Abstract
We measured dietary salt intake in 26 patients with primary aldosteronism treated with mineralocorticoid receptor antagonists and evaluated whether plasma renin levels were affected by dietary salt intake pre-treatment and post 6 months of mineralocorticoid receptor antagonist treatment. The dietary salt intake level was calculated using spot urine sodium and creatinine concentrations, body weight, height, and age. The clinical parameters pre- and post- treatment were compared. The systolic and diastolic blood pressure levels decreased, and the serum potassium and active renin concentration increased significantly. Although the dietary salt intake did not change after treatment, the differences in dietary salt intake and active renin concentration pre- and post- treatment were inversely correlated (r = –0.418, p = 0.03). The 26 patients were divided into two groups with active renin concentration levels ≥5 pg/mL (Group 1) and <5 pg/mL (Group 2) after treatment. The Group parameters did not differ pre- and post- treatment. Group 1 evidenced improvements in systolic and diastolic blood pressures, and the potassium level and active renin concentration over time; Group 2 did not. Group 1 evidenced no significant correlation between the differences in dietary salt intake and active renin concentration levels (r = –0.481, p = 0.11) but Group 2 showed a strong inverse correlation (r = –0.7599, p = 0.01). In conclusion, we found that an active renin concentration level <5 pg/mL post-mineralocorticoid receptor antagonist treatment may indicate that salt sensitivity has not adequately improved, emphasizing the importance of measuring plasma renin levels after such treatment.
Similar content being viewed by others
Introduction
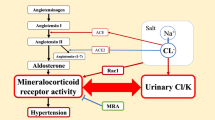
Primary aldosteronism (PA), a common form of secondary hypertension accounting for 5–13% of all hypertension [1,2,3], is associated with a high prevalence of cerebrocardiovascular events [4, 5]. PA is caused by excessive aldosterone (Ald) secretion from the adrenal glands; Ald suppresses the action of renin secreted by the kidneys. The treatment strategy depends on the PA subtype. Mineralocorticoid receptor antagonists (MRAs) are recommended for patients with bilateral PA [3, 6]. This attenuates the effects of excess Ald by inhibiting the binding of Ald to the MR, increasing the renin level. Hundemer et al. [7] reported that PA patients with plasma renin activities of at least 1 ng/mL/h receiving MRA therapy experienced fewer cardiovascular events (comparable to those of subjects with essential hypertension) independent of blood pressure (BP) control.
Salt intake affects BP. Tanaka et al. [8] reported that urine sodium (Na) and creatinine concentrations, height, weight, and age could be used to estimate dietary salt intake (eNaCl). Japanese Society of Hypertension Treatment Guidelines (2019) recommend that the Tanaka method should be used to monitor salt intake [9]. It is generally believed that salt restriction increases renin secretion by reducing the circulating plasma volume and urinary chloride concentration [10,11,12,13,14]. Hundemer et al. [7] did not seek a correlation between salt intake and renin levels when assessing renin status in PA patients on MRA therapy. To the best of our knowledge, no report has yet evaluated salt intake in detail and the effect thereof on the renin-angiotensin system during MRA treatment. We here examined the effect of salt intake on renin levels and BP; we measured the eNaCl in PA patients treated with MRAs to determine whether plasma renin levels were informative even during treatment.
Methods
Subjects
We enrolled 30 patients admitted to Oita University Hospital from September 2019 to December 2020 for treatment of PA; all received MRAs. Two who lacked eNaCl measurements at diagnosis and 6 months after commencing MRAs, one who developed a psychosis, and one with unilateral PA, were excluded; we finally analyzed 26 patients. Of these, 19 were diagnosed with bilateral PA via adrenal vein sampling (AVS). Seven did not undergo AVS or failed catheter insertion, but none evidenced hypokalemia; bilateral PA was thus suspected. All 26 patients visited our hospital at 1, 3, and 6 months after MRA commencement; at the 1- and 3-month visits, they were told to limit salt intake by the same physician (YY) based on their eNaCl measurements. After 6 months of MRA treatment, BP, serum levels of potassium (K), the active renin concentration (ARC), Ald, and eNaCl were assessed. Groups 1 and 2 evidenced ARC ≥ 5 pg/mL and <5 pg/mL, respectively (Fig. 1).
Laboratory tests
Serum Ald concentrations were measured using a Chemiluminescent Enzyme Immunoassay (CLEIA) Accuraseed Aldosterone Kit (Fujifilm Wako Pure Chemical Corp., Osaka, Japan). ARC were assayed employing a CLEIA Accuraseed Renin Kit (Fujifilm Wako Pure Chemical Corp.).
PA diagnosis
PA was diagnosed by reference to the Hypertension Treatment Guidelines of the Japanese Society of Hypertension (2019) [9]. The screening test included ARC and Ald measurements. The test was positive when the Ald/ARC ratio (ARR) was >40. A saline infusion test (SIT), captopril challenge test (CCT), and oral salt loading test (OSLT) served as confirmatory tests. The SIT featured an intravenous infusion of 2 L of saline over 4 h with the patient supine. An Ald ≥ 60 pg/mL after such loading was considered to be a positive result. The CCT featured administration of a 50-mg captopril tablet; blood was drawn after 90 min. When the ARR was >40, the test was considered positive. The OSLT featured analysis of 24-h urine pools after consumption of a high-salt diet. The test was considered positive when the 24-h urinary Ald and Na excretion levels were ≥8 μg/day and ≥170 mEq/day, respectively. When the urine Na level was <170 mEq/day, the data were excluded because NaCl loading had been inadequate. Antihypertensive drugs that affect the renin-angiotensin system, thus angiotensin-converting-enzyme inhibitors (ACE-Is), angiotensin II receptor blockers (ARBs), beta-adrenergic blockers, diuretics, and MRAs, were discontinued at the time of the confirmatory test.
AVS
AVS was performed to localize PA as described by Japan Endocrine Society Guidelines for the Treatment of Primary Aldosteronism (2021) [6]; successful catheter insertion was confirmed when the cortisol level after adrenocorticotropic hormone loading was five-fold higher than that in peripheral blood.
Antihypertensive drugs
Patients diagnosed with PA who received oral MRA therapy were given spironolactone or esaxerenone; if the BP fell excessively after starting MRAs, the doses of other hypertensive drugs (e.g., calcium channel blockers [CCBs]) were reduced. MRA levels were increased or decreased as needed while monitoring BP, serum K levels, and the ARC, but were not discontinued.
BP measurement
Pre-treatment BP was measured after hospitalization and bed rest. All other BP measurements to 6 months of treatment were the averages of three measurements taken at home.
eNaCl
The eNaCl was measured using the formula of Tanaka et al. [8] using spot urine specimens taken at any time (JSH 2019 [9]), thus: eNaCl (g/day) 24-h urinary sodium excretion/17, [24-h urinary sodium excretion (mmol/day)] = 21.98 × {urinary sodium (mmol/L)/[urinary creatinine (mg/dL) × 10] × predicted 24-h urinary creatinine excretion}0.392. The predicted 24-h urinary creatinine excretion (mg/day) = body weight (kg) × 14.89 + height (cm) × 16.14–age × 2.043–2244.45.
Statistical analysis
Data are expressed as medians [first to third quartiles]. The Wilcoxon signed-rank test was used to compare the Groups. The t-test was employed when the data were normally distributed and the Mann-Whitney U test otherwise. A p-value < 0.05 was considered significant. Sex proportions were compared with the aid of the chi-squared test, and correlations were sought using Spearman rank correlation coefficients. All analyses were performed with the aid of Prism ver. 7 software.
Results
Parameter changes in PA patients on MRAs
The 26 patients included 12 males and 14 females of mean age 51.5 years [48.0–61.5]. Three patients received spironolactone (25 mg daily) and 23 esaxerenone (22 received 2.5 mg and 1 received 5 mg daily). No patient was taking an ACE-I or ARB, beta-adrenergic blocker, or diuretic before or during MRA treatment. Eighteen patients received a CCB before an MRA, and three discontinued the CCB 6 months after MRA treatment. All 26 patients were compared before and 6 months after MRA treatment. The systolic BP (SBP) (138 mmHg [124.5–157.5] vs. 125 mmHg [117.8–130.8], p = 0.003) and diastolic BP (DBP) (86 mmHg [80.5–95.0] vs. 78 mmHg [74.5–86.3], p = 0.016) decreased, while the serum K level (3.9 mmol/L [3.8–4.3] vs. 4.3 mmol/L [4.0–4.6], p < 0.001) increased and the ARC (2.6 pg/mL [1.2–3.8] vs. 6.1 pg/mL [3.5–10.3], p < 0.001) increased significantly. However, the eNaCl (8.9 g/day [8.0–10.2] vs. 10.0 g/day [7.8–12.0], p = 0.272) did not change (Table 1).
Comparison of PA patients divided by ARC ≥ 5 and < 5 pg/mL after MRA treatment
All patients were divided into two groups after 6 months of MRA treatment: ARC ≥ 5 pg/mL (Group 1, N = 16) and ARC < 5 pg/mL (Group 2, N = 10) (Table 2). The pre-MRA and 6 months post-MRA parameters were compared. Before treatment, the two groups differed significantly in terms of only age (54.5 years [49.0–65.8] vs. 49.5 years [42.3–54.3], p = 0.023). After 6 months of MRA treatment, the ARC (8.9 pg/mL [6.3–11.3] vs 3.4 [2.8–4.0], p < 0.001) and the ARR (20 [14.0–33.7] vs. 55.7 [46.4–69.1], p < 0.001) differed significantly. Group 1 evidenced significant decreases in SBP (144 mmHg [129.5–158.5] vs. 123 mmHg [114.0–128.0], p = 0.002), DBP (86 mmHg [81.5–94.8] vs. 78 mmHg [71.3–81.8], p = 0.007) and the ARR (73.1 [45.0–102.1] vs. 20.0 [14.0–33.7], p < 0.001), and significant increases in the K level (3.9 mmol/L [3.7–4.1] vs. 4.4 mmol/L [4.1–4.6], p = 0.003) and ARC (2.5 pg/mL [1.4–3.1] vs. 8.9 pg/mL [6.3–11.3], p < 0.001). Group 2 evidenced no significant change in any parameter. Before MRA treatment, 12 patients in Group 1 and 6 in Group 2 were taking CCBs. After treatment, 11 patients in Group 1 and 4 in Group 2 were taking CCBs. In terms of oral MRAs, there was no difference between the two Groups. In Group 1, three patients received 25 mg of spironolactone daily and 13 received 2.5 mg of esaxerenone; in Group 2, nine patients were on 2.5 mg of esaxerenone and one on 5 mg of esaxerenone.
Correlations between the eNaCl and ARC changes before and after 6 months of MRAs
The differences in the eNaCl values and ARC before and 6 months after MRA treatment are abbreviated ΔeNaCl and ΔARC, respectively. The correlation between these values for all 26 cases was r = –0.418 (p = 0.0279), thus negative (Fig. 2a). Correlations were also derived separately for Groups 1 and 2; the figures were r = –0.481 (p = 0.1079) (Fig. 2b) and r = –0.7599 (p = 0.0139, thus strongly negative) (Fig. 2c), respectively.
Discussion
The eNaCl changes were inversely correlated with ARC variations in PA patients on MRAs. In particular, strong inverse correlations were observed in patients with post-MRA treatment ARC < 5 pg/mL. Patients with ARC < 5 pg/mL at that time evidenced no changes in BP or serum K level. This emphasizes the significance of post-MRA plasma renin levels; PA patients who failed to achieve ARC ≥ 5 pg/mL after MRA treatment remain salt-sensitive, probably because MR activation is inadequately suppressed.
First, is it useful to measure dietary salt intake in spot urine samples during MRA treatment? Ald binds to and activates the MR, in turn increasing urinary Na reabsorption by enhancing the activities of epithelial Na channels (ENaCs) in the principal cells of the kidney collecting tubules [15, 16]. Na re-absorption creates a lumen-negative electrical gradient that activates the basement membrane Na+-K+ ATPase, increasing K excretion from blood. In PA patients, excess Ald overactivates ENaCs, increasing urinary Na reabsorption and K excretion [17, 18]. MRAs inhibit urinary Na reabsorption by blocking MR activation by Ald. Rose et al. [18] reported that MRAs exhibited weak natriuretic activities; the maximum Na excretion in patients on MRAs is only 1–2% of the glomerular filtered Na volume. In contrast, loop diuretics trigger excretion of 20–25% of the glomerular filtered Na volume [18, 19]; the figure for thiazide diuretics is 3–5% [17, 18]. The natriuretic effects of MRAs are thus very weak. We compared changes in urinary Na excretion before and after MRA administration in the same patients; we did not average the data. We found it useful to measure changes in urinary Na excretion in PA patients on MRAs.
Second, this is the first study to examine the relationship between eNaCl and renin levels in PA patients on MRAs. Those with ARC < 5 pg/mL after MRA treatment (Group 2) evidenced an inverse correlation between the ΔeNaCl and ΔARC pre- and post-MRA treatment (Fig. 2c). Renin secretion is reduced by: (1) increased intravascular pressure in the afferent arterioles [10], (2) increased cardiac and intravascular pressures that activate the sympathetic nervous system and stimulate beta 1-adrenergic receptors [13, 14], and (3) increased chloride concentrations in the macula densa cells of the distal tubules [11, 12]. As described above, increased salt intake in normal subjects decreases renin secretion because of the rises in circulating plasma volume and chloride concentration in the distal tubules. In patients with PA, renin secretion is reduced because of increased Na reabsorption from the collecting ducts and increasing of circulating plasma volume by excess Ald. Thus, PA is a salt-sensitive form of hypertension that is strongly influenced by salt intake; adequate suppression of MR activation via both dietary salt restriction and MRAs is important. PA patients treated with MRAs exhibited decreased Na reabsorption from the collecting ducts and increased renin secretion (this had formerly been suppressed). No previous study has examined the relationship between salt intake and renin level in PA patients on MRAs. Only a few studies measured renin levels after MRA treatment. Fountoulakis et al. [20] found a relationship between salt restriction and changes in serum K levels in PA patients on MRAs, but did not seek a correlation between salt restriction and renin secretion. Hundemer et al. [7] found that MRAs reduced the incidence of cardiovascular events to the level of essential hypertension in patients with plasma renin activity levels (PRAs) ≥1 ng/mL/h, but not in those with PRAs <1 ng/mL/h. It was suggested that adequate MR inhibition by MRAs improved not only BP but also exerted direct effects on various organs, reducing myocardial fibrosis, left ventricular hypertrophy, and nephropathy [21,22,23,24]. A PRA ≥ 1 ng/mL/h is equivalent to an ARC ≥ 5 pg/mL [9]; thus, we divided the patients into two Groups (1 and 2) by whether an ARC ≥ 5 pg/mL was or was not (respectively) achieved after MRA treatment. Group 1 evidenced adequate suppression of MR activation; there was no correlation between the ΔeNaCl and ΔARC. In contrast, a strong negative correlation was observed in Group 2, suggesting inadequate inhibition of MR activation and thus persistent salt sensitivity. Apart from excessive salt intake, possible causes of hyporeninemia include an inadequate MRA dose, decreased renal function, advanced age, and sex. We found no difference in MRA dose or renal function between Groups 1 and 2, but Group 1 was older than Group 2; age-related hyporeninemia was not in play. In women, changes in renin levels over the sex hormone cycle should be considered [25, 26]. Although we did not do this, it is unlikely that renin levels were affected by sex because the proportions of women in Groups 1 and 2 were the same. Thus, PA patients who did not achieve ARC ≥ 5 pg/mL after MRA treatment either ingested excessive salt or lacked an adequate MRA dose. Our results comparing the two groups after MRA treatment are similar to those of Hundemer et al. [7]. However, over time, Group 1 exhibited significant improvements in BP and the K level; Group 2 did not (Table 2). Although we cannot rule out the possibility that the change in BP may have been influenced by a reduction in the CCB dose after MRA treatment, the K level of Group 2 changed little. Therefore, Group 2 requires guidance on salt restriction, or increased MRA doses, because of inadequate suppression of MR activation and residual salt sensitivity. In general, “salt sensitivity” is usually used when blood pressure levels are responsive as alterations of dietary salt intake. Instead, we postulate in the present study that the ΔARC as a sensitivity of the renin-angiotensin-aldosterone system during MRA treatment which may reflect a part of “salt sensitivity”. We, therefore, utilize the ΔARC as a surrogate marker of “salt sensitivity”.
Third, salt intake restriction has been reported to lower BP [27,28,29] and reduce cardiovascular events [28, 30] in both normal subjects and patients with essential hypertension. Several guidelines recommend Na intakes <1,500–2,300 mg/day, thus 3.8–5.8 g/day [31,32,33,34]. Filippini et al. [29] (in a meta-analysis) found a linear relationship between salt reduction and BP reduction, especially in hypertensive patients. Sacks et al. [27] reported that the salt restriction of the Dietary Approaches to Stop Hypertension (DASH) diet significantly lowered BP. In the present study, one physician (YY) issued salt restriction instructions based on the eNaCl results. The dietary guidance given was thus identical for all patients, but, unfortunately, the absolute eNaCl level did not decrease. Guidance by a dietitian and introduction of the DASH diet are desirable. Salt intake restrictions should be implemented before increasing the MRA dose if the ARC is <5 pg/mL after MRA treatment to reduce medical costs [35, 36]. As the eNaCl data of the two Groups never differed significantly, the post-MRA treatment ARC may reflect not only the eNaCl values but also other factors including genetic determinants of renin level.
Our work had several limitations. First, we measured only changes in renin levels. PA therapy seeks to prevent cerebrocardiovascular events; we encountered no such event. Future studies are required to confirm that salt restriction in combination with MRAs in fact reduces cerebrocardiovascular events. Second, the follow-up period was short and we used only one-spot eNaCl data; long-term studies are needed. Third, although we sought correlations between eNaCl levels and ARC, we did not explore individual salt sensitivities.
In conclusion, PA patients with ARC < 5 pg/mL after MRA treatment should reduce salt intake even while on MRAs because of inadequate suppression of MR activity and residual salt sensitivity.
References
Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Born-Frontsberg E, Reincke M, Rump LC, Hahner S, Diederich S, Lorenz R, et al. Cardiovascular and cerebrovascular comorbidities of hypokalemic and normokalemic primary aldosteronism: results of the German Conn’s Registry. J Clin Endocrinol Metab. 2009;94:1125–30.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: a multicenter study in Japan. Hypertension 2018;71:530–7.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Bock HA, Hermle M, Brunner FP, Thiel G. Pressure dependent modulation of renin release in isolated perfused glomeruli. Kidney Int. 1992;41:275–80.
Lorenz JN, Weihprecht H, Schnermann J, Skøtt O, Briggs JP. Renin release from isolated juxtaglomerular apparatus depends on macula densa chloride transport. Am J Physiol. 1991;260:F486–93.
Kotchen TA, Luke RG, Ott CE, Galla JH, Whitescarver S. Effect of chloride on renin and blood pressure responses to sodium chloride. Ann Intern Med. 1983;98:817–22.
Freeman RH, Davis JO, Villarreal D. Role of renal prostaglandins in the control of renin release. Circ Res. 1984;54:1–9.
Kopp U, DiBona GF. Interaction of renal beta 1-adrenoceptors and prostaglandins in reflex renin release. Am J Physiol. 1983;244:F418–24.
Frindt G, Sackin H, Palmer LG. Whole-cell currents in rat cortical collecting tubule: low-Na diet increases amiloride-sensitive conductance. Am J Physiol. 1990;258:F562–7.
Sansom S, Muto S, Giebisch G. Na-dependent effects of DOCA on cellular transport properties of CCDs from ADX rabbits. Am J Physiol. 1987;253:F753–9.
Hropot M, Fowler N, Karlmark B, Giebisch G. Tubular action of diuretics: distal effects on electrolyte transport and acidification. Kidney Int. 1985;28:477–89.
Rose BD. Diuretics. Kidney Int. 1991;39:336–52.
Stanton BA, Kaissling B. Adaptation of distal tubule and collecting duct to increased Na delivery. II. Na+ and K+ transport. Am J Physiol. 1988;255:F1269–75.
Fountoulakis S, Papanastasiou L, Voulgaris N, Kounadi T, Markou A, Chrousos GP, et al. Salt intake in mineralocorticoid receptor antagonist-treated primary aldosteronism: foe or ally? Hormones (Athens). 2020;19:223–32.
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension 2013;62:62–9.
Reincke M, Fischer E, Gerum S, Merkle K, Schulz S, Pallauf A, et al. Observational study mortality in treated primary aldosteronism: the German Conn’s registry. Hypertension 2012;60:618–24.
Weber KT. Aldosterone in congestive heart failure. N. Engl J Med. 2001;345:1689–97.
Sechi LA, Novello M, Lapenna R, Baroselli S, Nadalini E, Colussi GL, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA 2006;295:2638–45.
Michelakis AM, Yoshida H, Dormois JC. Plasma renin activity and plasma aldosterone during the normal menstrual cycle. Am J Obstet Gynecol. 1975;123:724–6.
Weinberger MH, Kramer NJ, Grim CE, Petersen LP. The effect of posture and saline loading on plasma renin activity and aldosterone concentration in pregnant, non-pregnant and estrogen-treated women. J Clin Endocrinol Metab. 1977;44:69–77.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl J Med. 2001;344:3–10.
Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, et al. Effect of salt substitution on cardiovascular events and death. N. Engl J Med. 2021;385:1067–77.
Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose-response meta-analysis of experimental studies. Circulation 2021;143:1542–67.
He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet 2011;378:380–2.
McGuire S. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv Nutr. 2016;7:202–4.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010;121:586–613.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–30.
Tobe SW, Stone JA, Anderson T, Bacon S, Cheng AYY, Daskalopoulou SS, et al. Canadian Cardiovascular Harmonized National Guidelines Endeavour (C-CHANGE) guideline for the prevention and management of cardiovascular disease in primary care: 2018 update. CMAJ 2018;190:E1192–e206.
Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N. Engl J Med. 2010;362:590–9.
Zhang D, Cogswell ME, Wang G, Bowman BA. Evidence of dietary improvement and preventable costs of cardiovascular disease. Am J Cardiol. 2017;120:1681–8.
Acknowledgements
We thank the physicians and medical staff of the Department of Endocrinology and Diabetology, Oita University Hospital, who treated the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HS has honorarium from Daiichi-Sankyo Company, Mochida Pharmaceuticals, Astrazeneca, Novartis Pharma, Bayer, and Astellas. HS also received scholarship from Chugai and Bayer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshida, Y., Fujiki, R., Kinoshita, M. et al. Importance of dietary salt restriction for patients with primary aldosteronism during treatment with mineralocorticoid receptor antagonists: The potential importance of post-treatment plasma renin levels. Hypertens Res 46, 100–107 (2023). https://doi.org/10.1038/s41440-022-01045-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01045-5
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
Hypertension Research (2024)
-
Effects of esaxerenone on blood pressure, urinary albumin excretion, serum levels of NT-proBNP, and quality of life in patients with primary aldosteronism
Hypertension Research (2024)
-
Clinical benefits and uncertainties of treatment with esaxerenone in primary aldosteronism
Hypertension Research (2024)
-
Renin as a Biomarker to Guide Medical Treatment in Primary Aldosteronism Patients. Findings from the SPAIN-ALDO Registry
High Blood Pressure & Cardiovascular Prevention (2024)