Abstract
Mild hyperkalemia is a common side effect of mineralocorticoid receptor antagonist (MRA) treatment of patients with primary aldosteronism (PA), which can be worsened by instructions to minimize salt intake. Our objective was to evaluate the effect of salt consumption on serum potassium levels and mean, mean minimal, and mean maximal systolic and diastolic blood pressure (BP) in MRA-treated hyperkalemic PA patients under relative salt restriction. Seventeen consecutive mildly hyperkalemic MRA-treated PA patients aged 66.3 ± 8.37 years were recruited. Body mass index (BMI) and BP were assessed, and serum and 24-h urinary sodium and potassium levels, plasma renin, and serum aldosterone were measured, while patients followed a relatively salt-restricted diet, after 1 month of controlled salt supplementation (usual salt-restricted diet plus 4 g salt/day) and after 6 months on instructions for free dietary salt consumption. Baseline salt consumption was additionally evaluated in two more patient groups (normotensive subjects and normokalemic MRA-treated PA patients). One month of controlled salt supplementation (24-h urine sodium (median, min, max): 195.2 (120.30–275.20) vs 110.13 (34.30–139.20) mEq/day, p < 0.001) resulted in increased kaliuresis (62.25 (40.69–97.0) vs 54.0 (23.28–79.60) mEq/day, p = 0.001) and a decrease of serum potassium (5.2 (5–5.70) vs 4.6 (3.8–5.1) mEq/L, p < 0.001), while serum sodium (139 (133–141) vs 1 39 (135–144) mEq/L) and mean systolic (130 (105–141 vs. 130 (106–141) mmHg) and diastolic (76 (53–85) vs75 (53–84) mmHg) BP remained stable. These findings were unchanged after 6 months of free salt consumption. BMI remained constant, while plasma renin and serum aldosterone decreased following salt repletion. Adequate salt consumption attenuates MRA-induced hyperkalemia in relatively salt-restricted PA patients without affecting BP or BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of primary aldosteronism (PA) is reported to be between 11.2% in hypertensive patients and 19.5% in patients with resistant hypertension [1]. Recent studies suggest that PA may account for as much as 30% of all cases of arterial hypertension, an estimate based on a novel diagnostic test, the post-fludrocortisone-dexamethasone suppression test (FDST) [2, 3]. PA patients are at a substantially higher cardiovascular and cerebrovascular risk compared to those with essential hypertension [4, 5]. However, there is to date a lack of clinical data regarding the clinical consequences of aldosterone excess diagnosed by FDST alone. Mineralocorticoid receptor antagonists (MRAs) have been effectively used as the first-line therapy for non-surgically treated cases of primary aldosteronism (PA) [6,7,8], while more recently, MRAs have been employed in lowering blood pressure (BP) in hypertensive patients with chronic stress ACTH-dependent aldosterone hypersecretion [2]. A common side effect of MRA therapy in cardiac and renal disease is hyperkalemia. On the other hand, there are few data on the frequency of hyperkalemia in MRA-treated PA patients [9, 10]. After apparent hyperkalemia due to hemolysis has been excluded, common causes of hyperkalemia include MRA over-dosing, declining glomerular filtration rate, advanced age, presence of diabetes mellitus, and/or increased potassium intake [11]. In the absence of these factors, long-term therapy with low-dose MRA is rarely related to severe hyperkalemia [8]. In certain cases, however, where the administration of a high MRA dose is required, hyperkalemia may necessitate dose reduction or discontinuation of therapy, thereby limiting the therapeutic potential of these useful agents.
Potassium excretion in urine is directly dependent on the amount of sodium that reaches the renal distal convoluted tubule (DCT) and cortical collecting duct (CCD), which are the main targets of aldosterone action. However, an undefined proportion of PA patients treated with MRAs may have sodium deficit for the following reasons: first, patients are often instructed to minimize their dietary salt intake to avoid sodium-related volume overload as sodium-restricted diet has been previously reported to be effective in the treatment of mild forms of PA [12] and, second, MRAs induce natriuresis through their inhibitory action on epithelial sodium channels (ENaC), sodium chloride co-transporters (NCC), and Na-K-Cl co-transporters (NKCC) [11]. Thus, in the presence of significant sodium deficit, MRA-treated PA patients may develop hyperkalemia given that restricted sodium delivery at the DCT and CCD targets of aldosterone may render these tissues ineffective in potassium elimination. In fact, animal data have shown that salt restriction in KO mice with selective inactivation of ENaC in the CCD, caused weight loss, increased urinary sodium excretion, and induced hyperkalemia [13]. In contrast, in EnaC-KO mice fed a high-sodium and reduced-potassium diet, body weight, plasma, and urinary electrolyte concentrations and excretion normalized, despite the fact that plasma aldosterone levels remained increased [14]. On the basis of these data, we hypothesized that restoration of adequate salt intake could correct the diminished kaliuresis and restore serum potassium concentrations to normal in relatively salt-restricted hyperkalemic MRA-treated PA patients.
To explore this hypothesis, we evaluated the effect of salt intake on serum potassium levels in relation to arterial BP, including mean systolic (SBP) and diastolic (DBP), as well as their mean minimal and maximal values, in MRA-treated hyperkalemic PA patients with relative salt restriction. Secondary outcomes included changes in body weight, body mass index (BMI), serum and urinary sodium and potassium levels, plasma renin, and serum aldosterone concentrations.
Patients and methods
Patients
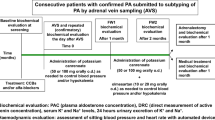
We prospectively studied the first 17 consecutive PA patients (age range 48–81 years), who developed hyperkalemia among 176 MRA-treated PA patients that were diagnosed in the Endocrine Clinic in 2010 and presented during 2015. The original diagnosis of PA was based on the combination of the post-fludrocortisone-dexamethasone suppression test (FDST) aldosterone:renin ratio (ARR) of at least 26 pmol/mIU (0.93 ng/dL/μU/ml) and post-FDST aldosterone levels at least 82 pmol/L (2.96 ng/dL), as previously described [3, 15]. Eligible PA patients were aged 35 years or older, treated with MRA alone or in combination with calcium channel blockers, who presented with hyperkalemia (serum potassium ≥ 5 mEq/L). Exclusion criteria included the presence of renal, thyroid, gastrointestinal, and/or hepatic disease; past or present malignancy; and rheumatologic disease, acute uncontrolled mental illness, and concomitant diuretic use or consumption of other potassium and/or sodium interfering drugs. Of the 176 PA patients, 12 met exclusion criteria due to renal or hepatic disease, potassium-interfering drugs, angiotensin-converting enzyme inhibitor (ACE-i), or angiotensin receptor blockers (ARB), and two were reluctant to participate. Of the remaining 162 that were assessed, 146 were followed up and among them 17 patients developed hyperkalemia. All 17 hyperkalemic MRA-treated PA patients were followed up and completed the study. The flowchart of the study is depicted in Fig. 1.
From the time the diagnosis of hypertension was made, patients were on a sodium-restricted diet, i.e., instructed to avoid salt consumption. The baseline daily dose of MRA was decided according to BP, circulating renin and potassium levels, e-GFR, and 24-h urinary potassium excretion rate, while patients were on a sodium-restricted diet. The daily dose of MRA was then individualized according to the severity of their hypertension. Patients with SBP < 160 mmHg and DBP < 100 mmHg were initially treated with 25 mg of spironolactone or 50 mg of eplerenone, whereas patients with SBP > 160 and DBP > 100 mmHg were initially treated with 50 mg of spironolactone or 100 mg of eplerenone. The MRA dose was kept the same for the month of controlled dietary salt supplementation and during the ensuing 6 months of free salt intake (Fig. 1). Informed consent was obtained from all subjects and the study protocol was approved by the hospital ethics committee. All procedures performed were in accordance with the ethical standards of General Hospital of Athens ‘G. Gennimatas’ research committee complies with the 1964 Declaration of Helsinki and its later amendments.
All hyperkalemic MRA-treated PA patients underwent recording of their medical history and had a complete physical examination and documentation of anthropometric characteristics (weight (kg), BMI (kg/m2) and waist circumference (cm)) by the same physician (S.F.) at baseline, under relative salt restriction (RRS), at 1 month of controlled salt supplementation (CS) (usual relatively salt-restricted diet plus 4 g salt/day) and at the end of the 6-month follow-up period on instructions for free dietary salt intake (FS) (Fig. 1). The demographic characteristics of the patients are shown in Table 1.
MRA antihypertensive therapy included either spironolactone at a dose of 25–100 mg/day or eplerenone at a dose of 50–100 mg/day. Ten patients received spironolactone and seven patients received eplerenone at a mean dose (SD) of 67.5 (28.98) mg/day and of 57.15 (18.9) mg/day, respectively. Further antihypertensive treatment with calcium channel blockers was administered in six patients with inadequate BP control on MRA. None of the patients received ACE-i or ARB treatment.
In order to investigate whether the development of hyperkalemia in the abovementioned 17 patients could be attributed to low sodium intake or was a consequence of a potential intrinsic propensity, two additional groups of 34MRA-treated normokalemic PA patients and of 43 normotensive subjects, matched for age and sex were additionally included (Table 2). The 34 normokalemic MRA-treated patients were selected according to their age to be matched with the hyperkalemic MRA-treated PA patients.
Methods
Blood pressure measurements and salt administration
All hyperkalemic MRA-treated PA patients participated in an initial 30-min educational presentation on the correct technique of measuring blood pressure with automated digital or manometric sphygmomanometers provided by Datascope (Accutorr Plus).
Home BP monitoring was used; measurements had to be taken at least an hour from smoking cigarettes, from alcohol or coffee consumption, and from exercise or after acute emotional stress. For each BP recording, patients were instructed to take two consecutive measurements at least 2 min apart while seated and to record the lowest values. After discarding the measurements of the first day, we calculated the average value of the remaining measurements. Normal BP was defined as systolic BP (SBP) of less than 135 mmHg and diastolic BP (DBP) less than 85 mmHg [16].
All hyperkalemic MRA-treated PA participants were instructed to measure and record their BP twice daily (morning and evening) for 30 days in a sitting position, while on their regular relatively salt-restricted diet and, subsequently, under controlled salt supplementation (usual relatively salt-restricted diet plus 4 g/day) for 1 month with the instruction of equal distribution of meals. They were also informed on the sodium content of various regularly consumed foods. Following data analysis, free salt consumption was suggested to all participants for the next 6-month follow-up period with the instruction to measure and register BP twice weekly. Adequate salt consumption was confirmed by 24-h urinary sodium measurement.
Furthermore, BP was monitored twice per month at the outpatient department by the patient and then by the same physician (S.F.) to ensure that the correct measuring technique was being followed by the patients.
Biochemical, hormonal, and imaging investigation
All patients underwent the following tests as outpatients: blood sampling for baseline serum aldosterone, cortisol and ACTH, plasma renin, serum and 24-h urinary creatinine, and potassium and sodium concentrations. To exclude hemolysis-induced pseudohyperkalemia, hemolysis was qualitatively analyzed in the hospital lab by a photometric method and hemolyzed samples were discarded and blood collection plus biochemical evaluation were repeated [17]. Twenty-four-hour urinary sodium excretion was considered as the most effective index of adequate salt intake.
An adrenal computed tomography (CT) scan with 2-mm sections using the Philips Brilliance 16 Spiral Scanner was performed in all 17 participants. Adrenal adenomas were defined as well-circumscribed adrenal lesions greater than 10 mm with a non-contrast CT attenuation coefficient of less than 10 Hounsfield units. Seven patients were diagnosed as having bilateral idiopathic adrenal hyperplasia (IAH), while adrenal adenomas were found in 10 patients (three bilateral and seven unilateral). Patients with bilateral adenomas were not operated on due to a lack of AVS in our facility. Of the remaining seven patients with unilateral adenomas, two could not be operated on due to other comorbidities, two were unwilling to undergo a surgical procedure, and three were on the waiting list for a unilateral adrenalectomy at the time of our study.
Blood pressure measurements and hormonal analysis in the additional control groups
SBP and DBP (mean of two measurements per week), as well as serum and 24-h urinary sodium and potassium levels were recorded, in a separate data set, in the two additional groups used as controls (i.e., normotensive subjects, and normokalemic MRA-treated PA patients) (Table 2). Plasma renin and serum aldosterone were also recorded in normo- and hyperkalemic PA patients on MRA treatment.
Biochemical and hormonal assays
Plasma renin concentration and serum aldosterone levels were measured as previously described [3, 15]. Serum sodium and potassium and 24-h urinary sodium and potassium concentrations were measured by integrated chip technology (using ARCHITECT cSystem analyzers, Abbott Laboratories). The normal range of potassium levels in our lab was between 3.2 and 4.8 mEq/L. Hemolysis was detected by a photometric method (using an ARCHITECT cSystem analyzer).
Statistical analysis
Statistical analysis was performed using the SPSS software package (SPSS Inc., version 17.0, Chicago, USA). The Wilcoxon test was performed accordingly to compare differences in continuous parameters between paired-samples (i.e., baseline vs. follow-up evaluation values). The Mann-Whitney U test was performed to compare differences in continuous parameters between different groups (i.e., normotensive normokalemic and hyperkalemic MRA-treated PA patients). Bonferroni adjustment for multiple comparisons was also performed.
Spearman correlation coefficient was used to evaluate correlations between continuous variables. Median (min, max) values were used to express the results and a two-tailed p value < 0.05 was considered statistically significant.
Results
The baseline, 1-month, and 6-month follow-up characteristics and laboratory measurements of the study population (n = 17) are shown in Table 1. The characteristics and the biochemical measurements of the normotensive, normokalemic and hyperkalemic MRA-treated PA patients are depicted in Table 2.
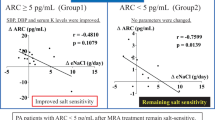
Serum potassium levels were within normal range, although slightly increased in normokalemic MRA-treated PA patients compared to normotensive subjects (p = 0.001). Hyperkalemic MRA-treated PA patients had lower 24-h urinary sodium excretion (110.13 (34.30–139.20) mEq/day) compared to the 24-h urinary sodium excretion of the normotensive (146 (79–260) mEq/day, p = 0.001) and normokalemic MRA-treated PA patients (143.25 (47–253) mEq/day, p = 0.006), indicating that these patients were on relative salt restriction. Normokalemic and hyperkalemic MRA-treated patients had a higher aldosterone-to-renin ratio compared to normotensive subjects (p < 0.05) (Table 2).
Multiple comparisons adjustment was also performed and showed similar results except for basal aldosterone-to-renin ratio between normotensive subjects and hyperkalemic MRA-treated patients. Contrary to comparisons with the Mann-Whitney test, multiple comparisons with the Bonferonni test did not show a statistically significant difference between the two abovementioned groups, probably, because of the small population size (17 patients) and the huge range of values.
Controlled (usual relatively salt-restricted diet plus 4 g salt/day) salt intake for a month resulted in an increase in 24-h urinary sodium excretion (195.20 (120.30–275.20) mEq/day, p < 0.001). This increase, though attenuated, was sustained after 6 months of follow-up, during which, patients stopped controlled salt intake and were simply instructed to maintain a free sodium intake resulting in an increased sodium excretion (175 (95.50–215) mEq/day, p < 0.001) compared to baseline. Serum sodium levels both at one and at 6 months of salt repletion did not show a significant change compared to baseline (p = 0.34, p = 0.37) (Fig. 2).
Serum sodium and potassium levels and 24-h urinary sodium and potassium excretion under relative salt restriction (RRS), at 1 month of controlled (usual salt-restricted diet plus 4 g/day) salt supplementation (CS) and at 6 months on instructions for free dietary salt intake (FS). Continuous variables are shown as median
Most importantly, hyperkalemic MRA-treated PA patients demonstrated a significant decrease in serum potassium levels after the implementation of 1 month of controlled salt intake (4.6 (3.8–5.1) mEq/L) compared to baseline (5.2 (5–5.7) mEq/L, p < 0.001). This normalization of serum potassium levels lasted as much as 6 months after instructions to patients to stop controlled salt intake and simply continue free salt consumption (4.5 (4.2–4.8) mEq/L, p < 0.001, compared to baseline). The reduction in serum potassium was accompanied by a significant increase in 24-h urinary potassium excretion (62.25 (40.69–97.0) mEq/day] compared to baseline (54.0 (23.28–79.60) mEq/day, p = 0.001), which remained high at 6 months (59.0 (37.30–85.40) mEq/day, p = 0.12) (Fig. 2).
Renin levels were higher in hyperkalemic compared to normokalemic MRA-treated PA patients indicating either more effective mineralocorticoid receptor blockade or/and moderate salt restriction.
Salt supplementation in hyperkalemic MRA-treated PA patients resulted in a significant decrease in plasma renin concentrations at 1-month compared to baseline (p = 0.002), and this was sustained at the 6-month follow-up (p = 0.002). This was followed by a concomitant reduction of aldosterone concentrations at the 1- (p = 0.001) and 6-month follow-ups (p = 0.001) compared to the initial salt-restricted period (Fig. 3).
No statistically significant alteration was observed in either SBP or DBP in hyperkalemic MRA-treated PA patients after controlled salt supplementation or free salt intake and all 17 participants remained normotensive. Neither 1 month nor 6 months of salt supplementation resulted in a significant increase in the body weight or BMI of the study participants. Furthermore, no difference was found, when RRS, CS, and FS e-GFRs were compared. No correlations were found between creatinine levels or e-GFR and serum potassium levels, while e-GFR was, as expected, negatively correlated with age.
Discussion
This prospective study showed that free salt intake in relatively salt-restricted mildly hyperkalemic MRA-treated PA patients can normalize potassium levels for as long as 7 months of follow-up. Patients’ BP, e-GFR, body weight, and BMI remained unchanged after repletion of salt intake, suggesting safe use of free dietary salt consumption. Their baseline relatively reduced salt intake was confirmed by 24-h urinary sodium excretion, which was much lower compared to the 24-h urinary sodium excretion of normotensive and normokalemic MRA-treated PA patients. In support of these findings, a recent study showed that healthy Greek adults had much higher 24-h urinary sodium excretion (175 mEq/day) than our hyperkalemic MRA-treated PA patients [18].
Moreover, both normokalemic and hyperkalemic MRA-treated patients had higher basal (before the FDST confirmatory test) aldosterone-to-renin ratio compared to normotensive subjects. This finding is in accordance with the results of Maiolino et al. which showed that the aldosterone-to-renin ratio was as accurate as that of post-confirmatory tests and thus, can simplify the diagnostic workup [19].
MRAs have been used as an effective treatment for PA for many decades. A spironolactone dose of 50 mg/day is considered sufficient for most PA patients, in terms of SBP/DBP control, albuminuria reduction and regression of left ventricular hypertrophy of the heart [8, 20]. Larger MRA doses may be occasionally required to sufficiently antagonize aldosterone effects on sodium and water retention, as well as on cardiac and vascular fibrosis [21].
The usual practice in the medical treatment of PA-driven hypertension is the addition of a low MRA dose to the existing classical antihypertensive treatment, which is titrated according to serum potassium levels, without simultaneous plasma renin measurements. However, serum potassium levels should not be considered an ideal index for MRA dose adjustments and, in fact, may lead to undertreatment of PA patients. In our study, we employed appropriate MRA doses and considered the restoration of both serum potassium and plasma renin levels within the normal range as the most appropriate guides for MRA dosage adjustment. MRA dosage titration according to plasma renin levels in PA patients has recently been addressed by Hundemer et al. [22] in PA patients under MRAs compared to age-matched patients with essential hypertension and comparable CV risk profiles and BP. The excess risk for cardiovascular events and mortality was limited to PA patients whose renin activity remained suppressed despite MRA treatment, whereas PA patients who were treated with higher MRA doses and had unsuppressed renin activity had insignificant excess risk. Thus, titration of MRAs in order to raise suppressed renin activity could mitigate excess CV risk.
Although treatment with MRA can induce hyperkalemia, it is generally associated with improved survival in patients with low-output heart failure (HF), while recent studies have shown that MRAs are safe even in subgroups at high risk of developing hyperkalemia, provided that potassium and creatinine levels are frequently monitored [11, 23,24,25,26,27,28]. Post hoc analyses of the EPHESUS study demonstrated that 25–50 mg/day eplerenone was associated with a 4.4% and a 1.6% absolute increase in the incidence of mild (K > 5.5 mEq/L) and marked hyperkalemia (K > 6.0 mEq/L), respectively [29]. In our study, we observed mild asymptomatic hyperkalemia at a higher incidence (9.7%) in PA patients, which might be ascribed to long-term administration of appropriate MRA dosage, based on BP and renin level findings.
MRA-induced hyperkalemia may be attributed to different causes. The EPHESUS study identified low e-GFR (less than 60 ml/min/1.73 m2) and elevated baseline serum potassium, the presence of diabetes mellitus and prior use of antiarrhythmic drugs as major predictors of marked hyperkalemia [29]. Other risk factors include advanced age (≥ 75 years), coadministration of MRA with ACE-I or ARBs, increased dietary potassium intake, and consumption of potassium-containing supplements [23, 25].
Daily sodium intake can be another factor related to potassium excretion in urine, which has been almost completely ignored so far. Our data from the two different control groups (normotensive subjects and normokalemic MRA-treated PA patients), who were on a relatively higher sodium intake diet compared to the MRA-treated hyperkalemic PA patients, may suggest that the development of hyperkalemia could be attributed to the relatively low sodium intake. Potassium excretion in urine depends directly on the amount of sodium that reaches the DCT and the CCD, which are the main targets of aldosterone action [8, 30, 31]. Thus, the reduced amount of filtered sodium in the kidneys may directly affect potassium excretion, which is independent of MRA administration in PA patients.
A proportion of PA patients treated with MRAs may have sodium deficit for the following reasons. First, current recommendations encourage hypertensive patients to minimize their salt intake, as this can decrease BP and reduce the risk of stroke and fatal coronary heart disease [32,33,34]. The WHO and the European Society of Hypertension/European Society of Cardiology (ESH/ESC) have suggested an upper daily sodium intake of 2000 mg (~ 5 g salt), whereas the American Heart Association (AHA) suggests as low as 1500 mg (3.75 g salt) in hypertensive patients [16, 35, 36]. Second, MRA may aggravate sodium deficit by inducing natriuresis by exerting an effect on the renal epithelial sodium channels (ENaC), sodium chloride co-transporters (NCC) and Na-K-Cl co-transporters (NKCC) [11].
The latter is supported by the results of this study, firstly because the basal 24-h urinary sodium of hyperkalemic MRA-treated PA patients was low, suggesting that they were on a relatively salt-restricted diet, and secondly, since both controlled salt supplementation and free daily dietary salt intake induced a significant increase in 24-h urinary sodium and potassium excretion in the PA patients, which was accompanied by restoration of serum potassium levels to normal, while serum sodium levels remained unaffected. Free salt consumption also induced a significant decrease of plasma renin as well as serum aldosterone levels in MRA-treated PA patients. Most importantly, the changes we observed occurred despite the fact that arterial BP remained unaffected in the MRA-treated PA patients. In support of these observations is a recent study by Ghazi et al., which showed that the antihypertensive effect of spironolactone is positively related to urinary sodium excretion (> 200 mEq/day), independently of circulating aldosterone concentrations [37]. This shows that sufficient salt intake may facilitate MRA action provided that it is given in appropriate doses. Further, our results imply that the kidneys of PA patients are able to manage the free sodium intake without this influencing arterial BP levels.
Among the limitations of our study is the small number of hyperkalemic MRA-treated participants, the lack of a standardized non-cumbersome method to evaluate daily sodium intake alternative to 24-h urine collections, the use of radioimmunoassay instead of HPLC-tandem mass spectrometry for the measurement of aldosterone, and the relatively short period of follow-up. Despite these limitations, this is the first study that addresses the importance of adequate salt intake in PA patients under MRA blockade and potentially offers a novel, interesting, simple and cost-effective alternative approach to the management of moderate hyperkalemia in MRA-treated PA patients minimizing the need to adjust MRA dosage or use of other drugs that reduce serum potassium levels. Larger long-range prospective studies should be conducted to clarify the potential long-term effects of salt intake on serum potassium, BP, and body weight, as well as risk for cardiovascular events or renal stone formation in these patients.
References
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Mattarello MJ, Moretti A, Palumbo G, Parenti G, Porteri E, Semplicini A, Rizzoni D, Rossi E, Boscaro M, Pessina AC, Mantero F, PAPY Study Investigators (2006) A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 48(11):2293–2300
Markou A, Sertedaki A, Kaltsas G, Androulakis II, Marakaki C, Pappa T, Gouli A, Papanastasiou L, Fountoulakis S, Zacharoulis A, Karavidas A, Ragkou D, Charmandari E, Chrousos GP, Piaditis GP (2015) Stress-induced aldosterone hyper-secretion in a substantial subset of patients with essential hypertension. J Clin Endocrinol Metab 100(8):2857–2864. https://doi.org/10.1210/jc.2015-1268
Papanastasiou L, Markou A, Pappa T, Gouli A, Tsounas P, Fountoulakis S, Kounadi T, Tsiama V, Dasou A, Gryparis A, Samara C, Zografos G, Kaltsas G, Chrousos G, Piaditis G (2014) Primary aldosteronism in hypertensive patients: clinical implications and target therapy. Eur J Clin Investig 44(8):697–706. https://doi.org/10.1111/eci.12286
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ (2005) Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiology 45(8):1243–1248. https://doi.org/10.1016/j.jacc.2005.01.015
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, Mulatero P (2018) Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 6(1):41–50. https://doi.org/10.1016/S2213-8587(17)30319-4
Lim PO, Jung RT, MacDonald TM (1999) Raised aldosterone to renin ratio predicts antihypertensive efficacy of spironolactone: a prospective cohort follow-up study. Br J ClinPharmacol 48(5):756–760
Parthasarathy HK, Menard J, White WB, Young WF, Jr., Williams GH, Williams B, Ruilope LM, McInnes GT, Connell JM, MacDonald TM. A (2011) A double-blind, randomized study comparing the antihypertensive effect of eplerenone and spironolactone in patients with hypertension and evidence of primary aldosteronism. J Hypertens 29(5):980–990. https://doi.org/10.1097/HJH.0b013e3283455ca5
Funder JW (2013) Primary aldosteronism and low renin hypertension: a continuum? Nephrol Dial Transplant 28(7):1625–1627. https://doi.org/10.1093/ndt/gft052
Karagiannis A, Tziomalos K, Papageorgiou A, Kakafika AI, Pagourelias ED, Anagnostis P, Athyros VG, Mikhailidis DP (2008) Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert OpinPharmacother9(4):509–515. https://doi.org/10.1517/14656566.9.4.509
Wada N, Shibayama Y, Umakoshi H, Ichijo T, Fujii Y, Kamemura K, Kai T, Sakamoto R, Ogo A, Matsuda Y, Fukuoka T, Tsuiki M, Suzuki T, Naruse M (2017) Hyperkalemia in both surgically and medically treated patients with primary aldosteronism. J Hum Hypertens 31(10):627–632. https://doi.org/10.1038/jhh.2017.38
Desai A (2008) Hyperkalemia associated with inhibitors of the renin-angiotensin-aldosterone system: balancing risk and benefit. Circulation 118(16):1609–1611. https://doi.org/10.1161/CIRCULATIONAHA.108.807917
Williams JS, Williams GH, Raji A, Jeunemaitre X, Brown NJ, Hopkins PN, Conlin PR (2006) Prevalence of primary hyperaldosteronism in mild to moderate hypertension without hypokalaemia. J Hum Hypertens 20(2):129–136. https://doi.org/10.1038/sj.jhh.1001948
Christensen BM, Perrier R, Wang Q, Zuber AM, Maillard M, Mordasini D, Malsure S, Ronzaud C, StehleJC RBC, Hummler E (2010) Sodium and potassium balance depends on αENaC expression in connecting tubule. J Am Soc Nephrol 21(11):1942–1951. https://doi.org/10.1681/ASN.2009101077
Perrier R, Boscardin E, Malsure S, Sergi C, Maillard MP, Loffing J, Loffing-Cueni D, Sørensen MV, Koesters R, Rossier BC, Frateschi S, Hummler E (2016) Severe salt-losing syndrome and hyperkalemia induced by adult nephron-specific knockout of the epithelial sodium channel α-subunit. J Am Soc Nephrol 27(8):2309–2318. https://doi.org/10.1681/ASN.2015020154
Markou A, Pappa T, Kaltsas G, Gouli A, Mitsakis K, Tsounas P, Prevoli A, Tsiavos V, Papanastasiou L, Zografos G, Chrousos GP, Piaditis GP (2013) Evidence of primary aldosteronism in a predominantly female cohort of normotensive individuals: a very high odds ratio for progression into arterial hypertension. J Clin Endocrinol Metab 98(4):1409–1416. https://doi.org/10.1210/jc.2012-3353
Eckel RH, JakicicJM AJD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TA, Yanovski SZ, Kendall KA, Morgan LC, Trisolini MG, Velasco G, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF (2014) American College of Cardiology/American Heart Association Task Force on Practice Guidelines.2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation 129(25 Suppl 2):S76–S99. https://doi.org/10.1161/01.cir.0000437740.48606.d1
Dolci A, Panteghini M (2014) Harmonization of automated hemolysis index assessment and use: is it possible? Clin Chim Acta 432:38–43. https://doi.org/10.1016/j.cca.2013.10.012
Vasara E, Marakis G, Breda J, Skepastianos P, Hassapidou M, Kafatos A, Rodopaios N, Koulouri AA, Cappuccio FP (2017) Sodium and potassium intake in healthy adults in Thessaloniki Greater Metropolitan Area-The Salt Intake in Northern Greece (SING) Study. Nutrients 9(4):E417. https://doi.org/10.3390/nu9040417
Maiolino G, Rossitto G, Bisogni V, Cesari M, Seccia TM, Plebani M, Rossi GP, PAPY Study Investigators (2017) Quantitative Value of aldosterone-renin ratio for detection of aldosterone-producing adenoma: the Aldosterone-Renin Ratio for Primary Aldosteronism (AQUARR) Study. J Am Heart Assoc 6(5):e005574. https://doi.org/10.1161/JAHA.117.005574
Ori Y, Chagnac A, Korzets A, Zingerman B, Herman-Edelstein M, Bergman M, Gafter U, Salman H (2013) Regression of left ventricular hypertrophy in patients with primary aldosteronism/low hypertension on low dose spironolactone. Nephrol Dial Transplant 28(7):1787–1793. https://doi.org/10.1093/ndt/gfs587
Bansal S, Lindenfeld J, Schrier RW (2009) Sodium retention in heart failure and cirrhosis: potential role of natriuretic doses of mineralocorticoid antagonist? Circ Heart Fail 2(4):370–376. https://doi.org/10.1161/CIRCHEARTFAILURE.108.821199
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A (2017) Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endrocrinol 6(1):51–59. https://doi.org/10.1016/S2213-8587(17)30367-4
Weir MR, Rolfe M (2010) Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin J Am SocNephrol 5(3):531–548. https://doi.org/10.2215/CJN.07821109
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA (2004) Rates of hyperkalemia after publication of the randomized aldactone evaluation study. N Engl J Med 351(6):543–551
Vardeny O, Claggett B, Anand I, Rossignol P, Desai AS, Zannad F, Pitt B, Solomon SD (2014) Randomized Aldactone evaluation study (RALES) investigators. Incidence, predictors, and outcomes related to hypo- and hyperkalemia in patients with severe heart failure treated with a mineralocorticoid receptor antagonist. Circ Heart Fail 7(4):573–579. https://doi.org/10.1161/CIRCHEARTFAILURE
Khosla N, Kalaitzidis R, Bakris GL (2009) Predictors of hyperkalemia risk following hypertension control with aldosterone blockade. Am J Nephrol 30(5):418–424. https://doi.org/10.1159/000237742
Pelliccia F, Patti G, Rosano G, Greco C, Gaudio C (2014) Efficacy and safety of eplerenone in the management of mild to moderate arterial hypertension: systematic review and meta-analysis. Int J Cardiol 177(1):219–228. https://doi.org/10.1016/j.ijcard.2014.09.091
Eschalier R, McMurray JJ, Swedberg K, van Veldhuisen DJ, Krum H, PocockSJ SH, Vincent J, Rossignol P, Zannad F, Pitt B (2013) Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure). J Am Coll Cardiol 62(17):1585–1593. https://doi.org/10.1016/j.jacc.2013.04.086
Pitt B, Bakris G, Ruilope LM, DiCarlo L, Mukherjee R (2008) Serum potassium and clinical outcomes in the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS). Circulation 118(16):1643–1650. https://doi.org/10.1161/CIRCULATIONAHA.108.778811
Lai L, Feng X, Liu D, Chen J, Zhang Y, Niu B, Gu Y, Cai H (2012) Dietary salt modulates the sodium chloride cotransporter expression likely through an aldosterone-mediated WNK4-ERK1/2 signaling pathway. Pflugers Arch 463(3):477–485. https://doi.org/10.1007/s00424-011-1062-y
Schiessl IM, Rosenauer A, Kattler V, Minuth WW, Oppermann M, Castrop H (2013) Dietary salt intake modulates differential splicing of the Na-K-2ClcotransporterNKCC2. Am J Physiol Renal Physiol 305(8):F1139–F1148. https://doi.org/10.1152/ajprenal.00259.2013
Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Li W, Lu Y, Yi S, Rensheng L, Iqbal R, Mony P, Yusuf R, Yusoff K, Szuba A, Oguz A, Rosengren A, Bahonar A, Yusufali A, Schutte AE, Chifamba J, Mann JF, Anand SS, Teo K, Yusuf S, PURE, EPIDREAM and ONTARGET/TRANSCEND Investigators (2016) Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet 388(10043):465–475. https://doi.org/10.1016/S0140-6736(16)30467-6
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ (2013) Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 346:f1326. https://doi.org/10.1136/bmj.f1326
Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M (1996) Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. BMJ 312(7041):1249–1253
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, TamargoJL TM, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, HitijJB CM, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA (2013) ESH/ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219. https://doi.org/10.1093/eurheartj/eht151
Vos M, Wylie-Rosett J, Kris-Etherton P (2016) American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council. Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: a Scientific Statement From the American Heart Association. Circulation 134(22):e505–e529. https://doi.org/10.1161/CIR.0000000000000462
Ghazi L, Dudenbostel T, Lin CP, Oparil S, Calhoun DA (2016) Urinary sodium excretion predicts blood pressure response to spironolactone in patients with resistant hypertension independent of aldosterone status. J Hypertens 34(5):1005–1010. https://doi.org/10.1097/HJH.0000000000000870
Author information
Authors and Affiliations
Contributions
SF examined the patients and wrote the article. LP organized the study, analyzed the data, and wrote the article. NV collected the data. TK carried out laboratory work. AM collected the data. GC contributed intellectually and edited the article. GP designed the study and assigned duties. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all subjects.
Ethical approval
All procedures performed were in accordance with the ethical standards of General Hospital of Athens ‘G. Gennimatas’ research committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fountoulakis, S., Papanastasiou, L., Voulgaris, N. et al. Salt intake in mineralocorticoid receptor antagonist-treated primary aldosteronism: foe or ally?. Hormones 19, 223–232 (2020). https://doi.org/10.1007/s42000-019-00167-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-019-00167-9