Abstract
With the progressive improvement in healthcare provision and socio-economic development globally, the average life expectancy has increased, resulting in an ageing population. Ageing is associated with a large number of renal physiological and histological changes, as well as an accumulation of comorbidity-related renal injury, all culminating in chronic kidney disease and predisposition to acute kidney injury. However, the management of kidney diseases in the ageing population carries a unique set of challenges. Ageing is frequently associated with frailty, polypharmacy and multiple comorbidities that require a tailored approach to management, with particular focus on quality of life, functional abilities and cognition. These factors are also important when considering renal replacement therapy, where standard life expectancy benefits or adverse events, including post-transplant infection or rejection rates, can often not be extrapolated to the ageing population.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning Objectives-
1.
To understand the challenges posed by the ageing CKD population
-
2.
To appreciate that physiological and psychosocial differences impact on the management of older patients with kidney disease, necessitating an individualised approach to their management
-
3.
To recognise that frailty is often the greatest predictor of patient outcome in the elderly rather than the modality or adequacy of renal replacement therapy
1 Introduction
The World Health Organization (WHO) estimates that by 2050 the proportion of the world’s population over the age of 60 will have nearly doubled from that in 2015, from 12% to 22%. In the UK the number of people over 60 is expected to reach 18.5 million by 2025. This will result in an increasingly polymorbid population (75% of 75-year-olds in the UK have more than one long-term condition [1], 30% with CKD; ◘ Fig. 45.1) and exponential rises in healthcare usage.
Estimated CKD stage 3–5 prevalence amongst 38,262 adults in England between 1998 and 2003. (Reproduced using data from Stevens et al. [2])
2 Ageing and Chronic Kidney Disease (CKD)
Ageing is associated with senescence of tissues. In the kidneys this results in an approximately 50% reduction in functional nephron mass by the age of 70 when compared to 29–30-year-olds (◘ Fig. 45.2), with a parallel decline in glomerular filtration rate (GFR). The structural changes seen in ageing are evident from studies of tissue from living donor kidneys, which demonstrate typical features such as tubular atrophy, glomerulosclerosis, interstitial fibrosis and athero- and arteriosclerosis (◘ Figs. 45.3 and 45.4). When added to the accrued damage from diseases, such as diabetes and hypertension, these result in an increased risk of CKD. There is also an increased predisposition to acute kidney injury due to toxicity from renally excreted drugs and ischaemic insults.
Effect of age on total kidney, cortical and medullary volumes based on histology from living kidney donors. Cortical volume declines, whereas medullary volume increases, making total kidney volume relatively stable until about 50 years of age. (Modified from O’Neill et al. [3])
Ageing-related changes in the kidney. (Adapted from Bolignano et al. [4])
The relationship between increasing age and prevalence of CKD is based on an estimated GFR (eGFR) cut-off of 60 ml/min/1.73 m2, as defined by the Kidney Disease Improving Global Outcomes (KDIGO) guidelines. This does not acknowledge the decline in kidney function with physiological ageing. In the original studies of age-related GFR changes in healthy subjects, a sequential reduction in GFR from 122.8 ± 16.4 ml/min/1.73 m2 to 65.3 ± 20.4 ml/min/1.73 m2 was found in patients in their 20s and 80s, respectively [5]. In a series of over 1000 healthy American kidney donors, GFR declined by 8 ml/decade after the age of 45 [6]. GFR is typically estimated using the MDRD and CKD-EPI equations, both of which were formulated using a study population under the age of 70. Additionally, they assume unvarying muscle mass, despite body composition changing with age.
It is likely that we have neither a reliable nor validated method of estimating GFR in the older population and that our standard cut-offs for CKD should be age adjusted. That said, the KDIGO eGFR cut-off was determined by a large meta-analysis looking at mortality, cardiovascular risk, risk of end-stage renal disease and progressive CKD, and a subgroup analysis of >65-year-olds included in the study showed similar increases in risk in all the aforementioned categories at an eGFR less than 60 ml/min/1.73 m2.
3 Ageing and the Management of Chronic Kidney Disease (CKD)
The management of CKD has evolved over the last decade to focus on targets for the management of complications, such as anaemia and mineral bone disease, and with planning and preparing for dialysis or transplantation in its later stages. There is also increasing emphasis on reducing cardiovascular risk by controlling hypertension, diabetes and hyperlipidaemia. These therapeutic targets are generally derived from clinical trials that exclude older patients (and thus lack a solid evidence base to support their implementation in this population) and have end points that are not as relevant (or even detrimental) to their care. For example, major CKD trials, such as AASK [7] and REIN2 [8], included patients only up to the age of 70, with a mean age of 54 years old.
Older patients are often polymorbid and may suffer from one or more of the ‘geriatric syndromes’, making application of standardised care challenging. In addition, many of these syndromes occur more commonly and severely in the context of CKD and frequently coexist. These include cognitive impairment and delirium, falls, polypharmacy, depression, immobility and frailty. Frailty (a phenotype partly defined by weight loss, muscle weakness and fatigue) is especially associated with adverse outcomes in geriatric populations [9].
Several factors should be considered when applying standardised treatment targets to elderly patients, one being the potential harmful impact of interventions: for example, aggressive blood pressure control can lead to postural hypotension and falls. Treatment priorities are often different in the ageing population: these may include maintaining mobility and independence, alleviating symptoms and suffering and maintaining social relationships. Furthermore, whilst hospital admission to expedite investigations and instigate aggressive treatment may improve outcomes for a younger patient, elderly patients will decondition rapidly and have higher risks of delirium and hospital-acquired infections, leading to prolonged hospital stays, pressure sores, low mood and reduced functional status at discharge (◘ Table 45.1).
4 End-Stage Renal Failure (ESRF) and Renal Replacement Therapy Decisions in the Elderly
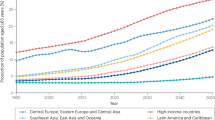
Starting dialysis therapy in later life does not carry the same mortality benefit seen in younger patients (◘ Fig. 45.5). However, within each age cohort, there is a wide degree of variation in life expectancy, with no validated method of predicting good outcomes on dialysis (although high frailty scores and low BMI have been associated with increased mortality in elderly dialysis patients [16]). Choices regarding dialysis become increasingly difficult in the context of mild to moderate cognitive impairment, when judgements about ‘quality of life’ come into question, and complex family and ethical issues need to be considered.
UK renal registry data on unadjusted survival of incident RRT patients by age (2014 cohort). (Open access article by Methven et al. [17])
Whilst there appears to be a modest survival benefit with dialysis (◘ Fig. 45.6), there are many potential drawbacks, including the tolerability of treatments, increased hospital attendance and admissions and an increased likelihood of dying in hospital. Some studies have suggested an increase in symptom burden upon starting dialysis, with a stepwise decline in functional ability with each hospital admission.
Mortality difference between patients randomised to dialysis therapy compared with medical management in different age groups, subdivided by eGFR at initiation of therapy. This data suggests that initiating dialysis at a higher eGFR results in a diminished mortality benefit compared to medical management, whereas starting dialysis at an eGFR of <6 had a greater mortality benefit, albeit a difference of only 19–26 months. (Reproduced using data from 73 349 US veterans from Tamura et al. [18])
Whilst it is suggested that most elderly patients would choose quality of life over longevity, it is not clear what strategy is best to achieve this goal. Further trials are needed to ascertain the right treatment options in this group, including better assessment tools to predict outcomes on dialysis, such as frailty scores, which will help guide clinicians, patients and families in decision-making. One such strategy may be to incorporate the comprehensive geriatric assessment (GCA) into the process. The GCA is a validated tool, which has been beneficial in the assessment of elderly surgical candidates and may be a useful adjunct when making these decisions. There has also been increasing use of augmented dialysis strategies, such as reduced frequency dialysis, which has been shown to improve quality of life for patients rather than regimes with aim to achieve the standard targets of dialysis adequacy (◘ Table 45.2).
5 Ageing and Transplantation
5.1 Patient and Allograft Outcomes
There is an overall increased survival in older patients after kidney transplantation compared to those who remain on dialysis [19]. However, special considerations should be made when considering transplantation in an older individual (◘ Fig. 45.7). As older recipients are more likely to die with a functioning graft, some argued that older donor kidneys or extended criteria donor (ECD) kidneys should be preferentially offered to older recipients. In Europe, the Eurotransplant Senior Program (ESP) initiative is aimed at reducing waiting times for older patients. Kidneys from donors >65 years of age are allocated to recipients >65 years of age within a small geographical area to minimise cold ischaemic time. The 15-year outcome from this showed that despite a higher complication rate (mainly due to atherosclerotic vascular disease of the recipient and donor), the patient and allograft survival are comparable with younger patients. However, both the patient and allograft survival in older kidney transplant recipients (KTRs) who received ECD kidneys are worse when compared to those who received standard criteria donors (SCD) or living donor kidneys, even when adjusted for other donor and recipient factors and pre-transplant dialysis vintage. Renal function at 1 year is similarly worse in older KTRs, who had received an ECD kidney, as compared to a SCD or living donor kidney [20, 21]. Overall, SCD and living donor transplantation is preferred for older patients, but ECD transplantation should be offered to those without a living donor who otherwise will have a very long wait for a SCD kidney.
5.2 Rejection
Acute rejection rates are overall lower in older transplant recipients, likely due to decreased immunocompetence. However, preventing acute rejection is critical in older KTRs as rejection can have a greater impact on long-term graft survival in the older compared to younger recipients.
5.3 Comorbidities and Frailty in the Older KTR
Frailty increases risks of adverse post-operative outcomes and is a predictor of prolonged hospital stays and early hospital readmission. It has also been identified to be the best predictor of 30-day post-operative complications independent of age and is an independent risk factor for mortality.
5.4 Immunosuppressive Therapy
The innate and adaptive immune systems change with age, as do the pharmacokinetics and pharmacodynamics of immunosuppressive drugs. Older KTRs have been found to require significantly lower doses of cyclosporine to achieve similar plasma drug concentrations than young recipients [22]. High calcineurin inhibitor (CNI) peak levels have nephrotoxic potential that can hasten graft failure especially in ECD kidneys. Age-related reduction in hepatic and renal clearance is compounded by factors, such as frailty, comorbidity and polypharmacy, resulting in drug interactions and changes in availability and distribution. For instance, mycophenolate mofetil (MMF) clearance decreases with falling renal function, albumin levels and haemoglobin – all of which are affected in older transplant recipients. MMF usage is also associated with a higher incidence of opportunistic infections (viral, fungal and mycobacterial) [23] in the elderly. The clinical implication of immunosuppressive therapy in older KTRs is clearly significant, but few studies have looked into the impact of these drugs in this age group. Ideally, age-specific immunosuppressive protocols should be developed to optimise both the patient and graft survival and reduce overall morbidity.
6 Individualisation of Treatment and Palliati ve Care
Older patients benefit from an individualised and multidisciplinary approach to care. The treatment priorities of an older patient often centre around social needs and quality of life rather than the standard outcomes of mortality and disease progression that is often used to guide treatment. Some centres in the USA, such as Mount Sinai in New York, have pioneered a multidisciplinary geriatric renal service for patients over the age of 60 with geriatric syndromes, which focuses on both dialysis and non-dialysis therapies and addresses many of the geriatric syndromes and symptom management. Their main focus is on improving quality of life, maintaining independence and avoiding hospital attendances.
The National Service Framework for Renal Services calls for renal patients to have a timely evaluation of their prognosis and information about the choices available to them. High-quality palliative care should be accessible at all stages of patient care, and systems in place to recognise patients who are struggling or declining on dialysis, and for providing opportunities to discuss withdrawal. Anticipatory prescribing for symptom control should be adapted to take renal function into account and an end of life care plan built around an individual’s needs and wishes should be made accessible to everyone involved in their care, including family members (see Palliative Care chapter).
Tips and Tricks
-
1.
Consider how therapeutic interventions might confer no benefit to, and even adversely affect, elderly patients.
-
2.
Always assess fall risk, including a postural BP measurement, before up-titrating BP medications, and avoid intensive blood pressure control in very frail patients, especially if non-ambulant and particularly if the pretreatment diastolic BP is low.
-
3.
The use of frailty scores and taking into consideration BMI and comprehensive geriatric assessment can be a useful tool in guiding decisions regarding renal replacement therapy.
-
4.
Changes in the ageing immune system, pharmacokinetics and pharmacodynamics of immunosuppressive drugs used necessitates careful consideration when prescribing immunosuppression for older recipients.
-
5.
A comprehensive evaluation of prospective older transplant recipients should include not only premorbid conditions but also baseline cognition and physical function.
-
6.
Consider additional treatment goals such as independence and quality of life when managing elderly patients.
Chapter Review Questions
-
1.
Should ACE/ARB inhibitors be used as first-line antihypertensive therapy for patients with diabetes-related CKD in the elderly?
-
2.
What is the best anticoagulant to use for stroke prevention in atrial fibrillation (AF) for older patients with CKD?
-
3.
Which type of donor kidney is preferred for older recipients?
-
4.
What is the major cause of graft loss in older KTRs?
Answers
-
1.
Not necessarily: The European Society of Hypertension and the American Heart Association both advise that it is the degree of BP control rather than the agent that had the greatest effect on improving outcomes. In the ALLHAT trial, lisinopril was less effective than chlorthalidone at improving cardiovascular end points. Although trials including IDNT and RENAAL both suggested renoprotective benefits of RAS blockade in type 2 diabetes, it is clear that elderly patients are at higher risk of AKI episodes, electrolyte disturbance and orthostatic hypotension, which should all be considered before commencing RAS blockade. However, all the major heart failure trials included large numbers of older patients and suggested that they would have the same benefit as a younger cohort, which may on balance mean that ACE/ARB therapy would be preferred where possible.
-
2.
Evidence supports the use of NOACs rather than warfarin. Apixaban is the favoured choice due to the lowest proportion of renal clearance (27%)46 and superiority to warfarin in stroke/VTE prevention seen in the ARISTOTLE trial and, more importantly, reduced risk of major bleeding (HR 0.5).29
-
3.
The best patient and graft survival outcomes in older KTRs are in those who receive living donor kidneys. However, older patients who receive ECD kidneys still have better outcomes than those who remain on dialysis.
-
4.
The major cause of graft loss in older KTRs is patient death with a functioning allograft. CVS disease and infection remain the predominant cause of death in older KTRs. A majority of infections occur in the first 6 months post transplantation.
Case Study
Case 1
A 76-year-old man is referred to the low clearance clinic with a stable eGFR of 30 ml/min/1.73 m2. He has a history of type 2 diabetes, symptomatic heart failure, atrial fibrillation and hypertension with a resting BP of 170/80 and his HbA1c is 7.4%. He lives at home with his wife and manages his activities of daily living independently. He is currently taking metformin, ramipril, bisoprolol, atorvastatin and sodium bicarbonate tablets. This man has advancing CKD with isolated systolic hypertension and is at high risk of stroke (as per his CHADS-VASC score of 5). His ramipril dose should be up-titrated to achieve a systolic BP of <140 mmHg but to avoid a DBP of <60, which was associated with increased risk of cardiovascular event in the SHEP study [24]. He should be offered anticoagulation with a novel oral anti-coagulant (NOAC), but other factors, such as fall risk, should be considered. He should then be monitored closely for deterioration in renal function, at which time metformin and NOAC treatment should be reviewed as there is limited data available on anticoagulation in advanced renal failure. He should not be offered aspirin therapy as there is increasing evidence that there is no benefit in primary prevention and excessive bleeding risks have been demonstrated with concurrent anticoagulant use. His diabetes control should not be intensified as this has been associated in increased mortality risk in the ACCORD trial [25]. He should be given advice on lifestyle modification including salt restriction, diet and exercise.
Case 2
A 69-year-old patient who received a kidney transplant 3 years ago presents to clinic feeling generally unwell. His blood tests come back showing a Hb of 98 g/dl, a creatinine of 180mcmol/l from a baseline of 150mcmol/l and a Cytomegalovirus (CMV) titre of 10,000 copies/ml. He has a history of diabetes with diabetic nephropathy leading to ESRF, hypertension and gout and continues to smoke ten cigarettes a day. His maintenance immunosuppression includes tacrolimus (with levels of 6–8) and mycophenolate mofetil 500 mg twice daily, and he never suffered from graft rejection before. This patient has CMV viraemia that warrants urgent treatment with antivirals. The rise in his creatinine is likely secondary to the viraemia, but in the context of a raised CNI level, CNI toxicity should also be considered if that was a true trough level. Given his advancing age and likely immunosenescence, his risk of rejection is low. Therefore, using conventional immunosuppression targets will put him at elevated risk of infections unnecessarily. CMV infection is associated with a significantly increased relative risk of cardiovascular (CVS) disease in older KTRs, and this patient’s CVS risk factors, such as diabetes and hypertension, should be well-controlled. He should also be provided support to stop smoking.
References
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet (London, England). 2012;380:37–43.
Stevens PE, O’Donoghue DJ, de Lusignan S, et al. Chronic kidney disease management in the United Kingdom: NEOERICA project results. Kidney Int. 2007;72:92–9.
O'Neill WC. Structure, not just function. Kidney Int. 2014;85:503–5.
Bolignano D, Mattace-Raso F, Sijbrands EJ, Zoccali C. The aging kidney revisited: a systematic review. Ageing Res Rev. 2014;14:65–80.
Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29:496–507.
Poggio ED, Rule AD, Tanchanco R, et al. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int. 2009;75:1079–87.
Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288:2421–31.
Ruggenenti P, Perna A, Loriga G, et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365:939–46.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56.
Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
Poortvliet RK, de Ruijter W, de Craen AJ, et al. Blood pressure trends and mortality: the Leiden 85-plus Study. J Hypertens. 2013;31:63–70.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet (London, England). 1998;351:1755–62.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Agnelli G, Buller HR, Cohen A, et al. Apixaban for extended treatment of venous thromboembolism. N Engl J Med. 2013;368:699–708.
Hohnloser SH, Hijazi Z, Thomas L, et al. Efficacy of apixaban when compared with warfarin in relation to renal function in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2012;33:2821–30.
Alfaadhel TA, Soroka SD, Kiberd BA, Landry D, Moorhouse P, Tennankore KK. Frailty and mortality in dialysis: evaluation of a clinical frailty scale. Clin J Am Soc Nephrol. 2015;10:832–40.
Methven S, Steenkamp R, Fraser S. UK renal registry 19th annual report: chapter 5 survival and causes of death in UK adult patients on renal replacement therapy in 2015: national and centre-specific analyses. Nephron. 2017;137(suppl 1):117–50.
Kurella Tamura M, Desai M, Kapphahn KI, Thomas IC, Asch SM, Chertow GM. Dialysis versus medical management at different ages and levels of kidney function in veterans with advanced CKD. J Am Soc Nephrol. 2018;29:2169.
Oniscu GC, Brown H, Forsythe JL. How great is the survival advantage of transplantation over dialysis in elderly patients? Nephrol Dial Transplant. 2004;19:945–51.
Frei U, Noeldeke J, Machold-Fabrizii V, et al. Prospective age-matching in elderly kidney transplant recipients--a 5-year analysis of the Eurotransplant Senior Program. Am J Transplant. 2008;8:50–7.
Gill J, Bunnapradist S, Danovitch GM, Gjertson D, Gill JS, Cecka M. Outcomes of kidney transplantation from older living donors to older recipients. Am J Kidney Dis. 2008;52:541–52.
Falck P, Asberg A, Byberg KT, et al. Reduced elimination of cyclosporine A in elderly (>65 years) kidney transplant recipients. Transplantation. 2008;86:1379–83.
Johnson DW, Nicol DL, Purdie DM, et al. Is mycophenolate mofetil less safe than azathioprine in elderly renal transplant recipients? Transplantation. 2002;73:1158–63.
Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991;265:3255–64.
Margolis KL, O'Connor PJ, Morgan TM, et al. Outcomes of combined cardiovascular risk factor management strategies in type 2 diabetes: the ACCORD randomized trial. Diabetes Care. 2014;37:1721–8.
Patient Information and Guidelines
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chong, S.M.Y., Hung, R.K.Y., White, W. (2022). Ageing and the Kidneys. In: Harber, M. (eds) Primer on Nephrology. Springer, Cham. https://doi.org/10.1007/978-3-030-76419-7_45
Download citation
DOI: https://doi.org/10.1007/978-3-030-76419-7_45
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76418-0
Online ISBN: 978-3-030-76419-7
eBook Packages: MedicineMedicine (R0)