Abstract
The objective of this study was to characterize cardiac sympathetic denervation in Parkinson's disease (PD) patients without neurogenic orthostatic hypotension (NOH), both in terms of hemodynamics and in its relation with vascular denervation. We studied 20 PD patients without NOH. We analyzed the heart rate and blood pressure variability during various physical maneuvers. The following parameters were calculated: expiratory-inspiratory ratio, stroke volume, cardiac output, cardiac index, left ventricular ejection time, left ventricular work index, thoracic fluid content, total peripheral resistance and baroreflex sensitivity (BRS). We also measured direct and spectral derivatives of cardiac (cardiovagal) parasympathetic function. Myocardial I-123 metaiodobenzylguanidine (MIBG) scintigraphy was performed and early and late heart/mediastinum uptake ratios were analyzed. We observed that the late heart/mediastinum uptake ratio was 1.33±0.21. This parameter was correlated with years since diagnosis (correlation coefficient:−0.485; P=0.05), Unified Parkinson’s Disease Rating Scale (UPDRS) III score (cc:−0.564; P=0.02) and pressure recovery time in the Valsalva maneuver (cc: 0.61; P<0.001). At rest, it was correlated with BRS (cc:0.75; P=0.003) and low-frequency diastolic blood pressure (LFDBP; cc: 0.58;P=0.017). We found no correlations with any of the cardiography impedance variables. In linear regression models, the variable that best correlated with MIBG results was LFDBP. Our results support that in absence of NOH the degree of denervation of the heart does not produce any effect on its inotropic function. Moreover, BRS and LFDBP can be used as an indirect measure of cardiac sympathetic denervation at rest.
Similar content being viewed by others
Introduction
Neurogenic orthostatic hypotension (NOH) is a common finding in Parkinson's disease (PD) affecting 30–40% of patients.1, 2 It results from the postganglionic sympathetic denervation that affects the heart and blood vessels3, 4, 5, 6 in PD. Interestingly, functional studies using I-123 metaiodobenzylguanidine (MIBG) myocardial scintigraphy reveal that this denervation is present in up to 80% of PD patients,7, 8 implying that many PD patients with these findings do not have NOH.8, 9 Indeed, cardiac sympathetic involvement seems to occur in the early stages of PD,10 possibly before the onset of motor clinical symptoms, as described in patients carrying high-penetrance genetic mutations of PD.11, 12 By contrast, NOH is frequently detected later during advanced stages of PD. Furthermore, in early stages of the disease there is no correlation between the symptoms of orthostatic intolerance and myocardial MIBG scintigraphy measures in PD.
All these findings rise two main hypotheses regarding the pathophysiology of cardiocirculatory involvement in PD: (1) there is a staged damage and the sympathetic denervation starts in the heart and then spreads to the rest of the vascular system;8, 12, 13 (2) there is a simultaneous damage of the innervation for the heart and peripheral vasculature, which is functionally compensated in the initial phases of PD by hemodynamic mechanism counteracting the vascular denervation.14
To date, only few studies have analyzed specifically the hemodynamic manifestations of cardiac postganglionic sympathetic denervation in PD patients and its relation with the staging of cardiocirculatory involvement.15
In this study, we have assessed the hemodynamic behavior of a series of PD patients without NOH using cardiac MIBG scintigraphy and non-invasive autonomic tests. Our objective was twofold: to define the hemodynamic profile of PD patients with cardiac sympathetic denervation, and to assess whether cardiac and vascular sympathetic denervation occurred simultaneously or in an organ-specific manner, with an initial selective affectation of the heart spreading to the rest of the vascular system.
Materials and methods
We performed a cross-sectional evaluation of 20 patients fulfilling Parkinson’s UK Brain Bank criteria for the diagnosis of PD16 (mean age 62.9±13.0 years and 7.7±5.9 years since diagnosis; eight women; Table 1). We prospectively selected consecutive eligible patients from the Movement Disorders and Autonomic Unit of University Hospital of Cruces who had been evaluated by cardiac MIBG scintigraphy and technetium (99mTc) 6-methoxy isobutyl isonitrile (99mTc-MIBI) single photon emission computed tomography (SPECT) in the last 6 months prior to study inclusion. We excluded patients with diabetes or with myocardial perfusion defects in the 99mTC-MIBI SPECT, and those patients who were not able to complete the test properly due to physical or cognitive disability. In order to discern more clearly the specific hemodynamic effects of cardiac sympathetic denervation, we also excluded subjects who presented NOH17 in our evaluation, either after 3 min of active standing or in tilt-table test (TTT). Although the primary aim of this study was to analyze the function of sympathetic innervation, we included variables accounting for direct and spectral derivatives of cardiac parasympathetic function (cardiovagal). A set of clinical-demographic data was also collected to further characterize the participants: gender, age and disease duration at study inclusion and the scoring of Unified Parkinson’s Disease Rating Scale (UPDRS) parts I–IV. Antiparkinsonian/dopaminergic medications were not withheld in the study. Of note, UPDRS was obtained before the first morning dose of dopaminergic treatment. The local research ethics committee approved the study, and all participants gave their written informed consent before they were admitted to the study.
Basic maneuvers for studying neurocirculatory dysfunction
The assessment was performed according to the accepted and standardized protocol of Ewing and Clarke autonomic function test,18 including cardiocirculatory responses to deep breathing, isometric handgrip, Valsalva maneuver (VM) and tilt test. Patients were assessed early in the morning under fasting conditions, and they were instructed to avoid the intake of any medication or food capable of modifying blood pressure in the previous 24 h. Heart rate and blood pressure variability were then assessed in supine rest (10 min) and in relation to different physical maneuvers: 20-min TTT at an inclination of 60 degrees, the VM (40 mm Hg for at least 15 s), isometric muscle contraction (using a handgrip dynamometer), and deep breathing (six inspiration/expiration cycles). The expiratory-inspiratory (E/I) ratio was calculated by dividing the longest mean inter-beat (RR) interval during expiration by the shortest RR interval during inspiration.
Autonomic dysfunction and hemodynamic measurements
A non-invasive hemodynamic monitoring device [Task Force Monitor (TFM), from CNSystems (Graz, Austria)], which provides beat-to-beat information, was used to study the patients. The heart rate was measured with an electrocardiogram; while impedance cardiography was used to calculate the stroke volume (SV), stroke index, cardiac output (CO=SV × heart rate), cardiac index (CI=CO/body surface area), left ventricular ejection time, left ventricular work index (LVWI=constant × (mean blood pressure − pulmonary artery occlusion pressure) × CI, acceleration index and thoracic fluid content.
Continuous beat-to-beat systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean blood pressure values were automatically measured in the right arm with TFM and with an oscillometric sphygmomanometer in the other arm. The calculation of the total peripheral resistance (TPR) was carried out based on the Ohm's law (TPR (mean arterial pressure − central venous pressure/CO)x 80).
Using autoregression analysis, the TFM automatically measures a set of variables accounting for the variability of the heart rate (RR interval) and of blood pressure: (1) the RR low-frequency (LFRR, 0.04–0.15 Hz) and high-frequency (HFRR, 0.15–0.40 Hz) bands; and (2) the DBP low-frequency band (LFDBP, 0.04–0.15 Hz). All the functions of this device have been validated and successfully used in recent clinical studies.19, 20
Calculation of the baroreflex sensitivity
We determined the spontaneous baroreflex sensitivity (BRS) by means of the so called ‘sequence method’.21 According to this method, RR interval and beat-to-beat SBP data are scanned and sequences of three or more beats in which the BP and RR interval concomitantly increase (or decrease) by more than a threshold value are identified (for BP, the threshold is ⩾1 mm Hg per heart beat and for RR interval ⩾4 ms per heart beat). The BRS is defined as the slope of the regression line between the data points in these sequences.
However, we also measured BRS in relation to VM. In this case, we obtained SBP and HR variation from baseline for all phases of VM to calculate adrenergic barosensitivity (BRS_a) and cardiovagal barosensitivity (BRS_v).
BRS_a was defined as the decrease in SBP associated with phase 3 of VM divided by the pressure recovery time. The pressure recovery time is defined as the interval between the lowest SBP of phase 3 of VM and its value after returning to baseline following the VM. BRS_v is expressed as the regression slope of heart period over SBP during early phase 2 of VM. The Valsalva ratio was calculated as the ratio between the highest HR reached in phase 2 and the lowest HR of phase 4 of VM.
Laboratory studies
All subjects underwent myocardial MIBG scintigraphy with a gamma camera no more than 6 months before study inclusion. We analyzed the early (15 min) and late (4 h) heart/mediastinum uptake ratios (H/M MIBG ratios). Patients also underwent 99mTc-MIBI SPECT to rule out myocardial perfusion defects.
Statistical analysis
Descriptive data were expressed using the mean and s.d. for the quantitative variables, and proportions for the qualitative variables. Normality and homogeneity of the variances were confirmed with the Kolmogorov-Smirnov and Levene’s tests, respectively. To examine the correlation between the late H/M MIBG ratio and other variables, Pearson’s correlation coefficients were calculated. Then, multiple stepwise regression analyses were performed to identify which variables were the strongest predictors of late H/M MIBG ratio in PD patients.
The SPSS-12 for Windows (SPSS, Chicago, IL, USA) package was used for the statistical analysis.
Results
The crude data and the results of the spectral analysis for the different outcome variables are reported in Tables 2 and 3. The E/I ratio, reflecting cardiovagal function, was found to be low. An overall increase in SBP and DBP (11.60±17.83 and 12.45±15.80 mm Hg, respectively) was observed 3 min after the TTT and the wide variability indicates that some patients could be considered ‘borderline’ with regard to NOH. The VM produced increases in blood pressure in phases IV and I, with the greatest reduction being observed in phase II while the recovery was in late phase II (Table 2).
Correlations between MIBG scintigraphy and clinical variables
The mean value of late (4 h) H/M MIBG uptake was 1.33±0.21 with a range of 1.07 to 1.75 (Table 1). Only three patients (15%) scored above 1.60, the threshold for normality in our hospital. MIBI scan detected no myocardial perfusion defects in any of the patients. The H/M MIBG ratio at 4 h was inversely correlated with time since diagnosis of the disease (correlation coefficient:−0.485; P=0.05) and with UPDRS III scores (cc:−0.564; P=0.02). No correlation was found between late H/M MIBG ratio and age or UPDRS I, II or IV scores.
Correlation between MIBG scintigraphy and quantitative autonomic tests
The values of the various hemodynamic parameters during the TTT, deep breathing and VM are reported in Table 2. No correlation was detected between changes in SBP and DBP after TTT and the late H/M MIBG ratio.
The late H/M MIBG ratio had a positive correlation with the E/I ratio in the deep breathing test, although the association did not reach statistical significance (0.43; P=0.06). In the case of the VM, we found positive significant correlations (P<0.001) between the late H/M MIBG ratio and the pressure recovery time (cc: 0.61; P<0.001), the BRS-cv (cc: 0.66; P<0.001), and the increases in blood pressure in phase IV (cc: 0.49; P<0.001).
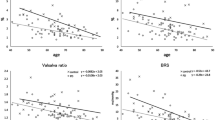
Correlation between MIBG scintigraphy and spectral analysis parameters
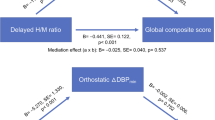
We studied the correlation between H/M MIBG ratio and hemodynamic parameters in the different studied settings (supine rest, deep breathing, VM, isometric contraction and TTT). At supine rest, a strong correlation was found with BRS (cc: 0.75; P=0.003) and low-frequency DBP variability (LF-dPA; cc: 0.58; P=0.017). LF-dPA and very low-frequency DBP variability (VLF-dPA) were both positively correlated with MIBG uptake ratios in all the different maneuvers: deep breathing: LF-dPA (cc: 0.56; P=0.015) and VLF-dPA (cc: 0.48; P=0.046); VM: LF-dPA (cc: 0.73; P=0.005) and VLF-dPA (cc: 0.58; P=0.038), isometric exercise: LF-dPA (cc: 0.52; P=0.021) and VLF-dPA (cc: 0.51; P=0.024); TTT: LF-dPA (cc: 0.58; P=0.007) and LF-dPA (cc: 0.52; P=0.017).
In summary, after stress tests, the only variables that correlated with the late H/M MIBG uptake ratio were LF-dPA and VLF-dPA, these being higher in the VM. At supine rest BRS showed a strong correlation with late H/M MIBG uptake ratio and LF-dPA was also correlated although with a lower intensity.
Relationship between late MIBG uptake ratio and cardiovascular parameters
No correlation was observed between the late H/M MIBG ratio and any of the impedance cardiography parameters considered (acceleration index, CO, LVWI, CI, SV, stroke index, left ventricular ejection time, TPR and thoracic fluid content). In addition, we did not find any correlation between the aforementioned parameters and chronotropic variables such as HR, maximum HR, or the spectral analysis of high frequency of RR interval variability (HF-RR). These correlation analyses included all the results from the different maneuvers (Table 3).
Regression analysis
All the correlated variables were included in a linear regression model using a stepwise procedure. The late H/M MIBG uptake ratio was the dependent variable and the model was adjusted for each setting: baseline, deep breathing, VM, isometric contraction and TTT independently. LF-dPA was found to appear in all the models, except for that for deep breathing (Table 4). The independent variables accounted for 60, 56, 53, 28 and 35% of the variance of late H/M MIBG ratio, respectively, in each of the settings. In addition, BRS (at rest), the E/I ratio and SV (deep breathing) contributed to the variance of the late H/M MIBG ratio (Table 4).
Discussion
In this study examining PD patients without NOH, we did not find a correlation between cardiac postganglionic sympathetic denervation (measured by MIBG scintigraphy and present in 85% of study subjects) and cardiac hemodynamic dysfunction (measured by a wide range of parameters obtained with continuous impedance cardiography in different hemodynamic settings). However, we found a positive correlation between cardiovagal function (as measured by E/I ratio) and cardiac postganglionic sympathetic denervation. These findings support that cardiac sympathetic and parasympathetic (cardiovagal) denervation occur somehow in parallel in PD. Furthermore, while in our study cardiac sympathetic denervation was common and increased with disease duration, it did not induce significant hemodynamic dysfunction. Thus, this suggests that cardiac sympathetic denervation by itself is not enough to induce the hemodynamic abnormalities of PD.
The influence of cardiac sympathetic denervation in the systemic hemodynamic misbalance of patients with PD is still not well understood. In heart-transplant recipients, one of the populations for which the hemodynamic consequences of cardiac sympathetic denervation are best described, this damage has been linked to impairment in chronotropic responsiveness and ventricular function. In addition, it has been found that in these patients sympathetic reinnervation is accompanied not only by an increase in the HR during exercise, but also by an increase in cardiac contractile function.22 In the case of PD, previous studies have reported signs of chronotropic incompetence15 in the premotor PD and a decrease in cardiac contractibility during ergometric exercise23 and during dobutamine stress echocardiography.24 In the latter studies, the authors only considered as measures of cardiac contractibility the initial acceleration of blood flow in the aorta (acceleration index), and the velocity index (peak velocity of blood in the aorta). In our study, in addition to acceleration index, we measured left ventricular ejection time and LVWI, which might be more accurate measures of cardiac contractility. Another explanation for the discordance with our results might reside in the stress methods used to induce hemodynamic responses. We believe that the motor status of patients with PD determines their capacity on ergometric exercise. Therefore, we avoided pharmacological or exercise maneuvers and we applied accepted and standardized maneuvers from Ewing and Clarke autonomic function test18 to induce sympathetic stress. Recently, Nakamura et al.25 have observed that under orthostatic stress, cardiac sympathetic denervation with failure to increase TPR leads to large reductions in systolic BP. Regarding the sequence of denervation, we did find a correlation between cardiac postganglionic sympathetic denervation as measured by late H/M MIBG ratio and the E/I ratio, a measure of cardiovagal function, suggesting that cardiac sympathetic and parasympathetic denervation occurred in parallel in these patients.26
Considering the lower prevalence of NOH compared to that of cardiac sympathetic denervation in early phases of PD, It seems likely that different compensation mechanisms prevent NOH until advanced stages of the disease. The main mechanism could be related with adrenergic denervation supersensitivity, as patients with cardiac denervation show exaggerated response to infused catecholamine in experimental studies.27 Other possible mechanism would be the greater decrease in norepinephrine clearance seen in PD patients.28 We previously published evidences supporting a selective vulnerability in the heart on the basis of normal catecholamine levels and the absence of orthostatic hypotension in symptomatic and asymptomatic carriers of genetic mutations of alpha-synuclein (SNCA) gene.12 However, in the present study we observed abnormal findings in the spectral analysis of the LF-dPA in the absence of NOH in patients with PD. This finding suggests an impaired sympathetic vascular regulation. It has been postulated that low-frequency RR variability may be useful for assessing cardiac sympathetic tone, however, recent studies have pointed to a role for this parameter in the analysis of baroreflex function.29
Previous studies have indicated progressive cardiac sympathetic denervation over the years in PD, suggesting a dying-back process,5, 6 which is the opposite to what is observed in cardiac reinnervation phenomena in transplanted patients.22 In the light of our findings, it seems this phenomenon may occur not only at the cardiac level, but also throughout the rest of the cardiovascular system.
The maneuvers for studying cardiac sympathetic function show that the correlation with BRS measured using the sequence method and the LFDBP is strongest at rest, suggesting that it could be sufficient to conduct such tests at rest to assess this function. In the case of the VM, the strongest correlation was found with pressure recovery time.30
The main weakness of our study was the small size of the sample (20 patients with idiopathic PD) and the potential impact of PD medications on autonomic tests. Seventy percent of patients were treated with dopamine agonists (Table 1); many of these drugs have long half-life in the blood and can cause signs and symptoms of dysautonomia. However, we believe that the homogeneity of the sample and the fact that they were PD patients without NOH, strengthens the validity of the study.
In summary, in our study performed in patients with PD without NOH, we did not find any correlation between the inotropic function of the heart measured by impedance cardiography and the degree of cardiac denervation measured using MIBG scintigraphy. However, the observation of a correlation between late H/M MIBG uptake ratio of the heart and LFDBP suggests that sympathetic denervation affects the heart and vascular systems simultaneously. It seems likely that different compensation mechanisms prevent NOH until advanced stages of the disease. Analysis of BRS and LFDBP at supine rest allows the level of sympathetic involvement to be predicted and quantified without requiring other maneuvers.

References
Kaufmann H, Goldstein DS . Autonomic dysfunction in Parkinson's disease. Handb Clin Neurol 2007; 83: 343–363.
Velseboer DC, de Haan RJ, Wieling W, Goldstein DS, de Bie RM . Prevalence of orthostatic hypotension in Parkinson's disease: a systematic review and meta-analysis. Parkinsonism Relat Disord 2011; 17 (10): 724–729.
Orimo S, Uchihara T, Nakamura A, Mori F, Kakita A, Wakabayashi K et al. Axonal alpha-synuclein aggregates herald centripetal degeneration of cardiac sympathetic nerve in Parkinson's disease. Brain 2008; 131 (Pt 3): 642–650.
Goldstein DS . Dysautonomia in Parkinson's disease: neurocardiological abnormalities. Lancet Neurol 2003; 2 (11): 669–676.
Li ST, Dendi R, Holmes C, Goldstein DS . Progressive loss of cardiac sympathetic innervation in Parkinson's disease. Ann Neurol 2002; 52 (2): 220–223.
Goldstein DS, Holmes C, Li ST, Bruce S, Metman LV, Cannon RO 3rd . Cardiac sympathetic denervation in Parkinson disease. Ann Intern Med 2000; 133 (5): 338–347.
Orimo S, Ozawa E, Nakade S, Sugimoto T, Mizusawa H . 123I-metaiodobenzylguanidine myocardial scintigraphy in Parkinson's disease. J Neurol Neurosurg Psychiatry 1999; 67 (2): 189–194.
Goldstein DS . Cardiac denervation in patients with Parkinson disease. Cleve Clin J Med 2007; 74 (Suppl 1): S91–S94.
Haensch CA, Lerch H, Jorg J, Isenmann S . Cardiac denervation occurs independent of orthostatic hypotension and impaired heart rate variability in Parkinson's disease. Parkinsonism Relat Disord 2009; 15 (2): 134–137.
Kaufmann H, Nahm K, Purohit D, Wolfe D . Autonomic failure as the initial presentation of Parkinson disease and dementia with Lewy bodies. Neurology 2004; 63 (6): 1093–1095.
Tijero B, Gomez-Esteban JC, Llorens V, Lezcano E, Gonzalez-Fernandez MC, de Pancorbo MM et al. Cardiac sympathetic denervation precedes nigrostriatal loss in the E46K mutation of the alpha-synuclein gene (SNCA). Clin Auton Res 2010; 20 (4): 267–269.
Tijero B, Gomez-Esteban JC, Lezcano E, Fernandez-Gonzalez C, Somme J, Llorens V et al. Cardiac sympathetic denervation in symptomatic and asymptomatic carriers of the E46K mutation in the alpha synuclein gene. Parkinsonism Relat Disord 2013; 19 (1): 95–100.
Goldstein DS . Cardiovascular aspects of Parkinson disease. J Neural Transm Suppl 2006; 70: 339–342.
Berganzo K, Tijero B, Somme JH, Llorens V, Sanchez-Manso JC, Low D et al. SCOPA-AUT scale in different parkinsonisms and its correlation with (123) I-MIBG cardiac scintigraphy. Parkinsonism Relat Disord 2012; 18 (1): 45–48.
Palma JA, Carmona-Abellan MM, Barriobero N, Trevino-Peinado C, Garcia-Lopez M, Fernandez-Jarne E et al. Is cardiac function impaired in premotor Parkinson's disease? A retrospective cohort study. Mov Disord 2013; 28 (5): 591–596.
Hughes AJ, Daniel SE, Kilford L, Lees AJ . Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992; 55 (3): 181–184.
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 2011; 21 (2): 69–72.
Ewing DJ, Clarke BF . Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed) 1982; 285 (6346): 916–918.
Gratze G, Mayer H, Luft FC, Skrabal F . Determinants of fast marathon performance: low basal sympathetic drive, enhanced postcompetition vasodilatation and preserved cardiac performance after competition. Br J Sports Med 2008; 42 (11): 882–888.
Gratze G, Rudnicki R, Urban W, Mayer H, Schlogl A, Skrabal F . Hemodynamic and autonomic changes induced by Ironman: prediction of competition time by blood pressure variability. J Appl Physiol 2005; 99 (5): 1728–1735.
Steptoe A, Vogele C . Cardiac baroreflex function during postural change assessed using non-invasive spontaneous sequence analysis in young men. Cardiovasc Res 1990; 24 (8): 627–632.
Bengel FM, Ueberfuhr P, Schiepel N, Nekolla SG, Reichart B, Schwaiger M . Effect of sympathetic reinnervation on cardiac performance after heart transplantation. N Engl J Med 2001; 345 (10): 731–738.
Nakamura T, Hirayama M, Yamashita F, Uchida K, Hama T, Watanabe H et al. Lowered cardiac sympathetic nerve performance in response to exercise in Parkinson's disease. Mov Disord 2010; 25 (9): 1183–1189.
Nakamura T, Hirayama M, Ito H, Takamori M, Hamada K, Takeuchi S et al. Dobutamine stress test unmasks cardiac sympathetic denervation in Parkinson's disease. J Neurol Sci 2007; 263 (1-2): 133–138.
Nakamura T, Hirayama M, Hara T, Mizutani Y, Suzuki J, Watanabe H et al. Role of cardiac sympathetic nerves in preventing orthostatic hypotension in Parkinson's disease. Parkinsonism Relat Disord 2014; 20: 409–414.
Shibata M, Morita Y, Shimizu T, Takahashi K, Suzuki N . Cardiac parasympathetic dysfunction concurrent with cardiac sympathetic denervation in Parkinson's disease. J Neurol Sci 2009; 276 (1-2): 79–83.
Imrich R, Eldadah BA, Bentho O, Pechnik S, Sharabi Y, Holmes C et al. Functional effects of cardiac sympathetic denervation in neurogenic orthostatic hypotension. Parkinsonism Relat Disord 2009; 15 (2): 122–127.
Jacob G, Shannon JR, Costa F, Furlan R, Biaggioni I, Mosqueda-Garcia R et al. Abnormal norepinephrine clearance and adrenergic receptor sensitivity in idiopathic orthostatic intolerance. Circulation 1999; 99 (13): 1706–1712.
Rahman F, Pechnik S, Gross D, Sewell L, Goldstein DS . Low frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Clin Auton Res 2011; 21 (3): 133–141.
Vogel ER, Sandroni P, Low PA . Blood pressure recovery from Valsalva maneuver in patients with autonomic failure. Neurology 2005; 65 (10): 1533–1537.
Acknowledgements
This study was funded by the Health Department of the Basque Government (dossier 2009111093), the Spanish Health Research Fund (Fondo de Investigación Sanitaria, FIS, PS09/01916), and the Department of Industry of the Basque Government (SAIOTEK, ref: S-PC09BF02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pérez, T., Tijero, B., Gabilondo, I. et al. Cardiocirculatory manifestations in Parkinson's disease patients without orthostatic hypotension. J Hum Hypertens 29, 604–609 (2015). https://doi.org/10.1038/jhh.2014.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2014.131
- Springer Nature Limited
This article is cited by
-
Optimal Protocol and Clinical Usefulness of 123I-MIBG Cardiac Scintigraphy for Differentiation of Parkinson’s Disease and Dementia with Lewy Body from Non-Parkinson’s Diseases
Nuclear Medicine and Molecular Imaging (2023)
-
Automatic detection of the mental state in responses towards relaxation
Neural Computing and Applications (2023)
-
The Effect of Skeletal Muscle-Pump on Blood Pressure and Postural Control in Parkinson's Disease
Cardiovascular Engineering and Technology (2023)
-
Heart-brain synchronization breakdown in Parkinson’s disease
npj Parkinson's Disease (2022)
-
Autonomic dysfunction is associated with neuropsychological impairment in Lewy body disease
Journal of Neurology (2020)