Abstract
Background
Risk factors for malignant tumours of the central nervous system (CNS) are largely unknown.
Methods
We pooled six European cohorts (N = 302,493) and assessed the association between residential exposure to nitrogen dioxide (NO2), fine particles (PM2.5), black carbon (BC), ozone (O3) and eight elemental components of PM2.5 (copper, iron, potassium, nickel, sulfur, silicon, vanadium, and zinc) and malignant intracranial CNS tumours defined according to the International Classification of Diseases ICD-9/ICD-10 codes 192.1/C70.0, 191.0–191.9/C71.0–C71.9, 192.0/C72.2–C72.5. We applied Cox proportional hazards models adjusting for potential confounders at the individual and area-level.
Results
During 5,497,514 person-years of follow-up (average 18.2 years), we observed 623 malignant CNS tumours. The results of the fully adjusted linear analyses showed a hazard ratio (95% confidence interval) of 1.07 (0.95, 1.21) per 10 μg/m³ NO2, 1.17 (0.96, 1.41) per 5 μg/m³ PM2.5, 1.10 (0.97, 1.25) per 0.5 10−5m−1 BC, and 0.99 (0.84, 1.17) per 10 μg/m³ O3.
Conclusions
We observed indications of an association between exposure to NO2, PM2.5, and BC and tumours of the CNS. The PM elements were not consistently associated with CNS tumour incidence.
Similar content being viewed by others
Introduction
Over the past decades, the incidence of malignant neoplasms of the brain and central nervous system (CNS) has risen in most parts of the world, with the highest age-standardised rates observed in Western European countries [1]. Globally, CNS tumours are still relatively rare with an age-standardised rates of 3.9 and 3.0 per 100,000 in men and women, respectively [2]. The consequences are, however, disproportionally severe because of the disabling nature of the disease and the high rate of mortality among CNS cancer patients [1]. The observed rise in incidence rates over the past decades reflects to some extent improved imaging techniques, diagnosis, cancer registrations, and sources of information, but also suggests a potential causal role of environmental and lifestyle factors.
Risk factors for malignant CNS tumours are largely unknown. The CNS tumour incidence varies according to age, sex, and ethnicity and a small fraction of all CNS tumours have been ascribed to hereditary genetic conditions [3, 4]. Exposure to ionising radiation is classified as a risk factor [5], and occupational exposures such as arsenic, lead, mercury, petroleum, and pesticides have been associated with CNS cancer [6, 7]. The use of mobile phones has also been investigated in numerous studies, but the current evidence does not indicate an association [8]. Overweight and obesity in both men and women [9], as well as female reproductive hormones and use of hormone therapy, are also suspected of playing a role, but to date the current literature is ambiguous regarding tumour subtypes and specific hormone therapy preparation [10, 11].
Air pollution with particulate matter (PM) has been classified as a human carcinogen based on evidence of associations with lung cancer by the International Agency for Research on Cancer (IARC) [12], and a few previous studies have investigated the association between outdoor air pollution and intracranial CNS tumours with mixed conclusions. The largest to date, a Danish, nationwide, register-based case-control study, observed an association between nitrogen dioxide (NO2), PM with a diameter of ≤ 2.5 µm (PM2.5), black carbon (BC) exposure and malignant non-glioma tumours of the brain and between NO2 exposure and meningioma [13]. The European Study of Cohorts for Air Pollution Effects (ESCAPE) study reported indicative evidence of an increased risk of malignant brain tumours with higher PM2.5 absorbance (a marker for BC) exposure [14]. Findings from the Danish Nurse Cohort study were suggestive of an increased risk of total brain tumours with higher NO2 and PM2.5 exposure [15].
Despite declining levels of air pollution over the past decades in Europe and North-America, adverse health effects are still observed in recent epidemiological studies, and more knowledge concerning the strength of the association and the contribution from specific sources and components is needed for risk regulation. In the present study, we aim to investigate the association between long-term exposure to NO2, PM2.5, BC, ozone (O3), and eight elemental components of PM2.5 (copper, iron, potassium, nickel, sulfur, silicon, vanadium, and zinc) and the risk of CNS tumours in the Effects of Low-level Air Pollution: a Study in Europe (ELAPSE). The ELAPSE collaboration builds on and extends ESCAPE by pooling data across cohorts and applying a more comprehensive standardised exposure assessment, and a longer follow-up period.
Methods
Study population
The ELAPSE collaboration pooled data from nine European cohorts. Key covariates were identified from each cohort and harmonised, and the data were stored on a secure server at Utrecht University. Of the nine pooled cohorts, six were eligible for the analyses of malignant CNS tumour incidence: Cardiovascular Effects of Air Pollution and Noise in Stockholm (CEANS)—which is the collective name of four sub-cohorts (Swedish National Study on Aging and Care in Kungsholmen [SNAC-K] [16]; Stockholm Screening Across the Lifespan Twin study [SALT] [17]; The Stockholm Cohort of 60-year-olds [Sixty] [18]; and Stockholm Diabetes Prevention Programme [SDPP] [19]); the Danish Diet, Cancer and Health cohort (DCH) [20]; the Danish Nurse Cohort (DNC) [21]; the Dutch European Investigation into Cancer and Nutrition (EPIC-NL)—consisting of the two sub-cohorts EPIC-Monitoring Project on Risk Factors and Chronic Diseases in the Netherlands (EPIC-MORGEN) and (EPIC-Prospect) [22]; the Etude Epidémiologique auprés de femmes de la Mutuelle Générale de l’Education Nationale (E3N or EPIC-France) [23]; and the Austrian Vorarlberg Health Monitoring and Prevention Programme (VHM&PP) [24]. All six cohorts contained baseline information on age, sex, smoking status, amount and duration of smoking in current smokers (E3N and VHM&PP only in classes), body mass index (BMI), employment status, and area-level socio-economic status (SES). We included all participants who were free of cancer at baseline (with the exception of non-melanoma skin cancer). Each included cohort and the covariates have been described in detail previously [25].
Exposure assessment
The model developed for assessing air pollution exposure and its validation has been described in detail elsewhere [26, 27]. In brief, Europe-wide hybrid land-use regression (LUR) models were developed, which incorporated as predictors satellite observations, chemistry and transport model (CTM) estimates, land use, and road variables. For the modelling of PM2.5, NO2 and O3 (warm season), routine monitoring data (2010 AirBase) maintained by the European Environmental Agency (EEA) were used and for black carbon (BC) and PM2.5 elemental composition ESCAPE monitoring data (2009–2010) were applied [28]. For the PM composition models, Supervised linear regression (SLR) and random forest algorithms were used for eight components representing major air pollution sources: Cu, Fe and Zn (non-tailpipe traffic emissions such as brake and tyre wear), S (secondary inorganic aerosols from long-range transported sulfur containing fuel combustion), Ni and V (mixed oil burning/industry emissions), Si (crustal material), and K (biomass burning) [27]. For PM2.5, BC, NO2 and O3 we only used SLR. Negative (SLR) predictions of PM components were truncated to zero, and a few unrealistically high predictions at close distance to industrial sources to a maximum modelled concentration for each element.19 No truncation was needed for the exposures modelled with random forest. The SLR and random forest models explained within-area variability similarly [27], and we therefore interpret the two models equally. We assigned exposures from the produced air pollution raster surfaces (100 x 100 m spatial resolution) to the geocoded baseline residential addresses of all cohort members.
Outcome
Participants were followed up in national cancer registries, death certificates or medical records with the exception of participants in the E3N cohort, which relied on self-reports from biannual questionnaires or death certificates. These were confirmed through pathological reports and reviewed by an oncologist. We defined malignant intracranial tumours according to the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) codes C70.0 (cerebral meninges), C71.0–C71.9 (brain), C72.2–C72.5 (cranial nerves) and correspondingly the International Classification of Diseases and Related Health Problems, 9th Revision (ICD-9) codes 192.1, 191.0–191.9, and 192.0.
Statistical analysis
We modelled the association between the air pollutants and malignant CNS tumours using Cox proportional hazards models with age as the underlying time-scale. Each cohort member was censored at time of first occurrence of any cancer other than in the CNS, date of death, emigration, loss to follow-up, or at the end of follow-up. We modelled each pollutant as a linear function and presented hazard ratios (HRs) for increments of 10, 5, 0.5 and 10 µg/m3 for NO2, PM2.5, BC and O3, respectively. The HRs for PM components were presented for increments of 5 ng/m3 Cu, 100 ng/m3 Fe, 50 ng/m3 K, 1 ng/m3 Ni, 200 ng/m3 S, 100 ng/m3 Si, 2 ng/m3 V, and 10 ng/m3 Zn. We included strata per sex and individual (sub) cohort to account for baseline hazard heterogeneity across the cohorts and to relax the proportional hazards assumption.
We defined three confounder models á priori: (1) accounting for age (underlying time-scale), (sub) cohort ID (strata), sex (strata), and adjustment for year of enrolment to take into account time-trends in exposure and outcome; (2) further adjusted for marital status (married/cohabiting, divorced, single, widowed), employment status (yes vs. no), smoking status (never, former, current), duration (years of smoking) and intensity (cigarettes/day) for current smokers, and BMI ( < 18.5, 18.5–24, 25–29, and 30+ kg/m2); (3) (main model) further adjusted for SES at the area-level, which we defined as mean income in 2001—most consistently available variable and year across cohorts. The spatial scale of these areas varied from smaller neighbourhoods and city districts (CEANS, EPIC-NL, E3N) to municipalities (DNS, DCH, and VHM&PP). We excluded participants with incomplete information on model 3 variables from all analyses. We evaluated the shape of the concentration-response function by natural cubic splines (3 degrees of freedom).
Sensitivity analyses included (1) alternative exposure definitions by (a) back-extrapolating to the baseline address for all cohort members and (b) time-varying air pollution exposure extrapolated according to address history from enrolment to end of follow-up in cohorts with the available information (excluding DNC and E3N). For the time-varying analyses, we specified a 1-year calendar time-period strata to handle time-trends in air pollution and intracranial CNS tumours. The extrapolation estimated concentrations from the Danish Eulerian Hemispheric Model (DEHM), which includes hourly values of a number of chemical species, averaged into monthly concentrations across Europe at 26 × 26 km spatial resolution [29]. We applied the trends predicted by the DEHM for NO2, PM2.5, BC, and O3 to calculate annual average concentrations for all years from baseline to the end of follow-up, allowing different spatial trends within Europe, and used the absolute difference and the ratio between the baseline and 2010 periods. (2) We additionally performed two-pollutant models to test the sensitivity of the estimates of one pollutant to inclusion of others. For the elemental components, we performed two-pollutant models with PM2.5 mass and NO2—the latter representing traffic exhaust emission. (3) We investigated potential effect measure modification by sex, BMI (<25, 25–29, 30+ kg/m2), and smoking status, by including an interaction term in the model tested by the Wald test. (4) Lastly, we investigated the sensitivity of the pooled effect estimates to exclusion of single cohorts.
We evaluated violation of the proportional hazards assumption of the Cox models for all covariates by test of a non-zero slope in a generalised linear regression of the scaled Schoenfeld residuals on time. We performed all analyses in R version 3.4.0.
Results
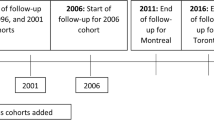
Cohorts were recruited between 1985 and 2005 with a follow-up until 2011 to 2015 (Table 1). In total, we included 302,493 participants of whom 623 developed a malignant intracranial CNS tumour during 5,497,514 person-years of follow-up. Of the 623 cases, 593 originated in the brain and only few in the cerebral meninges (N = 27) or the cranial nerves (N = 3). The mean age at baseline for the pooled cohort was 48.2 years ranging from 41.7 to 72.5 years in the individual (sub)cohorts. The mean age at baseline for cases was slightly higher (mean 52.0 years, SD 10.9). The main air pollution exposures varied across the (sub)cohorts as a consequence of differences in climate, urbanicity, and sources (area-level of industrialisation, population density, road density, types of vehicles (diesel vs. gasoline), abatement strategies etc.), with the highest levels in the more southern cohorts. Especially for BC and NO2, contrasts within cohorts were substantial (Fig. S1). Particularly BC and NO2 were highly correlated in all cohorts and PM2.5 was moderately to highly correlated with BC and NO2. O3 was negatively correlated with PM2.5 and with especially NO2 and BC (Table S1). For the PM elemental components, all concentrations except PM2.5 Ni, Si, and V were lower in the Northern compared to more Southern cohorts. The two exposure model algorithms provided similar concentrations overall, however, with large differences within individual cohorts (Fig. S2).
The baseline characteristics of each (sub)cohort and the pooled cohort are presented in Table 2. The pooled cohort consisted of 66% women, 42% were overweight or obese, 29% were not employed, and 72% were married or cohabiting at baseline. The fraction of current smokers was 24%, ranging from 13% in the French E3N cohort to 37% in the DNC-1993. The mean income at the area-level varied considerably across cohorts, with the lowest levels observed in the French and Dutch cohorts and the highest in the Swedish CEANS cohort.
The results of the linear analyses of air pollutants and malignant CNS tumours with increasing levels of confounder-adjustment are shown in Table 3. In the fully adjusted model 3, we observed a HR of 1.07 (95% confidence interval [CI]: 0.95, 1.21) per increment of 10 µg/m3 NO2, 1.17 (95% CI: 0.96, 1.41) per 5 µg/m3 PM2.5, and 1.10 (95% CI: 0.97, 1.25) per 0.5 10−5m−1 BC. For ozone in the warm season, we observed a HR of 0.99 (95% CI: 0.84, 1.17) per increment of 10 µg/m3. Stricter covariate adjustment increased the HRs for NO2, PM2.5, and BC, especially the inclusion of area-level income (model 3 versus model 2 HRs). The natural cubic splines showed a linear increase in the exposure-response function for PM2.5 and BC (Fig. 1). An indication of a decreasing trend at the end of the exposure range for PM2.5 and BC was found, however, with very wide CIs, related to sparse data. For NO2, a linear increase followed by levelling off at about 20 µg/m3 was found. The HRs for PM2.5 elemental components and splines are provided in Fig. 2 and Supplement Fig. S3. We observed (non-significantly) elevated risks in association with PM2.5 Ni, S, and V predicted by the SLR- and the random forest-model, also after adjustment for PM2.5 and NO2 (Fig. S5). For some elements including S, HRs had wide confidence bounds.
Supplement Table S5 shows the means, standard deviations (SD) and effect estimates of exposures extrapolated to the baseline year of the cohort participants and for the time-varying analysis. In general, the back-extrapolated baseline exposures were higher and more variable than the 2010-concentration, especially for PM2.5 with a mean (SD) of 28.9 (7.8) and 28.4 (8.4) for the difference and ratio method, respectively, compared to a mean of 14.9 (3.2) for the 2010 main exposure model. The effect estimates for the back-extrapolation and the 2010-exposure model did not vary considerably for NO2 and O3, whereas for PM2.5—and to some extent for BC—the HR estimates and confidence intervals for the baseline exposure (expressed for the same increment) were considerably lower than those of the 2010-exposure model. In the time-varying analysis applying exposure extrapolated across the address history, we observed similar effect estimates for PM2.5 compared to the 2010-exposure model. The estimates for the time-varying exposure of NO2 and BC were somewhat lower than those of the main 2010-exposure. The effect estimate for PM2.5 and CNS tumours was not sensitive to the inclusion of co-pollutants (Figs. S4 and S5). The association for NO2 was attenuated by the inclusion of PM2.5 and BC. The HR for BC increased with additional adjustment for NO2. Models with BC and NO2 are difficult to interpret because of the high correlation. For O3, a higher HR was observed with additional adjustment for NO2, PM2.5, and BC.
In stratified analyses, the HR for NO2 in relation to malignant CNS tumours was elevated for current smokers with a HR of 1.23 (95% CI: 1.00, 1.52) compared to ex-smokers (HR: 1.07; 95% CI: 0.85, 1.34) and never-smokers (HR: 1.00; 95% CI: 0.85, 1.17) and likewise for BC with corresponding HRs of 1.20 (95% CI: 0.98, 1.47), 1.07 (0.86, 1.33), and 1.07 (95% CI: 0.91, 1.25) (Fig. 3). These differences of HRs across smoking categories were not statistically significant (P-value for interaction >0.23). For PM2.5, we found no differences between smoking categories. For BMI, we observed higher HRs in the category of overweight persons compared to normal weight and obese for both PM2.5 and BC, whereas the HR for O3 was highest in the group of obese persons. The effect estimates for NO2, BC, and O3 were similar for men and women, but for PM2.5 HRs of 1.33 (95% CI: 1.04, 1.74) and 1.07 (95% CI: 0.86, 1.33) was observed in men and women, respectively. All p-values for interaction were above 0.09.
The estimates were generally not sensitive to exclusion of single cohorts (Fig. S6). The highest estimates for NO2 and PM2.5 were observed in a pooled cohort excluding the E3N cohort, whereas we found the highest estimates for BC and O3 when excluding the DCH cohort.
We detected deviation from the proportional hazards assumption for employment status, smoking intensity and duration. A sensitivity analysis incorporating these in strata (grouping intensity per 10 cigarettes per day and the duration in categories per 5 years) did not show results deviating from the main analysis.
Discussion
In this large Europe-wide pooled analysis study, we observed some indication of a higher risk of malignant intracranial CNS tumours with higher exposure to NO2, PM2.5, and BC. None of the eight evaluated elements was consistently associated with CNS tumour incidence.
Our findings are in line with those reported from the ESCAPE study for NO2 and BC, yet with a somewhat lower effect estimate for BC in our study, which was based on a more comprehensive standardised exposure assessment and a longer follow-up period [14]. In ESCAPE, no association between PM2.5 and malignant brain cancers was reported, with a HR of 0.98 (95% CI: 0.62, 1.56) per 5 µg/m3 in the fully adjusted model. Our current effect estimates are much more precise than the ESCAPE estimates, related to longer follow-up and pooling of data. A large, Danish, register-based case-control study, reported an OR of 1.042 (95% CI: 0.992, 1.095) for malignant intracranial tumours per interquartile range (IQR: 10.78 µg/m3) of NO2 and correspondingly, an OR of 1.034 (95% CI: 1.005, 1.065) for BC (IQR: 0.39 µg/m3), and 1.021 (95% CI: 0.926, 1.126) for PM2.5 (IQR: 5.39 µg/m3), respectively [13]. The study also observed indications of differential effects according to tumour subtypes, with stronger associations for PM2.5 and non-glioma tumours of the brain (OR: 1.267, 95% CI: 1.053–1.524 per IQR). The Danish Nurse cohort study reported an increased risk of total brain tumours with higher NO2 and PM2.5 exposure, however, in sub-analyses the increased risk was restricted to benign brain tumours, with no association observed for malignant brain tumours [15].
Air pollution may influence cancer development and progression through mechanisms of oxidative stress and inflammation [30]. PM has been found to exert DNA damage, promotion of cell turnover, and proliferation beyond the respiratory tract by entering the blood circulation [31, 32]. By crossing the blood-brain barrier, particles may enable toxicological damage of the CNS [33]. In addition, when particles are inhaled through the nasal cavity, they affect respiratory and olfactory epithelia, and thereby reach the brain via olfactory receptor neurons or the trigeminal nerve [34, 35]. The CNS may also be adversely affected via an indirect pathway of systemic inflammation, triggering the release of inflammatory mediators from other organs [34].
The findings of our study were strengthened by the relatively large sample size, the detailed information on SES factors at both the individual and the area-level as well as data on individual lifestyle, which were harmonised across the (sub)cohorts specifically for this project. We were thus able to adjust for a range of potential confounders. Compared to the ESCAPE study, we included a more comprehensive standardised hybrid exposure assessment developed within the ELAPSE collaboration, which ensured comparable exposure estimates for the whole study population, and the longer follow-up provided us with approximately 150 additional CNS tumour cases. We were also able to include specific elemental components of fine PM and to perform two-pollutant models to investigate potential inter-dependencies between pollutants due to the large sample size of our study.
Despite the large cohort and long follow-up, the number of cases was modest, consistent with CNS cancer being a relatively rare cancer. As a result, our effect estimates had relatively wide confidence intervals. We did not have access to information on tumour localisation or subtype (histology and morphology) adding to this uncertainty. If air pollution affects tumour subtypes differently, as suggested by some of the previous studies mentioned above, our results could be diluted. Also, underreporting of CNS tumours could bias our results if related to the levels of exposure (i.e., specific to certain areas/hospitals). In addition, we only included primary cancers, but cannot rule out the possibility that some of the cases were misclassified metastases from cancers in other organs. However, generally the completeness and the quality of the cancer registration in each included study is considered high [36,37,38,39]. Because risk factors for CNS cancer are relatively unknown, we cannot exclude residual confounding. The adjustment for individual and area-level SES probably has accounted for some confounding by known and unknown lifestyle factors. For a risk factor to be a confounder, it needs to be linked with air pollution exposure and SES provides a plausible mechanism for such a link. It is important to acknowledge that assigning exposure to air pollution based on a model imposes some degree of misclassification due to uncertainties in input data and because exposure modelled at the residential address is not equivalent to personal exposure [40]. Also, we do not have any information on time-activity patterns, ventilation rates or indoor sources of air pollution. We consider the potential misclassification of exposure associated with these uncertainties to be non-differential with respect to CNS tumour incidence, which would cause bias of the effect estimate towards the null. We also lacked data on more distant air pollution exposures, such as during childhood or adolescence, which could be of relevance to the development of CNS tumours. Also, the exposure model was developed for the year 2010 and applied to the baseline address of the study participants. The time span between baseline and 2010 varied between cohorts from a mean of 7.7 in the CEANS SNAC-K cohort to 20.0 years in E3N (Table S6). Previous studies from Europe have shown that the spatial distributions of NO2, black smoke, and traffic intensities were stable over several years [41,42,43]. Our exposure model was validated and compared for different time points in order to evaluate the stability of the spatial structure [26, 44], and the predictions from the 2010-model showed high correlations with models developed for 2000 and 2005 (2013 for PM2.5) at the European scale. Our sensitivity analysis, where we back-extrapolated exposures to the baseline year of participants, showed lower HRs for PM2.5 compared to the 2010 exposure. This probably reflects that the exposures in 2010 were lower than at baseline resulting in smaller contrasts (on the absolute scale) [45]. Also, some degree of misclassification as a result of back-extrapolation may be at play. The cohorts selected for the ELAPSE study represent areas in Europe within the lower end of the exposure range. Thus, the results might not be generalised to populations exposed to higher levels of air pollution.
Concentration levels of the studied major air pollutants except ozone have declined over the past decades in North-America and Europe and increased in some other (Asian) countries. The Incidence rates of CNS tumours are generally increasing. The opposite temporal trends is consistent with air pollution being a relatively weak risk factor among all potential determinants of CNS tumour incidence. Temporal trends of disease incidence over years is very complicated as many factors change, including diagnostic procedures, access to health care, socio-economic conditions, lifestyle, work conditions and the environment.
In conclusion, the results of the present study may indicate a role of long-term ambient air pollution in the development of malignant CNS tumours—even at relatively low exposure levels of air pollution.
Data availability
The exposure maps are available on request from Dr Kees de Hoogh (c.dehoogh@swisstph.ch). The cohort data is not available for sharing due to strict national data protection regulations and the General Data Protection Regulation of the European Union. The ELAPSE study protocol is available at http://www.elapseproject.eu/. A detailed statistical analysis plan is available on reasonable request from the corresponding author (ullah@cancer.dk).
References
Patel AP, Fisher JL, Nichols E, Abd-Allah F, Abdela J, Abraha HN, et al. Global, regional, and national burden of brain and other CNS cancer, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:376–93.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Barnholtz-Sloan JS, Ostrom QT, Cote D. Epidemiology of brain tumors. Neurol Clin. 2018;36:395–419.
Hemminki K, Tretli S, Olsen JH, Tryggvadottir L, Pukkala E, Sundquist J, et al. Familial risks in nervous system tumours: joint Nordic study. Br J Cancer. 2010;102:1786–90.
Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, et al. The epidemiology of glioma in adults: a "state of the science" review. Neuro Oncol. 2014;16:896–913.
Navas-Acién A, Pollán M, Gustavsson P, Plato N. Occupation, exposure to chemicals and risk of gliomas and meningiomas in Sweden. Am J Ind Med. 2002;42:214–27.
Baldi I, De Graaf L, Bouvier G, Gruber A, Loiseau H, Meryet-Figuiere M, et al. Occupational exposure to pesticides and central nervous system tumors: results from the CERENAT case-control study. Cancer Causes Control. 2021;32:773–82.
Röösli M, Lagorio S, Schoemaker MJ, Schüz J, Feychting M. Brain and salivary gland tumors and mobile phone use: evaluating the evidence from various epidemiological study designs. Annu Rev Public Health. 2019;40:221–38.
Sergentanis TN, Tsivgoulis G, Perlepe C, Ntanasis-Stathopoulos I, Tzanninis IG, Sergentanis IN, et al. Obesity and risk for brain/cns tumors, gliomas and meningiomas: a meta-analysis. PLoS ONE. 2015;10:e0136974.
Benson VS, Kirichek O, Beral V, Green J. Menopausal hormone therapy and central nervous system tumor risk: large UK prospective study and meta-analysis. Int J Cancer. 2015;136:2369–77.
Cowppli-Bony A, Bouvier G, Rué M, Loiseau H, Vital A, Lebailly P, et al. Brain tumors and hormonal factors: review of the epidemiological literature. Cancer Causes Control. 2011;22:697–714.
IARC. IARC monographs on the evaluation of carcinogenic risks to humans. vol. 109. Outdoor air pollution. Lyon: IARC; 2016.
Poulsen AH, Hvidtfeldt UA, Sørensen M, Puett R, Ketzel M, Brandt J, et al. Intracranial tumors of the central nervous system and air pollution—a nationwide case-control study from Denmark. Environ Health. 2020;19:81.
Andersen ZJ, Pedersen M, Weinmayr G, Stafoggia M, Galassi C, Jørgensen JT, et al. Long-term exposure to ambient air pollution and incidence of brain tumor: the European Study of Cohorts for Air Pollution Effects (ESCAPE). Neuro Oncol. 2018;20:420–32.
Jørgensen JT, Johansen MS, Ravnskjær L, Andersen KK, Bräuner EV, Loft S, et al. Long-term exposure to ambient air pollution and incidence of brain tumours: The Danish Nurse Cohort. Neurotoxicology. 2016;55:122–30.
Lagergren M, Fratiglioni L, Hallberg IR, Berglund J, Elmståhl S, Hagberg B, et al. A longitudinal study integrating population, care and social services data. The Swedish National study on Aging and Care (SNAC). Aging Clin Exp Res. 2004;16:158–68.
Magnusson PK, Almqvist C, Rahman I, Ganna A, Viktorin A, Walum H, et al. The Swedish Twin Registry: establishment of a biobank and other recent developments. Twin Res Hum Genet. 2013;16:317–29.
Wändell PE, Wajngot A, de Faire U, Hellénius ML. Increased prevalence of diabetes among immigrants from non-European countries in 60-year-old men and women in Sweden. Diabetes Metab. 2007;33:30–6.
Eriksson AK, Ekbom A, Granath F, Hilding A, Efendic S, Ostenson CG. Psychological distress and risk of pre-diabetes and Type 2 diabetes in a prospective study of Swedish middle-aged men and women. Diabet Med. 2008;25:834–42.
Tjønneland A, Olsen A, Boll K, Stripp C, Christensen J, Engholm G, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health. 2007;35:432–41.
Hundrup YA, Simonsen MK, Jørgensen T, Obel EB. Cohort profile: the Danish nurse cohort. Int J Epidemiol. 2012;41:1241–7.
Beulens JW, Monninkhof EM, Verschuren WM, van der Schouw YT, Smit J, Ocke MC, et al. Cohort profile: the EPIC-NL study. Int J Epidemiol. 2010;39:1170–8.
Clavel-Chapelon F. Cohort profile: The French E3N Cohort Study. Int J Epidemiol. 2015;44:801–9.
Ulmer H, Kelleher CC, Fitz-Simon N, Diem G, Concin H. Secular trends in cardiovascular risk factors: an age-period cohort analysis of 698,954 health examinations in 181,350 Austrian men and women. J Intern Med. 2007;261:566–76.
Hvidtfeldt UA, Severi G, Andersen ZJ, Atkinson R, Bauwelinck M, Bellander T, et al. Long-term low-level ambient air pollution exposure and risk of lung cancer—A pooled analysis of 7 European cohorts. Environ Int. 2021;146:106249.
de Hoogh K, Chen J, Gulliver J, Hoffmann B, Hertel O, Ketzel M, et al. Spatial PM(2.5), NO(2), O(3) and BC models for Western Europe—Evaluation of spatiotemporal stability. Environ Int. 2018;120:81–92.
Chen J, de Hoogh K, Gulliver J, Hoffmann B, Hertel O, Ketzel M, et al. Development of Europe-wide models for particle elemental composition using supervised linear regression and random forest. Environ Sci Technol. 2020;54:15698–709.
Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, Cirach M, et al. Development of Land Use Regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46:11195–205.
Brandt J, Silver JD, Frohn LM, Geels C, Gross A, Hansen AB, et al. An integrated model study for Europe and North America using the Danish Eulerian Hemispheric Model with focus on intercontinental transport of air pollution. Atmos Environ. 2012;53:156–76.
Straif K, Cohen A, Samet J. Air pollution and cancer. Lyon: World Health Organization; 2013.
Chen ST, Lin CC, Liu YS, Lin C, Hung PT, Jao CW, et al. Airborne particulate collected from central Taiwan induces DNA strand breaks, Poly(ADP-ribose) polymerase-1 activation, and estrogen-disrupting activity in human breast carcinoma cell lines. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2013;48:173–81.
Xie W, You J, Zhi C, Li L. The toxicity of ambient fine particulate matter (PM2.5) to vascular endothelial cells. J Appl Toxicol. 2021;41:713–23.
Calderón-Garcidueñas L, Azzarelli B, Acuna H, Garcia R, Gambling TM, Osnaya N, et al. Air pollution and brain damage. Toxicol Pathol. 2002;30:373–89.
Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol. 2012;2012:782462.
Costa LG, Cole TB, Coburn J, Chang YC, Dao K, Roqué PJ. Neurotoxicity of traffic-related air pollution. Neurotoxicology. 2017;59:133–9.
Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39:42–5.
Barlow L, Westergren K, Holmberg L, Talbäck M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48:27–33.
Hackl M, Waldhoer T. Estimation of completeness of case ascertainment of Austrian cancer incidence data using the flow method. Eur J Public Health. 2013;23:889–93.
van der Willik KD, Ruiter R, van Rooij FJA, Verkroost-van Heemst J, Hogewoning SJ, Timmermans K, et al. Ascertainment of cancer in longitudinal research: The concordance between the Rotterdam Study and the Netherlands Cancer Registry. Int J Cancer. 2020;147:633–40.
Evangelopoulos D, Katsouyanni K, Keogh RH, Samoli E, Schwartz J, Barratt B, et al. PM2.5 and NO2 exposure errors using proxy measures, including derived personal exposure from outdoor sources: a systematic review and meta-analysis. Environ Int. 2020;137:105500.
Beelen R, Hoek G, Fischer P, Brandt PAVD, Brunekreef B. Estimated long-term outdoor air pollution concentrations in a cohort study. Atmos Environ. 2007;41:1343–58.
Cesaroni G, Porta D, Badaloni C, Stafoggia M, Eeftens M, Meliefste K, et al. Nitrogen dioxide levels estimated from land use regression models several years apart and association with mortality in a large cohort study. Environ Health. 2012;11:48.
Gulliver J, Morris C, Lee K, Vienneau D, Briggs D, Hansell A. Land use regression modeling to estimate historic (1962-1991) concentrations of black smoke and sulfur dioxide for Great Britain. Environ Sci Technol. 2011;45:3526–32.
Chen J, de Hoogh K, Gulliver J, Hoffmann B, Hertel O, Ketzel M, et al. A comparison of linear regression, regularization, and machine learning algorithms to develop Europe-wide spatial models of fine particles and nitrogen dioxide. Environ Int. 2019;130:104934.
Brunekreef B, Strak M, Chen J, Andersen ZJ, Atkinson R, Bauwelinck M, et al. Mortality and morbidity effects of long-term exposure to low-level PM(2.5), BC, NO(2), and O(3): an analysis of European Cohorts in the ELAPSE project. Res Rep Health Eff Inst. 2021;208:1–127.
Acknowledgements
We thank Marjan Tewis for the data management tasks in creating the pooled cohort database and the National Institute for Public Health and the Environment (RIVM), Bilthoven, the Netherlands, for their contribution to the ELAPSE Study.
Funding
The research described in this article was conducted under contract to the Health Effects Institute (HEI), an organisation jointly funded by the United States Environmental Protection Agency (EPA) (Assistance Award No. R-82811201) and certain motor vehicle and engine manufacturers. The contents of this article do not necessarily reflect the views of HEI, or its sponsors, nor do they necessarily reflect the views and policies of the EPA or motor vehicle and engine manufacturers.
Author information
Authors and Affiliations
Contributions
GH, ORN and UAH: study conceptualisation and design; GH and BB: principal investigators of the ELAPSE project; UAH: statistical analysis and manuscript writing; GH, ORN and BB: supervision, manuscript review and editing; GH, BB, JC and MS: ELAPSE project coordination, preparing pooled data for analyses, and providing support with the access to pooled cohort data; SR, ES and KK: contribution of statistical analyses strategy and scripts for the statistical analyses; KdH, JC and GH: exposure assessment; JB: exposure data. All authors contributed to the interpretation of the results. All authors read and revised the manuscript for the important intellectual content and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study involved no contact with members of the study population and the published results does not allow identification of individuals. The analyses were undertaken in a secure IT environment where no individual level data can be retrieved. All included cohort studies were approved by the medical ethics committees in their respective countries.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hvidtfeldt, U.A., Chen, J., Rodopoulou, S. et al. Long-term air pollution exposure and malignant intracranial tumours of the central nervous system: a pooled analysis of six European cohorts. Br J Cancer 129, 656–664 (2023). https://doi.org/10.1038/s41416-023-02348-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02348-1
- Springer Nature Limited