Abstract
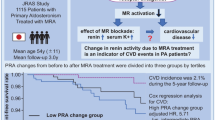
Patients with primary aldosteronism have an increased risk of developing cardiovascular disease. The response to mineralocorticoid receptor antagonists varies among individuals, indicating diverse mineralocorticoid receptor activities in these patients. This study explored the factors linked to the efficacy of blood pressure reduction through mineralocorticoid receptor antagonists in patients with primary aldosteronism. We examined the relationship between the reduction in blood pressure and patient characteristics in a group of 41 patients with primary aldosteronism (24 males, mean age 55 ± 13 years, including 34 patients diagnosed with bilateral primary aldosteronism) before and after undergoing treatment with mineralocorticoid receptor antagonists. Significant reductions in office blood pressure were observed 3 and 6 months after treatment initiation. Single correlation analyses showed that the urinary chloride-to-potassium ratio displayed the strongest positive association with blood pressure reduction, surpassing plasma aldosterone concentration, plasma renin activity, and urinary sodium-to-potassium ratio, at 3 and 6 months. Multiple correlation analyses revealed a consistent and independent positive correlation between the urinary chloride-to-potassium ratio and blood pressure reduction at 3 and 6 months. The optimal threshold for the urinary chloride-to-potassium ratio with respect to its ability to lower blood pressure, was determined as 3.18. These results imply that the urinary chloride-to-potassium ratio may be independently associated with the effectiveness of blood pressure reduction facilitated by mineralocorticoid receptor antagonists. Moreover, it could potentially serve as a valuable predictor of the effectiveness of these agents and function as an indicator of endogenous mineralocorticoid receptor activity in patients with primary aldosteronism.

Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is a prevalent form of secondary hypertension, that results from the autonomous overproduction of aldosterone due to adrenal gland lesions. It accounts for 5–10% of all hypertension cases [1,2,3]. Excess aldosterone not only induces hypertension but also leads to arteriosclerosis, kidney injury, cardiac fibrosis [4,5,6], diabetes mellitus, and metabolic syndrome [7,8,9,10] through the activation of mineralocorticoid receptors (MRs) in both epithelial and non-epithelial tissues. Patients with PA have a higher risk of developing cardiovascular disease and cerebrovascular events than those with essential hypertension [11,12,13,14,15].
Patients with unilateral PA are typically recommended to undergo laparoscopic adrenalectomy. Conversely, patients with bilateral adrenal hyperplasia or those unsuitable for surgery are advised to undergo preservation therapy, which includes treatment with MR antagonists (MRAs) [2, 16]. Furthermore, pharmacological MR blockade has been shown to have positive effects on both cardiovascular disease [17,18,19,20] and chronic kidney disease [21, 22].
MRAs have developed over time. They can be classified into two categories: steroidal (spironolactone and eplerenone) and non-steroidal (esaxerenone and finerenone) MRAs.
The extent of blood pressure (BP) reduction and organ protection achieved using MRAs varies among patients, suggesting individual differences in MR activity in patients with hypertension, including those with PA. Methods for predicting endogenous MR activity and, consequently, the degree of antihypertensive effects of MRAs have not yet been established. Therefore, in this study, we investigated the factors associated with the degree of BP reduction achieved with MRAs in patients with PA.
Methods
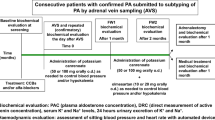
Participants
This study enrolled patients who visited the Department of Internal Medicine at the Tokyo Women’s Medical University Hospital between April 2014 and March 2023 for the treatment of PA. PA was diagnosed based on the diagnostic criteria outlined by the Japanese Society of Hypertension [23, 24]. All the patients included in this study were of Japanese descent. Informed consent was obtained using an opt-out method, and the procedures were approved by the Ethics Committee of Tokyo Women’s Medical University (Approval #: 2022-0081). Patients with secondary hypertension conditions other than PA, those with essential hypertension, or those who were administered MRAs before April 2014 were excluded from the study.
Background factors
We collected information concerning the patients’ sex, age, comorbidities, and use of antihypertensive agents. Body mass index (BMI), BP, pulse rate, urinary parameters, estimated daily salt intake, blood tests, and physiological function tests were performed before and after 3- and 6-month of treatment with MRAs.
Blood pressure and pulse rate
The BP and pulse rate were measured at our outpatient clinic, with the patient in a seated position after a resting period of at least 5 min, using an Omron HEM-907 monitor (Omron Healthcare, Kyoto, Japan). Only initial BP readings acquired during each visit were used in this study.
Urinary testing
Spot urine samples were collected, and the concentrations of creatinine (Cr), protein, sodium (Na), potassium (K), chloride (Cl), calcium (Ca), and phosphorus (P) were quantified at our clinical laboratory center using standardized laboratory evaluation methods. The excretion of proteins, Na, K, Cl, Ca, and P was assessed by dividing their concentrations by the Cr concentration. Furthermore, urinary Na/K and Cl/K ratios were calculated.
The estimated daily salt intake was calculated using the formula developed by Tanaka et al. [25]: (1) predicted value of 24-h urinary Cr excretion (mg/day) = body weight × 14.89 + height × 16.14 – age × 2.04 – 2244.45; (2) estimated 24-h urinary sodium excretion (mEq/day) = 21.98 × (spot urine Na/spot urine Cr/10 × predicted value of 24-h urinary Cr excretion)0.392 ; (3) estimated daily salt intake (g/day) = estimated 24-h urinary sodium excretion/17.
Blood testing
Albumin, Na, K, Cl, Cr, uric acid, aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transpeptidase (γ-GTP), lactate dehydrogenase (LDH), fasting blood glucose, hemoglobin A1c, high–density lipoprotein cholesterol (HDL), low–density lipoprotein cholesterol (LDL), triglycerides, and brain natriuretic peptide (BNP) were measured using standard laboratory methods at our clinical laboratory center. The estimated glomerular filtration rate (eGFR) was calculated using the following formula: eGFR (mL/min/1.73 m2) = 194 × creatinine−1.094 × age−0.287 (×0.739, if female) [26]. Plasma aldosterone concentration (PAC) and plasma renin activity (PRA) were measured using a radioimmunoassay at an external laboratory (SRL, Inc., Tokyo, Japan), and the aldosterone-renin ratio was calculated.
Body composition
Body fat mass and extracellular water-to-total body water ratio were measured by bioelectrical impedance analysis using an InBody 720 body composition analyzer (Biospace, Seoul, South Korea). Body fat percentage was evaluated by dividing body fat mass by body weight.
Statistical analysis
In this study, the MRAs used were exclusively spironolactone and esaxerenone. The dose of esaxerenone was converted to the equivalent spironolactone dose: 1.25 mg, 2.5 mg, 3.75 mg, and 5 mg of esaxerenone were converted to 25 mg, 50 mg, 75 mg, and 100 mg of spironolactone, respectively [27]. The BP-lowering effect of MRAs was defined as the decrease in systolic BP(ΔsBP) and diastolic BP(ΔdBP) divided by the spironolactone-equivalent dose of MRA at 3 months (ΔsBP 3 M and ΔdBP 3 M) and 6 months (ΔsBP 6 M and ΔdBP 6 M), respectively. Changes in parameters within the groups were analyzed using the paired t-test or Wilcoxon signed-rank test. Relationships between background factors and ΔsBP 3 M, ΔsBP 6 M, or urinary Cl/K were examined through single correlation analyses using Spearman’s rank correlation. Relationships between background factors and ΔsBP 3 M or ΔsBP 6 M were investigated using multiple correlation analyses. Backward and forward stepwise analysis with a threshold of P < 0.2 was applied to streamline the regression model, testing variables possibly associated with ΔsBP 3 M and ΔsBP 6 M, such as age, body fat percentage, urinary Cl/K or Na/K ratio, eGFR, HbA1c, PAC, and estimated daily salt intake. The selected variables were then subjected to linear regression analysis. To determine the cut-off value, receiver operating characteristic (ROC) curves and area under the curve (AUC) were examined. All data are expressed as the mean ± standard deviation or as the median value (interquartile range). The level of significance was set at P < 0.05. All statistical analyses were performed using JMP Pro, version 16 (SAS Institute Inc., Cary, NC, USA).
Results
Study disposition
This study enrolled 1357 patients diagnosed with PA and treated with MRAs (Fig. 1). Among them, 1315 patients were excluded due to loss to follow-up, change in MRA type, or modification of antihypertensive medication during the initial 3 months. Additionally, one patient was lost to follow-up in the subsequent 3 months. Finally, data from 41 patients were analyzed. Among them, 34 were diagnosed with bilateral PA using adrenal vein sampling.
Baseline characteristics
The baseline patient characteristics are shown in Table 1. Among all patients, 24 (59%) were male, with an average age of 55 ± 13 years and an average BMI of 25.1 ± 3.7 kg/m2. None of the patients were taking diuretics or steroids in addition to the MRAs. There were no alterations in the antihypertensive drug regimens except for MRAs.
The urinary Na/K ratio was 2.46 (1.34–3.76) and the urinary Cl/K ratio was 2.89 (1.86–3.89). The eGFR was 70.6 ± 12.9 (mL/min/1.73 m2), and none of the patients had an eGFR below 30 mL/min/1.73 m2. The hemoglobin A1c level was 5.7 (5.4–6.0) %, and the BNP level was 15.9 (9.5–30.3) pg/mL. PAC and PRA were 204 (156.5–233.5) pg/mL and 0.6 (0.3–0.9) ng/mL/h, respectively. The estimated daily salt intake was 9.0 ± 2.6 g/day.
Dose of MRAs
Of the 20 (49%) patients receiving spironolactone, 14 received 25 mg per day and 6 received 50 mg after the 3-month of treatment. After the 6-month of treatment, the doses were adjusted, with 10 patients administered with 25 mg, eight with 50 mg, one with 75 mg, and one with 100 mg of spironolactone. For the 21 (51%) patients receiving esaxerenone, 14 were administered with 1.25 mg, 6 with 2.5 mg, one with 3.75 mg, and two with 5 mg after the 3-month treatment. Following the 6-month treatment, the distribution was as follows: 11 patients received 1.25 mg, three received 2.5 mg, one received 3.75 mg, and six received 5 mg of esaxerenone.
Changes in parameters by MRA treatment
Blood pressure
Systolic BP significantly decreased from 140 ± 18 mmHg to 135 ± 14 mmHg (P < 0.05) at 3 months and to 128 ± 15 mmHg (P < 0.0001) at 6 months after MRA treatment initiation (Table 1). Diastolic BP also significantly decreased from 85 ± 12 mmHg to 80 ± 11 mmHg (P < 0.005) at 3 months and to 78 ± 11 mmHg (P < 0.0001) at 6 months. The ΔsBP at 6 months (12.7 ± 17.3 mmHg) was significantly greater than at 3 months (5.7 ± 17.6 mmHg) (P < 0.005). Similarly, ΔdBP at 6 months (7.1 ± 9.9 mmHg) was significantly higher than at 3 months (4.4 ± 9.4 mmHg) (P < 0.05). ΔsBP 6 M (0.28 ± 0.46 mmHg/mg) was significantly greater than ΔsBP 3 M (0.12 ± 0.52 mmHg/mg) (P < 0.05). However, ΔdBP 3 M and ΔdBP 6 M did not show significant differences.
Urinary electrolytes
The urinary excretion of protein, Na, K, Cl, and P did not significantly change after the initiation of MRA treatment, whereas the urinary excretion of Ca significantly decreased at both 3 and 6 months (Table 1). The urinary Cl/K ratio, urinary Na/K ratio, and estimated daily salt intake did not change significantly during the study period.
Blood tests
Serum potassium levels increased at 3 and 6 months (Table 1). eGFR and BNP levels significantly decreased, whereas Cr and uric acid levels significantly increased at 3 and 6 months. Additionally, the PAC and PRA significantly increased at both 3 and 6 months.
Body composition
Body fat percentage significantly increased at 6 months but not at 3 months (Table 1). The extracellular water-to-total body water ratio significantly decreased at 3 and 6 months.
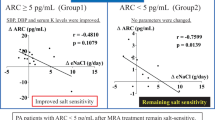
Single correlation analyses with ΔsBP 3 M and ΔsBP 6 M
In single correlation analyses with ΔSBP/MRA dose equivalent to spironolactone, urinary Na/K ratio and urinary Cl/K ratio before MRA treatment were significantly positively correlated with ΔsBP 3 M (P < 0.05). In addition, sex, urinary Na/K ratio, urinary Cl/K ratio, and HDL cholesterol before MRA treatment were significantly positively correlated with ΔsBP 6 M (P < 0.05) (Table 2 and Supplementary Fig. 1). Neither PAC nor PRA before MRA treatment showed significant correlations with ΔsBP 3 M and ΔsBP 6 M.
Multiple correlation analyses with ΔsBP 3 M and ΔsBP 6 M
Multiple regression analyses were conducted to assess the independence of background factors and to identify which factors were most significantly correlated with the BP-lowering effect. To assess the independence of background factors and to identify which factors are most significantly correlated with the BP-lowering effect, multiple regression analyses were conducted (Table 3a, b). In stepwise multiple correlation analyses that included age, body fat percentage, urinary Cl/K ratio, eGFR, hemoglobin A1c, PAC, and estimated daily salt intake before MRA treatment as independent variables, urinary Cl/K exhibited a significant positive correlation with ΔSBP at 3 and 6 months (Table 3a). In contrast, in the stepwise multiple correlation analyses that included age, body fat percentage, urinary Na/K ratio instead of urinary Cl/K ratio, eGFR, hemoglobin A1c, PAC, and estimated daily salt intake before MRA treatment as independent variables, the urinary Na/K ratio failed to show a significant correlation with sBP 3 M and sBP 6 M (Table 3b).
Cut-off values for predicting the ΔSBP 6 M based on the urinary Cl/K
To determine the cut-off value for predicting ΔsBP 6 M based on the urinary Cl/K ratio before MRA treatment, ROC curve analysis was performed. The analysis revealed a sensitivity of 0.72 and a specificity of 0.78. The AUC was 0.75, and the optimal cut-off value for the urinary Cl/K ratio was 3.18 (p = 0.026) in the ROC curve (Fig. 2).
Single correlation analysis between background factors and urinary Cl/K
To identify background factors associated with the urinary Cl/K ratio, single correlation analyses were conducted. The analyses revealed a significant and positive correlation between systolic BP and the urinary Cl/K ratio before MRA treatment (P = 0.010), while there were no significant correlations observed with diastolic BP or pulse rate (Table 4). Moreover, urinary excretions of Na, Cl, Ca, P, and the Na/K ratio were significantly and positively correlated, whereas serum Cr, PAC, and PRA were significantly and negatively correlated with the urinary Cl/K ratio before MRA treatment (P < 0.05) (Table 4). Furthermore, the estimated daily salt intake (P < 0.0001), body fat percentage (P < 0.05), and extracellular water/total body water ratio (P < 0.05), were significantly and positively correlated with the urinary Cl/K ratio.
Discussion
This study revealed five key aspects. First, the administration of MRAs resulted in BP reduction, with a more pronounced reduction per MRA dose observed at 6 months than at 3 months. Second, in single correlation analyses, the urinary Cl/K ratio exhibited the strongest positive correlation with the degree of BP reduction compared with other factors such as PAC, PRA, and urinary Na/K ratio at both 3 and 6 months. Third, in the multiple correlation analyses, the urinary Cl/K ratio showed a significant positive correlation with BP reduction at both 3 and 6 months, independent of other factors. Fourth, the optimal cut-off point of the Cl/K ratio for the BP-lowering effect was identified as 3.18. Additionally, the urinary Cl/K ratio showed a significant positive correlation with the baseline systolic BP levels and estimated daily salt intake. These findings suggest that the urinary Cl/K ratio might be independently related to the BP-lowering effect of MRAs and could serve as a valuable predictor of MRA efficacy in lowering BP (cut-off value of urinary Cl/K ratio: 3.18) and, consequently, as an indicator of endogenous MR activity in patients with PA.
MR activation by salt load through the aldosterone-independent Rac1 pathway
MRAs have proven effective in treating hypertension with elevated PAC; however, they are also effective in treating hypertension with normal PAC, known as MR-associated hypertension, a form of salt-sensitive hypertension [28, 29]. PA, which is characterized by elevated PAC, is a typical form of MR-associated hypertension. Additionally, it is independently activated by the small guanosine triphosphatase (GTPase) Ras-related C3 botulinum toxin substrate 1 (Rac1) [30], which is triggered by various factors such as high salt intake [31], cytokines [32], mechanical stress [33], and oxidative stress [34]. The activation of Rac1 during salt intake leads to enhanced nuclear translocation of MR [35, 36], amplifying MR activity, thereby contributing to the development of salt-sensitive hypertension and organ damage [31, 35].
Double-blind clinical trials illustrated the renal protective effects of MR antagonists; however, the effectiveness of these antagonists was found to be more closely associated with dietary salt intake than with aldosterone levels [37]. Notably, in this study, neither PAC nor PRA correlated with the degree of MRA-induced BP reduction (Table 2), indicating that they may not serve as reliable indicators of the degree of MR activation.
Stronger correlation of BP reduction with urinary Cl/K than urinary Na/K
The urinary Na/K ratio is commonly used as an indicator of salt load and demonstrates a closer association with BP than when urinary Na or K is analyzed alone [38, 39]. PA is a form of salt-sensitive hypertension that is greatly influenced by salt intake due to excessive aldosterone, which causes increased Na reabsorption and K excretion. Given these details, it was initially speculated that the urinary Na/K ratio might serve as an excellent indicator of the BP-lowering effects of MRA treatment. In this study, the urinary Na/K ratio displayed significant and positive correlations with ΔsBP 3 M and ΔsBP 6 M (Table 2). Additionally, the urinary Cl/K ratio revealed a significant and positive correlation with estimated salt intake (Table 4), along with significant and positive correlations with ΔsBP 3 M and ΔsBP 6 M (Table 2). Furthermore, it exhibited a stronger association with the BP-lowering effect of MRA treatment than with other indices such as the urinary Na/K ratio, PAC, and PRA (Table 3).
The exact mechanism underlying the relationship between urinary Cl/K ratio and the BP-lowering effect of MRA treatment remains unclear. However, reports have suggested an association between Cl and BP, as detailed below.
Activation of angiotensin-converting enzyme by Cl
In the renin-angiotensin-aldosterone system, angiotensinogen is processed by renin to form angiotensin I, which is then converted to angiotensin II by angiotensin-converting enzyme (ACE). Furthermore, angiotensin II is cleaved into angiotensin-(1-7) by ACE2. Angiotensin II has a hypertensive effect, whereas angiotensin-(1-7) has a hypotensive effect. Additionally, angiotensin II stimulates aldosterone secretion. Both ACE and ACE2 possess Cl-sensitive catalytic activities induced by the presence of chloride-binding sites, namely CL1 and CL2 for ACE and CL1 for ACE2. Cl binding induces subtle changes in the conformation of the active sites, thereby facilitating or hindering substrate binding. Studies have shown that chloride activates ACE [40,41,42]. Moreover, elevating Cl levels beyond 100 mM in human plasma inhibits ACE2 activity, increasing angiotensin II [41]. The serum Cl level in our study participants was 105 ± 2 mEq/L (Table 1), a value within the normal range. Nevertheless, it attains a level noteworthy for its potential to impede ACE2 activity, consequently eliciting an elevation in angiotensin II levels. Therefore, slightly increased serum Cl might have elevated angiotensin II levels, resulting in, a subtle increase in aldosterone concentration in our patients. These findings support our hypothesis that urinary Cl/K is associated with the antihypertensive effects of MRA through the action of chloride on ACE and ACE2. Further studies are required to validate this hypothesis.
Stronger associations of chloride intake with high BP than sodium intake
Dahl salt-sensitive rats developed hypertension when exposed to high NaCl concentrations; however, not when exposed to the same amount of Na in the form of sodium bicarbonate or other non-Cl salts of Na [43, 44]. Similar results were observed in a deoxycorticosterone acetate (DOCA) salt-sensitive hypertension model, where the BP in rats administered NaCl was significantly higher than that in rats administred sodium bicarbonate and/or sodium ascorbate [45]. Additionally, in most human populations, Na is almost always consumed as a Cl salt, and Na ions do not impact BP when Cl is substituted with another anion, such as sulfate or bicarbonate [46,47,48]. These observations suggest that it is not the Na ion but the Cl ion in the salt composition that affects the increase in BP.
BP regulated by Cl at the macula densa
The macula densa, a region in the renal juxtaglomerular apparatus, relies on Cl levels in the distal tubular fluid, rather than Na levels, to sense salt and volume status [49]. High Cl levels activate the tubule-glomerular feedback mechanism, leading to renal vasoconstriction and a decrease in the GFR [50, 51]. Consequently, the delivery of Cl to the macula densa in animals administered with Cl is believed to result in an increase in renal afferent arteriolar resistance, a decrease in renal blood flow and GFR, and an elevation in BP [52]. Therefore, it is possible that urinary Cl, rather than Na, increases BP via its action on the macula densa.
Association between MR and adipose tissue
It has been reported that excessive expression of MR in adipocytes increases body weight and fat mass in mice [53]. Eplerenone treatment has been shown to reduce the number of hypertrophic adipocytes in the adipose tissue of obese mice [54]. In contrast to these experimental findings, our data revealed a significant increase in body fat percentage at 6 months with MRA treatment, although BMI did not change significantly in patients with PA. Treatment with eplerenone did not result in changes in body weight, liver fat, visceral fat, and subcutaneous fat in patients with type 2 diabetes [55]. Similarly, treatment with spironolactone did not affect body weight and metabolic parameters in obese subjects [56]. The differences observed in these research outcomes may be reflective of variations in research design and study participants. Currently, the impact of MRA on obesity-related factors remains unclear. Further investigation is needed to explore the association between MR stimulation and the development of obesity.
Limitations
The present study has several limitations. First, the sample size was relatively small and this was a single-center study with subjects from a single ethnic population (Japanese). Second, this was a retrospective study, and meal quantities, including salt intake, were not standardized. Third, the MRAs used were limited to spironolactone and esaxerenone. Fourth, most subjects in this study were already on antihypertensive agents before MRA treatment, and their BP levels were not markedly elevated at baseline. Among the 41 subjects, 34 had bilateral PA. Consequently, since serum K levels were not low in these cases, there exists a potential for bias in the participant selection process. These findings may not be applicable to other MRAs, such as eplerenone. Future prospective studies with larger-scale clinical experiments are required to address these issues.
Conclusion
This study demonstrated that urinary Cl/K levels were significantly positively correlated with estimated daily salt intake. Moreover, the urinary Cl/K ratio, but not the PAC or PRA, was associated with the degree of BP reduction caused by MRA treatment. It is plausible that the association between urinary Cl/K ratios and BP reduction by MRA treatment may, at least in part, involve the activation of MRs mediated by salt-induced Rac1, activation of ACE, and inhibition of ACE2 by Cl, independent of Na. These findings suggest that urinary Cl/K levels could serve as predictors of the BP-lowering effects of MRAs, and consequently, as indicators of endogenous MR activity in patients with PA. Future studies are required to determine whether these findings apply to other types of hypertension, including essential hypertension.
References
Rossi GP, Bernini G, Desideri G, Fabris B, Ferri C, Giacchetti G, et al. Renal damage in primary aldosteronism: results of the PAPY Study. Hypertension. 2006;48:232–8.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol. 2017;69:1811–20.
Rossi GP, Sechi LA, Giacchetti G, Ronconi V, Strazzullo P, Funder JW. Primary aldosteronism: cardiovascular, renal and metabolic implications. Trends Endocrinol Metab. 2008;19:88–90.
Monticone S, Sconfienza E, D’Ascenzo F, Buffolo F, Satoh F, Sechi LA, et al. Renal damage in primary aldosteronism: a systematic review and meta-analysis. J Hypertens. 2020;38:3–12.
Chen YL, Chen CH, Xu TY, Xu JZ, Zhu LM, Li Y, Wang JG. Non-invasive left ventricular pressure-strain loop study on cardiac fibrosis in primary aldosteronism: a comparative study with cardiac magnetic resonance imaging. Hypertens Res. 2024;47:445–54.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, Mulatero P. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Akehi Y, Yanase T, Motonaga R, Umakoshi H, Tsuiki M, Takeda Y, et al. High Prevalence of Diabetes in Patients With Primary Aldosteronism (PA) Associated With Subclinical Hypercortisolism and Prediabetes More Prevalent in Bilateral Than Unilateral PA: A Large, Multicenter Cohort Study in Japan. Diabetes Care. 2019;42:938–45.
Huang WC, Chen YY, Yang SY, Lai CF, Lai TS, Chen HY, et al. Fat mass as an important predictor of persistent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res. 2023;46:1375–84.
Haze T, Ozawa M, Kawano R, Haruna A, Ohki Y, Suzuki S, et al. Effect of the interaction between the visceral-to-subcutaneous fat ratio and aldosterone on cardiac function in patients with primary aldosteronism. Hypertens Res. 2023;46:1132–44.
Born-Frontsberg E, Reincke M, Rump LC, Hahner S, Diederich S, Lorenz R, et al. Cardiovascular and cerebrovascular comorbidities of hypokalemic and normokalemic primary aldosteronism: results of the German Conn’s Registry. J Clin Endocrinol Metab. 2009;94:1125–30.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62:331–6.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of Cardiovascular Disease and Its Risk Factors in Primary Aldosteronism: A Multicenter Study in Japan. Hypertension. 2018;71:530–7.
Nomura M, Kurihara I, Itoh H, Ichijo T, Katabami T, Tsuiki M, et al. Association of cardiovascular disease risk and changes in renin levels by mineralocorticoid receptor antagonists in patients with primary aldosteronism. Hypertens Res. 2022;45:1476–85.
Lee BC, Tsai HH, Chen ZW, Chang CC, Huang JZ, Chang YY, et al. Aldosteronism is associated with more severe cerebral small vessel disease in hypertensive intracerebral hemorrhage. Hypertens Res. 2024;47:608–17.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Wei J, Ni J, Huang D, Chen M, Yan S, Peng Y. The effect of aldosterone antagonists for ventricular arrhythmia: a meta-analysis. Clin Cardiol. 2010;33:572–7.
Simopoulos V, Tagarakis G, Hatziefthimiou A, Skoularigis I, Triposkiadis F, Trantou V, et al. Effectiveness of aldosterone antagonists for preventing atrial fibrillation after cardiac surgery in patients with systolic heart failure: a retrospective study. Clin Res Cardiol. 2015;104:31–7.
Chung YW, Yang YH, Wu CK, Yu CC, Juang JM, Wang YC, et al. Spironolactone is associated with reduced risk of new-onset atrial fibrillation in patients receiving renal replacement therapy. Int J Cardiol. 2016;202:962–6.
Beygui F, Labbé JP, Cayla G, Ennezat PV, Motreff P, Roubille F, et al. Early mineralocorticoid receptor blockade in primary percutaneous coronary intervention for ST-elevation myocardial infarction is associated with a reduction of life-threatening ventricular arrhythmia. Int J Cardiol. 2013;167:73–9.
Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. Aldosterone antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst Rev. 2014;4:Cd007004.
Currie G, Taylor AH, Fujita T, Ohtsu H, Lindhardt M, Rossing P, et al. Effect of mineralocorticoid receptor antagonists on proteinuria and progression of chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. 2016;17:127.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Ito S, Itoh H, Rakugi H, Okuda Y, Yoshimura M, Yamakawa S. Double-Blind Randomized Phase 3 Study Comparing Esaxerenone (CS-3150) and Eplerenone in Patients With Essential Hypertension (ESAX-HTN Study). Hypertension. 2020;75:51–8.
Shibata H, Itoh H. Mineralocorticoid receptor-associated hypertension and its organ damage: clinical relevance for resistant hypertension. Am J Hypertens. 2012;25:514–23.
Yoshida Y, Fujiki R, Kinoshita M, Sada K, Miyamoto S, Ozeki Y, et al. Importance of dietary salt restriction for patients with primary aldosteronism during treatment with mineralocorticoid receptor antagonists: The potential importance of post-treatment plasma renin levels. Hypertens Res. 2023;46:100–7.
Ando K, Fujita T. Pathophysiology of salt sensitivity hypertension. Ann Med. 2012;44:S119–26.
Shibata S, Mu S, Kawarazaki H, Muraoka K, Ishizawa K, Yoshida S, et al. Rac1 GTPase in rodent kidneys is essential for salt-sensitive hypertension via a mineralocorticoid receptor-dependent pathway. J Clin Invest. 2011;121:3233–43.
Uddin S, Lekmine F, Sharma N, Majchrzak B, Mayer I, Young PR, et al. The Rac1/p38 mitogen-activated protein kinase pathway is required for interferon alpha-dependent transcriptional activation but not serine phosphorylation of Stat proteins. J Biol Chem. 2000;275:27634–40.
Gao G, Shen N, Jiang X, Sun H, Xu N, Zhou D, et al. Periodic mechanical stress activates EGFR-dependent Rac1 mitogenic signals in rat nucleus pulpous cells via ERK1/2. Biochem Biophys Res Commun. 2016;469:723–30.
Nagase M, Ayuzawa N, Kawarazaki W, Ishizawa K, Ueda K, Yoshida S, Fujita T. Oxidative stress causes mineralocorticoid receptor activation in rat cardiomyocytes: role of small GTPase Rac1. Hypertension. 2012;59:500–6.
Shibata S, Nagase M, Yoshida S, Kawarazaki W, Kurihara H, Tanaka H, et al. Modification of mineralocorticoid receptor function by Rac1 GTPase: implication in proteinuric kidney disease. Nat Med. 2008;14:1370–6.
Shibata S, Ishizawa K, Uchida S. Mineralocorticoid receptor as a therapeutic target in chronic kidney disease and hypertension. Hypertens Res. 2017;40:221–5.
Ando K, Ohtsu H, Uchida S, Kaname S, Arakawa Y, Fujita T, Group ES. Anti-albuminuric effect of the aldosterone blocker eplerenone in non-diabetic hypertensive patients with albuminuria: a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2014;2:944–53.
Tabara Y, Takahashi Y, Kumagai K, Setoh K, Kawaguchi T, Takahashi M, et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–13.
Higo Y, Nagashima S, Tabara Y, Setoh K, Kawaguchi T, Takahashi Y, et al. Association of the spot urine sodium-to-potassium ratio with blood pressure is independent of urinary Na and K levels: The Nagahama study. Hypertens Res. 2019;42:1624–30.
Kato H, Taguchi T, Okuda H, Kondo M, Takara M. Antihypertensive effect of chitosan in rats and humans. Journal of Traditional Medicine. 1994;11:198–205.
Rushworth CA, Guy JL, Turner AJ. Residues affecting the chloride regulation and substrate selectivity of the angiotensin-converting enzymes (ACE and ACE2) identified by site-directed mutagenesis. FEBS J. 2008;275:6033–42.
Masuyer G, Yates CJ, Sturrock ED, Acharya KR. Angiotensin-I converting enzyme (ACE): structure, biological roles, and molecular basis for chloride ion dependence. Biol Chem. 2014;395:1135–49.
Kotchen TA, Galla JH, Luke RG. Failure of NaHCO3 and KHCO3 to inhibit renin in the rat. Am J Physiol. 1976;231:1050–6.
Kotchen TA, Luke RG, Ott CE, Galla JH, Whitescarver S. Effect of chloride on renin and blood pressure responses to sodium chloride. Ann Intern Med. 1983;98:817–22.
Kurtz TW, Morris RC Jr. Dietary chloride as a determinant of “sodium-dependent” hypertension. Science. 1983;222:1139–41.
Kurtz TW, Al-Bander HA, Morris RC Jr. “Salt-sensitive” essential hypertension in men. Is the sodium ion alone important? N Engl J Med. 1987;317:1043–8.
Luft FC, Zemel MB, Sowers JA, Fineberg NS, Weinberger MH. Sodium bicarbonate and sodium chloride: effects on blood pressure and electrolyte homeostasis in normal and hypertensive man. J Hypertens. 1990;8:663–70.
Schorr U, Distler A, Sharma AM. Effect of sodium chloride- and sodium bicarbonate-rich mineral water on blood pressure and metabolic parameters in elderly normotensive individuals: a randomized double-blind crossover trial. J Hypertens. 1996;14:131–5.
Rivera FB, Alfonso P, Golbin JM, Lo K, Lerma E, Volgman AS, Kazory A. The Role of Serum Chloride in Acute and Chronic Heart Failure: A Narrative Review. Cardiorenal Med. 2021;11:87–98.
Schmidlin O, Tanaka M, Bollen AW, Yi SL, Morris RC Jr. Chloride-dominant salt sensitivity in the stroke-prone spontaneously hypertensive rat. Hypertension. 2005;45:867–73.
Schmidlin O, Tanaka M, Sebastian A, Morris RC Jr. Selective chloride loading is pressor in the stroke-prone spontaneously hypertensive rat despite hydrochlorothiazide-induced natriuresis. J Hypertens. 2010;28:87–94.
McCallum L, Lip S, Padmanabhan S. The hidden hand of chloride in hypertension. Pflugers Arch. 2015;467:595–603.
Urbanet R, Nguyen Dinh Cat A, Feraco A, Venteclef N, El Mogrhabi S, Sierra-Ramos C, et al. Adipocyte Mineralocorticoid Receptor Activation Leads to Metabolic Syndrome and Induction of Prostaglandin D2 Synthase. Hypertension. 2015;66:149–57.
Hirata A, Maeda N, Hiuge A, Hibuse T, Fujita K, Okada T, et al. Blockade of mineralocorticoid receptor reverses adipocyte dysfunction and insulin resistance in obese mice. Cardiovasc Res. 2009;84:164–72.
Johansen ML, Schou M, Rossignol P, Holm MR, Rasmussen J, Brandt N, et al. Effect of the mineralocorticoid receptor antagonist eplerenone on liver fat and metabolism in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial (MIRAD trial). Diabetes Obes Metab. 2019;21:2305–14.
Garg R, Kneen L, Williams GH, Adler GK. Effect of mineralocorticoid receptor antagonist on insulin resistance and endothelial function in obese subjects. Diabetes Obes Metab. 2014;16:268–72.
Acknowledgements
We express our gratitude to the physicians and medical staff in our department who provided care to the patients enrolled in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SM and AI received honorariums as a lecture fee from Daiichi Sankyo Company Limited.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ikemoto, M., Morimoto, S. & Ichihara, A. Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism. Hypertens Res 47, 1707–1718 (2024). https://doi.org/10.1038/s41440-024-01651-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-024-01651-5
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Urinary chloride-to-potassium ratio as a potential novel index for MR activity in patients with hypertension
Hypertension Research (2024)