Abstract
The combination of having a low physical performance and obesity results in a vicious cycle, but the effect of this combination on the incidence of hypertension is still unknown. This article aims to examine the effect of obesity and low physical performance on the incidence of hypertension in older adults. The sample was comprised of 349 Chinese community-dwelling participants (199 women; mean age 66.30 ± 5.78 years) without hypertension at baseline. Obesity was defined as having a body mass index (BMI) greater than or equal to 28 kg/m2. Participants scoring in the top 20% on the Timed Up and Go Test (TUGT) or in the slowest 20% of the 4-m walking test were defined as having a low physical performance. The outcome was new onset hypertension at the 1-year follow-up. We found that 89 (25.5%) of the 349 participants without hypertension at baseline had developed hypertension at their 1-year follow-up. After multivariate adjustments, it was found that the incidence of hypertension was associated with the combination of obesity and having a low physical performance (OR = 7.30, 95% CI = 1.36–39.11), but not solely with obesity (OR = 1.40, 95% CI = 0.68–2.88) or solely with low physical performance (OR = 0.98, 95% CI = 0.29–3.27). Hence, although obesity and low physical performance did not independently affect the incidence of hypertension after one year, the combination of the two can significantly increase the incidence of hypertension in Chinese community-dwelling older adults.
Similar content being viewed by others
Introduction
Hypertension is the most prevalent chronic noncommunicable disease in China [1], affecting 39% of the population [2]. It leads to serious complications, such as cerebral vascular disease, heart disease, heart failure, and renal failure [1]. It becomes more of an issue as patients age because its prevalence increases with age (59.4% of patients aged ≥ 60 years and 72.8% of patients aged ≥ 75 years have hypertension in China), it becomes more difficult to treat, and it increasingly negatively impacts quality of life [2, 3]. As China’s population is aging rapidly, the prevalence of hypertension will continue to rise and will continue to place an escalating burden on the Chinese economy and society [4]. Therefore, the prevention and treatment of hypertension in the older adults should be a priority.
Obesity is a well-known risk factor for hypertension. Several studies have shown a clear association between obesity and increased blood pressure, and one study showed that the prevalence of obesity was 2–5 times higher in obese individuals compared to non-obese individuals [5,6,7]. However, data from some epidemiological studies suggest that being overweight is associated with a significantly lower all-cause mortality risk in the older adults [8,9,10]. Furthermore, obesity in old age could reduce the risk of dementia [11], and a high body mass index is protective against sarcopenia [12, 13]. Therefore, it is necessary to confirm whether obesity is a risk factor for the incidence of hypertension in the older adults.
Gait speed as a measurement of functional mobility is one of the most important indicators of health in the older adults [14]. Research has shown that low physical performance is associated with hypertension and more specifically that hypertension is associated with both lower gait speed and a higher decline in gait speed in the older adults [15,16,17]. However, the majority of the above studies conclude that hypertension is a risk factor for developing low physical performance. There is minimal research on whether low physical performance is a risk factor for the development of hypertension.
The combination of having a low physical performance and obesity results in a vicious cycle: individuals who have a low physical performance become obese because being physically active is difficult for them, and, in turn, they become even more limited in their mobility due to their lack of physical activity. Low physical performance also poses additional health problems, such as falls and injuries [18, 19]. Although the effect of this combination on the incidence of hypertension is still unknown, we hypothesize that it may increase the incidence of hypertension in the older adults more than each factor by itself. In the present study, we aimed to examine the combined and separate effects of obesity and low physical performance on the incidence of hypertension in Chinese community-dwelling older adults to better understand how hypertension develops and thus how it can be prevented.
Methods
Study participants
This study was approved by our university ethics committee, which reviews studies in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained from all participants.
All participants had participated in the National Free Medical Examination Program at the Tianjin Hangu Health Center in China. Inclusion criteria were: (1) 60 years of age or older at baseline and (2) willingness to participate in baseline studies. The exclusion criteria for this study were: (1) history of a diagnosis hypertension; (2) history of a diagnosis stroke; (3) inability to have blood pressure taken at the right upper arm; (4) failure to perform the Timed Up and Go Test (TUGT) or the 4-m walking test; (5) unable to stand for measurement of body weight and height; (6) inability to communicate with the interviewer.
Study procedures
Baseline data were collected in July 2015. After completing their free medical examinations as part of the National Free Medical Examination Program, all participants were invited to a face-to-face interview to answer a standardized questionnaire. The questionnaire included questions about age, sex, occupation, educational level, marital status (never married, living together, divorced, separated, or widowed), smoking habits (never smoking, past smoker, and current smoker), and drinking habits (never drinking, drinking alcohol < 7 days/week, and drinking daily). Physical activity was assessed using the short form of the International Physical Activity Questionnaire (IPAQ) [20, 21]. A history of physical illness was evaluated based on participants’ responses (yes or no) to questions about their history, past diagnoses made by physicians, and current or historical medication regimens. Diseases of interest included type 2 diabetes mellitus (T2DM), hyperlipidemia, heart disease (coronary artery disease or congestive heart failure), peptic ulcer disease, osteoarthritis, cancer, kidney disease, hepatic disease, biliary tract disease, and thyroid disease.
Blood pressure (BP) was measured by a trained interviewer using an Omron electronic sphygmomanometer. The participants were required to rest in a seated position for at least 5 min before the measurement. Measurements were always taken using the participants’ right upper arm. Hypertension was defined as either an average systolic blood pressure (SBP) ≥ 140 mmHg, and/or a measured average diastolic blood pressure (DBP) ≥ 90 mmHg [22], a diagnosis of hypertension made by a physician, or self-reported use of anti-hypertensive medications during the previous 2 weeks. Follow-up visits during which blood pressure measurements were taken were completed in July 2016.
Body weight was measured to the nearest 0.1 kg using a standard balance beam scale. Height was measured barefoot to the nearest 0.1 cm using a stadiometer. BMI was calculated as weight divided by height squared (kilogram per square meter). Obesity was defined as having a BMI greater than or equal to 28 kg/m2, using the criteria established by the Working Group on Obesity in China [23].
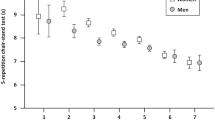
Physical performance was measured using the following tasks: the 4-m walking test and the TUGT. The 4-m walking test consists of participants being timed while walking 4 m at their usual pace. Walking aids were allowed for participants who typically use an aid to walk short distances [24]. Participants completed the test twice; the average time between the two trials was then calculated and used for further analysis. The TUGT beings with the participant sitting on a chair in a relaxed position with his/her upper body upright, his/her back flush with the back of the chair, his/her hands placed flat on his/her thighs, his/her feet on the ground, and his/her toes facing forward. The participant is timed as he/she rises from the chair, walks 3 m in any direction, and then returns to the chair. Walking aids were allowed [25]. Participants scoring in the top 20% on the TUGT or in the slowest 20% for the 4-m walking test were defined as having low physical performance [26, 27].
Statistical analysis
IPAQ responses at baseline were reported as medians ± 25–75th percentiles. All other continuous variables were presented as means plus standard deviations. Classification variables were reported as percentages. Regarding between groups comparisons of obesity and low physical performance alone, chi-square tests were conducted for categorical variables, Kruskal–Wallis test for skewed continuous variables, and t-tests for normally distributed continuous variables.
Linear regression models were used to examine the relationship between different groups and continuous performance outcomes. Adjusted means with 95% confidence intervals were obtained using the least squared means procedure. Logistic regression models where both obesity and low physical performance served as separate referents and as one combined referent were built; outcomes were compared between the different models. All models were adjusted for potential confounders known to affect hypertension, obesity, and low physical performance. Age, BMI, literacy, IPAQ results, diabetes, hyperlipidemia, heart disease, and cancer were included in these models. All statistical analyses were performed using SPSS v 19.0 (SPSS Inc, Chicago, IL). P values of less than 0.05 were considered statistically significant.
Results
Overall characteristics
800 participants were initially enrolled. 429 were excluded due to having baseline hypertension, 19 were lost to follow-up (3 deaths, 5 institutionalized, and 11 bedridden), and 3 participants were found to have incomplete data. 349 participants (150 men, 199 women; mean age at baseline 66.30 ± 5.78 years) were ultimately included in the final analysis. The detailed selecting information is showed in Figure 1.
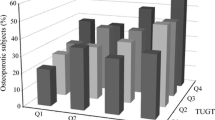
At 1-year follow up, 89 (25.5%) participants had new onset hypertension. Obesity and low physical performance rates are shown in Table 1. Overall, 33.8% of women and 28.9% of men were non-obese and had no low physical performance. 14.3% of non-obese women and 9.5% of non-obese men were classified as having low physical performance. 5.7% of women and 3.2% of men who are obese with normal physical performance. Finally, 3.2% of women and 1.4% of men were both obese and had low physical performance. Overall participants with low physical performance were older than other subjects. Participants who were both obese and had low physical performance had lower 4-m walking test and TUGT scores than the participants who were not obese and did not have low physical performance and the participants who were obese but did not have low physical performance; however, those who were both obese and had low physical performance had no significant difference to participants who had low physical performance but were not obese. Participants who were obese and had low physical performance had a higher incidence of heart disease and cancer when compared with other groups.
Risk of new incidence of hypertension
Compared to other groups, participants who were both obese and had low physical performance had an increased incidence of hypertension. The associations between obesity and low physical performance and the risk of developing hypertension are explored in Table 2. The adjusted risk of the incidence of hypertension was progressively greater in obese subjects with low physical performance (OR = 7.30, 95% CI = 1.36–39.11). This was not the case for participants who had low physical performance but were not obese (OR = 0.98, 95% CI = 0.29–3.27) or for participants who were obese but did not have low physical performance (OR = 1.40, 95% CI = 0.68–2.88). Interactions between obesity and low physical performance in the final regression model were found to be significant (P < 0.001).
Discussion
As far as we know, this is the first study to address the associations between obesity, low physical performance, and the incidence of hypertension in a Chinese community-dwelling older population. The results of this study provide evidence that, after adjustments for potential confounders, the combination of obesity and low physical performance increase the risk of hypertension in a Chinese community-dwelling older population, but obesity and low physical performance independently do not increase the risk of hypertension in the older adults.
The incidence of hypertension
At the 1-year follow-up 25.5% of participants (26.7% of men and 24.6% of women) had developed new onset hypertension. This finding was similar to a study that found that the incidence of hypertension was 26.9% in an older population with an average age of 65 years (65.7 ± 0.8) [28].
Obesity does not precipitate new onset hypertension
Our results show that obesity alone does not precipitate new onset hypertension after one year. More specifically there was no difference in the percent body fat between the non-hypertensive subjects and the subjects with new onset hypertension (28.67 ± 8.73% Vs 29.43 ± 8.98%, P > 0.05). Our results are similar to previous findings that obesity alone is not associated with hypertension [29]. Our obesity indicator was BMI, and they used abdominal circumference. However, other evidence [30] has indicated that BMI is the best predictor of new onset hypertension and that the risk of hypertension increases with a higher BMI [31,32,33]. Several studies have even shown a clear association between an increase in blood pressure and an increase in obesity [5, 6] possibly because 60% of hypertension is attributable to an increase in adipose stores [6].
The controversy regarding the association between BMI and hypertension has been studied specifically in Chinese population [34, 35]. Chen et al. studied a Taiwanese community in China and found that an increase in BMI was associated with a greater risk of new onset hypertension in men, but that this was not the case for women unless menopausal status was statistically adjusted for as menopause does impact blood pressure [34, 36]. Another study conducted in the study of Jiangsu Province in China found that, regardless of the menopausal status of women, changes in BMI were associated with the incidence of hypertension in men and women [35]. However, in contrast to our definition of obesity as having a BMI ≥ 28 kg/m2, that study [35] defined obesity as having a BMI ≥ 25 kg/m2, a cut-off value that may not be appropriate for an older Chinese population as BMI cutoffs for older people should be increased [31]. The potential mechanisms linking obesity and hypertension are not entirely clear. In our study, obesity as defined by BMI alone was not an independent predictor of incident hypertension, which may be due to our short follow-up time and small sample size, and we intend to extend the follow-up time and increase the sample size to see if this leads to any change. In addition, there are many kinds of obesity, and there are also differences in race and population.
Low physical performance do not precipitate new onset hypertension
Although there were significant differences in the TUGT (8.49 ± 1.98 s Vs 9.16 ± 1.97 s, P = 0.007) and the 4-m walking tests (1.01 ± 0.17 m/s Vs 0.94 ± 0.13 m/s, P < 0.001) between subjects who developed hypertension and those that did not, the results of our regression analyses did not show that low physical performance precipitate new onset hypertension after one year. This may be in line with research [37] that showed that blood pressure below 120/80, rather than hypertension, is associated with an increased risk of low physical performance in people aged ≥ 60 years and an increased risk for poor health outcomes among frail older people [38]. However, it is in contrast to previous studies suggesting that hypertension in the older adults is associated with both lower gait speed and a more rapid decline in gait speed most likely due to the impact hypertension has on cerebral blood vessels [7,8,9]. This discrepancy may be due to a difference in how low physical performance was defined in different studies. In this study, we used a simple and reliable measurement method, which is considered to be a better predictor of health risk, to evaluate the physical performance of the elderly. These measurements can not only predict the occurrence of disability in non-disabled people [39], but also more comprehensive than the scale evaluation method [40].
The combination of obesity and low physical performance can increase the incidence of hypertension
Although obesity alone and low physical performance alone did not affect the incidence of hypertension, the combination of these two increased the incidence of hypertension by 7.3 times within one years. Although there are no previous studies available for comparison that evaluated this relationship, there may be several reasons for the association between the combination of obesity and of low physical performance and the increased incidence of hypertension. Having a low physical performance implies an increased risk for weight gain because one becomes less physically active while obesity implies an increased risk for developing a low physical performance because the additional weight on the knee joints is associated with musculoskeletal impairments and because obesity accelerates age-related declines in functional ability. Therefore either condition increase the risk for eventually having the combination of both obesity and a low physical performance [19, 41,42,43]. The mechanism behind how this combination precipitates hypertension is less clear, but it is known that the renin-angiotensin-aldosterone system and the sympathetic system are overactivated in obese subjects, both of which would increase blood pressure [44]. Furthermore, hyperinsulinemia and decreased insulin sensitivity, which are associated with obesity, may also form a necessary link between the combination of obesity and having a low physical performance and hypertension, although this interaction has yet to be fully explained.
Strengths and limitations
The main strength of this study is that it is the first cohort study to report that the combination of obesity and having a low physical performance is a strong risk factor for the incidence of hypertension in Asia. Despite extensive efforts to curb study limitations, some limitations did exist. First, our participants were relatively healthy, as we did not include participants who were unable to participate in the free annual national physical examination. Thus, this choice could constitute a healthy selection bias. Second, the follow-up period was short. In future research, we plan to increase sample sizes and extend the time to follow-up to increase statistical power to evaluate the relationships between obesity, low physical performance, and hypertension. Third, many of the variables were self-reported and may have been subject to recall bias.
Conclusion
In summary, our results indicate that the combination of obesity and having a low physical performance increased the risk of new onset hypertension in Chinese community-dwelling older adults. One of the clinical implications of this study is that the combination of obesity and having a low physical performance can be used to identify individuals at a high risk for developing hypertension. These individuals can then receive lifestyle interventions to prevent the development of hypertension. Cutoff levels for obesity and standardizing the definition of having a low physical performance warrant further investigation in order to better stratify the risk of hypertension.
Summary
What is known about topic
-
Obesity is associated with hypertension.
-
Low physical performance is associated with hypertension.
What this study adds
-
Obesity and low physical performance did not independently affect the incidence of hypertension after one year.
-
The combination of the two can significantly increase the incidence of hypertension in Chinese community-dwelling older adults.
References
Zhang Y, Zhou Z, Gao J, Wang D, Zhang Q, Zhou Z, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. 2016; 16:277.
Sheng CS, Liu M, Kang YY, Wei FF, Zhang L, Li GL, et al. Prevalence, awareness, treatment and control of hypertension in elderly Chinese. Hypertens Res. 2013;36:824–8.
Collaborators GRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659–724.
Yang X, Yang G, Li W, Zhang Y, Wang J. Therapeutic effect of Ilex hainanensis Merr. extract on essential hypertension: a systematic review and meta-analysis of randomized controlled trials. Front Pharm. 2018;9:424.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med. 2004;164:2126–34.
Ma WJ, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, et al. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens. 2012;25:590–6.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories. JAMA. 2013;309:71–82.
Veronese N, Cereda E, Solmi M, Fowler SA, Manzato E, Maggi S, et al. Inverse relationship between body mass index and mortality in older nursing home residents: a meta-analysis of 19,538 elderly subjects. Obes Rev. 2015;16:1001–15.
Wang J, Taylor AW, Zhang T, Appleton S, Shi Z. Association between body mass index and all-cause mortality among oldest old Chinese. J Nutr Health Aging. 2018;22:262–8.
Emmerzaal TL, Kiliaan AJ, Gustafson DR. 2003-2013: a decade of body mass index, alzheimer’s disease, and dementia. J Alzheimers Dis. 2015;43:739–55.
Yu R, Wong M, Leung J, Lee J, Auyeung TW, Woo J. Incidence, reversibility, risk factors and the protective effect of high body mass index against sarcopenia in community-dwelling older Chinese adults. Geriatr Gerontol Int. 2014;14(Suppl 1):15–28.
Han P, Zhao J, Guo Q, Wang J, Zhang W, Shen S, et al. Incidence, risk factors, and the protective effect of high body mass index against sarcopenia in suburb-dwelling elderly Chinese populations. J Nutr Health Aging. 2016;20:1056–60.
Busch TDA, Duarte YA, Pires Nunes D, Lebrão ML, Satya Naslavsky M, Dos Santos Rodrigues A. et al. Factors associated with lower gait speed among the elderly living in a developing country: a cross-sectional population-based study. BMC Geriatr. 2015;15:35.
Rosano C, Longstreth WT, Boudreau R, Taylor CA, Du Y, Kuller LH, et al. High blood pressure accelerates gait slowing in well-functioning older adults over 18-years of follow-up. J Am Geriatr Soc. 2011;59:390–7.
Dumurgier J, Elbaz A, Dufouil C, Tavernier B, Tzourio C. Hypertension and lower walking speed in the elderly: the three-city study. J Hypertens. 2010;28:1506–14.
Odden MC, Peralta CA, Berlowitz DR, Johnson KC, Whittle J, Kitzman DW, et al. Effect of intensive blood pressure control on gait speed and mobility limitation in adults 75 years or older. JAMA Intern Med. 2017;177:500–7.
Forhan M, Gill SV. Obesity, functional mobility and quality of life. Best Pr Res Cl En. 2013;27:129–37.
de Munter JS, Tynelius P, Ahlström G, Rasmussen F. The bidirectional association between body weight and mobility disability: a population based cohort. Disabil Health J 2016;9:632–7.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Zhang W, Shen S, Wang W, Zhou C, Xu L, Qiu J, et al. Poor lower extremity function was associated with Pre-Diabetes and diabetes in older chinese people. PLoS One. 2014;9:e115883.
Writing Group of 2010 Chinese Guidelines for the Management of Hypertension 2010 Chinese guidelines for the management of hypertension. Chin J Hypertens. 2011;19:701–43.
Zhou BF. China CMGO. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in chinese adults - study on optimal cut-off points of body mass index and waist circumference in chinese adults. Biomed Environ Sci. 2002;15:83–96.
Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 1985;2003:1851–60.
Shimada H, Suzuki T, Suzukawa M, Makizako H, Doi T, Yoshida D, et al. Performance-based assessments and demand for personal care in older Japanese people: a cross-sectional study. BMJ Open. 2013;3:e2424.
Ishii S, Tanaka T, Shibasaki K, Ouchi Y, Kikutani T, Higashiguchi T, et al. Development of a simple screening test for sarcopenia in older adults. Geriatr Gerontol Int. 2014;14:93–101.
Li CI, Li TC, Lin WY, Liu CS, Hsu CC, Hsiung CA, et al. Combined association of chronic disease and low skeletal muscle mass with physical performance in older adults in the Sarcopenia and Translational Aging Research in Taiwan (START) study. BMC Geriatr. 2015;15:11.
Dauphinot V, Roche F, Kossovsky MP, Schott A, Pichot V, Gaspoz J, et al. C-reactive protein implications in new-onset hypertension in a healthy population initially aged 65 years: the proof study. J Hypertens. 2009;27:736–43.
Fujii M, Ohnishi H, Saitoh S, Akasaka H, Miura T, Mori M. The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno-Sobetsu study. Hypertens Res. 2015;38:426–32.
Gupta S, Kapoor S. Optimal cut-off values of anthropometric markers to predict hypertension in north indian population. J Commun Health. 2012;37:441–7.
Nguyen TT, Adair LS, He K, Popkin BM. Optimal cutoff values for overweight: using body mass index to predict incidence of hypertension in 18- to 65-year-old Chinese adults1,2. J Nutr. 2008;138:1377–82.
Nyamdorj R. BMI compared with central obesity indicators in relation to diabetes and hypertension in asians. Obes (Silver Spring) 2008;16:1622–35.
Uchiyama A, Shimizu T, Nakagawa T, Tanaka T. Association of hypertension with changes in the body mass index of university students. Environ Health Prev Med. 2008;13:271–80.
Chen PC, Sung FC, Su TC, Chien KL, Hsu HC, Lee YT. Two-year change in body mass index and subsequent risk of hypertension among men and women in a Taiwan community. J Hypertens. 2009;27:1370–6.
Luo W, Chen F, Guo Z, Wu M, Hao C, Zhou Z, et al. Comparison of the suitability of 2 years change in waist circum- ference and body mass index in predicting hypertension risk: a prospective study in Chinese-Han. Iran J Public Health. 2014;43:1212–20.
Zanchetti A, Facchetti R, Cesana GC, Modena MG, Pirrelli A, Sega R, et al. Menopause-related blood pressure increase and its relationship to age and body mass index: the SIMONA epidemiological study. J Hypertens. 2005;23:2269–76.
Welmer AK, Angleman S, Rydwik E, Fratiglioni L, Qiu C. Association of cardiovascular burden with mobility limitation among elderly people: a population-based study. PLoS One. 2013;8:e65815.
Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults. Arch Intern Med. 2012;172:1162–8.
Ostir GV, Markides KS, Black SA, Goodwin JS. Lower body functioning as a predictor of subsequent disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 1998;53:M491–5.
Bohannon RW, DePasquale L. Physical Functioning Scale of the Short-Form (SF) 36: internal consistency and validity with older adults. J Geriatr Phys Ther. 2010;33:16–18.
Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L. The impact of obesity on the musculoskeletal system. Int J Obes. 2008;32:211–22.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Bell JA, Sabia S, Singh-Manoux A, Hamer M, Kivimaki M. Healthy obesity and risk of accelerated functional decline and disability. Int J Obes. 2017;41:866–72.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure. Hypertension. 2003;42:878–84.
Acknowledgements
The authors thank Guiyan Shao from the Chadian public health center and Xiaofang Ren from Hangu welfare house for providing place and organization.
Funding
This work was supported by the National Natural Science Foundation of China (81372118); the Hygiene and Health Commission of Shanghai Municipality (2019HP76).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Chen, Y., Han, P. et al. Combined effect of obesity and low physical performance on the incidence of hypertension in Chinese community-dwelling older population. J Hum Hypertens 35, 970–977 (2021). https://doi.org/10.1038/s41371-020-00442-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00442-y
- Springer Nature Limited