiPietro, J. A. In sync: Physiological correlates of behavioral synchrony in infants and mothers. Dev. Psychol. 55, 1034–1045 (2019).
Lunkenheimer, E., Brown, K. M. & Fuchs, A. Differences in mother-child and father-child RSA synchrony: Moderation by child self-regulation and dyadic affect. Dev. Psychobiol. 63, 1210–1224 (2021).
McFarland, D. H., Fortin, A. J. & Polka, L. Physiological measures of mother-infant interactional synchrony. Dev. Psychobiol. 62, 50–61 (2020).
Somers, J. A., Luecken, L. J., McNeish, D., Lemery-Chalfant, K. & Spinrad, T. L. Second-by-second infant and mother emotion regulation and coregulation processes. Dev. Psychopathol. 1–14 (2021).
Carozza, S. & Leong, V. The role of affectionate caregiver touch in early neurodevelopment and parent–infant interactional synchrony. Front. Neurosci. 14 (2021).
Feldman, R., Singer, M. & Zagoory, O. Touch attenuates infants’ physiological reactivity to stress. Dev. Sci. 13, 271–278 (2010).
Feldman, R. Parent?infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J. Child Psychol. Psychiat. 48, 329–354 (2007).
Fox, N. A. & Reeb, B. C. Cortical Asymmetry. In Handbook of Approach and Avoidance Motivation 35–49 (Psychology Press, 2013).
Trevarthen, C. Lateral asymmetries in infancy: Implications for the development of the hemispheres. Neurosci. Biobehav. Rev. 20, 571–586 (1996).
Johnson, M. H. Interactive specialization: A domain-general framework for human functional brain development?. Dev. Cogn. Neurosci. 1, 7–21 (2011).
Nguyen, T., Hoehl, S., Bertenthal, B. I. & Abney, D. H. Coupling between prefrontal brain activity and respiratory sinus arrhythmia in infants and adults. Dev. Cogn. Neurosci. 58, 101184 (2022).
Levin, A. R., Méndez Leal, A. S., Gabard-Durnam, L. J. & O’Leary, H. M. BEAPP: The batch electroencephalography automated processing platform. Front. Neurosci. 12, 513 (2018).
Gabard-Durnam, L. J., Mendez Leal, A. S., Wilkinson, C. L. & Levin, A. R. The harvard automated processing pipeline for electroencephalography (HAPPE): Standardized processing software for developmental and high-artifact data. Front. Neurosci. 12, 97 (2018).
Winkler, I., Haufe, S. & Tangermann, M. Automatic classification of artifactual ICA-components for artifact removal in EEG signals. Behav. Brain Funct. 7, 30 (2011).
Saby, J. N. & Marshall, P. J. The utility of EEG band power analysis in the study of infancy and early childhood. Dev. Neuropsychol. 37, 253–273 (2012).
Haegens, S. et al. Beta oscillations in the monkey sensorimotor network reflect somatosensory decision making. Proc. Natl. Acad. Sci. U.S.A. 108, 10708–10713 (2011).
Bell, M. A. & Cuevas, K. Using EEG to study cognitive development: Issues and practices. J. Cogn. Dev. 13, 281–294 (2012).
Law, E. C. et al. Associations between infant screen use, electroencephalography markers, and cognitive outcomes. JAMA Pediatr. 177, 311–318 (2023).
Arns, M., Conners, C. K. & Kraemer, H. C. A decade of EEG theta/beta ratio research in ADHD: A meta-analysis. J. Atten. Disord. 17, 374–383 (2013).
Gasser, T., Bächer, P. & Möcks, J. Transformations towards the normal distribution of broad band spectral parameters of the EEG. Electroencephalogr. Clin. Neurophysiol. 53, 119–124 (1982).
Allen, J. J. B., Chambers, A. S. & Towers, D. N. The many metrics of cardiac chronotropy: A pragmatic primer and a brief comparison of metrics. Biol. Psychol. 74, 243–262 (2007).
Pham, T., Lau, Z. J., Chen, S. H. A. & Makowski, D. Heart rate variability in psychology: A review of HRV indices and an analysis tutorial. Sensors 21 (2021).
Gomes, P., Margaritoff, P. & Silva, H. pyHRV: Development and evaluation of an open-source python toolbox for heart rate variability (HRV). In Proceedings of International Conference Electrical, Electronic and Computing Engineering (2019).
Camm, A. J. et al. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task force of the european society of cardiology and the north american society of pacing and electrophysiology. Circulation 93, 1043–1065 (1996).
Shaffer, F. & Ginsberg, J. P. An overview of heart rate variability metrics and norms. Front. Public Health 5, 258 (2017).
Quintana, D. S., Alvares, G. A. & Heathers, J. A. J. Guidelines for reporting articles on psychiatry and heart rate variability (GRAPH): Recommendations to advance research communication. Transl. Psychiatry 6, e803 (2016).
Wallis, L. A., Healy, M., Undy, M. B. & Maconochie, I. Age related reference ranges for respiration rate and heart rate from 4 to 16 years. Arch. Dis. Child. 90, 1117–1121 (2005).
Voss, A., Schulz, S., Schroeder, R., Baumert, M. & Caminal, P. Methods derived from nonlinear dynamics for analysing heart rate variability. Philos. Trans. A Math. Phys. Eng. Sci. 367, 277–296 (2009).
Peng, C. K., Havlin, S., Stanley, H. E. & Goldberger, A. L. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5, 82–87 (1995).
Rosseel, Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 48, 1–36 (2012).
Oshri, A., Liu, S., Suveg, C. M., Caughy, M. O. & Goodgame Huffman, L. Biological sensitivity to context as a dyadic construct: An investigation of child-parent RSA synchrony among low-SES youth. Dev. Psychopathol. 35, 95–108 (2023).
Bar-Haim, Y., Marshall, P. J. & Fox, N. A. Developmental changes in heart period and high-frequency heart period variability from 4 months to 4 years of age. Dev. Psychobiol. 37, 44–56 (2000).
Feldman, R., Magori-Cohen, R., Galili, G., Singer, M. & Louzoun, Y. Mother and infant coordinate heart rhythms through episodes of interaction synchrony. Infant Behav. Dev. 34, 569–577 (2011).
Trapletti, A., Hornik, K., LeBaron, B. & Hornik, M. K. Package ‘tseries.’ R project (2015).
Laborde, S., Mosley, E. & Thayer, J. F. Heart rate variability and cardiac vagal tone in psychophysiological research—Recommendations for experiment planning, data analysis, and data reporting. Front. Psychol. 8, 1–18 (2017).
Aiken, L. S., West, S. G. & Reno, R. R. Multiple Regression: Testing and Interpreting Interactions (SAGE, 1991).
Shrout, P. E. & Bolger, N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol. Methods 7, 422–445 (2002).
Fox, J. & Weisberg, S. An R Companion to Applied Regression (SAGE Publications, 2018).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. 57, 289–300 (1995).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiat. 150, 782–786 (1987).
Spielberger, C. D. State-Trait Anxiety Inventory for Adults (STAI-AD) [Database record]. APA PsycTests. (1983).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J. health soc. behav. 24(4), 385–396 (1983).
Funding
The funding was provided by NICHD (No. HD086255, HD086255, HD086255, HD086255, HD086255, HD086255).
Author information
Authors and Affiliations
Contributions
ABA, NHB, and DW wrote the main manuscript text NHB directed the study AH and MZ conducted study procedures and provided manuscript edits All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Brandes-Aitken, A., Hume, A., Braren, S. et al. Maternal heart rate variability at 3-months postpartum is associated with maternal mental health and infant neurophysiology. Sci Rep 14, 18766 (2024). https://doi.org/10.1038/s41598-024-68398-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68398-4
- Springer Nature Limited