Abstract
Objective
To assess tidal volume (Vt) and minute ventilation (MV) during cardiopulmonary resuscitation (CPR) with two different chest compressions techniques: two-finger (TFT) or two-thumb technique (TTT) in a neonatal model.
Methods
Vt and MV were continuously measured during consecutive periods of resuscitation in an intubated manikin. Thirty participants performed the two compression techniques in a random order for 2-min periods while performing positive pressure ventilation using a T-piece resuscitator (TPR) or a self-inflating bag (SIB).
Results
Vt during CPR with TFT was significantly higher than TTT with either TPR: 44.9 ± 4.3 vs 39.2 ± 5.4 ml (p < 0.001) or SIB: 39.2 ± 5.7 vs 35.6 ± 6.5 ml (p < 0.023). Similarly MV was significantly higher in TFT than TTT with either mode: 1346 ± 130 vs 1175 ± 162 ml/min, respectively, with TPR (p < 0.001) and 1177 ± 170 vs 1069 ± 196 ml/min with SIB (p < 0.03).
Conclusions
Chest compressions during CPR using the TFT achieved higher Vt and MV than TTT in this model of neonatal resuscitation.
Similar content being viewed by others
Introduction
Two chest compressions techniques are recommended for newborn cardiopulmonary resuscitation (CPR): the two-finger technique (TFT) and the two-thumb technique (TTT) [1, 2]. The TFT consists of compressing the lower half of the sternum immediately below the intermammary line with the middle and ring fingers. In the TTT, the newborn’s chest is encircled with both hands and thumbs placed on the lower half of the sternum. In both, the chest should be compressed at least one-third of its anterior–posterior diameter.
There is little evidence to determine which practice is more effective. Several studies compare both techniques in animal and manikin models and few in human newborns [3,4,5,6]. Most studies are focused on the quality of the chest compression and its hemodynamic repercussion. Based on some of these publications, the International Liaison Committee on Resuscitation consensus recommends using the TTT preferably because it produces a deeper compression that can generate higher systolic pressures [1, 6]. However other studies have shown that the TTT is less effective than TFT in terms of chest recoil [7, 8]. Decreased recoil is probably due to the maintenance of rescuer’s hands position encircling and compressing the thorax. We are not aware of studies aimed to evaluate the impact of these techniques on ventilation. We believe that the TTT while surrounding the chest with both hands can restrict ventilation. We did pilot ventilation measurements in a neonatal manikin model finding lower values with this technique. Given the importance of ventilation during neonatal resuscitation, we decided to carry out this study aimed to evaluate the effects on ventilation of these two CPR techniques during neonatal resuscitation.
Design and methods
Prospective randomized crossover trial in a laboratory setting. We measured tidal volume (Vt) and minute ventilation (MV) during consecutive periods of chest compressions using the two techniques in a neonatal manikin model.
Participants
Thirty neonatal resuscitation trained professionals: neonatologists, neonatal fellows, pediatric residents, nurses and respiratory therapists. The study was approved by the Ethics Committee of the Faculty of Medicine Universidad Católica de Chile, and a written informed consent of the participants was required.
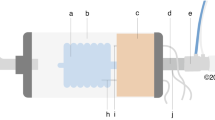
Neonatal model
A modified neonatal manikin (ResusciBaby® Laerdal Medical Corp, NY). Two neonatal test lung models (EasyLung® Bellavista Medical, NZ) were placed inside the thorax connected with a silicone pipe and fixed to a regular 3.5 uncuffed endotracheal tube that was introduced through the model’s airway. Positive pressure ventilation (PPV) was delivered by a continuous flow T-piece resuscitator equipment (Neopuff® Fisher and Paykel, Auckland, NZ) or by a self-inflating bag.
Ventilation measurements
Vt, MV and airway pressures were continuously measured using a variable orifice differential pressure flow transducer interposed between the endotracheal tube and the resuscitator equipment and connected to a pulmonary function monitor (VarFlex® and Bicore® CP-100, respectively, Allied Healthcare, CA, USA).
Protocol
Two professionals participated at a time: one performing ventilation and the other chest compressions. They performed the two compression techniques in a random order for 2-min periods each one while performing PPV using the T-piece resuscitator. Ventilations were given at a rate of 30 breaths/min coordinated 1:3 with 90 compressions/min. Peak inspiratory pressure limit was set at 25-cm H2O and PEEP at 5-cm H2O. The same sequence was repeated using a self-inflating bag connected to a manometer. A metronome was set at 120 beats/min, and instructions were given to perform one compression for each beat alternating one ventilation every three compressions. The order of the compression technique was randomly selected using sequentially sealed opaque envelopes from a computer-generated randomization list. Ventilation measurements were obtained during the second minute of recordings and values for each experiment were the average of 15 consecutive breaths. Participants were blinded to study measurements.
Before testing, participants received a brief theoretical introduction on chest compressions and ventilation according to Neonatal Resuscitation Program (NRP) guidelines including a demonstration of TFT and TTT showing correct fingers position and depth of compressions. Participants were then asked to practice both techniques and ventilation on a manikin placed on a standard neonatal ICU bed. A 2-min practice trial period prior to measurements was performed for each of the two professionals in order to get familiar with the model and practice both compression techniques coordinated with ventilation. These trial periods were supervised by NRP instructors, and if there were errors, participants received feedback and performed correction actions until they mastered the technique. During this pre-trial period, the manikin was also connected to a Laerdal Skillguide® performance indicator and a green light flashed-on when correct depth (≥3 cm) and finger position were achieved for each compression.
Sample size
Based on data from our pilot measurements where tidal volume measurements were 15% below with the TTT, we estimated the enrollment of at least 25 participants taking into account a reduction of mean Vt from 45 ml with TFT to 38 ml with the TTT considering an alpha of 0.05 and a power of 80%. To ensure that we meet our goals, we aimed to enroll 30 participants.
Statistical analysis
Continuous variables were compared using the Student “t” test or Mann–Whitney test as appropriate. Categorical variables were compared using the chi-square test and if the expected number of observations was <5 Fisher’s exact test was used. A p value ≤ 0.05 was considered significant.
Results
Thirty participants were enrolled 5 males and 25 females. Of them, 5 were staff neonatologists, 3 neonatal fellows, 4 pediatric residents, 15 neonatal nurses, and 3 respiratory therapists. Their median (range) age was 34 years old (25–50).
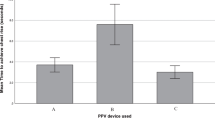
As shown in Table 1, Vt measurements with the TFT were significantly higher than those with the TTT while performing PPV either with the T-piece resuscitator or the self-inflating bag, despite there was no difference in ventilation pressures nor in respiratory rate. Similarly MV measurements with the TFT were significantly higher than with the TTT with both ventilation modes (Fig. 1). Interestingly MV measured during PPV with T-piece resuscitator were significantly higher than those obtained with the self-inflating bag (Fig. 1).
Discussion
In this experimental manikin randomized study, we observed that chest compressions using the TFT during CPR resulted in higher Vt and MV than the TTT. Given the importance of ventilation during neonatal resuscitation, we believe that this observation should be considered and evaluated in future neonatal resuscitation clinical studies to further elucidate which technique is more appropriate to use in neonatal resuscitation.
Several studies comparing these compression techniques in animal and manikin models have shown that TTT generates higher systolic pressures and a deeper compression [2,3,4,5,6]. Other described advantages for the TTT are that it is less tiring and suitable for providers with long fingernails compared with TFT [2, 6]. Also, the TTT achieves a higher proportion of correct finger placement [4, 5]. We are not aware of studies aimed to evaluate the impact on ventilation of these techniques. During the TTT, the newborn’s chest is encircled with both hands and both thumbs placed on the sternum. In some guidelines, it is also recommended that rescuers should maintain their hands position encircling the thorax to decrease the hands-off time that may impact hemodynamic performance. However this maneuver may also restrict ventilation. Manikin studies have shown that TTT is less effective than TFT in terms of chest recoil [7, 8]. Decreased recoil is probably due to the maintenance of rescuer’s hands position encircling the thorax. In contrast during TFT, the thorax can be fully released after each chest compression. Although some studies comparing these techniques reported no differences in ventilation, this was indirectly measured by the manikin software or the methods of ventilation were not comparable between the groups. Decreased expiratory Vt has also been reported once CPR with TTT was started [9]. Furthermore Li et al. [10] reported that during compressions with TTT coordinated 3:1 with PPV each compression cycle resulted in lung derecruitment with a net Vt loss of 4.5 mL/kg. Another consideration is that incomplete chest recoil may leave residual positive intrathoracic pressure, which may decrease venous return and brain blood flow [11]. There are also other studies comparing these two chest compressios techniques but in a different scenario of one lone rescuer. In those studies, investigators have observed that although the TTT was associated with a more effective compression depth, the hand-off time was longer than the TFT [12, 13]. As a result the TFT can provide a higher number of compressions and ventilations. However in this study ventilation rate was the same in both groups.
The present study confirms the described observations of decreased ventilation and chest recoil during the two-thumb encircling hands technique using very precise ventilation-volumes measurement. This observation should be considered by neonatal resuscitation investigators, and future studies are needed to better evaluate chest compression techniques and their effects on human newborns. The current evidence in newborns is mainly based on simulation manikin studies animal data and expert opinions. There is a need for basic/translational evidence, and additional clinical trial studies ideally using data obtained from newborn humans to further elucidate the clinical outcomes of each technique.
This study has some limitations. First the simulation setting: a modified manikin, which is an imperfect representation of the newborn especially in terms of chest compliance that may be an important factor influencing ventilation. However, the manikin and lung models used are accepted and frequently utilized as training instruments and allowed us to provide conclusions within the mentioned limitation. Second, we were focused on ventilation and we did not evaluate chest compression depth and efficacy at the same time. Although we made efforts to standardize compression depth prior to measurements, these different techniques have been associated with differences in compression depth that may influence hemodynamic function. Future studies are needed with combined evaluation of ventilation and cardiac function to better elucidate which technique is more appropriate in a clinical scenario.
In conclusion, chest compressions with TFT during CPR established higher tidal volume and minute ventilation compared with TTT in this model of neonatal resuscitation.
References
Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: neonatal resuscitation 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint). Pediatrics. 2015;136:S196–218. https://doi.org/10.1542/peds.2015-3373G.
Perlman JM, Wyllie JP, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Pediatrics. 2015;136:S204–41. https://doi.org/10.1542/peds.2015-3373D.
Menegazzi JJ, Auble TE, Nicklas KA, Hosack GM, Rack L, Goode JS. Two-thumb versus two-finger chest compression during CPR in a swine infant model of cardiac arrest. Ann Emerg Med. 1993;22:240–3.
Christman C, Hemway RJ, Wyckoff MH, Perlman JM. The two-thumb is superior to the two-finger method for administering chest compressions in a manikin model of neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2011;96:F99–101.
Saini SS, Gupta N, Kumar P, Bhalla AK, Kaur H. A comparison of two-fingers technique and two-thumbs encircling hands technique of chest compression in neonates. J Perinatol. 2012;32:690–4.
Millin MG, Bogumil D, Fishe JN, Burke RV. Comparing the two-finger versus two-thumb technique for single person infant CPR: a systematic review and meta-analysis. Resuscitation. 2020;148:161–72.
Martin PS, Kemp AM, Theobald PS, Maguire SA, Jones MD. Does a more “physiological” infant manikin design effect chest compression quality and create a potential for thoracic over-compression during simulated infant CPR? Resuscitation. 2013;84:666–71.
Jo CH, Jung HS, Cho GC, Oh YJ. Over-the-head two-thumb encircling technique as an alternative to the two-finger technique in the in-hospital infant cardiac arrest setting: a randomised crossover simulation study. Emerg Med J. 2015;32:703–7.
Solevag AL, Madland JM, Gjaerum E, Nakstad B. Minute ventilation at different compression to ventilation ratios different ventilation rates and continuous chest compressions with asynchronous ventilation in a newborn manikin. Scand J Trauma Resusc Emerg Med. 2012;20:73.
Li ES, Cheung PY, O’Reilly M, Schmölzer GM. Change in tidal volume during cardiopulmonary resuscitation in newborn piglets. Arch Dis Child Fetal Neonatal Ed. 2015;100:F530–3.
Yannopoulos D, McKnite S, Aufderheide TP, Sigurdsson G, Pirrallo RG, Benditt D, et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64:363–72.
Lee SY, Hong JY, Oh JH, Son SH. The superiority of the two-thumb over the two-finger technique for single-rescuer infant cardiopulmonary resuscitation. Eur J Emerg Med. 2018;25:372–6.
Udassi S, Udassi JP, Lamb MA, Theriaque DW, Shuster JJ, Zaritsky A, et al. Two-thumb technique is superior to two-finger technique during lone rescuer infant manikin CPR. Resuscitation. 2010;81:712–7.
Acknowledgements
We are grateful to Edgardo Szyld MD for his critical review of this manuscript and for the valuable help of all participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jahnsen, J., González, A., Fabres, J. et al. Effect of two different chest compression techniques on ventilation during neonatal resuscitation. J Perinatol 41, 1571–1574 (2021). https://doi.org/10.1038/s41372-021-01061-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01061-2
- Springer Nature America, Inc.