Abstract
Background/Objectives:
OxLDL–β2GPI complex has been suggested to have a role in the development of atherosclerosis and other inflammatory diseases. The aim of this study was to investigate the possible association of circulating oxLDL–β2GPI with obesity-induced inflammatory state of adipose tissue and related comorbidities as metabolic syndrome development.
Subjects/Methods:
Two cohorts of subjects were examined in the study. Cohort I: 36 women with wide range of body mass index (17–48 kg m−2) and metabolic status (with or without metabolic syndrome (MS); cohort II: 20 obese women undergoing a dietary intervention (DI) consisting of 1-month very-low-calorie diet, and 5 months of weight-stabilization period. Serum levels of oxLDL–β2GPI were measured by enzyme-linked immunosorbent assay. Insulin sensitivity was evaluated by hyperinsulinemic-euglycemic clamp and homeostasis model assessment of insulin resistance. mRNA expression of macrophage markers was determined in both subcutaneous (SAT) and visceral (VAT) adipose tissue in cohort I and in SAT in cohort II.
Results:
Serum oxLDL–β2GPI levels were increased in obese subjects with MS compared to lean or obese without MS (obese with MS: 26.6±5.0 vs lean: 15.17±1.97, P<0.001; vs obese without MS: 16.36±2.89, P<0.05). Serum oxLDL–β2GPI correlated with MS indices (glucose, high-density lipoprotein, triglyceride and ureic acid) and with mRNA expression of macrophage markers in VAT. Weight-reducing DI decreased serum oxLDL–β2GPI levels together with lipid parameters and the mRNA expression of inflammatory markers in SAT.
Conclusions:
OxLDL–β2GPI seems to be an important marker of visceral adipose tissue inflammation and possibly a factor contributing to insulin resistance and metabolic syndrome development in obese patients.
Similar content being viewed by others
Introduction
Chronic low inflammation is believed to have a key role in the pathogenesis of insulin resistance syndrome with all its components—hyperinsulinemia, hyperglycemia, dyslipidemia, abdominal obesity, hypertension, prothrombotic state and development of type 2 diabetes mellitus.1, 2
It has been demonstrated that insulin resistance is closely associated with plasma concentrations of oxidized low-density lipoproteins (oxLDL), which not only serve as a biomarker of oxidative stress but also have a key role in the pathogenesis of atherosclerosis.3 Small dense LDL particles (LDL subclass B) are associated with hypertriglyceridemia and low high-density lipoprotein (HDL)-cholesterol in obese individuals and diabetic patients, and are more prone to oxidative modification than the larger LDL particles (subclass A).4 Besides insulin resistance and diabetes, increased levels of oxLDL were observed in autoimmune inflammatory diseases, chronic infection, chronic renal failure or elevated iron levels.5, 6, 7, 8 Through its cytotoxic effects, oxLDL cause endothelial dysfunction and consequently promote recruitment of macrophages and T lymphocytes to the site of the atherosclerotic lesion.9 Within the subendothelial space of the arterial intima, oxLDL is readily taken up by macrophages via scavenger receptors resulting in foam-cell formation.10 In addition, oxLDL form complexes with β2-glycoprotein I (β2GPI), a member of the plasma complement control protein superfamily.11 In atherosclerotic lesions, β2GPI co-localizes with macrophage-derived foam cells and activated smooth muscle cells.12 Moreover, both oxLDL and β2GPI were found in co-localization with lymphocytes and immunoglobulins within atherosclerotic plaque.13 Greco et al.14 documented significant correlation of serum oxLDL–β2GPI with the severity and outcomes of coronary heart disease in patients with acute coronary syndrome. Other studies have demonstrated association of the oxLDL–β2GPI complex with chronic autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, antiphospholipid syndrome or systemic sclerosis, as well as chronic renal disease and diabetes mellitus.15, 16 In our previous study, we demonstrated that healthy men with abdominal obesity had significantly higher plasma concentration of oxLDL–β2GPI than non-obese subjects. Moreover, in that study plasma oxLDL–β2GPI were associated with markers of insulin resistance.17 This finding implies that oxLDL–β2GPI may have a role in a systemic inflammatory state associated with adipose tissue inflammation, which probably contributes to insulin resistance development. Thus, the aim of the present study was to elucidate possible relation between oxLDL–β2GPI and markers of adipose tissue inflammation in a cohort of women with a wide range of body mass index (BMI) and different metabolic profile (presence/absence of metabolic syndrome). Crucial role in the development of insulin resistance and obesity-associated inflammatory state is traditionally attributed to the visceral adipose tissue,18, 19, 20 therefore we analyzed the expression of inflammatory markers in both visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) in our cross-sectional study. Moreover, we aimed to elucidate whether 6 months of weight-reducing dietary intervention (DI) could alter the serum oxLDL–β2GPI concentrations.
Materials and methods
Subjects
Two cohorts of Caucasian women participated in the study.
Cohort I
Thirty-six women with a wide range of BMI (age 27–63 years, BMI 17.3–48.5 kg m−2) scheduled to have abdominal surgery (laparoscopic cholecystectomy, hysterectomy or gastric banding) were included in the study. Exclusion criteria were as follows: malignancy; congestive heart failure; chronic liver or kidney disease; psychiatric disorders; and body weight fluctuations >3 kg over the preceding 3 months. According to BMI and to presence or absence of the metabolic syndrome (evaluated according to the International Diabetes Federation criteria,21) 36 participants were stratified into 3 groups: lean (LE; n=12 subjects), obese (OB; n=12) and obese with metabolic syndrome (OB/MS; n=12).
Cohort II
This cohort consisted of 20 obese premenopausal women (age 40±2 years; BMI 33.5±0.6 kg m−2). Exclusion criteria were as follows: malignancy; hypertension; diabetes; hyperlipidemia treated by drugs; weight change of >3 kg within the 3 months before the study; drug-treated obesity; pregnancy; participation in other trials; and alcohol or drug abuse.
Written informed consent was obtained from all subjects in the study. The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the ethical committee of the Third Faculty of Medicine of Charles University in Prague, Czech Republic.
Study design
Study I (cohort I)
Clinical investigation was realized 7–14 days before the surgery. Anthropometric measurements, blood sampling and euglycemic-hyperinsulinemic clamp were performed at rest after an overnight fast. Body composition was evaluated using bioelectrical impedance (QuadScan 4000, Bodystat Ltd., Douglas, Isle of Man, UK). Visceral and subcutaneous fat areas were assessed using computed tomography scans at the level L4–5.22 Blood samples were obtained before the clamp and plasma parameters were measured, using standard procedures. Insulin sensitivity was assessed using euglycemic-hyperinsulinemic clamp according to De Fronzo et al.23 During the surgical procedure, paired samples of subcutaneous (SAT) and omental visceral adipose tissue (VAT) were obtained and processed immediately. Adipose tissue (AT) was washed in physiological saline, homogenized in RLT lysis buffer (Qiagen, Hilden, Germany) and stored at −80 °C until total RNA extraction.
Study II (cohort II)
Participants underwent DI consisting of a 1-month very-low-calorie diet (800 kcal per day, liquid formula Redita; Promil, Nový Bydžov, Czech Republic) and of a subsequent weight-stabilization phase. The latter consisted in 2 months’ low-calorie diet (600 kcal per day less than the estimated energy requirement) followed by 3 months’ weight maintenance phase. Patients consulted a dietitian once a week during energy restriction (very-low-calorie diet and low-calorie diet) and once a month during the weight maintenance phase. They provided a written 3-day dietary record at each dietary consultation during the weight stabilization phase.
Clinical investigation, anthropometric measurements and blood sampling were performed in the morning at fasting state at baseline (before the DI) and at the end of whole DI. Needle biopsy of SAT was performed under local anesthesia (1% xylocaine; AstraZeneca PLC, London, UK) from the abdominal region (14–20 cm lateral to the umbilicus).24 Analysis of insulin sensitivity was performed by the euglycemic-hyperinsulinemic clamp according to the De Fronzo method. Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as ‘fasting blood glucose (mmol l−1) × fasting insulin (mU l−1)/22.5’.
Blood analysis
Plasma concentrations of glucose, insulin, lipids and high-sensitivity C-reactive protein were determined using standard biochemical methods. Serum concentration of oxLDL–β2GPI was determined by ELISA AtherOx Test kit (Corgenix, Inc., Broomfield, CO, USA). The inter-assay precision of the current assay was 2.75±1.8%, the limit of detection was 0.06 ng ml−1. Serum concentrations of tumor necrosis factor alpha (TNFα) and monocyte chemoattractant protein-1 (MCP-1) were determined using high-sensitivity Quantikine (TNFα) and Quantikine (MCP-1) ELISA kits (R&D Systems, Minneapolis, MN, USA).
Quantitative real time-PCR
Total RNA isolation was performed as previously described.24 Genomic DNA was removed by DNAse I treatment (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA). cDNA was obtained by reverse transcription (High Capacity cDNA Reverse Transcription Kit, Applied Biosystems, Carlsbad, CA, USA). Macrophage-specific markers were chosen from a panel of genes that were identified in our previous study using a combination of DNA microarray technology and immunosorting of cells residing in AT.25 The highly specific genes for adipose tissue resident CD34−/CD14+ macrophages (namely CD14, CD68, CD163, IRF5, KYNU, MSR1, LIPA and ACP5) were selected according to the following criteria: (1) gene expression more than 10- and 2-fold higher in macrophages than in adipocytes and other non-adipocyte cell types, respectively; (2) more than 1.5-fold higher expression in macrophages than in stroma-vascular fraction; and (3) high inter-correlations of SAT and VAT gene expression. Moreover, the gene expression of inflammatory cytokines (TNFα, interleukin (IL)-6, IL-8 and MCP-1), and the genes/macrophage markers, which have been associated with metabolic or cardiovascular diseases (PLA2G7(ref. 26) and SPP1(ref. 27)) and/or oxLDL–β2GPI binding (FCGBP) was determined. The mRNA expression was assessed by real-time quantitative PCR on ABI PRISM 7900 or 7500 sequence detection system using Custom TaqMan Low Density Arrays or TaqMan Gene Expression Assay (Applied Biosystems). Level of expression of target genes was normalized to GUSB and fold change of expression was calculated using ΔΔCt method.
Statistical analysis
Study I
To compare plasma and mRNA levels between the three groups of subjects, the data were analyzed by univariate regression analysis with adjustment for age, followed by Bonferroni post hoc analysis (SPSS 12.0 for Windows, SPSS Inc., Chicago, IL, USA, and GraphPad Prism version 6.00 for Windows, La Jolla, CA, USA). Correlations between the respective variables were assessed using the Pearson’s parametric test.
Study II
To evaluate the diet-induced evolution of clinical variables and plasma and mRNA levels, data were analyzed using paired T-test. Correlations between the diet-induced relative changes of respective variables were assessed using the Pearson’s parametric test (GraphPad Software).
The sample size for both studies was chosen according to power analysis (GPower 3.1, Dusseldorf, Germany), pre-specified effect size was evaluated according to previous data.17 Data were expressed as means±s.e.m., P<0.05 was considered statistically significant.
Results
Study I: cross-sectional
Clinical and metabolic characteristics of the three groups of subjects (LE, OB and OB/MS) are shown in Table 1. OB and OB/MS group was similar in weight, BMI, fat mass and fat-free mass. OB/MS subjects had higher visceral fat in total fat volume, increased ureic acid, triglycerides and glucose levels, and lower HDL-cholesterol levels, all of these parameters are associated with MS diagnostics/appearance.21, 28 Insulin sensitivity assessed as metabolic clearance of glucose was lower in both, OB and OB/MS, when compared with the LE group and not different between OB and OB/MS groups. Serum levels of oxLDL–β2GPI were higher in OB/MS than in LE and OB groups (Table 1). Serum levels of TNFα, MCP-1 and high-sensitivity C-reactive protein were not different among the groups (Table 1).
Correlations
Circulating oxLDL–β2GPI levels correlated with most of the variables associated with the metabolic syndrome, that is, positive correlation with blood glucose, triglycerides and uric acid, and inverse correlation with HDL-cholesterol and metabolic clearance of glucose (Table 2). A trend to correlate with the amount of visceral fat related to subcutaneous fat was observed (visceral fat/subcutaneous fat; Table 2).
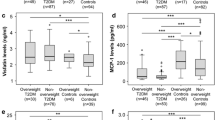
Moreover, oxLDL–β2GPI levels correlated positively with the mRNA expression of number of macrophage markers in VAT, namely TNFα, MSR1, PLA2G7, ACP5, FCGBP, KYNU, LIPA and SPP1 (Figure 1, Supplementary Table 1). The correlations of mRNA expression of these markers with oxLDL–β2GPI in SAT were not significant (or had borderline significance), except for TNFα.
Study II: DI
Clinical and metabolic characteristics of subjects in cohort II before and after DI are summarized in Table 3. The body weight was lower by 16.9% at the end of DI when compared with baseline. HOMA-IR was lower, when compared with the pre-diet baseline value, at the end of DI, while metabolic clearance of glucose was higher than baseline values at the end of diet.
Weight-reducing DI induced a decrease of oxLDL–β2GPI serum levels. mRNA levels of several macrophage markers in SAT, namely MSR1, PLA2G7, ACP5, FCGBP and IRF5 were markedly reduced at the end of DI as well (Figure 2). mRNA expression of TNFα in SAT was not changed during the DI (Figure 2).
Correlations
Baseline values and the diet-induced changes of circulating oxLDL–β2GPI correlated positively with corresponding values and changes of BMI, triglycerides and cholesterol (Supplementary Figure 1).
Discussion
Our study was focused on oxLDL–β2GPI as a possible marker of both oxidative stress and the inflammatory process in the adipose tissue contributing to the development of obesity-related comorbidities as insulin resistance and metabolic syndrome.
In the cross-sectional study, the plasma concentrations of oxLDL–β2GPI did not statistically differ between the lean and obese subjects, however the levels were almost doubled in the obese women with metabolic syndrome compared to the lean individuals or obese group without MS. There may be discrepancy with our previous study, where oxLDL–β2GPI was increased in group of obese men compared to lean.17 However, the possible gender differences should be taken into account. Further, the group of obese men was not divided according to presence of metabolic syndrome components. Thus, the group was probably mixed in this respect. Moreover, the higher visceral fat thickness was present in obese men in previous study, similarly as increased visceral fat area in the group of women with MS in present study. In univariate regression analysis, oxLDL–β2GPI complex showed correlation with waist-to-hip ratio and general parameters of metabolic syndrome and insulin resistance (positive corr. with glucose and triglycerides; inverse corr. with HDL-cholesterol and metabolic clearance of glucose). Positive correlation with circulating ureic acid, a new marker of MS,28 was also found. These findings imply that increase of circulating oxLDL–β2GPI becomes significant especially when insulin resistance and metabolic syndrome is developed.
oxLDL–β2GPI complex was associated with arterial and venous disease, atherosclerosis and other inflammatory diseases.15, 16, 29 However, its role in obesity-derived inflammation was not yet elucidated. In obesity, pro-inflammatory environment within the white adipose tissue develops and is expressed by increased accumulation of adipose tissue macrophages, a switch from anti-inflammatory M2 to pro-inflammatory M1 phenotype of macrophages, and increased secretion of pro-inflammatory cytokines (such as TNF-α, IL-1β and IL-6).30 The inflammatory state in AT is associated with the development of insulin resistance also on systemic level. Increased secretion of TNF-α and other inflammatory cytokines, higher influx of free fatty acids due to upregulated lipolysis in AT together with increased oxidative stress have inhibitory effect on insulin responsive substance thereby inhibiting insulin downstream signaling.31 In this study, oxLDL–β2GPI levels correlated positively with the mRNA expression of several macrophage markers in VAT and with the expression of pro-inflammatory cytokine TNFα in both VAT and SAT. This is in line with the study of Zhang et al.32 showing that the in vitro treatment of peritoneal mice macrophages with oxLDL–β2GPI complexed with anti-β2GPI antibody increased activity of nuclear factor κB (NFκB) and enhanced secretion of TNFα and MCP-1, while all these processes were reduced in macrophages isolated from TLR4-KO mice. Thus, it has been suggested that oxLDL–β2GPI/anti-β2GPI stimulates expression of TNFα and other pro-inflammatory cytokines via activation of TLR4 receptors and NFκB pathway. Activated NFκB regulates the expression of genes involved in inflammation and immune processes in response to oxidative stress.33 In fact, oxidative stress and inflammation are closely related processes and one can be induced by the other. Inflammatory cells produce reactive species, on the other hand reactive oxygen and nitrogen species can serve as signaling molecules enhancing pro-inflammatory gene expression in tissues.34, 35 Thus, it might be suggested that the oxidative stress and inflammatory state in obese adipose tissue might be partially triggered by the oxLDL–β2GPI in association with TNFα expression. Interestingly, the correlation of oxLDL–β2GPI with circulating cytokines (TNFα and MCP-1) was not found in this study, which suggests that the levels of oxLDL–β2GPI do not reflect systemic inflammation in obese women, but are linked specifically with adipose tissue inflammation.
The oxLDL particles seem to be highly immunogenic and its immunogenicity is enhanced when bound to β2GPI in stable complex. The oxLDL–β2GPI itself may activate mechanisms of both adaptive and innate immunity in autoimmune-mediated and also non-autoimmune atherothrombotic diseases.36 As proposed by Kajiwara et al.,12 oxLDL–β2GPI form immune complexes with IgG autoantibodies that can be subsequently absorbed by macrophages through FcγRI-mediated phagocytosis and presented to autoreactive CD4+ T lymphocytes via major histocompatibility complex class II molecules.37 Moreover, it has been demonstrated that immune complexes of oxLDL–β2GPI with IgG antibody upregulate the expression of scavenger and FcγRI receptors in macrophages and also contribute to the activation of inflammasome resulting in maturation of IL-1 family cytokines, namely IL-1β.36 It could be hypothesized that the effects of oxLDL–β2GPI on macrophage activation observed in autoimmune atherothrombotic diseases might be present also in metabolic syndrome. In accordance, we have found a strong positive correlation between oxLDL–β2GPI and FCGBP—Fc fragment of IgG-binding protein—expression in visceral adipose tissue. Interestingly, the significant correlation between oxLDL–β2GPI and the mRNA expression of several other macrophage markers was observed in visceral adipose tissue, but not (or only in tendency) in SAT. Indeed, inflammation of visceral AT seems to have a crucial role in insulin resistance development. It has been demonstrated that macrophages preferentially accumulate and proliferate in VAT of obese mice.38 In a human study, it was documented that the presence of pro-inflammatory M1 macrophages is almost twice as high in visceral and perivascular tissue than in SAT.39 Considering our findings it might be suggested that the circulating levels of oxLDL–β2GPI reflect the adipose tissue inflammation mainly in the visceral area. In addition, oxLDL–β2GPI may further perpetuate the inflammatory state through Fc fragment of IgG and TNFα, as mentioned above.
The results from the intervention study demonstrate that weight-reducing diet associated with improvement of dyslipidemia (decrease of triglycerides increase of HDL) and insulin resistance (HOMA-IR) resulted in a significant decrease of plasma oxLDL–β2GPI as well as mRNA expression of certain markers of macrophage activation in SAT. The decrease of macrophage markers is in agreement with the previously published studies of our and others, where the decrease in macrophage populations,40 or T lymphocytes41 in SAT after weight-reducing DIs was shown. Interestingly, we did not observe any change in TNFα expression during the diet, which suggests another mechanism in inflammatory state lowering than via TNFα signaling.
It should be mentioned that the DI study evaluated only changes in SAT but not in VAT. It was not possible to obtain specimen of VAT due to major invasiveness of such procedure in our volunteers who were not undergoing abdominal surgery. We may however expect similar response in macrophage markers after dietary weight-reducing intervention in VAT as well, since similar pattern in macrophage markers/inflammatory state expression in SAT and VAT has already been described.42 This assumption is also supported by the fact that the relative decrease of VAT volume after weight loss induced by DI, exercise or bariatric surgery is greater than the relative decrease of SAT,19 and thus it might be hypothesized that the effects of reduction of AT volume in visceral area on inflammatory markers could be even more striking.
Although in the cross-sectional study we observed markedly increased oxLDL–β2GPI levels only in subjects with MS, after weight loss the slight but significant decrease of oxLDL–β2GPI complex was achieved also in obese women. It should be noted that oxLDL–β2GPI correlated in both cohorts mainly with lipid parameters, which was also importantly improved after weight-reducing DI (Table 3). In addition, there may be a direct impact of both physical activity and dietary factors on oxidative stress and inflammation.43, 44
In conclusion, in this study we documented that circulating oxLDL–β2GPI reflects inflammatory status of visceral adipose tissue in obese subjects and correlates with metabolic syndrome indices. The improvement of metabolic and inflammatory parameters during weight loss was reflected by decreased levels of oxLDL–β2GPI in serum. Thus, oxLDL–β2GPI seems to be an important marker of AT inflammatory state and possibly a factor contributing to obesity-related comorbidities as metabolic syndrome or cardiovascular diseases.
References
Daniele G, Guardado Mendoza R, Winnier D, Fiorentino TV, Pengou Z, Cornell J et al. The inflammatory status score including IL-6, TNF-alpha, osteopontin, fractalkine, MCP-1 and adiponectin underlies whole-body insulin resistance and hyperglycemia in type 2 diabetes mellitus. Acta Diabetol 2014; 51: 123–131.
Osborn O, Olefsky JM . The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med 2012; 18: 363–374.
Holvoet P, Mertens A, Verhamme P, Bogaerts K, Beyens G, Verhaeghe R et al. Circulating oxidized LDL is a useful marker for identifying patients with coronary artery disease. Arterioscler Thromb Vasc Biol 2001; 21: 844–848.
Sanchez-Quesada JL, Vinagre I, De Juan-Franco E, Sanchez-Hernandez J, Bonet-Marques R, Blanco-Vaca F et al. Impact of the LDL subfraction phenotype on Lp-PLA2 distribution, LDL modification and HDL composition in type 2 diabetes. Cardiovasc Diabetol 2013; 12: 112.
Aranda N, Fernandez-Cao JC, Tous M, Arija V . Increased iron levels and lipid peroxidation in a Mediterranean population of Spain. Eur J Clin Invest 2016; 46: 520–526.
Frostegard J . Autoimmunity, oxidized LDL and cardiovascular disease. Autoimmun Rev 2002; 1: 233–237.
Liu J, Rosner MH . Lipid abnormalities associated with end-stage renal disease. Semin Dial 2006; 19: 32–40.
Mayr M, Kiechl S, Tsimikas S, Miller E, Sheldon J, Willeit J et al. Oxidized low-density lipoprotein autoantibodies, chronic infections, and carotid atherosclerosis in a population-based study. J Am Coll Cardiol 2006; 47: 2436–2443.
Frostegard J, Haegerstrand A, Gidlund M, Nilsson J . Biologically modified LDL increases the adhesive properties of endothelial cells. Atherosclerosis 1991; 90: 119–126.
Boullier A, Bird DA, Chang MK, Dennis EA, Friedman P, Gillotre-Taylor K et al. Scavenger receptors, oxidized LDL, and atherosclerosis. Ann N Y Acad Sci 2001; 947: 214–222 discussion 222-223.
Hasunuma Y, Matsuura E, Makita Z, Katahira T, Nishi S, Koike T . Involvement of beta 2-glycoprotein I and anticardiolipin antibodies in oxidatively modified low-density lipoprotein uptake by macrophages. Clin Exp Immunol 1997; 107: 569–573.
Kajiwara T, Yasuda T, Matsuura E . Intracellular trafficking of beta2-glycoprotein I complexes with lipid vesicles in macrophages: implications on the development of antiphospholipid syndrome. J Autoimmun 2007; 29: 164–173.
George J, Harats D, Gilburd B, Afek A, Levy Y, Schneiderman J et al. Immunolocalization of beta2-glycoprotein I (apolipoprotein H) to human atherosclerotic plaques: potential implications for lesion progression. Circulation 1999; 99: 2227–2230.
Greco TP, Conti-Kelly AM, Anthony JR, Greco Jr T, Doyle R, Boisen M et al. Oxidized-LDL/beta(2)-glycoprotein I complexes are associated with disease severity and increased risk for adverse outcomes in patients with acute coronary syndromes. Am J Clin Pathol 2010; 133: 737–743.
Lopez LR, Hurley BL, Simpson DF, Matsuura E . Oxidized low-density lipoprotein/beta2-glycoprotein I complexes and autoantibodies in patients with type 2 diabetes mellitus. Ann N Y Acad Sci 2005; 1051: 97–103.
Lopez LR, Simpson DF, Hurley BL, Matsuura E . OxLDL/beta2GPI complexes and autoantibodies in patients with systemic lupus erythematosus, systemic sclerosis, and antiphospholipid syndrome: pathogenic implications for vascular involvement. Ann N Y Acad Sci 2005; 1051: 313–322.
Kraml PJ, Syrovatka P, Potockova J, Andel M . The oxidized low-density lipoprotein/beta2-glycoprotein I complex is associated with abdominal obesity in healthy middle-aged men. Ann Nutr Metab 2013; 62: 7–13.
Arner P . Not all fat is alike. Lancet 1998; 351: 1301–1302.
Merlotti C, Ceriani V, Morabito A, Pontiroli AE . Subcutaneous fat loss is greater than visceral fat loss with diet and exercise, weight-loss promoting drugs and bariatric surgery: a critical review and meta-analysis. Int J Obes (Lond) 2017; 41: 672–682.
Montague CT, O'Rahilly S . The perils of portliness: causes and consequences of visceral adiposity. Diabetes 2000; 49: 883–888.
Alberti KG, Zimmet P, Shaw J, Group IDFETFC. The metabolic syndrome—a new worldwide definition. Lancet 2005; 366: 1059–1062.
Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S . Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987; 36: 54–59.
DeFronzo RA, Tobin JD, Andres R . Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 1979; 237: E214–E223.
Rossmeislova L, Malisova L, Kracmerova J, Tencerova M, Kovacova Z, Koc M et al. Weight loss improves the adipogenic capacity of human preadipocytes and modulates their secretory profile. Diabetes 2013; 62: 1990–1995.
Klimcakova E, Roussel B, Kovacova Z, Kovacikova M, Siklova-Vitkova M, Combes M et al. Macrophage gene expression is related to obesity and the metabolic syndrome in human subcutaneous fat as well as in visceral fat. Diabetologia 2011; 54: 876–887.
Garg PK, McClelland RL, Jenny NS, Criqui MH, Greenland P, Rosenson RS et al. Lipoprotein-associated phospholipase A2 and risk of incident cardiovascular disease in a multi-ethnic cohort: the multi ethnic study of atherosclerosis. Atherosclerosis 2015; 241: 176–182.
Liu J, Ren Y, Kang L, Zhang L . Oxidized low-density lipoprotein increases the proliferation and migration of human coronary artery smooth muscle cells through the upregulation of osteopontin. Int J Mol Med 2014; 33: 1341–1347.
Mangge H, Zelzer S, Puerstner P, Schnedl WJ, Reeves G, Postolache TT et al. Uric acid best predicts metabolically unhealthy obesity with increased cardiovascular risk in youth and adults. Obesity (Silver Spring) 2013; 21: E71–E77.
Berger JS, Rockman CB, Guyer KE, Lopez LR . Proatherogenic oxidized low-density lipoprotein/beta2-glycoprotein I complexes in arterial and venous disease. J Immunol Res 2014; 2014: 234316.
Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N . Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 2014; 105: 141–150.
Boden G . Fatty acid-induced inflammation and insulin resistance in skeletal muscle and liver. Curr Diab Rep 2006; 6: 177–181.
Zhang X, Xie Y, Zhou H, Xu Y, Liu J, Xie H et al. Involvement of TLR4 in oxidized LDL/beta2GPI/anti-beta2GPI-induced transformation of macrophages to foam cells. J Atheroscler Thromb 2014; 21: 1140–1151.
Sies H, Berndt C, Jones DP . Oxidative stress. Annu Rev Biochem 2017; 86: 715–748.
Anderson MT, Staal FJ, Gitler C, Herzenberg LA, Herzenberg LA . Separation of oxidant-initiated and redox-regulated steps in the NF-kappa B signal transduction pathway. Proc Natl Acad Sci USA 1994; 91: 11527–11531.
Flohe L, Brigelius-Flohe R, Saliou C, Traber MG, Packer L . Redox regulation of NF-kappa B activation. Free Radic Biol Med 1997; 22: 1115–1126.
Matsuura E, Lopez LR, Shoenfeld Y, Ames PR . beta2-glycoprotein I and oxidative inflammation in early atherogenesis: a progression from innate to adaptive immunity? Autoimmun Rev 2012; 12: 241–249.
Kuwana M, Matsuura E, Kobayashi K, Okazaki Y, Kaburaki J, Ikeda Y et al. Binding of beta 2-glycoprotein I to anionic phospholipids facilitates processing and presentation of a cryptic epitope that activates pathogenic autoreactive T cells. Blood 2005; 105: 1552–1557.
Amano SU, Cohen JL, Vangala P, Tencerova M, Nicoloro SM, Yawe JC et al. Local proliferation of macrophages contributes to obesity-associated adipose tissue inflammation. Cell Metab 2014; 19: 162–171.
Kralova Lesna I, Kralova A, Cejkova S, Fronek J, Petras M, Sekerkova A et al. Characterisation and comparison of adipose tissue macrophages from human subcutaneous, visceral and perivascular adipose tissue. J Transl Med 2016; 14: 208.
Kovacikova M, Sengenes C, Kovacova Z, Siklova-Vitkova M, Klimcakova E, Polak J et al. Dietary intervention-induced weight loss decreases macrophage content in adipose tissue of obese women. Int J Obes (Lond) 2011; 35: 91–98.
Viardot A, Lord RV . Samaras K. The effects of weight loss and gastric banding on the innate and adaptive immune system in type 2 diabetes and prediabetes. J Clin Endocrinol Metab 2010; 95: 2845–2850.
Capel F, Klimcakova E, Viguerie N, Roussel B, Vitkova M, Kovacikova M et al. Macrophages and adipocytes in human obesity: adipose tissue gene expression and insulin sensitivity during calorie restriction and weight stabilization. Diabetes 2009; 58: 1558–1567.
Antunes BM, Rossi FE, Cholewa JM, Lira FS . Regular physical activity and vascular aging. Curr Pharm Des 2016; 22: 3715–3729.
Lin N, Shi JJ, Li YM, Zhang XY, Chen Y, Calder PC et al. What is the impact of n-3 PUFAs on inflammation markers in type 2 diabetic mellitus populations?: a systematic review and meta-analysis of randomized controlled trials. Lipids Health Dis 2016; 15: 133.
Acknowledgements
The work was supported by grant 16-14048S from the Grant Agency of Czech Republic, and by Projects PRVOUK P31 and UNCE 20431 from Charles University in Prague.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Siklova, M., Koc, M., Rossmeislová, L. et al. Serum oxLDL–β2GPI complex reflects metabolic syndrome and inflammation in adipose tissue in obese. Int J Obes 42, 405–411 (2018). https://doi.org/10.1038/ijo.2017.260
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.260
- Springer Nature Limited