Abstract
The aim of the study was to determine the cut-offs of anthropometric markers for detecting hypertension in an endogamous North Indian population. A cross-sectional study was carried out to collect data from 578 adult Aggarwal Baniya subjects (271 men and 307 women, mean age: 43.4 ± 5.3 and 38.7 ± 4.9 respectively) using multistage, stratified sampling method. Individual body weight, height, waist circumference (WC), hip circumference, blood pressure were assessed. Receiver operating characteristic (ROC) analysis was used to find out the optimal cut-off values of various anthropometric markers to predict hypertension. The likelihood ratios for having hypertension in subjects with various cut-off values were calculated. Logistic regression analysis was used to examine the independent relationship between the anthropometric markers and odds of having hypertension. The BMI cut-off to predict hypertension was 22.8 kg/m2 in men and 28.8 kg/m2 in women. The optimal WC cut-offs varied from 91–92 cm in both men and women. The WHR cut-off was about 0.90 in men and 0.78 in women respectively, and the optimal WHtR cut-off was 0.56 in men and 0.43 in women. The cut-off levels for BMI, WC and WHtR corresponded to the inflexion points in the likelihood ratio graphs. The area under curve (AUC) and odds ratios showed that the risk of having hypertension was highest with respect to increased BMI and that BMI is the best predictor of having hypertension. The cut-off points for detecting cardiovascular risk factors among our population are lower than the criteria by the World Health Organization. Although these results may not be readily applied to the rest of the Indian populations due to the multiethnic composition, they point to the necessity of similar studies with large randomized samples to find the cut-off levels for chronic conditions in different populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association of adiposity with cardiovascular risk factors is well established. However classified, the burden of major risk factors is substantially greater in overweight than in lean individuals. Epidemiological studies focusing on persons of European descent have verified that obesity standards based on BMI by WHO [1] are, indeed, associated with incremental risk for cardiovascular events and all-cause death [2, 3]. However it has been found that cardiovascular and metabolic risk in Asians occur at a lower BMI than in Europeans. There is increasing evidence of a high prevalence of type 2 diabetes mellitus and elevated cardiovascular risk in certain Asian countries, despite an average BMI in these countries that is <25 kg/m2 [4, 5]. McNeely et al. [6] found that for Asian-Americans, the prevalence of diabetes mellitus after adjustment for BMI was 60% higher than in their European counterpart.
To address the issue that the international cut off points may not accurately reflect risk in non-European populations, the panel recommended ranges of BMI for determining potential public health and clinical action, which countries may pursue through the use of scientifically sound approaches to make decisions about the definition of obesity related risk in their own population [7]. Although based on the revised standards, Indian have been categorized under the high vulnerability group. Besides, these revised standards of BMI are based on the data obtained in Korea and Hongkong who are of Mongoloid origin and that group constitutes a sizeable fraction of Indian population residing in North-East. This has generated debate about the appropriateness of ethnic-specific cut-off points for defining obesity [8]. Besides population of mongoloid features we have many ethnic groups in India exhibiting varied physical features and physical types, therefore, it is not advisable to blindly accept this BMI scheme without testing to avoid further complications.
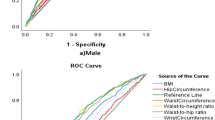
In this study, we examined four anthropometric markers (BMI, WC, WHR, WHtR) with hypertension and used receiver operating characteristic (ROC) analysis to assess the optimal cut-off values of these anthropometric markers for overweight or obese in an endogamous population of North India.
Materials and Methods
Data for the present study was collected on 578 adult Aggarwal Baniya subjects (271 men, 307 women) aged 30 years upwards using multistage, stratified sampling method.
Target Population
Baniyas is an endogamous caste group which is divided into three sub groups based on language difference. These languages are Hindi, Marwari and Punjabi. However, they are not identified as Punjabi Baniyas, Malwari Baniyas or Hindi Baniyas. They are the trading community which mostly have sedentary lifestyle. Their food habits also involve lots of oily eatables which dispose them to many cardiovascular health risk. They are divided into 18 gotras. They generally practice caste endogamy and gotra exogamy. Marriage is monogamous.
Data Collection
Participants were interviewed through structured proforma. Anthropometric measurements including height, weight, skinfold thickness, waist and hip circumference and blood pressure measurements were obtained using standardized procedures. Various indices of obesity such as body mass index (BMI), waist hip ratio (WHR), waist to height ratio (WHtR) was further calculated.
Body weight was measured by using spring balance to the nearest 500 gm, stature with the help of Martin’s Anthropometer to the nearest mm. Waist circumference and hip circumference were measured with a non stretchable steel tape measure to the nearest 0.1 cm. Measurements were conducted by trained personnel and all instruments were calibrated once weekly. Blood pressure was measured using manual (mercury) sphygmomanometer. The subject was asked to sit relaxed on a chair with her or his arm supported comfortably at the vertical level. The pressure cuff was applied closely to the upper arm, the cuff was rapidly inflated until the artery was completely occluded. The stethoscope was the placed lightly over the brachial artery, and the mercury column was allowed to fall at the rate of 2 mmHg per second. The Systolic blood pressure was determined by the appearance of Korotkoff sound. After recording the systolic blood pressure the mercury column was allowed to fall further till the sound ceased to be tapping in quality, become fully muffled and finally disappeared. The level where it disappeared was taken as diastolic blood pressure. Three reading were taken for each measurement and there mean was taken as the final reading.
The protocol for the study was reviewed and approved by Ethical Committees in the Department of Anthropology, Faculty of Sciences of the University of Delhi, India.
Statistical Analysis
Data was analyzed using the computer software SPSS version 15.0 for windows (SPSS Inc., Chicago, USA). Results have been described by summary statistics such as mean and standard deviation. Receiver operating characteristic (ROC) analysis was used to compare the predictive validity, and to determine their optimal cut-off values [9–11]. Area under the curve (AUC) was also measured to determine the diagnostic power of a test, and to describe the probability that a test would correctly identify subjects with the disorder. Optimal cut-off values were measured by calculating the sensitivity and specificity of the anthropometric measurements at various cut-off points. Odds ratios were calculated as the ratios of having hypertension by the proposed cut-off points.
The likelihood ratio (LR) was calculated to estimate the odds of having hypertension in subjects with various cut-off values of the anthropometric indexes [12]. LR is defined as sensitivity/(1−specificity). The sensitivity and specificity of having chronic conditions at various anthropometric cut-off values were calculated using the adjusted population classified with reference to each cutoff level and hence the corresponding LR was derived. Since LR refers to actual test results before disease status is known, it is more immediately useful to clinicians than sensitivity and specificity [12].
Results
The means and standard deviations of various anthropometric markers are presented in Table 1. A high prevalence of obesity in this community is evident in the gender specific mean BMI values (men, 26.1 kg/m2; women, 29.4 kg/m2). Although the women were 3 BMI units heavier than the men, the systolic blood pressure (SBP) and diastolic blood pressure (DBP) values were significantly higher among men. As expected, women had significantly larger hip circumferences compared with men whereas waist circumference was higher in men.
ROC curve analysis of various anthropometric markers with hypertension are summarized in Table 2. The results of the AUC analysis were significantly different from what was expected by chance (P < 0.05). Among the markers of obesity, BMI showed the highest AUC in both men and women. The values for AUC tented to be higher in men than in women. The AUCs for BMI was-0.72 in men, 0.62 in women; for WC-0.71 in men, 0.55 in women; for WHR-0.64 in men, 0.45 in women and for WHtR-0.69 in men, 0.60 in women. The cut-off points of the variables to detect the risk factors were determined as the point of intersection of the curves for sensitivity and specificity. The optimal BMI cut-off values for predicting hypertension was 22.8 kg/m2 in men and 28.8 kg/m2 in women. The optimal WC cut-off values was 92.0 cm in men and 91.3 cm in women. The optimal cut-off values of WHR that correctly identified the highest numbers of subjects with or without hypertension was 0.90 in men and 0.78 in women whereas the optimal WHtR cut-off values was 0.56 in men and 0.43 in women.
Figures 1 and 2 shows the likelihood ratios of having hypertension in subjects with different values for these four anthropometric indexes. The cut-off levels for BMI, WC and WHtR corresponded to the inflexion points in the likelihood ratio graphs. There was a significant increase in the risks for hypertension beyond the cut-off points for all anthropometric markers except WHR in both genders.
Logistic regression analysis was performed to see if the determined cut-off points of various markers of obesity, that is BMI, WC, WHR and WHtR independently reflected the increased risk of having hypertension (Table 3). For systolic blood pressure, odds ratio for BMI, WC and WHtR were significant in men whereas in women, odds ratio for BMI and WC were significant. For diastolic blood pressure, odds ratio for all anthropometric markers were statistically significant except for WHtR in women. In men, the odds of higher systolic blood pressure (SBP) or diastolic blood pressure (DBP) was significantly more in those who had BMI, WC or WHtR in risk category whereas in women it was significant for all markers except for WHtR.
Discussion
Obesity is an independent risk factor for cardiovascular disease (CVD) and it is known to be associated with other risk factors such as hypertension, dyslipidaemia and diabetes mellitus. Body mass index is known to be closely related to the total amount of body fat and is widely used to define the criteria for overweight or obesity [13]. Many population studied showed increasing morbidity and mortality risk with increasing BMI [14].
The recent data showed excess cardiovascular morbidity at the ‘normal’ range of body mass index (BMI) in the Asian populations. In Hong Kong Chinese men, the optimal BMI cutoff to predict diabetes, hypertension and dyslipidemia was lower than currently recommended for the diagnosis of obesity [15]. Similar data showing high cardiovascular-related morbidities at upper ‘normal’ BMI range have been reported for the ethnic groups in several Asian countries: Korea [16], Singapore [17], Japan [18], and Taiwan [19]. Therefore, WHO recently proposed lower BMI values to define overweight and obesity in people of the Asia–Pacific region [7]. However, the cut-off values of overweight and obesity in these regions were only based on data from few reports, predicted on small-scale or cross-sectional studies. Data from Indian population is lacking to verify these cut-offs. Therefore, the present study is an attempt to verify these cut-off values which examine the health risk of obesity.
The four anthropometric markers studied (BMI, WC, WHR and WHtR) have all been noted to be associated with several CVD risk factors [20–24]. Some studies have reported WC as the better predictor of CVD risk factors [25–27] whereas others recommended WHR and WHtR [15].
In the present study, the cut-off points of anthropometric variables for detecting risk factors were lower than those recommended by WHO [1]. WHO recommended BMIs of 25 and 30 kg/m2 as cutoff points for overweight and obesity, respectively. In our population, the specificity of these values to predict risk factors in men was more than 70%, but the sensitivity was less than 20% whereas in women the specificity of these values to predict risk factors was 72%, but the sensitivity was only 46%. The cut-off points of WC and WHR set by WHO were 102 cm and 1.0 for males and 88 cm and 0.85 for females, respectively. The specificity of these cut-off points for predicting risk factors was more than 35%, with a sensitivity of less than 55% for males and less than 70% for females. Accordingly, it is suggested that the WHO cut-off points may not be sufficiently sensitive and accurate for detecting cardiovascular risk factors in the Indian population.
Of the four anthropometric markers we studied, BMI was found to have the largest area under the ROC curve in relation to hypertension among both men and women. Our result suggested that BMI was a better predictor of CVD risk factors as compared to other anthropometric markers. BMI is closely related to the total amount of body fat and is used to define the criteria of overweight or obesity [13, 28] Both obesity related morbidity and mortality risk have been shown to increase with increasing BMI in population study [29]. In our study, we also found the increasing risk of hypertension with increasing BMI in both genders.
The optimal cut-off values of BMIs for overweight or obesity from our study were found to be 22.8 kg/m2 in men and 28.8 kg/m2 in women, which were similar in men but different in women to those of other studies [15, 30, 31]. As mentioned previously, Asians with lower BMIs have been found to be at increased risk for obesity. Taken together, our study supported the conclusion that cut-off values using BMI to define obesity should be much lower in Indian population than in Western countries.
The increasing risk of having hypertension was also found to be associated with increasing WC in both sexes (Fig. 2). The optimal cut-off values using WC were 92.0 cm in men and 91.3 cm in women in our study. These values of WC in men were apparently lower than the values for Caucasians (102 cm) [1] but were higher then that recommended for Asians (90 cm) [7]. The values for WC in women were much higher than those recommended for Caucasians (88 cm) and Asians (80 cm). In summary, further studies are needed to find out the appropriate cut-off values for overweight and obesity in the Asia–Pacific region. Similarly, the cut-off points for WHR and WHtR in the present study were also found lower than those recommended by WHO. Further, higher cut-off points of all anthropometric markers for men compared with women indicate sex-specific relations between obesity and cardiovascular risk factors as observed by other researcher also [32–34].
In conclusion, the cut-off points of anthropometric markers (except for WC) for detecting cardiovascular risk factors in the Indian population were lower than the WHO criteria. Though these cut-off values for men were in good accordance with those reported for Asians, they were much higher for women indicating need for further research in ascertaining the cut-off values for Asian population. Although these results may not be readily applied to the rest of the Indian populations, they point to the necessity for similar studies with large randomized samples to find the cut-off levels for chronic conditions in different populations.
References
World Health Organization. (1998). Obesity: Preventing and managing the global epidemic. Report of a WHO consultation of obesity, 3–5 June. WHO: Geneva.
Calle, E. E., Thun, M. J., Petrelli, J. M., Rodriguez, C., & Heath, C. W. (1999). Body-mass index and mortality in a prospective cohort of US adults. New England Journal of Medicine, 341, 1097–1105.
Mora, S., Yanek, L. R., Moy, T. F., Fallin, M. D., Becker, L. C., & Becker, D. M. (2005). Interaction of body-mass index and Framingham risk score in predicting incident coronary disease in families. Circulation, 111, 1871–1876.
WHO Expert Consultation. (2004). Appropriate body-mass Index for Asian populations and its implications for policy and intervention strategies. Lancet, 363, 157–163.
Deurenberg-Yap, M., & Deurenberg, P. (2003). Is a reevaluation of WHO body mass index cut-off values need? The case of Asians in Singapore. Nutrition Reviews, 61, S80–S87.
McNeely, M. J., & Boyko, E. J. (2004). Type 2 diabetes prevalence in Asian Americans. Diabetes Care, 27, 66–69.
WHO/IASO/IOTF. (2000). The Asia-Pacific perspective: Redefining obesity and its treatment. Melbourne: Health Communications Australia.
Steven, J. (2003). Ethnic-specific cut-points for obesity vs country-specific guidelines for action. International Journal of Obesity and Related Metabolic Disorders, 27, 287–288.
Swets, J. A. (1973). The relative operating characteristics in psychology. Science, 182, 990–1000.
Metz, C. E. (1978). Basic principles of ROC analysis. Seminars in Nuclears Medicine, 8, 283–298.
Van der Schouw, Y. T., Verbeek, A. L. M., & Ruijs, J. H. J. (1992). ROC curves for the initial assessment of new diagnostic tests. Family Practice, 9, 506–511.
Simel, D. L., Samsa, G. P., & Matchar, D. B. (1991). Likelihood ratios with confidence: Sample size estimation for diagnostic test studies. Journal of Clinical Epidemiology, 44, 763–770.
Gallagher, D., Visser, M., Sepulveda, D., Pierson, R. N., Harris, T., & Hemysfield, S. B. (1996). How useful is body mass index for comparison of body fatness across age, sex and ethnic groups? American Journal of Epidemiology, 143, 228–239.
Kopelman, P. G. (2000). Obesity as a medical problem. Nature, 404, 635–643.
Ko, G. T. C., Chan, J. C. N., Cockram, C. S., & Woo, J. (1999). Prediction of hypertension, diabetes, dyslipidemia or albuminuria using simple anthropometric indexes in Hong Kong Chinese. International Journal of Obesity and Related Metabolic Disorders, 23, 1136–1142.
Moon, O. R., Kim, N. S., Jang, S. M., Yoon, T. H., & Kim, S. O. (2002). The relationship between body mass index and the prevalence of obesity-related diseases based on 1995 National Health Interview Survey in Korea. Obesity Review, 3, 191–196.
Deurenberg-Yap, M., Chew, S. K., Lin, V. F., Tan, B. Y., van Staveren, W. A., & Deurenberg, P. (2001). Relationships between indices of obesity and its comorbidities in multi-ethnic Singapore. International Journal of Obesity and Related Metabolic Disorders, 25, 1554–1562.
Ito, H., Nakasuga, K., Ohshima, A., Maruyama, T., Kaji, Y., Harada, M., et al. (2003). Detection of cardiovascular risk factors by indices of obesity obtained from anthropometry and dual-energy X-ray absorptiometry in Japanese individuals. International Journal of Obesity and Related Metabolic Disorders, 27, 232–237.
Lin, W. Y., Lee, L. T., Chen, C. Y., Lo, H., Hsia, H. H., Liu, I. L., et al. (2002). Optimal cut-off values for obesity: Using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. International Journal of Obesity and Related Metabolic Disorders, 26, 1232–1238.
Kannel, W. B. (2000). Risk stratification in hypertension: New insight from the Framingham study. American Journal of Hypertension, 13, 3S–10S.
Dı′az, M. E. (2002). Hypertension and obesity. Journal of Human Hypertension, 16, S18–S22.
Dalton, M., Cameron, A. J., Zimmet, P. Z., et al. (2003). Waist circumference, waist–hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. Journal of Internal Medicine, 254, 555–563.
Ferguson, T. S., Younger, N. O., Tulloch-Reid, M. K., et al. (2008). Prevalence of prehypertension and its relationship to risk factors for cardiovascular disease in Jamaica: Analysis from a cross-sectional survey. BMC Cardiovascular Disorders, 8, 20.
Gupta, S., & Kapoor, S. (2010). Sex differences in blood pressure levels and its association With obesity indices: Who is at greater risk. Ethnicity and Disease, 2010(20), 370–375.
Rissanen, P., Hamalainen, P., Vanninen, E., Tenhunen-Eskelinen, M., & Uusitupa, M. (1997). Relationship of metabolic variables to abdominal adiposity measures by different anthropometric measurements and dual-energy X-ray absorptiometry in obese middle-aged women. International Journal of Obesity and Related Metabolic Disorders, 21, 367–371.
Han, T. S., Van Leer, E. M., Seidell, J. C., & Lean, M. E. J. (1995). Waist circumference action levels in the identification of cardiovascular risk factors: Prevalence study in a random sample. British Medical Journal, 311, 1401–1405.
Lean, M. E. J., Han, T. S., & Morrison, C. E. (1995). Waist circumference as a measure for indicating need for weight management. British Medical Journal, 311, 158–161.
Deurenberg, P., Yap, M., & Van Staveren, W. A. (1988). Body mass index and percent body fat: A meta-analysis among different ethnic groups. International Journal of Obesity and Related Metabolic Disorders, 22, 1164–1171.
Pi-Sunyer, X. (1991). Health implications of obesity. American Journal of Clinical Nutrition, 53, 1595s–1603s.
Zaher, Z. M., Zambari, R., Pheng, C. S., et al. (2009). Optimal cut-off levels to define obesity: Body mass index and waist circumference, and their relationship to cardiovascular disease, dyslipidaemia, hypertension and diabetes in Malaysia. Asia Pacific Journal of Clinical Nutrition, 18, 209–216.
Nguyen, T. T., Adair, L. S., Suchindran, C. M., He, K., & Popkin, B. M. (2009). The association between body mass index and hypertension is different between East and Southeast Asians. American Journal of Clinical Nutrition, 89, 1905–1912.
Rosenfalck, A. M., Almdal, T., Gotfredsen, A., & Hilsted, J. (1996). Body composition in normal subjects: Relation to lipid and glucose variables. International Journal of Obesity and Related Metabolic Disorders, 20, 1006–1013.
Ko, G. T. C., Chan, J. C. N., Woo, J., et al. (1997). Simple anthropometric indexes and cardiovascular risk factors in Chinese. International Journal of Obesity and Related Metabolic Disorders, 21, 995–1001.
Wu, C. H., Yao, W. J., Lu, F. H., Wu, J. S., & Chang, C. J. (1998). Relationship between glycosylated hemoglobin, blood pressure, serum lipid profiles and body fat distribution in healthy Chinese. Atherosclerosis, 137, 157–165.
Acknowledgments
The financial assistance to SG from Indian Council of Medical Research (ICMR) is gratefully acknowledged. We extend our gratitude to all our participant without whom cooperation this data could not have been known. We also acknowledge the support of Department of Anthropology, University of Delhi, India for providing us the infrastructure for conducting our study.
Conflict of interest
No conflict of interest was declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, S., Kapoor, S. Optimal Cut-Off Values of Anthropometric Markers to Predict Hypertension in North Indian Population. J Community Health 37, 441–447 (2012). https://doi.org/10.1007/s10900-011-9461-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-011-9461-8