Abstract
A recent report stated that patients with primary aldosteronism who remain renin suppressed during mineralocorticoid receptor antagonist treatment might have a higher risk of developing cardiovascular disease than those with unsuppressed renin activity. We retrospectively investigated the incidence of composite cardiovascular disease and risk factors for cardiovascular disease in 1115 Japanese patients with primary aldosteronism treated with mineralocorticoid receptor antagonists. The median follow-up period was 3.0 years, and the incidence of cardiovascular events was very low (2.1%) throughout 5 years of follow-up. Changes in plasma renin activity from before to after mineralocorticoid receptor antagonist treatment were divided into three groups based on tertile, low, intermediate, and high plasma renin activity change groups, with incidences of cardiovascular disease events of 2.1%, 0.5%, and 3.7%, respectively. Multivariate Cox regression analysis revealed age (adjusted hazard ratio, 1.07; 95% confidence interval, [1.02–1.12]) and body mass index (adjusted hazard ratio, 1.13 [1.04–1.23]) as independent risk factors for cardiovascular disease. The high plasma renin activity change group had significantly higher cardiovascular disease risk with mineralocorticoid receptor antagonist treatment than the intermediate plasma renin activity change group (adjusted hazard ratio, 5.71 [1.28–25.5]). These data suggest that a high change in renin level after mineralocorticoid receptor antagonist treatment may not necessarily predict a better prognosis of cardiovascular disease in patients with primary aldosteronism.
Similar content being viewed by others
Introduction
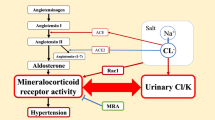
Primary aldosteronism (PA) is a form of secondary hypertension caused by autonomous overproduction of aldosterone, with renin activity usually being suppressed [1, 2]. Aldosterone-producing adenoma and idiopathic hyperaldosteronism are the main subtypes of PA [3]. Compared with essential hypertension, PA is associated with a higher incidence of cardiovascular and cerebrovascular diseases [4,5,6], and these important comorbidities are mediated by excessive mineralocorticoid receptor (MR) activation [7]. Therefore, clinical guidelines recommend treatment with an MR antagonist (MRA) in cases in which patients with PA have bilateral PA or when they are unwilling or unable to undergo surgery [2]. However, previous studies have shown that some patients with PA treated with MRA have a higher rate of cardiovascular disease (CVD) than hypertensive controls [8, 9]. The plasma aldosterone concentration (PAC) and plasma renin activity (PRA), which increase with MRA administration, are important indicators of the effect of MR inhibition, and a higher increase in PRA level from baseline indicates that MRA may more strongly inhibit MR activity [10, 11]. In a previous large PA cohort study, the risk of CVD development in patients with PA who had unsuppressed renin levels with MRA treatment was comparable to that of patients with essential hypertension [8]. Thus, titration of MRA aimed at avoiding suppression of renin activity may help to improve CVD outcomes in patients with PA. To date, very few large studies have focused on CVD outcomes and risk factors, including renin levels, in patients with PA receiving MRA treatment.
Therefore, this study aimed to investigate the association between CVD outcomes and the change in renin level from before to after MRA treatment using a large Japanese cohort database of patients with PA.
Methods
Study patients
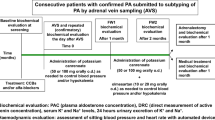
This retrospective cohort study was conducted using data from a nationwide multicenter collaborative PA registry [Japan Primary Aldosteronism Study (JPAS)/Japan Rare/Intractable Adrenal Disease Study (JRAS)] involving 41 referral centers [12]. Patients who were diagnosed with PA between January 2006 and March 2019 were enrolled. Eligible patients were men or women aged 20–90 years. Over the 5-year follow-up period, we enrolled a total of 1115 patients with PA treated with MRAs whose clinical outcomes and blood sample results, including PRA before and after MRA treatment, could be confirmed. The indications for medical treatment with MRA for patients with PA were determined by each center’s attending physician based on adrenal venous sampling (AVS) results, imaging findings, clinical features, and patient requests. PA diagnoses were performed in accordance with the guidelines of the Japan Endocrine Society and the Japan Society of Hypertension [13, 14]. Screening for PA was considered positive at a PAC/PRA ratio of >200 or a PAC/active renin concentration (ARC) ratio of >40. PA was diagnosed when at least one of the following tests was positive: captopril challenge, saline infusion, furosemide-upright, and oral salt-loading. Before the PA screening test, the antihypertensive drug was changed to a calcium channel or an α-adrenergic blocker, as necessary. Potassium was replenished if hypokalemia was present before the confirmatory test. The PA subtype in this study was diagnosed primarily based on AVS results using adrenocorticotropic hormone (ACTH) stimulation [15, 16]. The selectivity index (SI) was defined as the ratio of cortisol of the adrenal vein to that of the inferior vena cava, and cannulation of the adrenal vein was considered successful if the SI was >5. The lateralization index (LI) was defined as the dominant adrenal vein aldosterone-to-cortisol ratio (A/C) divided by the nondominant adrenal vein A/C ratio. The contralateral ratio (CR) was defined as the nondominant adrenal vein A/C ratio divided by the inferior vena cava A/C ratio. Unilateral PA was diagnosed when LI > 4 and CR < 1 after ACTH stimulation.
Data collection
Clinical and laboratory data were available for visit dates of the patients at baseline and at 6, 12, 36, and 60 months after definitive PA diagnosis. Blood samples were collected using the method followed at each medical institution, which was standardly conducted after 30 min of rest in the supine position. Treatment with an MRA was commenced after the study participants received a definitive diagnosis of PA, including AVS. We used PRA data measured before and after starting MRA treatment. If a CVD event occurred before a specified visit date, we used the PRA data obtained before the onset of a CVD event. Follow-up periods included the date of definitive diagnosis to the date of occurrence of a CVD event. For patients who did not develop a CVD event during the observation period, their follow-up was terminated on the last consultation day over the 5-year observation period.
The estimated glomerular filtration rate (eGFR) was calculated using the following equation prepared by the Japan Society of Nephrology, as follows:
The unified MRA dose was analyzed by multiplying the total daily dose of spironolactone by 2 for conversion to a dose equivalent to eplerenone [17, 18]. The details of the assay method, including PRA, ARC, and PAC, are presented in the Supplementary Methods. The PRA change with MRA treatment was calculated by subtracting the PRA value before treatment from that during MRA treatment. The PAC change with MRA treatment was calculated by subtracting the PAC value before treatment from that during MRA treatment.
The results of adrenal localization diagnosis by AVS are presented as the proportion of unilateral categories. Diabetes and dyslipidemia were confirmed based on medical history or medication use. A CVD history included myocardial infarction, cerebral hemorrhage, cerebral infarction, and heart failure of New York Heart Association class II or higher.
Definition of cardiovascular outcomes
The primary outcome was the occurrence of CVD-related events and death. We defined composite CVD as the presence of stroke, ischemic heart disease, heart failure necessitating hospitalization, and atrial fibrillation. Heart failure included causes of severe aortic stenosis and sick sinus syndrome, both of which require hospitalization. In this study, CVD events consisted of composite CVD and mortality and excluded death caused by overt malignancy.
Data analysis
Characteristics before and after MRA treatment were compared between the CVD occurrence and nonoccurrence groups.
In this study, patients with PA were divided into three groups according to the tertile of PRA change with MRA treatment: low (≤0.1 ng/mL/h), intermediate (0.2–0.7 ng/mL/h), and high (≥0.8 ng/mL/h) PRA change groups. The characteristics of the groups, including the incidence of CVD, were compared.
Continuous variables with a normal distribution are expressed as means (standard deviations), whereas those with a nonnormal distribution are expressed as medians (interquartile ranges [IQRs]). For comparative analysis between two groups, we performed Fisher’s exact test for categorical variables and Student’s t-test or the Mann–Whitney U test for continuous variables. Comparison of the three groups was performed using Fisher’s exact test, one-way analysis of variance, and the Kruskal–Wallis test. The P-value was adjusted using the Bonferroni method.
The incidence of CVD events among PRA changes stratified by MRA treatment was estimated using a Kaplan–Meier survival curve and evaluated with the log-rank test. The P-value was adjusted using the Bonferroni method.
Univariate and multivariate Cox proportional hazard models were employed to identify factors significantly associated with the development of CVD events. Variables with a P-value of <0.05 in univariate analysis and sex were selected in multivariate analysis. The goodness-of-fit for the multivariate Cox proportional hazards model was confirmed by the Wald test, and the proportional hazards assumption was confirmed by a correlation test using Schoenfeld residuals.
Spearman’s rank correlation coefficient was used for correlation analysis of PRA changes by MRA and other parameters.
All statistical analyses were conducted using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [19]. P values were two-sided, and a P-value of <0.05 indicated statistical significance.
Ethics
This study was performed in accordance with the guidelines for clinical studies published by the Ministry of Health and Labor of Japan and was approved by the institutional ethics committees of all participating facilities. This observational study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN ID 18756 and 32525). The opt-out option was posted on the website.
Results
Study patients
In this study, data for 1115 eligible patients with PA who were followed up for a median duration of 3.0 years (IQR, 1.1–5.0) were analyzed. The overall prevalence of composite CVD events in our study population was 2.1% over the 5-year observation period. Details of the composite CVD events and the incidence of each cardiovascular event are presented in Supplementary Table 1.
Comparison of the characteristics of patients with PA with and without CVD events during the follow-up period is presented in Table 1. Patients in the CVD event occurrence group were older (P = 0.001), had a higher body mass index (BMI) (P = 0.02), had a lower eGFR at baseline and during MRA treatment (P = 0.04 and P = 0.03, respectively), and had a longer duration of hypertension (P = 0.003) than those in the nonevent occurrence group. There was also a higher proportion of patients with more than urinary protein 1 + (P = 0.01) in the CVD event occurrence group. However, the prevalence of CVD history, dyslipidemia, and diabetes mellitus did not differ between the two groups. During follow-up, no significant differences were observed in MRA dose, blood pressure, or K level, as well as changes in PRA and PAC, with MRA treatment between the groups.
CVD risk factors during MRA treatment
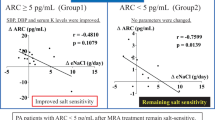
As changes in PRA are substantial as an indicator of the effect of MRAs, we compared variables among the three groups stratified by tertile of PRA changes with MRA treatment (Table 2). The incidence rates of CVD events in the low, intermediate, and high PRA change groups were 2.1%, 0.5%, and 3.7%, respectively, a difference that was significant (P = 0.008). The high PRA change group had a higher incidence of CVD events than the intermediate PRA change group (P = 0.009). In addition, the low PRA change group tended to have a higher incidence of CVD events than the intermediate change group, though the difference was not significant. Kaplan–Meier survival curve analysis showed that the incidence of CVD events was higher in the high PRA change group than in the intermediate PRA change group throughout the observation period (P = 0.01) (Fig. 1). In univariate Cox proportional hazards regression analysis to investigate CVD risk factors during MRA treatment, variables with P values of <0.05 included high PRA change, age, BMI, eGFR at baseline, proteinuria, and duration of hypertension (Table 3). Multivariate Cox proportional hazards analysis indicated that the risk of composite CVD, including death, was significantly greater in the high PRA change group than in the intermediate group (adjusted hazard ratio (AHR), 5.71 [95% CI, 1.28–25.5]). Other significant CVD risk factors in multivariate analysis were age (AHR, 1.07 [1.02–1.12]) and BMI (AHR, 1.13 [1.04–1.23]). Proteinuria and duration of hypertension were excluded as covariates in the multivariate regression model because they were unknown in several cases.
Factors Associated with High PRA Change with MRA Treatment
As shown in Table 2, the proportion of male individuals was greater in the high than in the intermediate (P = 0.02) and low (P < 0.001) PRA change groups. The high PRA change group also had a significantly higher BMI than the low PRA change group (P = 0.04). MRA doses were significantly higher in the high than in the low and intermediate groups (P < 0.001 for both comparisons). During MRA treatment, systolic and diastolic blood pressures were significantly lower in the high PRA change group. Moreover, serum Na and K levels were significantly lower and higher, respectively, in the high PRA change group. These findings suggest that MR blockade was relatively sufficient in the high PRA change group. Along with changes in PRA, PAC levels increased with MRA treatment, indicating that the large PAC change due to MRA treatment might be attributed to higher activity of the renin-angiotensin system (RAS) in the high PRA change group. The use of RAS inhibitors, such as angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors, did not differ among the three PRA change groups.
The degree of change in PRA level from before to after MRA treatment correlated highly with the PRA value during MRA treatment according to Spearman’s test (ρ = 0.86, P < 0.001) but did not correlate with PRA before MRA and showed only a weak correlation with MRA dose (ρ = 0.17, P < 0.001) (Supplementary Table 2).
Discussion
The increase in PRA level with MRA treatment is considered an important indicator for the effect of MR inhibition. In this study, we investigated the predictive potential of PRA changes caused by MRA treatment with regard to the development of CVD during follow-up period in patients with PA treated with MRAs. Unexpectedly, the high PRA change group had a significantly higher risk of CVD than the intermediate PRA change group. The low PRA change group also had a higher incidence of CVD events than the intermediate PRA change group, in line with the results of a previous report [8], though with no significant difference. In addition to PRA changes, age and BMI were identified as independent CVD risk factors for the study subjects. Indeed, age and obesity are known independent risk factors for CVD [20, 21]. Potassium and blood pressure levels, which are considered to be markers of PA severity, were not identified as such in our model, likely due to lower detection sensitivity than PRA change.
A question that could be raised is why CVD risk was higher in the high PRA change group of our cohort. Interestingly, the high PRA change group had a higher proportion of male participants than the other groups. One study reported that in normotensive populations, men have higher PRA than women [22]. Moreover, a study on postmenopausal women has shown that women who undergo estrogen replacement therapy have lower renin activity than those who do not or men [23]. Another previous study reported that the response of PRA to an intravenous furosemide test was lower in women than in men [24]. In a prospective study of pretreatment hypertension, the high renin-sodium profile group was more likely to have myocardial infarction than the low and normal groups, and men had a higher renin profile than women [25]. In animal studies, testosterone increases renin activity, with a strong positive linear relationship between testosterone and PRA [26,27,28]. Based on these previous reports, it can be hypothesized that the higher proportion of male individuals resulted in high PRA and a high risk of CVD.
Another characteristic of the high PRA change group was higher BMI than in the other groups. An increase in renin level has been reported for patients with obesity due to sympathetic nervous system activation [29]. Moreover, significant decreases in renin and aldosterone levels occurred with weight loss in patients with obesity [30]. In this study, although the difference in BMI was small among the three groups, BMI was one of the independent CVD risk factors. Therefore, the higher BMI may be partly related to the high CVD risk in the high PRA change group. Nevertheless, as the aforementioned studies did not examine the PRA response to MRA treatment, their applicability to the discussion of our study is limited, and further studies are needed to clarify the involvement of male and obesity profiles in this context. The PAC change with MRA treatment was proportionally high in the high PRA change group, demonstrating that RAS activity was intact in this context. As RAS is located upstream of MR, MRA does not inhibit but rather activates the system, which might lead to undesirable outcomes. Although the dose of MRA used in the high PRA change group was relatively high, the correlation between PRA change and MRA dose was very weak. Therefore, we do not recommend reducing the MRA dose when encountering individuals with high PRA changes with MRA treatment. We should instead combine RAS inhibitors for such cases while considering the possible development of hyperkalemia. The optimal approach to reducing CVD risk in patients with a high PRA change needs to be investigated and established in future studies.
Our cohort study showed that a very low (2.1%) incidence of CVD development in Japanese patients with PA treated with MRA during a 5-year observation period. One of the possible reasons for the low incidence of CVD is that many patients had bilateral PA, which is a relatively mild PA subtype. Second, the median follow-up duration of this study was 3 years, which is a relatively short period. Third, the Japanese population has been reported to have the longest life expectancy, the lowest prevalence of obesity, and the lowest mortality due to ischemic heart disease compared to populations of other Organization for Economic Cooperation and Development countries. The greater longevity observed in the Japanese population might be attributed to their healthy lifestyle, diet, universal and equitable health care coverage, and social determinants [31, 32].
This study has some limitations. First, the retrospective design may have affected the quality of the data. Second, we did not collect data on urinary Na excretion during the follow-up period; therefore, we could not assess the effect of Na intake on renin levels during MRA treatment. Third, this study did not exclude patients with a history of CVD because many of those who developed a CVD event during the 5-year follow-up already had a history of CVD at the time of PA diagnosis. This setting was different from that of a previous similar study [8]. Hence, we cannot argue why the result of our study was different from the previous one.
Last, the PRA change used in this study is not currently authorized as a marker of MRA effect; thus, the validity of this marker should be confirmed in future research.
In conclusion, this study indicates that the risk of CVD is unexpectedly higher in patients with PA with high PRA change due to MRA treatment. Although the PRA change caused by MRA treatment is an indicator of the effect of MR inhibition, other factors are also involved in the PRA change induced by MRA treatment. Therefore, a high PRA change may not necessarily be a better prognostic marker. Further studies are needed to establish the optimal approach to predict CVD risk in patients with PA treated with MRAs.
References
Conn JW, Cohen EL, Rovner DR. Suppression of plasma renin activity in primary aldosteronism: distinguishing primary From secondary aldosteronism in hypertensive disease. JAMA. 1964;190:213–21.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Young WF. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. Intern Med J. 2019;285:126–48.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Mulatero P, Monticone S, Bertello C, Viola A, Tizzani D, Iannaccone A, et al. Long-term cardio- and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metab. 2013;98:4826–33.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Vaidya A, Mulatero P, Baudrand R, Adler GK. The expanding spectrum of primary aldosteronism: implications for diagnosis, pathogenesis, and treatment. Endocr Rev. 2018;39:1057–88.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Rossi GP, Maiolino G, Flego A, Belfiore A, Bernini G, Fabris B, et al. Adrenalectomy lowers incident atrial fibrillation in primary aldosteronism patients at long term. Hypertension. 2018;71:585–91.
Ito S, Itoh H, Rakugi H, Okuda Y, Yoshimura M, Yamakawa S. Double-blind randomized phase 3 study comparing esaxerenone (CS-3150) and eplerenone in patients With essential hypertension (ESAX-HTN study). Hypertension. 2020;75:51–8.
Ito S, Itoh H, Rakugi H, Okuda Y, Iijima S. Antihypertensive effects and safety of esaxerenone in patients with moderate kidney dysfunction. Hypertens Res. 2021;44:489–97.
Nakamaru R, Yamamoto K, Akasaka H, Rakugi H, Kurihara I, Yoneda T, et al. Sex differences in renal outcomes After medical treatment for bilateral primary aldosteronism. Hypertension. 2021;77:537–45.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism-the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, Van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004;136:1227–35.
Webb R, Mathur A, Chang R, Baid S, Nilubol N, Libutti SK, et al. What is the best criterion for the interpretation of adrenal vein sample results in patients with primary hyperaldosteronism? Ann Surg Oncol. 2012;19:1881–6.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR From serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Weinberger MH, Roniker B, Krause SL, Weiss RJ. Eplerenone, a Selective aldosterone Blocker, in mild-to-moderate hypertension. Am J Hypertens. 2002;15:709–16.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Dhingra R, Vasan RS. Age as a cardiovascular risk factor. Med Clin North Am. 2012;96:87–91.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on obesity and heart disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918.
James GD, Sealey JE, Müller F, Alderman M, Madhavan S, Laragh JH. Renin relationship to sex, race and age in a normotensive population. J Hypertens Suppl. 1986;4:S387–9.
Schunkert H, Danser AH, Hense HW, Derkx FHM, Kürzinger S, Riegger GAJ. Effects of estrogen replacement therapy on the renin-angiotensin system in postmenopausal women. Circulation. 1997;95:39–45.
Kaplan NM, Kem DC, Holland OB, Kramer NJ, Higgins J, Gomez-Sanchez C. The intravenous furosemide test: a simple way to evaluate renin responsiveness. Ann Intern Med. 1976;84:639–45.
Alderman MH, Madhavan S, Ooi WL, Cohen H, Sealey JE, Laragh JH. Association of the Renin-Sodium Profile with the risk of myocardial infarction in patients with hypertension. N. Engl J Med. 1991;324:1098–104.
Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001;37:1199–208.
Katz FH, Roper EF. Testosterone effect on renin system in rats. Proceedings of the Society for Experimental Biology & Medicine. Proc Soc Exp Biol Med. 1977;155:330–3.
Chen YF, Naftilan AJ, Oparil S. Androgen-dependent angiotensinogen and renin messenger RNA expression in hypertensive rats. Hypertension. 1992;19:456–63.
Kalil GZ, Haynes WG. Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hyperten Res. 2012;35:4–16.
Tuck ML, Sowers J, Dornfeld L, Kledzik G, Maxwell M. The effect of weight reduction on blood pressure, plasma renin activity, and plasma aldosterone levels in obese patients. N. Engl J Med. 1981;304:930–3.
OECD. iLibrary. Health at a Glance 2019: OECD Indicators. OECD Publishing, Paris, https://doi.org/10.1787/4dd50c09-en. Accessed 19 July 2021.
Sakamoto H, Mizanur R, Nomura S, Okamoto E, Koike S, Yasunaga H, et al. (2018). World Health Organization. Regional Office for South-East Asia. Japan Health System Review. http://apps.who.int/iris/handle/10665/259941. Accessed 19 July 2021.
Acknowledgements
This study was conducted as part of the JPAS and JRAS by a Research Grant from the Japan Agency for Medical Research and Development (AMED) [grant number JP17ek0109122 and JP20ek0109352] and the National Center for Global Health and Medicine, Japan [grant number 27–1402, 30–1008]. This study was partly supported by the Research Committee on Disorders of Adrenal Hormones, a Grant-in-Aid from the Ministry of Health, Labor, and Welfare of Japan (Nanjiseisikkanseisakukenkyujigyo [grant number 20FC1020]).
JPAS/JRAS Study Group
Hisashi Fukuda25, Yasushi Tanaka26, Yoshiyu Takeda27, Hironobu Umakoshi28, Yui Shibayama29, Takanobu Yoshimoto30, Junji Kawashima31, Katsutoshi Takahashi32, Megumi Fujita33, Minemori Watanabe34, Yuichi Matsuda35, Hirotaka Shibata36, Kohei Kamemura37, Yuichi Fujii38, Hiromi Rakugi39, Atsushi Ogo40, Shintaro Okamura41, Shozo Miyauchi42, Toshihiko Yanase43, Takashi Kawamura44, Tomikazu Fukuoka45, Tatsuya Kai46, Yuichiro Yoshikawa47, Shigeatsu Hashimoto48, Masanobu Yamada49, Ryuichi Sakamoto50, Chiba Yoshiro51
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nomura, M., Kurihara, I., Itoh, H. et al. Association of cardiovascular disease risk and changes in renin levels by mineralocorticoid receptor antagonists in patients with primary aldosteronism. Hypertens Res 45, 1476–1485 (2022). https://doi.org/10.1038/s41440-022-00960-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00960-x
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
Hypertension Research (2024)
-
Renin as a Biomarker to Guide Medical Treatment in Primary Aldosteronism Patients. Findings from the SPAIN-ALDO Registry
High Blood Pressure & Cardiovascular Prevention (2024)
-
Esaxerenone for nocturnal hypertension and possible future direction for treatment of hypertension-cardiovascular-kidney comorbidity
Hypertension Research (2023)
-
Importance of plasma aldosterone concentrations as a clinical indicator of nocturnal hypertension in primary aldosteronism
Hypertension Research (2023)
-
Recent progress in the diagnosis and treatment of primary aldosteronism
Hypertension Research (2023)