Abstract
Objectives
To determine efficacy of non-invasive positive pressure face mask ventilation using a ventilator device (NIPPmV) for achieving early effective ventilation compared to that by self-inflating bag (SIB) or T- piece resuscitator (TPR).
Methods
The authors video recorded 33 trained resuscitators using NIPPmV (provided using ventilator device), SIB [a 500 ml silicone SIB without a positive end expiratory pressure (PEEP) valve] and a TPR. Using a continuous pressure recording system and a neonatal manikin, the authors evaluated the efficacy of the ventilation to achieve early effective ventilation during 30 s of ventilation. The primary outcome was time to achieve effective chest rise. Secondary outcomes were peak inspiratory pressure (PIP), ventilation rate and the need to perform ventilation corrective steps during positive pressure ventilation (PPV) among the devices.
Results
Total 99 videos were recorded. The time(s) taken to achieve the first chest rise was significantly lesser in NIPPmV group compared to SIB and TPR (3.0 ± 1.7 vs. 3.7 ± 1.9 vs. 7.5 ± 5.4, respectively, p <0.001). The mean PIP delivered by NIPPmV compared to SIB & TPR (19.8 ± 1.6 vs. 35.6 ± 7.4 vs. 17.8 ± 2.0 cm H20 respectively; p <0.001) was more accurate with preset PIP. Ventilation, in terms of breath rate, was observed to be controlled more accurately with NIPPmV compared to SIB & TPR (50 vs. 42 vs. 33 per min respectively; p <0.001).
Conclusions
The non-invasive positive pressure face mask ventilation using a ventilator (NIPPmV) resulted in achieving early, effective and consistent ventilation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 19% of newborn deaths in India are related to asphyxia [1]. Transition from intrauterine to extrauterine life is an important phase for newborns. Approximately 10% of term newborns will need some assistance to make this transition at birth; five percent require positive pressure ventilation (PPV) [2]. Therefore, provision of effective PPV is important to improve outcomes for those who fail to initiate spontaneous breathing at birth. Improper PPV can lead to barotrauma, volutrauma, atelectotrauma and oxytrauma [3]. Therefore, the pressures, volume and oxygen should be used within the ranges of safety for establishing optimum ventilation while preventing the lung injury.
Among the three recommended ventilation devices, self-inflating bag (SIB) and T-piece resuscitator (TPR) are the commonly used ones for PPV in delivery rooms [2]. The SIB is the most frequently used ventilation device, and its effectiveness depends upon the resuscitator’s training and experience [4]. SIBs commonly used in India do not have a manometer to control peak inspiratory pressure (PIP) or a positive end expiratory pressure (PEEP) valve. The TPR provides ventilation with a preset PIP and PEEP. In most studies, TPR seems to be the most effective and the safest device [5]. The pressure, volume and rate generated by it are operator dependent and vary depending upon the specialization and experience of the personnel who operates the device [4]. In developing countries, effective ventilation strategies can reduce the early neonatal mortality rate by almost 45% [6]. There is an urgent need to innovate a ventilation device which could achieve early, effective and sustained lung ventilation irrespective of its operator’s skills and experience.
Nasal intermittent positive pressure ventilation (NIPPV) is commonly used modality for non-invasive respiratory support in preterm infants who otherwise would undergo endotracheal intubation and ventilation. It augments continuous positive airway pressure (CPAP) by superimposing inflations, typically from a ventilator, with a set peak pressure delivered through nasal prongs or mask. The available evidence suggests modest benefit of NIPPV over CPAP with no harm in treating apnea of prematurity [7]. Present manikin-based study was designed to explore use of non-invasive positive pressure mask ventilation (NIPPmV) for ventilating apneic term newborns in delivery room setting. The hypothesis was whether ventilating an apneic term newborn by NIPPmV will result in better effective ventilation compared to SIB or TPR.
Material and Methods
The present open label randomized control trial (CTRI registration number: CTRI/2021/02/031553) was conducted in level III neonatal intensive care unit of a tertiary care hospital. The study was approved by the institute ethics committee. The study compared three ventilation devices used for newborn resuscitation. Written informed consent was taken from the participants. Health care professionals (HCPs) who regularly participate and are certified in neonatal resuscitation were enrolled. In this paper, authors present results of the effects of different types of devices for achieving early effective ventilation.
Pilot observations using bag ventilation suggested that time to chest rise would be mean (SD) 6 (3) s. Assuming reduction in time to chest rise by 33% using NIPPmV with alpha of 0.05, a total of 34 observations were needed in each arm to achieve 80% power by ANOVA. One of the observer’s recorded videos were blur; hence were excluded. Thus, 33 observers were included in each group.
Healthcare professionals of different specialties with varying degree of experience participated in this study. Prior to beginning the study, the HCPs completed the Neonatal Resuscitation Program course, which was taught by a certified instructor. The course was divided into two sessions. The first session involved participants' theoretical briefing and self-study. The second practical part focused on the proper mask seal and the proper use of the PPV device to ensure that this was not a factor influencing the results. A standard simulation case scenario of a term neonate requiring PPV in the delivery room was developed. The participants were given a pre-briefing on the case scenario, neonatal resuscitation protocol, and ventilation device to be used. Prior to data collection, participants had the opportunity to practice with each device under the supervision of an instructor who reviewed proper technique using a checklist. The data collection phase began after each participant demonstrated proper device use.
A specially developed neonatal mannequin (approximating a 7lb neonate, 21 inches long) with emulated patient monitor software and wireless facilitator control (CAE Luna baby simulator) were used. Three devices were compared:
Device A—500 ml, silicone, self-inflating bag without a PEEP valve (manufactured by Anaesthetics India Pvt. Ltd, India). The self-inflating bag had a pop off valve set to activate at PIPs in excess of 40 cmH2O.
Device B—A T-piece resuscitator (Neopuff®, Fisher & Paykel Healthcare). The TPR settings were preset (PIP 20 cmH20, PEEP 5 cmH2O) by each participant before testing.
Device C—A ventilator device Drager Babylog VN500. While using the ventilator device non-invasive positive pressure ventilation mode was used with the preset ventilation settings of PIP 20 cmH2O, PEEP 5 cmH2O, rates 50/min and inspiratory time (Ti 0.4 s).
The flow for all three devices was kept to be 10 L/min. A pressure manometer connected to a vital sign monitor (Philips vm6 monitor) was used for all interventions. For consistency, the same pressure manometer was used with all three devices connected via. a T-adapter placed between the mask and the ventilation device. The manometer was calibrated to a pressure transducer between device and participants. The pressures were video recorded continuously via. a pressure transducer. The measurements were taken in millimetres of mercury (mmHg), which were later converted to centimetres of water (cmH2O).
The sequence of use of a device during the study by each participant was randomized using lottery method. Before beginning the scenario, each participant was instructed to draw a chit from a container. Three folded word chits were kept in the container (5 cm × 5 cm). The chits were prepared by the neonatologist who was not part of the study. Each chit was labelled with A (for SIB), B (for TPR), or C (for NIPPmV). Before each case scenario, the participant drew a chit and was then assigned a ventilation device (Supplementary Fig. S1). Participants were asked to provide positive pressure ventilation for a period of two minutes with each of the three devices, aiming to achieve 40 to 60 breaths per min, delivering a PIP and PEEP of 20 cmH2O and 5 cmH2O respectively. Each operator was able to observe chest rise during ventilation in addition to the manometer while using either the Neopuff or the ventilator device. The timer clock was not visible to the participants. Participants were not allowed to view their continuous recordings. The scenarios were video recorded using a mobile device (Apple iphone 11). The radiant warmer, resuscitator position, ventilation devices, monitor and video camera ergonomics were all maintained at all times (Supplementary Figs. S2A & S2B).
Main outcomes of interest were time to chest rise from the time of application of facemask, PIP, ventilation rate and need to perform ventilation corrective steps. The recorded video was analysed by three outcome assessors who were clinicians with more than 10 y experience in clinical pediatrics and who were not part of the study. One outcome assessor was shown the video with the mannequin’s face and ventilation device obscured by an animated black box & was asked to record time of the chest rise. The second outcome assessor was shown the video with mannequin’s chest obscured and was asked to record the time of mask application. Secondary outcomes were assessed by both separately. Any dispute during analysis was resolved by third outcome assessor.
For all participants, a post-scenario debriefing was conducted using advocacy inquiry. The NASA Task Load Index (TLx) was used to evaluate the subjective mental workload during PPV with each ventilation device. The participants are asked to rate their performance on a scale ranging from low (1) to high (5) [8].
The authors used mean and standard deviation or medians with interquartile length, as appropriate to describe numeric variables. They used proportions to describe qualitative variables. Since outcome parameters were not normally distributed and were not independent, they used dependent non-parametric tests to compare the three devices. Thus, Friedman’s test was used to compare time to achieve chest rise and other outcome parameters between the three devices used. Wilcoxon’s signed rank test was used for post-hoc pairwise comparison of each of the two devices. Bonferroni’s adjustment was used for multiple comparisons. Since the authors had three post-hoc comparisons, they considered P less than 0.017 for each comparison as statistically significant to achieve and overall alpha error of 0.05. All reported P values are two sided.
Results
Total 33 healthcare professionals participated in the study. The participants included 15 pediatric resident doctors, 3 neonatal fellows, 2 neonatologists, 7 pediatricians, 3 pediatric anesthetists, 3 cardiac anesthetists. The years of experience varied from >1 y to greater than 20 y. All participants completed all aspects of the evaluation, which required approximately 30 min for each participant. Total 99 (33 × 3) observations were recorded. Results are summarized in Tables 1 and 2.
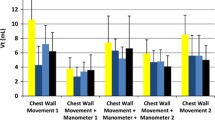
The time taken to achieve the first chest rise after mask application for PPV was 3.0 ± 1.7 s with NIPPmV, 3.7 ± 1.9 s with SIB, and 7.5 ± 5.4 with TPR. When compared to SIB (p 0.022) and TPR (p <0.001), NIPPmV achieved chest rise significantly earlier (Fig. 1). Effective ventilation was said to be established after the first chest rise. Average PIP delivered during the first 30 s after mask application was calculated. Mean PIP delivered by NIPPmV was 19.8 ± 1.6, with SIB was 35.6 ± 7.4 and that by TPR was 17.8 ± 2.0 cmH2O. NIPPmV resulted in effective and consistent PIP delivery during the first 30 s after mask application when compared to SIB (p <0.001) and TPR (p <0.001). The maximum and minimum PIP delivered by the devices varied significantly. PIP delivered by SIB was found to be significantly higher than that delivered by TPR and NIPPmV (40.4 ± 9.2 vs. 18.3 ± 1.8 vs. 21.5 ± 1.5 respectively; p <0.01).
The controlled ventilation provided by NIPPmV resulted in the consistent delivery of preset 50 BPM with a constant inspiratory time of 0.4 s. While SIB matched the physiological rate of ventilation with median breath rate of 42 (35 – 55), TPR resulted in hypoventilation with median breath rates of 33 (28 – 41). Except for the TPR, breath rates were effectively delivered by SIB and NIPPmV. The tidal volume delivered during the first minute after the start of PPV was found to vary significantly between the three devices. Compared to SIB (294 ml) and TPR (271 ml), NIPPmV (235.4 ml) delivered lower total tidal volume (p <0.001). Highest tidal volume per breath was delivered by SIB (294.1 ml, p <0.001) (Table 1). Interruptions while PPV were observed during ventilation corrective steps. Number of interruptions were observed to be more with TPR compared SIB or NIPPmV (p <0.05).
Subjective mental workload was analyzed using NASA TLX tool. The participants self-rated on a scale of 1 (low) to 20 (high) for each device used for PPV. Overall total workload was rated to be significantly less with NIPPmV compared to both SIB and TPR (10, 20, 24 respectively p <0.001). Total workload demand was observed to be highest while performing PPV using SIB. Except for performance, TPR mental workload was comparable with NIPPmV. Though SIB was less mentally demanding and resulted in subjectively good performance, it was associated with high physical and temporal demand.
Discussion
Recent studies have highlighted the variety of resuscitation equipments in routine use in newborn resuscitation corner based on availability, resuscitator training level, and level of care provided in the hospital [9]. In India, SIB appears to be the most common PPV device, followed by TPR. Though non-invasive ventilation has been routinely used in NICUs, it’s use in delivery room settings has not been explored. To authors’ knowledge, this is the first study that addresses the use of non-invasive positive pressure face mask ventilation for ventilating an apneic term newborn in the delivery room.
The “Golden Minute” refers to the first 60 s of an infant’s life [2]. Within this time, the infant should begin breathing on his or her own, or interventions for lung ventilation must be started [2]. Every second’s delay may compromise the baby further. Hence the present study’s primary outcome was to compare the time for achieving chest rise after the face mask application, an indicator for effective positive pressure ventilation [2]. NIPPmV was observed to achieve first chest inflation significantly earlier compared to the other two devices. With NIPPmV, the resuscitator achieved the face mask seal by two hand hold technique and the preset pressure, rate and FiO2 was automatically delivered by the ventilator and was not dependent upon the resuscitator. The resuscitator had to focus only on positioning the mannequin and maintaining the seal while providing PPV. Limiting multitasking might have helped in establishing lung ventilation the earliest.
Studies have shown TPR and flow inflating bags to be safest for delivering desired PIP and PEEP compared to SIB [10]. In the present study, both TPR and NIPPmV were observed to achieve preset pressure. However, NIPPmV was observed to be delivering more accurate and consistent preset PIP compared to the other two methods. Automatic control of pressure delivery independent of the operator could have resulted in the accurate and consistent pressure delivery.
The ability to provide a consistent predetermined rate of ventilation has been studied previously [11]. Whyte et al. described problems with the required respiratory rate; regardless of the device used, none of the evaluated practitioners administered frequencies in the required ranges, and all rates were well below recommendations [11]. In the present study, authors observed similar results with the TPR device. However, SIB and NIPPmV lead to delivery of breath rates within the target range of 40 to 60 per min. NIPPmV consistently delivered breath rates at the preset rate of 50 breaths per min.
Following the scenario, all participants were evaluated for their subjective mental workload on each device using the NASA TLX tool. Mental load while providing PPV to an apneic newborn was observed to be significantly less with NIPPmV compared to SIB and TPR. The present is the first study to compare ventilation-related workloads among the users. NIPPmV ventilation had the added benefit of delivering heated humidified blended oxygen during resuscitation. This aspect has not been studied and requires further research for its impact on establishing lung ventilation in delivery room settings.
In the present study, it was observed that NIPPmV resulted in establishing effective ventilation earlier than SIB or TPR. Delivered pressure, tidal volume and breath rate were observed to be more frequent within the safe range with NIPPmV than on other devices tested, and the results were statistically significant. These findings suggest that the use of NIPPmV by trained personnel can improve newborn respiratory assistance and support quality newborn survival.
The present study has certain limitations. It was conducted in a NICU. In situ simulation could have helped in identifying system gaps. Larger self-inflating bag (500 ml) compared to the smaller deliver higher pressures. The authors did not compare smaller self-inflating bag for the delivered peak pressures. Post hoc analysis was not performed. More studies with clinical outcomes and comparing smaller SBI are needed. However, it may not be feasible to have ventilators at delivery points in most places in our country.
Conclusions
The non-invasive positive pressure face mask ventilation using a ventilator (NIPPmV) facilitates in achieving early, effective and consistent ventilation. Further research is needed to validate the findings in real-world patients.
References
Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–40.
Aziz K, Lee CHC, Escobedo MB, et al. Part 5: Neonatal Resuscitation 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2021;147:e2020038505E.
Hussey SG, Ryan CA, Murphy BP. Comparison of three manual ventilation devices using an intubated mannequin. Arch Dis Child Fetal Neonatal Ed. 2004;89:F490–3.
Augustine JA, Seidel DR, McCabe JB. Ventilation performance using a self-inflating anesthesia bag: effect of operator characteristics. Am J Emerg Med. 1987;5:267–70.
Leone TA, Finer NN, Rich W. Delivery room respiratory management of the term and preterm infant. Clin Perinatol. 2012;39:431–40.
Goudar SS, Somannavar MS, Clark R, et al. Stillbirth and newborn mortality in India after helping babies breathe training. Pediatrics. 2013;131:e344–52.
Lemyre B, Davis PG, de Paoli AG. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for apnea of prematurity. Cochrane Database Syst Rev. 2002;1:CD002272.
Laurie-Rose C, Frey M, Ennis A, Zamary A. Measuring perceived mental workload in children. Am J Psychol. 2014;127:107–25.
Roehr CC, Davis PG, Weiner GM, Jonathan Wyllie J, Wyckoff MH, Trevisanuto D. T-piece resuscitator or self-inflating bag during neonatal resuscitation: a scoping review. Pediatr Res. 2021;89:760–6.
Trevisanuto D, Roehr CC, Davis PG, et al. Devices for administering ventilation at birth: a systematic review. Pediatrics. 2021;148:e2021050174.
Whyte SD, Sinha AK, Wyllie JP. Neonatal resuscitation: a practical assessment. Resuscitation. 1999;40:21–5.
Acknowledgements
The authors sincerely thank Dr. Niranjan Khambete from Department of Clinical Engineering, for his inputs during data collection and Dr. Rajan Joshi HOD Pediatrics, for his valuable inputs while preparing the manuscript. The authors also thank team PediSTARS, Dr Jennifer Arnold, Dr Jonathan Duff, INSPIRE scientific review committee and IPSSV for their valuable inputs during initial designing of the study. They also thank CAE Healthcare for providing CAE Luna baby simulator for the study purpose.
Author information
Authors and Affiliations
Contributions
SK conceptualized and designed the study. She collected the data, wrote initial draft and gave final approval. VU collected the data, did literature search, revised the manuscript critically and gave final approval. AVM analysed and interpreted the data, revised the manuscript critically for important intellectual content and approved the final manuscript. APP collected the data, did literature search, revised the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Guarantor
Dr Rajan Joshi, Head, Department of Pediatrics, Deenanath Mangeshkar Hospital, Pune
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalane, S., Upadhye, V., Mulay, A.V. et al. Comparison of Efficacy of Pressure Controlled vs. Traditional Manual Mask Ventilation for Newborn Resuscitation – A Simulation-Based Pilot Randomized Control Trial. Indian J Pediatr 91, 1008–1013 (2024). https://doi.org/10.1007/s12098-023-04938-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04938-6