Abstract
The kidney is a metabolically active organ that requires energy to drive processes such as tubular reabsorption and secretion, and shows a decline in function with advancing age. Various molecular mechanisms, including genomic instability, telomere attrition, inflammation, autophagy, mitochondrial function, and changes to the sirtuin and Klotho signalling pathways, are recognized regulators of individual lifespan and pivotal factors that govern kidney ageing. Thus, mechanisms that contribute to ageing not only dictate renal outcomes but also exert a substantial influence over life expectancy. Conversely, kidney dysfunction, in the context of chronic kidney disease (CKD), precipitates an expedited ageing trajectory in individuals, leading to premature ageing and a disconnect between biological and chronological age. As CKD advances, age-related manifestations such as frailty become increasingly conspicuous. Hence, the pursuit of healthy ageing necessitates not only the management of age-related complications but also a comprehensive understanding of the processes and markers that underlie systemic ageing. Here, we examine the hallmarks of ageing, focusing on the mechanisms by which they affect kidney health and contribute to premature organ ageing. We also review diagnostic methodologies and interventions for premature ageing, with special consideration given to the potential of emerging therapeutic avenues to target age-related kidney diseases.
Key points
-
The kidney is a metabolically active organ that requires energy for processes such as tubular reabsorption and secretion; however, kidney function declines with age.
-
Various molecular mechanisms, including cellular senescence, inflammation, mitochondrial function, changes to the sirtuin and Klotho signalling pathways, and the autophagy–lysosome system, are recognized as regulators of individual lifespan and are important factors that govern kidney ageing.
-
Chronic kidney disease (CKD) and premature ageing share several common features and pathophysiological mechanisms; CKD is therefore considered a disease associated with accelerated or premature ageing.
-
The accelerated ageing phenotype of the kidney in the context of CKD results in a disconnect between the biological age of the kidney and the chronological age of the individual, known as the ‘age gap’.
-
Emerging technologies and biomarkers hold promise for improving the early detection, diagnosis and management of age-related kidney diseases and premature ageing.
-
Targeting the pathways associated with inflammation, mitochondrial function, oxidative stress, senescence and the autophagy–lysosome system holds promise for developing therapeutic interventions to prevent, delay or attenuate age-related kidney diseases and promote healthy ageing.
Similar content being viewed by others
Introduction
Human life expectancy has increased consistently due to advances in health care. The prevalence of age-related conditions and the average age of patients receiving medical care has risen concurrently — a trend that is particularly conspicuous in nephrology. Multiple studies have shown that the ageing process markedly amplifies the risk of acute kidney injury (AKI) and chronic kidney disease (CKD), thereby imposing substantial burdens on society and the economy1,2,3. This heightened risk is clinically relevant, and implies a predisposition to unfavourable renal outcomes with age; however, the precise mechanisms underlying kidney dysfunction in older individuals remain unknown.
Over a decade ago, researchers described nine hallmarks of ageing, including: genomic instability, telomere attrition, epigenetic modifications, disruption of proteostasis, dysregulated nutrient sensing, cellular senescence, stem cell exhaustion, altered intracellular communication and mitochondrial dysfunction4. More recently, the hallmarks of ageing were updated to include disabled macroautophagy (hereafter referred to as autophagy), chronic inflammation and dysbiosis5. These hallmarks represent key biological processes that underlie the ageing process and are often implicated in age-related diseases, including CKD. Although not all hallmarks may directly contribute to every aspect of CKD, several connections exist between these hallmarks and the development of kidney disease with age. For example, mitochondrial dysfunction and chronic inflammation are well-recognized hallmarks of kidney ageing. Autophagy, which maintains intracellular homeostasis by degrading cellular components in lysosomes6, exerts a protective effect against various kidney pathologies7,8. Emerging evidence indicates that autophagic activity declines with age and that upregulation of autophagy delays the ageing process9,10.
Conversely, ageing of the kidney in itself accelerates systemic ageing11. New findings have revealed that CKD is an important risk factor for the progressive ageing of other organ systems, such as the brain and heart12. These findings highlight the need to separately consider biological and chronological age, and underscore the potential systemic benefits that might be achieved through the use of interventions that target kidney ageing.
These insights highlight the need to comprehensively understand the underlying pathological mechanisms and the intricate interplay between ageing and kidney diseases. In this Review, we describe hallmarks of ageing that are relevant to age-related kidney diseases, and the pathological mechanisms of CKD in the context of premature ageing. Finally, we explore diagnostic approaches and effective interventions for premature ageing, focusing on the potential to target the hallmarks of ageing to promote healthy ageing and prevent age-related kidney diseases.
Pathological drivers of kidney ageing
Kidney ageing is a complex process characterized by structural and functional changes that occur with advancing age13. The ageing process is associated with a gradual loss of nephrons, leading to reduced renal mass. A progressive decline in renal blood flow and vascular function is associated with alterations in the structure and function of the renal microvasculature. These alterations are highly age-dependent and affect the development and progression of kidney disease. Consequently, older age is an important risk factor for CKD1,14,15.
Within the glomerulus, ageing is associated with thickening of the glomerular basement membrane (GBM) and expansion of the mesangial compartment, which leads to glomerular enlargement and hyperfiltration. These changes, coupled with an accumulation of extracellular matrix contribute to progressive glomerulosclerosis16, which can lead to a subsequent decline in glomerular filtration rate (GFR)17. Age-related changes in the glomerular vasculature, particularly in juxtamedullary glomeruli, can result in the formation of an arteriovenous shunt between afferent and efferent arterioles, which may impair osmotic gradient formation and reduce the urine-concentrating ability of the kidney18.
To compensate for reduced GFR, glomeruli undergo further hypertrophy. However, studies in mice have shown that the number and density of podocytes — which act to maintain and support the GBM — decrease with age16. The density of parietal epithelial cells (PECs) also decreases in aged mice; however, the proportion of CD44-positive, activated PECs is increased in aged kidneys. These activated PECs colocalize to phosphorylated ERK and are associated with elevated extracellular matrix proteins, suggesting PEC transformation via epithelial-to-mesenchymal transition. These findings suggest that ageing induces important alterations in PECs, reducing their regenerative capacity and inducing characteristics of pericytes and mesenchymal fibroblasts, which may contribute to glomerulosclerosis16.
Chronic hypoxia is another important factor that can contribute to kidney injury and influences several pathogenic pathways that can lead to kidney failure19,20. The complex microvasculature and high oxygen demands of the kidneys renders them particularly susceptible to hypoxic injury. With ageing, rarefaction of peritubular capillaries, increased oxygen demand by proximal tubule epithelial cells (PTECs) and anaemia can aggravate hypoxia, in turn exacerbating the risk of kidney injury19,20.
Hypoxia triggers adaptive responses in the kidney, including the activation of hypoxia-inducible factors (HIFs), which regulate genes involved in angiogenesis, erythropoiesis, metabolism and cell survival. These adaptive responses might initially be protective, but hypoxia-induced expression of HIF1α in the aged kidney can lead to maladaptive changes and exacerbate CKD progression via the induction of oxidative stress, tubulointerstitial injury and inflammation20,21. Conversely, the NAD-dependent histone deacetylase, sirtuin 1 (SIRT1), can mediate a range of cellular responses, some of which are achieved through the deacetylation of lysine residues on HIF1α21,22,23. Decreased expression of SIRT1 in the kidneys of aged mice is associated with a decrease in stress-induced autophagy in response to hypoxia22,24. SIRT1 also activates the transcription factor FOXO3a via its deacetylase activity, which induces the transcription of Bnip3 — a gene involved in mitophagy25. In aged mice, decreased SIRT1 mRNA and protein expression in the kidney is associated with an accumulation of abnormal mitochondria24. SIRT1 also seems to be important for podocyte morphology and function. Podocyte-specific deletion of Sirt1 in mice exacerbates age-related glomerulosclerosis and albuminuria, which is accompanied by increased oxidative stress and impaired podocyte maturation26.
Kidney fibrosis is another important and common manifestation of progressive kidney diseases. Studies from the past few years have identified reductions in basement membrane components, such as laminins, type IV collagen and type XVIII collagen, and increases in interstitial matrix proteins such as collagens I, III, VI and XV, fibrinogens, and nephronectin as a common signature in kidney ageing and disease27. Transforming growth factor-β (TGFβ) has an important role in the pathogenesis of fibrosis by upregulating matrix protein synthesis, inhibiting matrix degradation, and altering cell–cell interactions28, although therapeutic targeting of TGFβ has met with limited success.
Hallmarks of kidney ageing
Growing evidence supports the notion that the above-described pathological drivers of kidney ageing interact bidirectionally with several of the so-called hallmarks of ageing (Fig. 1).
Several hallmarks of ageing have been linked to pathogenic processes underlying the development of kidney disease. These hallmarks, along with other processes, lead to manifestations that commonly present in patients with chronic kidney disease, including glomerulosclerosis, tubulointerstitial injury and fibrosis, and can therefore be considered hallmarks of kidney ageing.
Primary hallmarks and cellular senescence
Genomic instability, telomere attrition and epigenetic alterations
Genomic instability, telomere attrition and epigenetic alterations are categorized as ‘primary’ hallmarks of ageing, defined as hallmarks that progressively accumulate with time and unambiguously contribute to the ageing process5. Genomic instability is associated with an increased risk of DNA damage and mutations over time, resulting in an accumulation of genomic damage with ageing29. DNA damage can trigger inflammatory responses and cell death pathways in the kidneys, contributing to CKD progression30. In men, age-related mosaic loss of the Y chromosome (mLOY) is associated with various pathologies. Use of single-cell RNA and assay for transposase-accessible chromatin (ATAC) sequencing in human kidneys revealed that mLOY varies by nephron location, with PTECs being most affected31. As described above, PTECs are particularly vulnerable to hypoxic injury, which can trigger cell dedifferentiation and may render them particularly susceptible to mLOY31.
Telomeres are protective caps at the ends of chromosomes that shorten with each cell division. Telomere shortening can trigger cellular senescence. It has been observed in aged kidneys and is associated with various degenerative and age-related diseases, including CKD32,33. Notably, telomere shortening is linked to inflammation, low fetuin-A levels and high mortality in patients undergoing prevalent haemodialysis34. Dysregulation of epigenetic mechanisms has also been implicated in the development and progression of CKD. For instance, altered DNA methylation patterns have been observed in kidney cells from individuals with CKD, which affect the expression of genes involved in kidney function and fibrosis35.
Cellular senescence
Cellular senescence refers to a state of irreversible cell cycle arrest that can arise in response to various stressors including DNA damage and telomere shortening. It is categorized as an ‘antagonistic’ hallmark of ageing, which means that it reflects responses to damage and has a more nuanced role in the ageing process. Cellular senescence increases with age36, and has been implicated in kidney ageing37,38,39, in part through the release of pro-inflammatory cytokines and the propagation of inflammation via the manifestation of a senescence-associated secretory phenotype (SASP). Ageing-associated impairment of immune function may allow senescent cells to escape immune clearance. In a model of chronic ischaemia, maladaptive tubular cell senescence, characterized by the upregulation of p16, p19 and p21 expression, was associated with kidney dysfunction and injury40. Podocyte senescence also has a central role in kidney ageing. For example, podocyte-specific deletion of CAAT enhancer-binding protein-α (C/EBPα) in aged mice exacerbates podocyte senescence, leading to glomerulosclerosis. Moreover, the ensuing albuminuria induces PTEC senescence41. A 2022 study also found that age-related overexpression and hyperactivation of glycogen synthase kinase 3 (GSK3β) drives podocyte senescence by inducing mediators of senescence signalling, such as p16 and p53 (ref. 42). Another study revealed a key role for the immune checkpoint protein, PD1, in podocyte ageing and in SASP induction. Overexpression of PD1 in the podocytes of aged mice correlated with reduced GFR and with increased glomerulosclerosis and in the vascular arterial intima-to-lumen ratio. Blocking of PD1 signalling with a neutralizing anti-PD1 antibody reduced podocyte senescence and inflammatory signalling and was associated with increased podocyte lifespan43. These studies highlight the importance of senescent podocytes and PTECs as potential targets in kidney ageing.
The removal of senescent cells through senolysis may ameliorate age-related pathologies36,39,44. Indeed, studies in transgenic mouse models show that the removal of senescent cells can prevent or delay tissue dysfunction and extend healthspan45,46. Targeted elimination of senescent cells by small-molecule senolytic drugs, by disrupting key senescent events through the administration of senomorphic agents, or through the inhibition of processes that promote the accumulation of senescent cells, might therefore represent promising therapeutic strategies for preventing or treating age-related diseases36,47,48. For example, inhibition of glutaminolysis may represent one approach to target senescent cells. Glutaminase is induced in response to a reduction in the pH of senescent cells following damage to lysosomal membranes. The resulting glutaminolysis induces ammonia production, which neutralizes the pH and aids the survival of senescent cells. By contrast, inhibition of glutaminolysis in aged mice specifically eliminated senescent cells and ameliorated age-related dysfunction and fibrosis of the kidney49.
Inflammaging
Chronic low-grade inflammation is considered to be an integrative hallmark of ageing, defined as a feature that arises when the accumulated damage inflicted by the primary and antagonistic hallmarks can no longer be compensated for. Ageing affects the composition and function of the immune system, leading to immunosenescence, which is characterized by defective immune responses and increased systemic inflammation (also known as inflammaging)50. This maladaptive phenomenon results from various mechanisms, including aberrant inflammasome activation, microbial dysbiosis, the accumulation of senescent cells and primary dysregulation of immune cells51,52.
Various mediators promote chronic inflammation in CKD, including oxidative stress and the adoption of a pro-inflammatory phenotype by resident kidney cells. The regulation of pro-inflammatory and anti-inflammatory mediators through gene transcription mediated by NF-κB and nuclear factor erythroid 2-like 2 (NRF2), respectively, also has a critical role in the glomerular and tubular cell response to kidney injury53. NRF2 protects against AKI and progression to CKD54,55, and decreased NRF2 expression in aged kidneys may in part underlie the susceptibility of aged kidneys to injury and incomplete recovery after ischaemia–reperfusion injury56. Interestingly, one study that integrated GFR-associated loci with transcriptional data developed a molecular map of CKD, which revealed that all pathways aggregated into two main clusters that comprised inflammation-related and metabolism-related pathways, with the NRF2-mediated oxidative stress response pathway serving as a hub between the two clusters57.
Inflammasome activation is another pivotal mechanism that contributes to inflammaging. Nod-like receptor 3 (NLRP3) can be activated by many danger signals, including reactive oxygen species (ROS), cathepsin released from destabilized lysosomes and aggregated proteins, all of which evoke cellular stress and are involved in the ageing process58. Chronic activation of the NLRP3 inflammasome induces the persistent production of pro-inflammatory cytokines such as IL-1β and IL-18, creating a feedback loop of inflammation and tissue damage that accelerates the ageing process59. Transcriptomic analyses have revealed that the podocytes of aged mice demonstrate an inflammatory phenotype, characterized by increased levels of the NLRP3 inflammasome, IL-6, TNF and IFNγ. NLRP3 signalling in podocytes is further increased in aged mice following the experimental induction of focal segmental glomerulosclerosis. In human glomeruli, higher expression of NLRP3 is associated with reduced podocyte density, increased glomerular volume and total glomerulosclerosis60.
Tertiary lymphoid tissues (TLTs) have also received attention for their role in the pathophysiological response to ageing52. The formation of TLTs within the kidneys of aged mouse models of AKI prolongs inflammation and impedes repair processes, thereby exacerbating kidney injury61. TLTs in non-lymphoid organs act as inflammatory niches to initiate acquired immunity, involving the activation and proliferation of T cells and B cells. Of note, ageing-induced TLTs have been observed in the bladder and liver, as well as in the kidney, suggesting that TLT formation is a systemic effect of ageing62,63. In the kidneys, TLTs tend to form beneath the renal capsule, around blood vessels and adjacent to glomeruli64. Estimates suggest that they are present in approximately half of kidneys from older people, and that they mature through three stages, with more advanced TLT stages forming in the presence of underlying kidney inflammation or injury65. The immunosuppressive drug, dexamethasone, has demonstrated efficacy in preventing and reducing the formation of TLTs in the mouse kidney61,65, although it is associated with adverse effects and is not specific to TLTs. The expansion of TLTs relies on CD153–CD30 signalling between senescence-associated T cells and age-associated B cells, which emerge with ageing. Blocking this signal suppressed TLT formation and improved kidney function in aged kidney injury models66. TLTs have also been linked to pathological conditions independent of ageing. Analyses of protocol kidney biopsy samples after transplantation revealed the presence of TLTs in about 50% of kidneys after 1 month; stage II TLTs (that is, the stage at which follicular dendritic cells develop) were present in approximately 20% of kidneys after 1 year, and their presence correlated with poorer renal outcomes 5 years after transplantation67. TLT formation has also been reported in patients with various kidney diseases, including IgA nephropathy and ANCA-associated vasculitis, suggesting potential as a disease-agnostic prognostic indicator and therapeutic target52. Further findings indicate that TLTs confer an inflammatory phenotype on PTECs and renal fibroblasts to impair repair capacity; conversely, inflammatory parenchymal cells facilitate leukocyte trafficking and survival and thereby contribute to TLT expansion68.
Mitochondrial dysfunction and oxidative stress
Mitochondria are the cellular powerhouses that are responsible for producing energy in the form of ATP, which is critical for the reabsorptive capacity of the proximal tubule. The citric acid cycle in the mitochondrial matrix generates ATP by consuming acetyl-CoA and water, reducing NAD+ to NADH, and releasing carbon dioxide and water. In the aged kidney, low NAD levels and NAD-dependent mitochondrial sirtuin activity are associated with impaired mitochondrial respiration, energy deficiency and ROS accumulation69. An NAD+ precursor, nicotinamide mononucleotide, rescued age-related susceptibility to AKI in a SIRT1-dependent manner in mice70.
Mitochondrial dysfunction, characterized by impaired oxidative phosphorylation and increased production of ROS, is considered to be an antagonistic hallmark of ageing, and has been observed in aged kidneys and in various kidney diseases71,72. Mitochondrial dysfunction can compromise the utilization of cellular oxygen and exacerbate tissue hypoxia in the aged kidney, leading to increased oxidative stress. Increased oxidative stress, characterized by an imbalance between ROS production and antioxidant defence mechanisms, can trigger cell death through apoptosis and ferroptosis. These effects, in turn, induce the release of inflammatory cytokines and contribute to kidney ageing and CKD pathogenesis69,73,74.
Fibroblast growth factor 21 (FGF21) is a hormone-like member of the FGF family that controls metabolic multiorgan crosstalk by enhancing energy expenditure. It acts as a stress hormone induced by endoplasmic reticulum (ER) stress and mitochondrial dysfunction in several tissues75. Studies from the past decade have revealed that FGF21 counteracts kidney disease progression during ageing and obesity by maintaining mitochondrial homeostasis and decreasing oxidative damage in mice71,76.
Defective lipid metabolism
Although the kidney comprises only 0.5% of the total body weight, it uses approximately 10% of the oxygen consumed by the body. Mitochondrial β-oxidation of non-esterified free fatty acids represents a major source of renal ATP, particularly in PTECs, which have a particularly high energy demand and relatively little glycolytic capacity77,78,79,80,81,82. Although not strictly considered a hallmark of ageing, emerging evidence suggests that lipids have crucial roles in regulating ageing and longevity, and that lipid metabolic enzymes undergo substantial changes during ageing83. Omics studies have identified alterations in lipid metabolism, including defective fatty acid oxidation (FAO) by PTECs, in aged mouse kidneys84. Importantly, defective FAO and the intracellular deposition of lipids in PTECs has been linked to the development of fibrosis in mouse and human kidneys85. Multiple studies have now highlighted the contributory role of defective lipid metabolism, particularly dysregulated fatty acid metabolism, in CKD progression69,82.
Several transcription factors, including ESRRα86 and PPARα87, as well as the transcriptional coactivator PGC1α88, regulate FAO in PTECs. Reduced expression of ESRRα, PPARα and PGC1α has been observed in both AKI and CKD in mouse and human kidneys, associated with impaired FAO, reduced ATP levels, an accumulation of lipids and loss of PTEC integrity25,69.
Klotho, phosphate toxicity and calciprotein particles
Klotho is expressed in the kidney, especially in the distal tubule, and functions as the coreceptor for FGF23, a bone-derived hormone that induces phosphate excretion into urine. Klotho deficiency leads to premature ageing and shortened life expectancy in mice; mice lacking Klotho also develop complications similar to those in patients with kidney failure, including atherosclerosis, ectopic calcification, osteoporosis, skin atrophy and gonadal dysfunction. These effects are mitigated by a low phosphate diet, indicating that they are caused by phosphate overload. Furthermore, expression of the gene that encodes Klotho decreases with CKD progression89,90. In addition, Klotho mitigates the progression of AKI to CKD in mice through the activation of autophagy91, and dysregulation of lipid homeostasis induced by Klotho deficiency promotes AKI to CKD transition92. Therefore, a decline in systemic and renal Klotho levels may be considered a novel hallmark of kidney ageing, although it should be noted that Klotho was not associated with clinical outcomes in a large, diverse, well-characterized cohort of patients with CKD. Moreover, Klotho deficiency did not confound the association of FGF23 with mortality or heart failure hospitalization in that study93.
Hyperphosphataemia contributes to the pathophysiology of CKD; it is also independently implicated in cardiovascular and all-cause mortality in patients with CKD, attributed to endothelial dysfunction and vascular calcification11,94,95. Inorganic phosphate activates the AKT–mTOR pathway and shortens the lifespan of Klotho-deficient mice96. Phosphate may also accelerate kidney ageing in humans97. Although the adverse effects of phosphate over-consumption are largely overlooked, contemporary dietary habits often involve the consumption of phosphate-rich foods such as red meat and dairy products, along with the widespread use of phosphate-containing food additives in processed foods98,99,100.
Mechanistically, dietary phosphate induces an increase in circulating FGF23, which acts on the Klotho receptor in kidney tubules to inhibit phosphate reabsorption and thereby increase urinary phosphate excretion98. If the concentration of phosphate in the tubule fluid surpasses its solubility threshold, it forms calcium phosphate precipitates, ultimately forming colloidal particles known as calciprotein particles (CPPs). These CPPs can cause direct injury to PTECs and induce inflammation through the binding and activation of Toll-like receptors98. The decline in nephron numbers with age or injury places a greater phosphate burden on each remaining nephron, leading to further elevations in FGF23 levels and thereby perpetuating a vicious cycle98. We have shown that autophagy in PTECs acts as a mechanism to protect the kidney from phosphate overload-induced injury in mice94.
Magnesium is an essential ion that regulates numerous physiological and pathological processes. Magnesium deficiency is very common in old age101, and hypomagnesaemia predicts mortality and CKD progression in individuals with diabetic kidney disease (DKD)102. In a cross-sectional study that compared the prevalence of electrolyte abnormalities in 5,126 patients with CKD who were not on dialysis, hypomagnesaemia was the most common electrolyte abnormality (14.7%) with similar prevalence across stages of CKD. Proteinuria was a risk factor for hypomagnesaemia — an effect that may be mediated by renal magnesium wasting103.
Emerging data also support an association between the consumption of ultra-processed food and the risk of incident CKD104,105. One potential mechanism for this association may be the toxicity of inorganic phosphate in food additives. Alternatively, the association may be driven by a lower intake of magnesium. Indeed, a population-based cohort study found an association between lower dietary intake of magnesium and decline in kidney function106. The importance of dietary magnesium is recognized particularly in the context of phosphate toxicity. In hemi-nephrectomized mice, a low-magnesium diet exacerbated kidney injury induced by a high-phosphate diet, associated with a marked downregulation of Klotho expression in the kidney107. Dietary magnesium may also inhibit intestinal phosphate absorption108. Moreover, magnesium might prevent phosphate-induced mitochondrial dysfunction by attenuating phosphate-induced mitochondrial permeability transition, cell death and PTEC inflammation109. Additionally, findings in dolphins suggest that CPP-induced kidney injury is attenuated by magnesium110. In a cohort study in patients with CKD, higher serum phosphate levels were associated with an increased risk of kidney failure only when serum magnesium levels were low109. These findings suggest that the hazardous nature of ultra-processed food attributable to phosphate may be amplified by magnesium deficiency.
The consumption of ultra-processed food by patients with CKD may also predispose individuals to, and/or exacerbate, uraemic metabolic derangements, such as insulin resistance, metabolic acidosis, hypertension and gut dysbiosis100. Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite of dietary phosphatidylcholine and carnitine and betaine, which are commonly found in red meat, eggs and certain fish; in experimental models, TMAO caused kidney injury and tubulointerstitial fibrosis111. In a 2024 study of community-based adults in the USA, higher plasma TMAO levels were associated with a higher risk of incident CKD and a greater rate of kidney function decline112. Thus, the role of high phosphate and TMAO in red meat and food additives in processed food may be an underestimated contributor to the kidney ageing process and should be considered in the context of therapeutic interventions.
Dysregulation of autophagy
Defective autophagy has a crucial role in the pathogenesis of age-related diseases by exacerbating tissue damage and impairing the regenerative capacity of organs. Emerging evidence suggests that although basal autophagic activity increases with ageing due to the increased presence of pathological ageing stressors, the capacity of autophagy to upregulate further in response to additional stressors accelerates kidney ageing and may be associated with age-related kidney diseases71 (Fig. 2a).
a, In proximal tubular epithelial cells (PTECs) from young mice, autophagy increases in response to cellular stress as an adaptive mechanism. By contrast, PTECs from aged mice demonstrate higher basal autophagy due to persistent ageing stress. However, the ability of aged cells to increase autophagic activity in response to additional stressors is impeded. The x-axis represents time (hours to days), and the y-axis represents autophagic activity. b, Age-dependent dysregulation of autophagy is induced by lysosomal dysfunction and/or abnormal autophagosome maturation rather than decreased autophagosome biogenesis during kidney ageing. Specifically, increased levels of mTOR in aged kidneys in response to decreases in α-Klotho and AMPK inhibits the induction of autophagy. Downregulation of the glucose-responsive transcription factor, MondoA, with age, leads to increased expression of Rubicon — a negative regulator of autophagosome maturation. Moreover, lysosomal dysfunction in PTECs may also contribute to the age-dependent dysregulation of autophagy. ROS, reactive oxygen species. Adapted with permission from ref. 117, Elsevier.
In the aged kidney, the cumulative effect of autophagy impairment is thought to accelerate the decline in kidney function. This hypothesis is supported by the finding that aged (24-month-old) mice with deficiency of autophagy specifically in PTECs exhibit a significant deterioration in kidney function and fibrosis, concomitant with mitochondrial dysfunction, mitochondrial DNA abnormalities and nuclear DNA damage71. Obese mice fed a high-fat diet (HFD) exhibit similar hallmark features of kidney ageing at 12 months of age, along with evidence of dysfunctional autophagy, supporting the notion that dysregulation of autophagy can accelerate kidney ageing77.
Interestingly, the mitigation of disease progression by Klotho may be partly mediated through the induction of autophagy91. This hypothesis is supported by the finding that dysregulation of autophagy not only promotes CKD but also increases AKI vulnerability71,77,113,114, probably by reducing the ability of kidneys to respond to stressors.
Lysosomal dysfunction
Lysosomes are catabolic organelles that degrade intracellular constituents through autophagy and extracellular components through endocytosis, phagocytosis and macropinocytosis115. Lysosomal functions are tightly regulated by the transcription factors TFEB and TFE3 (ref. 115). The high endocytic activity of the kidney places a high burden on PTEC lysosomes116,117, highlighting their role as central organelles in PTEC homeostasis, in metabolic regulation and in the response to environmental changes, including nutrient stressors, ER stress and defects in proteostasis115. Indeed, lysosomal dysfunction is a common feature of senescent cells49, and giant autolysosomes containing undigested material have been observed in atrophic PTECs76, suggesting that lysosomal dysfunction in PTECs is — at least in part — responsible for the age-dependent dysregulation of autophagy. Moreover, a 2024 study showed that HKDC1, a target of TFEB, prevents cellular senescence by maintaining both mitochondrial and lysosomal homeostasis118.
Lysosomal dysfunction has been linked to a variety of diseases, including autoimmune, metabolic and kidney diseases119. HFD-induced obesity in mice triggers lysosomal dysfunction and defective autophagy, which exacerbates renal lipotoxicity77. Although lipid overload induces autophagy to repair organelle membranes and maintain PTEC integrity, overloading of lysosomes leads to the stagnation of autophagy, which in the context of lipotoxicity manifests as an accumulation of phospholipids in lysosomes120. Interestingly, an accumulation of phospholipids was observed in tubular lysosomes in renal biopsy samples from older patients with CKD and from patients with obesity and CKD77,116,121. The induction of TFEB-mediated lysosomal exocytosis has therefore emerged as a potential approach to alleviate lipotoxicity by expelling accumulated phospholipids121.
Abnormal maturation or biogenesis of the autophagosome
Available evidence suggests that age-dependent dysregulation of autophagy is induced by lysosomal dysfunction and/or abnormal autophagosome maturation rather than decreased autophagosome biogenesis (Fig. 2b). Rubicon is a negative regulator of autophagosome maturation122. Levels of Rubicon increase in the kidney of aged mice; and knockout of Rubicon in aged mice is associated with improved autophagosome maturation and decreased kidney fibrosis123. The glucose-responsive transcription factor, MondoA, directly suppresses Rubicon expression and inhibits cellular senescence, in part by activating autophagy124. Notably, MONDOA expression is downregulated in renal biopsy samples from older individuals and patients with CKD124,125.
Nutrient sensing pathways, such as the AMPK and mTOR pathways, are positive and negative regulators of autophagosome biogenesis, respectively126, and have been implicated in the pathogenesis of CKD127. Levels of AMPK and mTOR are decreased and increased, respectively, in aged kidneys, whereas drug-induced AMPK activation and mTOR inhibition suppress CKD progression in mice117. The oxidative stress response factor, NRF2, also interacts bidirectionally with autophagy processes. Specifically, NRF2 activation enhances autophagy to mitigate oxidative stress and cellular damage, and conversely, the induction of autophagy can promote NRF2 activation128. Dysregulation of NRF2 or autophagy — which commonly occurs in aged kidneys — may disrupt this crosstalk and accelerate kidney ageing71.
CKD and premature ageing
A growing body of literature demonstrates that CKD is an important risk factor for the ageing of other organ systems in humans12,129,130. This link may underlie the association between CKD and frailty in older individuals.
Biological versus chronological age
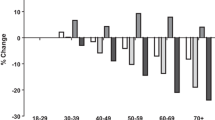
Chronological age alone does not fully capture the complexity of the ageing process in relation to organ function, which is also influenced by a multitude of genetic and environmental factors. Biological age, which reflects the physiological state of an individual, can be accelerated by various lifestyle choices and environmental exposures. These influences can lead to a disconnect between chronological and biological age, known as the ‘age gap’, which serves as a valuable complementary measure in assessments of organ ageing131 (Fig. 3). Consequently, efforts to promote healthy ageing necessitate a deeper understanding of biological age and the molecular mechanisms that influence biological age.
Biological ageing refers to the decline in tissue or organismal function, whereas chronological ageing simply indicates the time passed since birth. In individuals who age ‘normally’, chronological age equates to biological age. The difference between biological age and chronological age is denoted as the ‘age gap’ and serves as a complementary indicator of ageing. Chronic kidney disease accelerates the biological ageing of the kidney and promotes premature ageing via a multiorgan disease network.
The exposome refers to the cumulative impact of environmental exposures throughout an individual’s lifetime, and includes lifestyle factors, diet, pollutants and stressors. These exposures interact with, and modify various physiological processes, affecting various aspects that are relevant to the health of the individual and contributing to the ageing process132. For example, numerous stressors can activate inflammatory responses, disrupt the microbiota balance, induce oxidative stress and impair mitochondrial function, thereby increasing the risk of lifestyle-related diseases that accumulate with age133. Emerging environmental factors such as global warming, deforestation and pollution may exacerbate these effects133.
The role of CKD in the ageing process
CKD is associated with accelerated or premature ageing to the extent that the biological age of patients with CKD is approximately 5 years older than their chronological age. Moreover, and as mentioned previously, CKD is an important risk factor for the progressive ageing of other organ systems such as the brain and heart12 (Fig. 4).
Susceptibility to chronic kidney disease (CKD), acute kidney disease (AKI) and CKD progression is influenced by a variety of pathological mechanisms that overlap with the classic hallmarks of ageing. CKD is associated with a higher biological age — indicative of accelerated or premature ageing — and is a risk factor for the ageing of other organ systems in humans via a multiorgan disease network. This accelerated ageing phenotype manifests as an increased burden of age-related conditions and comorbidities, such as cardiovascular disease (CVD), cognitive impairment and sarcopenia, and is associated with an increased risk of frailty. Frailty and premature ageing in turn may exaggerate the pathologies of kidney ageing and disease. The exposome, defined as the cumulative impact of environmental exposures throughout an individual’s lifetime, may exacerbate this cycle, leading to further deterioration of kidney health and contributing to the overall ageing processes.
The higher biological age of the kidney in patients with CKD relative to chronological age may be mediated by pathophysiological mechanisms that are common to both ageing pathways and CKD11,134. For example, hormonal imbalances, glycative stress and nitrogenous metabolites, as well as the above-described hallmarks of ageing, that contribute to CKD progression, such as inflammation and oxidative stress, contribute to premature ageing in the kidney, but also contribute to the ageing of other systems, particularly the vessels and muscles. This accelerated ageing phenotype manifests as an increased burden of age-related conditions and comorbidities, such as cardiovascular disease, cognitive impairment, sarcopenia and frailty11,134,135. These effects culminate in a high risk of cardiovascular events and sarcopenia, contributing to impaired health status, reduced quality of life and premature mortality in individuals with CKD134,136.
Frailty in patients with CKD
Frailty is a multidimensional concept that encompasses various aspects of health, independence and quality of life, typically in older patients137. It refers to a systemic state of increased vulnerability to stressors due to age-related declines in physiological reserves and functional capacity. Frailty is characterized by diminished strength, endurance, balance and cognitive function, as well as increased susceptibility to adverse health outcomes such as disability, falls, hospitalization and mortality137.
In older patients with CKD, frailty is particularly relevant due to the overlapping risk factors and pathophysiological mechanisms shared between frailty and CKD (Fig. 4). These include chronic inflammation, sarcopenia, protein energy wasting, comorbidities and polypharmacy. Moreover, frailty may exacerbate CKD progression and increase the risk of adverse events138. Collectively, these findings underscore the systemic benefits that can be achieved through interventions targeting kidney ageing and disease.
Diagnostic implications
Current diagnostic methods for kidney diseases involve a combination of clinical evaluation, blood and urine tests, imaging studies, and in some cases, kidney biopsy. A number of emerging technologies and biomarkers hold promise for improving the early detection, diagnosis and management of age-related diseases, including kidney disease131,139,140,141,142.
Emerging technologies and biomarkers
Advances in single-cell transcriptomics have markedly enhanced our understanding of cellular heterogeneity and the molecular processes underlying kidney injury and ageing131,139,141,142. For instance, use of single-cell RNA sequencing (scRNA-seq) facilitated the characterization of a dedifferentiated VCAM1+ population of PTECs and revealed its broad relevance in kidney injury and fibrosis141,143. In addition, scRNA-seq of freshly dissociated cells from healthy and stenotic mouse kidneys enabled the identification of stenotic kidney epithelial cells undergoing both mesenchymal transition and senescence40. Single-nucleus RNA sequencing on aged mouse kidneys with TLTs identified pro-inflammatory and profibrotic VCAM1+ injured PTECs with activation of NF-κB and IFN-inducible transcription factors68. Profiling studies have also led to the identification of biomarkers of ageing, which have the potential to aid the identification of individuals who may be frail and/or at risk of multimorbidity, or to define the most suitable therapeutic targets in a given patient or disease setting. Of note, longitudinal and deep multiomics profiling of 106 healthy individuals aged between 29 and 75 years of age revealed correlations between ‘omics’ measurements, including transcripts, proteins, metabolites, cytokines, microorganisms and clinical laboratory values, and age144. For example, components related to acute-phase response signalling, inflammation such as HMGB1 and Toll-like receptor signalling pathways and the coagulation pathway increased with age. Moreover, the study confirmed the positive association between age and HbA1c level and between age and apolipoprotein A-IV protein (ApoA4) level.
As described above, senescence is considered to be an important cellular mechanism that underlies kidney ageing and susceptibility to injury36. SA-β-Gal, p21 and p16, pro-inflammatory cytokines, and markers of oxidative stress, including malondialdehyde and 8-OHdG, are indicative of cellular senescence74.
Lipidomics technologies have also provided insights into the pathophysiological changes that underlie kidney disease and ageing at the cellular and molecular levels145. For instance, urinary levels of various phospholipids (such as bis(monoacylglycerol)phosphate (BMP) — a lysosomal phospholipid the tissue levels of which are increased in patients with phospholipidosis) are increased in obese mice121. A 2024 study in which untargeted lipidomics was performed on samples from mice of different ages identified a number of molecules from different lipid classes that exhibited common and tissue-specific changes146. For example, levels of BMP containing polyunsaturated fatty acids were increased in the kidney in aged mice146.
A growing body of evidence suggests that mitochondria may represent a promising diagnostic and therapeutic target for age-related kidney diseases. Mitokines are signalling molecules that enable communication of local mitochondrial stress to other mitochondria in distant cells and tissues. Among these molecules are FGF21 and growth differentiation factor 15 (GDF15)147. Interestingly, deficiency of autophagy specifically in the skeletal muscle of mice induced the secretion of FGF21 from skeletal muscle, which protected against diet-induced obesity and insulin resistance148. FGF21 is also robustly induced by disturbances in autophagy in PTECs and protects against CKD progression in mice76. These data imply that FGF21 could act as a compensation mechanism for autophagy stagnation and mitochondrial dysfunction during kidney ageing147.
As described above, CPPs can cause direct injury to PTECs and induce inflammation. We have shown that serum levels of a fetuin-A mineral complex, composed of fetuin-A, fibrinogen, fibronectin 1 and calcium, are correlated with extraosseous calcification stress in patients on haemodialysis149. These findings are supported by those of a more recent study, which showed that circulating levels of CPPs are correlated with inflammation and vascular calcification or stiffness in patients with CKD150. In that study, circulating CPP levels were quantified using a fluorescent probe that bound to calcium phosphate crystals, which may also prove useful for the evaluation of cardiovascular risk in patients with CKD. Another potential tool for the evaluation of cardiovascular risk is skin autofluorescence — a measure of advanced glycation end-products (AGEs) in skin collagen. AGEs can be obtained through dietary sources or produced endogenously, and are associated with oxidative stress and inflammation. Skin autofluorescence could therefore be considered a potential surrogate marker of ageing151,152.
Assessment of premature ageing in older patients with CKD
The susceptibility of the kidney to premature ageing and the association between CKD and age highlights the potential utility of an objective measure of biological (as opposed to chronological) age. An epigenetic ageing clock, based on epigenetic marks at specific genomic loci, may represent one approach to estimate biological age. Interestingly, a 2024 study that estimated biological age based on blood biomarkers, skin autofluorescence and three separate DNA methylation-based epigenetic clocks revealed that kidney transplantation, but not dialysis, partially reduces the acceleration of biological age in patients with advanced CKD153.
Therapeutic implications
Improved understanding of the molecular mechanisms underlying age-related kidney diseases and premature ageing has led to the discovery of novel molecular targets that may decelerate the ageing process and/or protect the kidney from ageing-associated factors154,155. Of note, although anti-ageing drugs hold great potential, their current status is one of promise rather than proven efficacy and safety in the context of human ageing. As research in this field progresses, a strategic, evidence-based approach to their use will be essential. This approach should prioritize high-risk individuals initially, incorporate principles of personalized medicine based on biomarker and genomic insights, and integrate comprehensive and appropriately supported modifications to lifestyle. It will also be important to address ethical, social and public health implications that may arise from the development of anti-ageing drugs to ensure that such therapeutic advances benefit society as a whole.
The long-term safety of anti-ageing drugs is a critical concern. Continuous monitoring of patients will be essential, with regular assessment of biomarkers and health outcomes to adapt treatment plans and ensure ongoing effectiveness and safety.
Approaches to target pathological mechanisms of kidney ageing
A variety of strategies have been investigated to target the pathological mechanisms of ageing, including those that target cellular senescence, inflammatory pathways, mitochondrial dysfunction and the Klotho–phosphate–FGF23 axis134. As described above, targeted elimination of senescent cells through the use of senolytic drugs has been proposed as a therapeutic strategy for preventing or treating age-related diseases. In one study, intermittent oral administration of senolytics to naturally aged mice or to mice transplanted with senescent cells alleviated physical dysfunction and increased survival156. Some senolytic agents, notably dasatinib and quercetin (D + Q) and fisetin, have progressed to clinical testing for use in conditions including DKD157,158,159,160,161. Findings from an open label, phase I trial in patients with DKD demonstrated that a 3-day oral course of D + Q reduces the proportion of senescent cells in adipose and skin biopsy samples as well as circulating SASP factors in blood samples, suggesting that senolytics can reduce senescent cell burden and alleviate symptoms associated with age-related diseases158. Moreover, a 2024 study revealed that SGLT2 inhibitors exert an indirect senolytic effect in mice by increasing immune surveillance of senescent cells through downregulation of PDL1 expression162.
Of note, continuous or acute elimination of senescent vascular endothelial cells, particularly in liver sinusoids, disrupts blood–tissue barriers and leads to fibrosis, as these cells are not replaced after removal and have important structural and functional roles163. Other concerns include a potential increased risk of thrombocytopenia and neutropenia47. On the other hand, the induction of senolysis through inhibition of glutaminolysis49 may more specifically eliminate senescent PTECs where glutaminolysis is active164, highlighting the importance of a strategic approach in the development of senolytic therapies.
Targeting of mitochondrial function is another potential approach to ameliorate age-related diseases. Mitochonic acid 5 (MA-5) is a mitochondrial-targeted drug that has shown potential in preclinical models of kidney disease154. Mechanistically, MA-5 seems to attenuate oxidative stress-induced expression of the cytokine, GDF15, facilitate mitochondrial ATP production and reduce levels of ROS, suggesting that MA-5 may have potential as a drug for the treatment of several mitochondrial diseases155.
Therapeutic interventions that target autophagy pathways, such as mTOR inhibitors and autophagy enhancers, are also under investigation as potential strategies to promote kidney health117. Of note, the activation of autophagy may place strain on the lysosomal system, highlighting the need to also maintain lysosomal homeostasis. We have shown that supplementation with the polyunsaturated fatty acid, eicosapentaenoic acid — which attenuates the palmitic acid-induced redistribution of phospholipids from cellular membranes into lysosomes — reduces several hallmarks of kidney ageing in HFD-fed obese mice, including dysfunctional autophagy, lysosomal and mitochondrial dysfunction, inflammation and fibrosis78.
Mounting evidence also suggests that FGF21 can alleviate age-related metabolic disorders, such as atherosclerosis, obesity, diabetes and some cardiovascular diseases, by maintaining mitochondrial homeostasis and preventing stagnation of autophagy76. These findings are supported by the observation that transgenic mice that overexpress Fgf21 have an extended lifespan75,165. Notably, randomized controlled trials have demonstrated positive outcomes of FGF21 analogues in patients with severe hypertriglyceridaemia and non-alcoholic steatohepatitis166,167, suggesting that these agents may also demonstrate benefits in patients with CKD.
Approaches to target the gut–kidney axis
Gut dysbiosis, defined as an imbalance in the microbial composition of the gut, can lead to a loss of beneficial bacteria, the overgrowth of pathogenic bacteria and reduced microbial diversity168,169. Gut dysbiosis can be influenced by various factors including diet, use of antibiotics, infections and chronic diseases, and has been linked to numerous health conditions, including kidney disease99. The gut–kidney axis refers to multidirectional interactions between gut microbiota, gut microbiota-derived metabolites such as TMAO and the kidney that can contribute to progression of CKD168. As described above, TMAO has been associated with inflammation, oxidative stress and vascular dysfunction, with elevated levels associated with increased cardiovascular risk and kidney impairment51,170. Importantly, gut dysbiosis can increase the abundance of bacteria that convert dietary nutrients into trimethylamine (TMA), which is subsequently oxidized to TMAO169.
In patients with CKD, the reduced ability to excrete TMAO contributes to higher circulating levels, which exacerbates kidney damage. Dysbiosis-related inflammation can also affect kidney function through the release of inflammatory cytokines and endotoxins168,171. Interventions to manage TMAO and dysbiosis include reduced intake of red meat and choline-rich foods, increased fibre intake, and use of probiotics and prebiotics to support a healthy gut microbiota, although the evidence supporting the efficacy of these interventions is weak. Interestingly, in a 2022 study, high levels of 3-carboxy-4-methyl-5-propyl-2-furanpropionate, a biomarker of fish intake, were found to confer health benefits independently of TMAO and other clinically relevant confounders, prompting the researchers to suggest that fish intake might counteract the unfavourable actions of TMAO172. Pharmacological approaches to target TMAO, such as inhibitors of TMA formation and TMAO scavengers, are also being explored111.
Dietary interventions in patients with CKD
In the absence of pharmacological therapies, behavioural approaches, such as calorie restriction, regular exercise and certain anti-inflammatory medications, are currently the most promising strategies to promote healthy ageing173. Protein restriction may reduce the risk of CKD progression, but might increase the risk of sarcopenia. A 2024 study suggested that a low-protein diet that is prescribed and monitored is safe in older adults with CKD approaching kidney failure174.
Current evidence suggests that adopting plant-based diets has few risks but potential benefits for preventing and delaying the progression of CKD175,176. The potential mechanisms underlying these benefits are manifold. Plant phosphorus has a lower bioavailability than animal phosphorus and might therefore enable better control of hyperphosphataemia. The consumption of plant foods might increase levels of micronutrients such as magnesium, which may lower the cardiovascular risk associated with hyperphosphataemia177. Furthermore, plant-based diets might also help to manage and prevent some of the symptoms and metabolic complications of CKD175,176. Of interest, sulforaphane — a natural compound derived from broccoli and broccoli sprouts — not only ameliorates obesity-related kidney disease by enhancing autophagy, but also ameliorates age-related mitochondrial dysfunction and renal impairment via activation of NRF2 (refs. 178,179). Dietary bioactive compounds, such as phenolics, flavonoids and carotenoids are non-nutrient natural compounds found in various fruits, vegetables and other plant-based foods that may help to maintain cellular homeostasis and promote health through the regulation of autophagy and epigenetic marks, and the reduction of senescence and oxidative stress180.
Conclusions and future perspectives
CKD is associated with accelerated biological ageing, as evidenced by cellular senescence, inflammation, mitochondrial dysfunction, oxidative stress and defective autophagy. Improved understanding of the pathological mechanisms underlying this premature ageing phenotype in CKD could unveil novel therapeutic avenues for preventing age-related complications and improving outcomes in affected patients. Kidney ageing is not solely determined by genetic factors but can also be influenced by lifestyle, environment and concurrent illnesses. Therefore, assessments of CKD risk for early preventive measures should focus on biological age rather than chronological age. Despite the existence of numerous markers of biological age, their correlations with each other are often lower than anticipated131,181, indicating that various markers may capture distinct facets of the ageing process. Further research is therefore needed to validate and refine existing ageing biomarkers while also identifying more accurate and robust indicators of kidney ageing. By pinpointing factors and diseases that affect the pace of kidney ageing, several anti-ageing strategies have been proposed to promote healthy kidney ageing and delay the development of age-related kidney diseases. Improved understanding of the intricate interplay between the hallmarks of kidney ageing and susceptibility to age-related pathologies holds promise for the development of clinical interventions aimed at fostering long-term kidney health and improving overall health outcomes.
References
Ishani, A. et al. Acute kidney injury increases risk of ESRD among elderly. J. Am. Soc. Nephrol. 20, 223–228 (2009).
Ferenbach, D. A. & Bonventre, J. V. Mechanisms of maladaptive repair after AKI leading to accelerated kidney ageing and CKD. Nat. Rev. Nephrol. 11, 264–276 (2015).
Wang, X., Bonventre, J. V. & Parrish, A. R. The aging kidney: increased susceptibility to nephrotoxicity. Int. J. Mol. Sci. 15, 15358–15376 (2014).
Lopez-Otin, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. The hallmarks of aging. Cell 153, 1194–1217 (2013).
Lopez-Otin, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. Hallmarks of aging: an expanding universe. Cell 186, 243–278 (2023).
Mizushima, N. & Levine, B. Autophagy in human diseases. N. Engl. J. Med. 383, 1564–1576 (2020).
Takabatake, Y., Kimura, T., Takahashi, A. & Isaka, Y. Autophagy and the kidney: health and disease. Nephrol. Dial. Transpl. 29, 1639–1647 (2014).
Tang, C., Livingston, M. J., Liu, Z. & Dong, Z. Autophagy in kidney homeostasis and disease. Nat. Rev. Nephrol. 16, 489–508 (2020).
Kaushik, S. et al. Autophagy and the hallmarks of aging. Ageing Res. Rev. 72, 101468 (2021).
Aman, Y. et al. Autophagy in healthy aging and disease. Nat. Aging 1, 634–650 (2021).
Kooman, J. P., Kotanko, P., Schols, A. M., Shiels, P. G. & Stenvinkel, P. Chronic kidney disease and premature ageing. Nat. Rev. Nephrol. 10, 732–742 (2014).
Tian, Y. E. et al. Heterogeneous aging across multiple organ systems and prediction of chronic disease and mortality. Nat. Med. 29, 1221–1231 (2023).
Hommos, M. S., Glassock, R. J. & Rule, A. D. Structural and functional changes in human kidneys with healthy aging. J. Am. Soc. Nephrol. 28, 2838–2844 (2017).
Tan, J. C. et al. Effects of aging on glomerular function and number in living kidney donors. Kidney Int. 78, 686–692 (2010).
Glassock, R. J. & Rule, A. D. The implications of anatomical and functional changes of the aging kidney: with an emphasis on the glomeruli. Kidney Int. 82, 270–277 (2012).
Roeder, S. S. et al. Changes in glomerular parietal epithelial cells in mouse kidneys with advanced age. Am. J. Physiol. Ren. Physiol. 309, F164–F178 (2015).
Wiggins, J. E. Aging in the glomerulus. J. Gerontol. A Biol. Sci. Med. Sci. 67, 1358–1364 (2012).
Goligorsky, M. S. Emerging insights into glomerular vascular pole and microcirculation. J. Am. Soc. Nephrol. 33, 1641–1648 (2022).
Nangaku, M. Chronic hypoxia and tubulointerstitial injury: a final common pathway to end-stage renal failure. J. Am. Soc. Nephrol. 17, 17–25 (2006).
Tanaka, T. et al. Hypoxia and expression of hypoxia-inducible factor in the aging kidney. J. Gerontol. A Biol. Sci. Med. Sci. 61, 795–805 (2006).
Ryu, D. R. et al. Sirt1-hypoxia-inducible factor-1α interaction is a key mediator of tubulointerstitial damage in the aged kidney. Aging Cell 18, e12904 (2019).
Perico, L., Remuzzi, G. & Benigni, A. Sirtuins in kidney health and disease. Nat. Rev. Nephrol. 20, 313–329 (2024).
Semenza, G. L. Hypoxia-inducible factor 1: regulator of mitochondrial metabolism and mediator of ischemic preconditioning. Biochim. Biophys. Acta 1813, 1263–1268 (2011).
Kume, S. et al. Calorie restriction enhances cell adaptation to hypoxia through Sirt1-dependent mitochondrial autophagy in mouse aged kidney. J. Clin. Invest. 120, 1043–1055 (2010).
Mohandes, S. et al. Molecular pathways that drive diabetic kidney disease. J. Clin. Invest. 133, e165654 (2023).
Chuang, P. Y. et al. Reduction in podocyte SIRT1 accelerates kidney injury in aging mice. Am. J. Physiol. Ren. Physiol. 313, F621–F628 (2017).
Randles, M. J. et al. Identification of an altered matrix signature in kidney aging and disease. J. Am. Soc. Nephrol. 32, 1713–1732 (2021).
Isaka, Y. Targeting TGF-β signaling in kidney fibrosis. Int. J. Mol. Sci. 19, 2532 (2018).
Schumacher, B., Pothof, J., Vijg, J. & Hoeijmakers, J. H. J. The central role of DNA damage in the ageing process. Nature 592, 695–703 (2021).
Garaycoechea, J. I., Quinlan, C. & Luijsterburg, M. S. Pathological consequences of DNA damage in the kidney. Nat. Rev. Nephrol. 19, 229–243 (2023).
Wilson, P. C. et al. Mosaic loss of Y chromosome is associated with aging and epithelial injury in chronic kidney disease. Genome Biol. 25, 36 (2024).
Melk, A. et al. Telomere shortening in kidneys with age. J. Am. Soc. Nephrol. 11, 444–453 (2000).
Park, S. et al. A Mendelian randomization study found causal linkage between telomere attrition and chronic kidney disease. Kidney Int. 100, 1063–1070 (2021).
Carrero, J. J. et al. Telomere attrition is associated with inflammation, low fetuin-A levels and high mortality in prevalent haemodialysis patients. J. Intern. Med. 263, 302–312 (2008).
Shiels, P. G., McGuinness, D., Eriksson, M., Kooman, J. P. & Stenvinkel, P. The role of epigenetics in renal ageing. Nat. Rev. Nephrol. 13, 471–482 (2017).
Di Micco, R., Krizhanovsky, V., Baker, D. & d’Adda di Fagagna, F. Cellular senescence in ageing: from mechanisms to therapeutic opportunities. Nat. Rev. Mol. Cell Biol. 22, 75–95 (2021).
Docherty, M. H., O’Sullivan, E. D., Bonventre, J. V. & Ferenbach, D. A. Cellular senescence in the kidney. J. Am. Soc. Nephrol. 30, 726–736 (2019).
Sturmlechner, I., Durik, M., Sieben, C. J., Baker, D. J. & van Deursen, J. M. Cellular senescence in renal ageing and disease. Nat. Rev. Nephrol. 13, 77–89 (2017).
Huang, W., Hickson, L. J., Eirin, A., Kirkland, J. L. & Lerman, L. O. Cellular senescence: the good, the bad and the unknown. Nat. Rev. Nephrol. 18, 611–627 (2022).
Kim, S. R. et al. Progressive cellular senescence mediates renal dysfunction in ischemic nephropathy. J. Am. Soc. Nephrol. 32, 1987–2004 (2021).
Zhang, L. et al. C/EBPα deficiency in podocytes aggravates podocyte senescence and kidney injury in aging mice. Cell Death Dis. 10, 684 (2019).
Fang, Y. et al. Age-related GSK3β overexpression drives podocyte senescence and glomerular aging. J. Clin. Invest. 132, e141848 (2022).
Pippin, J. W. et al. Upregulated PD-1 signaling antagonizes glomerular health in aged kidneys and disease. J. Clin. Invest. 132, e156250 (2022).
Mylonas, K. J. et al. Cellular senescence inhibits renal regeneration after injury in mice, with senolytic treatment promoting repair. Sci. Transl. Med. 13, eabb0203 (2021).
Baker, D. J. et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 479, 232–236 (2011).
Jin, H. et al. Epithelial innate immunity mediates tubular cell senescence after kidney injury. JCI Insight 4, e125490 (2019).
Paez-Ribes, M., Gonzalez-Gualda, E., Doherty, G. J. & Munoz-Espin, D. Targeting senescent cells in translational medicine. EMBO Mol. Med. 11, e10234 (2019).
Chaib, S., Tchkonia, T. & Kirkland, J. L. Cellular senescence and senolytics: the path to the clinic. Nat. Med. 28, 1556–1568 (2022).
Johmura, Y. et al. Senolysis by glutaminolysis inhibition ameliorates various age-associated disorders. Science 371, 265–270 (2021).
Franceschi, C., Garagnani, P., Parini, P., Giuliani, C. & Santoro, A. Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 14, 576–590 (2018).
Evenepoel, P., Stenvinkel, P., Shanahan, C. & Pacifici, R. Inflammation and gut dysbiosis as drivers of CKD-MBD. Nat. Rev. Nephrol. 19, 646–657 (2023).
Sato, Y., Silina, K., van den Broek, M., Hirahara, K. & Yanagita, M. The roles of tertiary lymphoid structures in chronic diseases. Nat. Rev. Nephrol. 19, 525–537 (2023).
Stenvinkel, P. et al. Chronic inflammation in chronic kidney disease progression: role of Nrf2. Kidney Int. Rep. 6, 1775–1787 (2021).
Shelton, L. M., Park, B. K. & Copple, I. M. Role of Nrf2 in protection against acute kidney injury. Kidney Int. 84, 1090–1095 (2013).
Nezu, M. et al. Transcription factor Nrf2 hyperactivation in early-phase renal ischemia-reperfusion injury prevents tubular damage progression. Kidney Int. 91, 387–401 (2017).
Jo, M. J. et al. Impaired NRF2 inhibits recovery from ischemic reperfusion injury in the aging kidney. Antioxidants 12, 1440 (2023).
Martini, S. et al. Integrative biology identifies shared transcriptional networks in CKD. J. Am. Soc. Nephrol. 25, 2559–2572 (2014).
Salminen, A., Kaarniranta, K. & Kauppinen, A. Inflammaging: disturbed interplay between autophagy and inflammasomes. Aging 4, 166–175 (2012).
Komada, T. & Muruve, D. A. The role of inflammasomes in kidney disease. Nat. Rev. Nephrol. 15, 501–520 (2019).
Kaverina, N. et al. Inhibiting NLRP3 signaling in aging podocytes improves their life- and health-span. Aging 15, 6658–6689 (2023).
Sato, Y. et al. Heterogeneous fibroblasts underlie age-dependent tertiary lymphoid tissues in the kidney. JCI Insight 1, e87680 (2016).
Ligon, M. M. et al. Single cell and tissue-transcriptomic analysis of murine bladders reveals age- and TNFalpha-dependent but microbiota-independent tertiary lymphoid tissue formation. Mucosal Immunol. 13, 908–918 (2020).
Singh, P. et al. Lymphoid neogenesis and immune infiltration in aged liver. Hepatology 47, 1680–1690 (2008).
Sato, Y. & Yanagita, M. Immunology of the ageing kidney. Nat. Rev. Nephrol. 15, 625–640 (2019).
Sato, Y. et al. Developmental stages of tertiary lymphoid tissue reflect local injury and inflammation in mouse and human kidneys. Kidney Int. 98, 448–463 (2020).
Sato, Y. et al. CD153-CD30 signaling promotes age-dependent tertiary lymphoid tissue expansion and kidney injury. J. Clin. Invest. 132, e146071 (2021).
Lee, Y. H. et al. Advanced tertiary lymphoid tissues in protocol biopsies are associated with progressive graft dysfunction in kidney transplant recipients. J. Am. Soc. Nephrol. 33, 186–200 (2021).
Yoshikawa, T. et al. Tertiary lymphoid tissues are microenvironments with intensive interactions between immune cells and proinflammatory parenchymal cells in aged kidneys. J. Am. Soc. Nephrol. 34, 1687–1708 (2023).
Doke, T. & Susztak, K. The multifaceted role of kidney tubule mitochondrial dysfunction in kidney disease development. Trends Cell Biol. 32, 841–853 (2022).
Guan, Y. et al. Nicotinamide mononucleotide, an NAD+ precursor, rescues age-associated susceptibility to AKI in a sirtuin 1-dependent manner. J. Am. Soc. Nephrol. 28, 2337–2352 (2017).
Yamamoto, T. et al. Time-dependent dysregulation of autophagy: implications in aging and mitochondrial homeostasis in the kidney proximal tubule. Autophagy 12, 801–813 (2016).
Tang, C. et al. Mitochondrial quality control in kidney injury and repair. Nat. Rev. Nephrol. 17, 299–318 (2021).
Miwa, S., Kashyap, S., Chini, E. & von Zglinicki, T. Mitochondrial dysfunction in cell senescence and aging. J. Clin. Invest. 132, e158447 (2022).
Kishi, S., Nagasu, H., Kidokoro, K. & Kashihara, N. Oxidative stress and the role of redox signalling in chronic kidney disease. Nat. Rev. Nephrol. 20, 101–119 (2024).
Salminen, A., Kaarniranta, K. & Kauppinen, A. Regulation of longevity by FGF21: interaction between energy metabolism and stress responses. Ageing Res. Rev. 37, 79–93 (2017).
Minami, S. et al. FGF21 and autophagy coordinately counteract kidney disease progression during aging and obesity. Autophagy 20, 489–504 (2023).
Yamamoto, T. et al. High-fat diet-induced lysosomal dysfunction and impaired autophagic flux contribute to lipotoxicity in the kidney. J. Am. Soc. Nephrol. 28, 1534–1551 (2017).
Yamamoto, T. et al. Eicosapentaenoic acid attenuates renal lipotoxicity by restoring autophagic flux. Autophagy 17, 1700–1713 (2021).
Minami, S. et al. Lipophagy maintains energy homeostasis in the kidney proximal tubule during prolonged starvation. Autophagy 13, 1629–1647 (2017).
Matsumoto, A. et al. Spatiotemporally quantitative in vivo imaging of mitochondrial fatty acid β-oxidation at cellular-level resolution in mice. Am. J. Physiol. Endocrinol. Metab. 325, E552–E561 (2023).
Noels, H., Lehrke, M., Vanholder, R. & Jankowski, J. Lipoproteins and fatty acids in chronic kidney disease: molecular and metabolic alterations. Nat. Rev. Nephrol. 17, 528–542 (2021).
Mitrofanova, A., Merscher, S. & Fornoni, A. Kidney lipid dysmetabolism and lipid droplet accumulation in chronic kidney disease. Nat. Rev. Nephrol. 19, 629–645 (2023).
Mutlu, A. S., Duffy, J. & Wang, M. C. Lipid metabolism and lipid signals in aging and longevity. Dev. Cell 56, 1394–1407 (2021).
Braun, F. et al. Altered lipid metabolism in the aging kidney identified by three layered omic analysis. Aging 8, 441–457 (2016).
Kang, H. M. et al. Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat. Med. 21, 37–46 (2015).
Dhillon, P. et al. The nuclear receptor ESRRA protects from kidney disease by coupling metabolism and differentiation. Cell Metab. 33, 379–394.e8 (2021).
Chung, K. W. et al. Impairment of PPARα and the fatty acid oxidation pathway aggravates renal fibrosis during aging. J. Am. Soc. Nephrol. 29, 1223–1237 (2018).
Lee, G. et al. PGC-1α, a potential therapeutic target against kidney aging. Aging Cell 18, e12994 (2019).
Kuro-o, M. et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 390, 45–51 (1997).
Kurosu, H. et al. Suppression of aging in mice by the hormone Klotho. Science 309, 1829–1833 (2005).
Shi, M. et al. αKlotho mitigates progression of AKI to CKD through activation of autophagy. J. Am. Soc. Nephrol. 27, 2331–2345 (2016).
Wang, Y. et al. Imbalanced lipid homeostasis caused by membrane αKlotho deficiency contributes to the acute kidney injury to chronic kidney disease transition. Kidney Int. 104, 956–974 (2023).
Edmonston, D. et al. Klotho and clinical outcomes in CKD. Am. J. Kidney Dis. https://doi.org/10.1053/j.ajkd.2024.02.008 (2024).
Fujimura, R. et al. Autophagy protects kidney from phosphate-induced mitochondrial injury. Biochem. Biophys. Res. Commun. 524, 636–642 (2020).
Kuro, O. M. Phosphate as a pathogen of arteriosclerosis and aging. J. Atheroscler. Thromb. 28, 203–213 (2021).
Kawai, M., Kinoshita, S., Ozono, K. & Michigami, T. Inorganic phosphate activates the AKT/mTORC1 pathway and shortens the life span of an α-klotho-deficient model. J. Am. Soc. Nephrol. 27, 2810–2824 (2016).
Kuro, O. M. Klotho and calciprotein particles as therapeutic targets against accelerated ageing. Clin. Sci. 135, 1915–1927 (2021).
Shiizaki, K. et al. Calcium phosphate microcrystals in the renal tubular fluid accelerate chronic kidney disease progression. J. Clin. Invest. 131, e145693 (2021).
Mafra, D. et al. Food as medicine: targeting the uraemic phenotype in chronic kidney disease. Nat. Rev. Nephrol. 17, 153–171 (2021).
Avesani, C. M., Cuppari, L., Nerbass, F. B., Lindholm, B. & Stenvinkel, P. Ultraprocessed foods and chronic kidney disease – double trouble. Clin. Kidney J. 16, 1723–1736 (2023).
Dominguez, L. J., Veronese, N. & Barbagallo, M. Magnesium and the hallmarks of aging. Nutrients 16, 496 (2024).
Sakaguchi, Y. et al. Hypomagnesemia in type 2 diabetic nephropathy: a novel predictor of end-stage renal disease. Diabetes Care 35, 1591–1597 (2012).
Oka, T. et al. Proteinuria-associated renal magnesium wasting leads to hypomagnesemia: a common electrolyte abnormality in chronic kidney disease. Nephrol. Dial. Transpl. 34, 1154–1162 (2019).
Du, S., Kim, H., Crews, D. C., White, K. & Rebholz, C. M. Association between ultraprocessed food consumption and risk of incident CKD: a prospective cohort study. Am. J. Kidney Dis. 80, 589–598.e1 (2022).
Su, D. et al. Metabolomic markers of ultra-processed food and incident CKD. Clin. J. Am. Soc. Nephrol. 18, 327–336 (2023).
Rebholz, C. M. et al. Dietary magnesium and kidney function decline: the healthy aging in neighborhoods of diversity across the life span study. Am. J. Nephrol. 44, 381–387 (2016).
Sakaguchi, Y. et al. Low magnesium diet aggravates phosphate-induced kidney injury. Nephrol. Dial. Transpl. 34, 1310–1319 (2019).
Diaz-Tocados, J. M. et al. Dietary magnesium supplementation prevents and reverses vascular and soft tissue calcifications in uremic rats. Kidney Int. 92, 1084–1099 (2017).
Sakaguchi, Y. et al. Magnesium modifies the association between serum phosphate and the risk of progression to end-stage kidney disease in patients with non-diabetic chronic kidney disease. Kidney Int. 88, 833–842 (2015).
Jahan, N. et al. Possible contribution of phosphate to the pathogenesis of chronic kidney disease in dolphins. Sci. Rep. 13, 5161 (2023).
Gupta, N. et al. Targeted inhibition of gut microbial trimethylamine N-oxide production reduces renal tubulointerstitial fibrosis and functional impairment in a murine model of chronic kidney disease. Arterioscler. Thromb. Vasc. Biol. 40, 1239–1255 (2020).
Wang, M. et al. The gut microbial metabolite trimethylamine N-oxide, incident CKD, and kidney function decline. J. Am. Soc. Nephrol. 9, 934113 (2024).
Sakai, S. et al. Proximal tubule autophagy differs in type 1 and 2 diabetes. J. Am. Soc. Nephrol. 30, 929–945 (2019).
Takahashi, A. et al. Autophagy inhibits the accumulation of advanced glycation end products by promoting lysosomal biogenesis and function in the kidney proximal tubules. Diabetes 66, 1359–1372 (2017).
Ballabio, A. & Bonifacino, J. S. Lysosomes as dynamic regulators of cell and organismal homeostasis. Nat. Rev. Mol. Cell Biol. 21, 101–118 (2020).
Yamamoto, T., Nakamura, J., Takabatake, Y. & Isaka, Y. Obesity-related proximal tubulopathy: an emerging threat to kidney health. Autophagy Rep. 2, https://doi.org/10.1080/27694127.2023.2200341 (2023).
Minami, S., Yamamoto, T., Yamamoto-Imoto, H., Isaka, Y. & Hamasaki, M. Autophagy and kidney aging. Prog. Biophys. Mol. Biol. 179, 10–15 (2023).
Cui, M. et al. HKDC1, a target of TFEB, is essential to maintain both mitochondrial and lysosomal homeostasis, preventing cellular senescence. Proc. Natl Acad. Sci. USA 121, e2306454120 (2024).
Gros, F. & Muller, S. The role of lysosomes in metabolic and autoimmune diseases. Nat. Rev. Nephrol. 19, 366–383 (2023).
Takabatake, Y., Yamamoto, T. & Isaka, Y. Stagnation of autophagy: a novel mechanism of renal lipotoxicity. Autophagy 13, 775–776 (2017).
Nakamura, J. et al. TFEB-mediated lysosomal exocytosis alleviates high-fat diet-induced lipotoxicity in the kidney. JCI Insight 8, e162498 (2023).
Matsunaga, K. et al. Two Beclin 1-binding proteins, Atg14L and Rubicon, reciprocally regulate autophagy at different stages. Nat. Cell Biol. 11, 385–396 (2009).
Nakamura, S. et al. Suppression of autophagic activity by Rubicon is a signature of aging. Nat. Commun. 10, 847 (2019).
Yamamoto-Imoto, H. et al. Age-associated decline of MondoA drives cellular senescence through impaired autophagy and mitochondrial homeostasis. Cell Rep. 38, 110444 (2022).
Maeda, S. et al. MondoA and AKI and AKI-to-CKD transition. J. Am. Soc. Nephrol. https://doi.org/10.1681/ASN.0000000000000414 (2024).
Kim, J., Kundu, M., Viollet, B. & Guan, K. L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat. Cell Biol. 13, 132–141 (2011).
Huynh, C., Ryu, J., Lee, J., Inoki, A. & Inoki, K. Nutrient-sensing mTORC1 and AMPK pathways in chronic kidney diseases. Nat. Rev. Nephrol. 19, 102–122 (2023).
Zhang, W., Feng, C. & Jiang, H. Novel target for treating Alzheimer’s diseases: crosstalk between the Nrf2 pathway and autophagy. Ageing Res. Rev. 65, 101207 (2021).
Oh, H. S. et al. Organ aging signatures in the plasma proteome track health and disease. Nature 624, 164–172 (2023).
Cohen, N. M. et al. Longitudinal machine learning uncouples healthy aging factors from chronic disease risks. Nat. Aging 4, 129–144 (2024).
Rutledge, J., Oh, H. & Wyss-Coray, T. Measuring biological age using omics data. Nat. Rev. Genet. 23, 715–727 (2022).
Shiels, P. G. et al. Manipulating the exposome to enable better ageing. Biochem. J. 478, 2889–2898 (2021).
Stenvinkel, P., Avesani, C. M., Gordon, L. J., Schalling, M. & Shiels, P. G. Biomimetics provides lessons from nature for contemporary ways to improve human health. J. Clin. Transl. Sci. 5, e128 (2021).
Ebert, T. et al. Inflammation and premature ageing in chronic kidney disease. Toxins 12, 227 (2020).
Singh, M., Stewart, R. & White, H. Importance of frailty in patients with cardiovascular disease. Eur. Heart J. 35, 1726–1731 (2014).
Otobe, Y., Rhee, C. M., Nguyen, M., Kalantar-Zadeh, K. & Kopple, J. D. Current status of the assessment of sarcopenia, frailty, physical performance and functional status in chronic kidney disease patients. Curr. Opin. Nephrol. Hypertens. 31, 109–128 (2022).
Fried, L. P. et al. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146–M156 (2001).
Nixon, A. C. et al. Frailty and chronic kidney disease: current evidence and continuing uncertainties. Clin. Kidney J. 11, 236–245 (2018).
Miao, Z., Humphreys, B. D., McMahon, A. P. & Kim, J. Multi-omics integration in the age of million single-cell data. Nat. Rev. Nephrol. 17, 710–724 (2021).
Klinkhammer, B. M. et al. Non-invasive molecular imaging of kidney diseases. Nat. Rev. Nephrol. 17, 688–703 (2021).
Schreibing, F. & Kramann, R. Mapping the human kidney using single-cell genomics. Nat. Rev. Nephrol. 18, 347–360 (2022).
He, X., Memczak, S., Qu, J., Belmonte, J. C. I. & Liu, G. H. Single-cell omics in ageing: a young and growing field. Nat. Metab. 2, 293–302 (2020).
Kirita, Y., Wu, H., Uchimura, K., Wilson, P. C. & Humphreys, B. D. Cell profiling of mouse acute kidney injury reveals conserved cellular responses to injury. Proc. Natl Acad. Sci. USA 117, 15874–15883 (2020).
Ahadi, S. et al. Personal aging markers and ageotypes revealed by deep longitudinal profiling. Nat. Med. 26, 83–90 (2020).
Baek, J., He, C., Afshinnia, F., Michailidis, G. & Pennathur, S. Lipidomic approaches to dissect dysregulated lipid metabolism in kidney disease. Nat. Rev. Nephrol. 18, 38–55 (2022).
Tsugawa, H. et al. A lipidome landscape of aging in mice. Nat. Aging 4, 709–726 (2024).
Burtscher, J. et al. Mitochondrial stress and mitokines in aging. Aging Cell 22, e13770 (2023).
Kim, K. H. et al. Autophagy deficiency leads to protection from obesity and insulin resistance by inducing Fgf21 as a mitokine. Nat. Med. 19, 83–92 (2013).
Hamano, T. et al. Fetuin-mineral complex reflects extraosseous calcification stress in CKD. J. Am. Soc. Nephrol. 21, 1998–2007 (2010).
Miura, Y., Kurosu, H. & Kuro, O. M. Quantification of calciprotein particles (CPPs) in serum/plasma samples using a fluorescent bisphosphonate. Methods Mol. Biol. 2664, 333–341 (2023).
Mukai, H. et al. Skin autofluorescence, arterial stiffness and Framingham risk score as predictors of clinical outcome in chronic kidney disease patients: a cohort study. Nephrol. Dial. Transpl. 34, 442–448 (2019).
Reurean-Pintilei, D. et al. Skin autofluorescence as a potential adjunctive marker for cardiovascular risk assessment in type 2 diabetes: a systematic review. Int. J. Mol. Sci. 25, 3889 (2024).
Neytchev, O. et al. Epigenetic clocks indicate that kidney transplantation and not dialysis mitigate the effects of renal ageing. J. Intern. Med. 295, 79–90 (2024).
Suzuki, T. et al. Mitochonic acid 5 binds mitochondria and ameliorates renal tubular and cardiac myocyte damage. J. Am. Soc. Nephrol. 27, 1925–1932 (2016).
Matsuhashi, T. et al. Mitochonic acid 5 (MA-5) facilitates ATP synthase oligomerization and cell survival in various mitochondrial diseases. EBioMedicine 20, 27–38 (2017).
Xu, M. et al. Senolytics improve physical function and increase lifespan in old age. Nat. Med. 24, 1246–1256 (2018).
Zhang, L. et al. Cellular senescence: a key therapeutic target in aging and diseases. J. Clin. Invest. 132, e158450 (2022).
Hickson, L. J. et al. Senolytics decrease senescent cells in humans: preliminary report from a clinical trial of dasatinib plus quercetin in individuals with diabetic kidney disease. EBioMedicine 47, 446–456 (2019).
US National Library of Medicine. ClinicalTrials.gov www.clinicaltrials.gov/study/NCT02848131?term=NCT02848131&rank=1 (2024).
US National Library of Medicine. ClinicalTrials.gov www.clinicaltrials.gov/study/NCT04313634?term=NCT04313634&rank=1 (2024).
US National Library of Medicine. ClinicalTrials.gov www.clinicaltrials.gov/study/NCT04733534?term=NCT04733534&rank=1 (2023).
Katsuumi, G. et al. SGLT2 inhibition eliminates senescent cells and alleviates pathological aging. Nat. Aging 10.1038/s43587-024-00642-y (2024).
Grosse, L. et al. Defined p16High senescent cell types are indispensable for mouse healthspan. Cell Metab. 32, 87–99.e6 (2020).
Namba, T. et al. Autophagic clearance of mitochondria in the kidney copes with metabolic acidosis. J. Am. Soc. Nephrol. 25, 2254–2266 (2014).
Zhang, Y. et al. The starvation hormone, fibroblast growth factor-21, extends lifespan in mice. Elife 1, e00065 (2012).
Bhatt, D. L. et al. The FGF21 analog pegozafermin in severe hypertriglyceridemia: a randomized phase 2 trial. Nat. Med. 29, 1782–1792 (2023).
Loomba, R. et al. Randomized, controlled trial of the FGF21 analogue pegozafermin in NASH. N. Engl. J. Med. 389, 998–1008 (2023).
Yang, T., Richards, E. M., Pepine, C. J. & Raizada, M. K. The gut microbiota and the brain–gut–kidney axis in hypertension and chronic kidney disease. Nat. Rev. Nephrol. 14, 442–456 (2018).
Buffa, J. A. et al. The microbial gbu gene cluster links cardiovascular disease risk associated with red meat consumption to microbiota l-carnitine catabolism. Nat. Microbiol. 7, 73–86 (2022).
Lew, Q. J. et al. Red meat intake and risk of ESRD. J. Am. Soc. Nephrol. 28, 304–312 (2017).
Taguchi, K., Fukami, K., Elias, B. C. & Brooks, C. R. Dysbiosis-related advanced glycation endproducts and trimethylamine N-oxide in chronic kidney disease. Toxins 13, 361 (2021).
Dai, L. et al. The association between TMAO, CMPF, and clinical outcomes in advanced chronic kidney disease: results from the European QUALity (EQUAL) study. Am. J. Clin. Nutr. 116, 1842–1851 (2022).
Fontana, L. & Partridge, L. Promoting health and longevity through diet: from model organisms to humans. Cell 161, 106–118 (2015).
Windahl, K. et al. The safety of a low protein diet in older adults with advanced chronic kidney disease. Nephrol. Dial. Transpl. https://doi.org/10.1093/ndt/gfae077 (2024).
Carrero, J. J. et al. Plant-based diets to manage the risks and complications of chronic kidney disease. Nat. Rev. Nephrol. 16, 525–542 (2020).
Sakaguchi, Y., Kaimori, J. Y. & Isaka, Y. Plant-dominant low protein diet: a potential alternative dietary practice for patients with chronic kidney disease. Nutrients 15, 1002 (2023).
Sakaguchi, Y., Hamano, T. & Isaka, Y. Effects of magnesium on the phosphate toxicity in chronic kidney disease: time for intervention studies. Nutrients 9, 112 (2017).
Lu, Y., Zhang, Y., Lou, Y., Cui, W. & Miao, L. Sulforaphane suppresses obesity-related glomerulopathy-induced damage by enhancing autophagy via Nrf2. Life Sci. 258, 118153 (2020).
Mohammad, R. S., Lokhandwala, M. F. & Banday, A. A. Age-related mitochondrial impairment and renal injury is ameliorated by sulforaphane via activation of transcription factor NRF2. Antioxidants 11, 156 (2022).
Luis, C. et al. Nutritional senolytics and senomorphics: implications to immune cells metabolism and aging – from theory to practice. Front. Nutr. 9, 958563 (2022).
Jylhava, J., Pedersen, N. L. & Hagg, S. Biological age predictors. EBioMedicine 21, 29–36 (2017).
Acknowledgements
The authors’ work is supported by Japan Society for the Promotion of Science (21K16163, 23K07671 to T.Y. and 21H02935 to Y.I.), Japan Agency for Medical Research and Development (JP23ek0310022 to T.Y. and JP22gm1410014 to Y.I.), the Astellas Foundation for Research on Metabolic Disorders, Naito Foundation, Kato Memorial Bioscience Foundation, Salt Science Research Foundation, Sumitomo Insurance Welfare Foundation, G-7 Scholarship Foundation, and Takeda Medical Research Foundation (to T. Y.).
Author information
Authors and Affiliations
Contributions
Both authors made substantial contributions to discussions of the content and wrote, reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Jeroen Kooman, Motoko Yanagita, Oliver Wessely and Peter Stenvinkel for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamamoto, T., Isaka, Y. Pathological mechanisms of kidney disease in ageing. Nat Rev Nephrol 20, 603–615 (2024). https://doi.org/10.1038/s41581-024-00868-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-024-00868-4
- Springer Nature Limited
This article is cited by
-
A focus on kidney ageing
Nature Reviews Nephrology (2024)