Abstract
Hepatitis C virus (HCV)-induced, end-stage liver disease is a major indication for liver transplantation, but systematic graft reinfection accelerates liver disease recurrence. Transplantation recipients may be ineligible for direct-acting antivirals, owing to toxicity, resistance or advanced liver disease. Adoptive immunotherapy with liver graft-derived, ex vivo-activated lymphocytes was previously shown to prevent HCV-induced graft reinfections. Alternatively, the applicability and therapeutic efficacy of adoptive immunotherapy may be enhanced by ‘ready for use’ suicide gene-modified lymphocytes from healthy blood donors; moreover, conditional, prodrug-induced cell suicide may prevent potential side effects. Here, we demonstrate that allogeneic suicide gene-modified lymphocytes (SGMLs) could potently, dose- and time-dependently, inhibit viral replication. The effect occurs at effector:target cell ratios that exhibits no concomitant cytotoxicity toward virus-infected target cells. The effect, mediated mostly by CD56+ lymphocytes, is interleukin-2-dependent, IFN-γ-mediated and, importantly, resistant to calcineurin inhibitors. Thus, post-transplant immunosuppression may not interfere with this adoptive cell immunotherapy approach. Furthermore, these cells are indeed amenable to conditional cell suicide; in particular, the inducible caspase 9 suicide gene is superior to the herpes simplex virus thymidine kinase suicide gene. Our data provide in vitro proof-of-concept that allogeneic, third-party, SGMLs may prevent HCV-induced liver graft reinfection.
Similar content being viewed by others
Introduction
Chronic hepatitis C virus (HCV) infections are a major public health problem, due to the high prevalence (3% of global population; that is, 170 million people worldwide)1 and the severity of HCV-related complications, including liver cirrhosis and hepatocellular carcinoma. HCV-induced end-stage liver disease is a major indication for liver transplantation (LT).2 However, LT is associated with accelerated recurrence of liver disease due to systematic graft reinfections.3 Currently there is no preventive vaccine for HCV infection. The available treatments, which combine ribavirin and pegylated Interferon-α, are limited by major secondary effects, low effectiveness (50% treatment failure) and high costs.4 New treatments for HCV infections are currently under development. Many comprise different combinations of direct-acting antiviral drugs, like a protease and a polymerase inhibitor, which target several viral proteins essential for HCV replication and maturation. Those therapies were tested in treatment-naive and treatment-experienced patients, with preliminary results, suggesting good efficacy with limited treatment durations. Patients with HCV infection have been reported to be efficiently treated with interferon-free sofosbuvir-based regimens both before5 and after6 LT, with high rates of sustained virological responses, little resistance development, absence of drug–drug interactions and virtually no toxicity. Despite these promising results, novel directly antiviral drugs will not prevent recurrent hepatitis C in all patients with LT and a fraction of patients that await LT may be still ineligible for these new compounds, owing to toxicity, resistance or advanced liver disease. Moreover, drug interactions with calcineurin inhibitors still limit their use in patients with LTs,7 for whom no authorization for temporary use has been delivered. Thus, new approaches remain mandatory to provide a therapeutic option for preventing HCV reinfection of the liver graft, at least for specific subgroups of patients.
A phase I study conducted by Ohira et al.8 that included seven patients with HCV infections showed that an injection of activated lymphocytes reduced the HCV viral load after LT. Before transplantation, lymphocytes from the liver graft were recovered by perfusion of the graft; then, they were ex vivo activated for 3 days, and reinjected into the patient. A decrease in viral load was observed in five patients, and two of those five exhibited undetectable HCV levels; of the latter two, one relapsed, but the other continued to exhibit persistently HCV-negative serum, which strongly suggested that the chronic infection had healed. The decrease in viral load was more pronounced and persistent when the pre-transplant viral load was low; this finding suggested that the therapeutic effect was limited by reinfection of the graft. Indeed, when activated lymphocytes were injected into the patient 3 days after transplantation, the graft had already been reinfected.
Consequently, we reasoned that a cell infusion given at the time of transplantation might be more efficient than an infusion performed 3 days after transplantation. This approach would require injecting lymphocytes that had been activated prior to the transplantation. To that end, we propose to produce a bank of ‘ready for use’ activated lymphocytes from healthy donors that express a suicide gene. With this readily available store, at the time a patient receives a transplant, a batch of suicide gene-modified lymphocytes (SGMLs) could be chosen from the bank and administrated immediately, without wasting the time required for SGML production and qualification. However, there is a risk that allogeneic SGMLs might exert alloreactivity toward the patient’s cells or the liver graft, which could lead to severe side effects like graft-versus-host disease (GvHD) or liver graft rejection, respectively. To avoid these side effects, a suicide gene could be introduced into the lymphocytes prior to injection. Then, when side effects were detected, the SGMLs could be specifically eliminated by administering a prodrug that targets the suicide gene. These SGMLs are currently being tested as a gene therapy product in a phase III clinical study of patients who received haplo-identical allogeneic hematopoietic stem cell (HSC) transplantation. The SGMLs were successfully and safely infused into dozens of patients without major side effects.9, 10, 11, 12 Currently, those patients have undergone up to 15 years follow-up12, 13, 14 (for review, see15).
In this study, we investigated whether allogeneic SGMLs generated from healthy donors could provide a potent antiviral effect toward HCV-infected cells, as an in vitro proof-of-concept that such immunotherapy could be considered in patients with HCV infections that received a LT. Our findings provide perspective on the clinical use of SGMLs for preventing HCV reinfection of a liver graft.
Results
Suicide gene-modified cells inhibit in vitro HCV replication
With an HCV replicon-infected cell model, we first evaluated the antiviral activity of SGMLs. The SGMLs were generated after CD3 activation or CD3/CD28 costimulation to induce low and high alloreactivity, respectively.16, 17 Both SGML preparations produced a similar dose-dependent reduction in HCV replication; they achieved an ~3-log reduction in HCV replication at an effector:target cell ratio of 2:1 (Figure 1a). We confirmed this antiviral effect in a more relevant cell culture model system, where Huh7.5.1 cells were infected with the infectious cell culture produced-HCV (HCVcc) Jc1 strain (Supplementary Figure S1a). In both cell models, the antiviral effect was observed without significant SGML-mediated cytotoxicity toward the target cells (Figure 1b, Supplementary Figure S1b). Previous studies that evaluated various GvHD models17 found that SGMLs produced after CD3/CD28 costimulation were more aggressive in vivo than SGMLs produced after CD3 activation. Therefore, we used only the latter product for subsequent experiments.
Dose- and time-dependent inhibition of HCV replication by suicide gene-modified lymphocytes (SGMLs) in the absence of cytotoxicity against target cells (a) Inhibition of HCV replication by SGMLs. Fixed amounts of Huh7.5.1 cells were electroporated with a luciferase-expressing hepatitis C virus (HCV) replicon and cocultured with increasing numbers of effector cells (black circles, full line: SGMLs generated after CD3 activation; white circles, dashed line: SGMLs generated after CD3/CD28 costimulation). Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells cultured alone: 6.19 × 106±0.51 × 106 relative light units (RLU); n=6). (b) Target cell viability at different effector:target cell ratios. Target cells were stained with crystal violet at the end of the coculture experiments. Data correspond to experiments shown in (a), and cell viability is expressed as the mean±s.e. % optical density of cells cultured with SGMLs compared with that of control (target cells: 0.51±0.13; n=6). (c) Antiviral activity of SGMLs. Huh7.5.1 cells infected with the HCV replicon were cultured in the presence or absence of either varying numbers of effector cells, with or without 500 IU ml−1 IL-2 (a cofactor required for effector cell survival and proliferation) or in the presence or absence of 100 ng ml−1 IFN-γ (a positive control for antiviral activity, in the absence of effector cells; white circle). SGMLs: white diamonds, dashed line, n=4; non-transduced expanded control lymphocytes (Co)+IL-2: black triangles, full line, n=4; SGMLs+IL-2: black diamonds, full line, n=5. HCV replication was evaluated by quantifying luciferase activity 3 days after HCV infection. Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells alone, cultured without IL-2 or IFN- γ: 5.03 × 106±3.53 × 106 RLU; n=4). (d) Effect of IL-2 on antiviral activity in the HCVcc model. Huh7.5.1 cells infected with HCVcc were cultured as described in (c). HCV replication was evaluated by quantifying luciferase activity 3 days after infection. Antiviral activity is expressed as the mean±SE %HCV replication compared with that in control (target cells cultured without IL-2: 1.43 × 106±0.62 × 106RLU; n=3). (e) Effect of time on antiviral activity of SGMLs. At different times after infection, effector cells were incubated with Huh7.5.1 target cells infected with HCVcc. The cocultures were maintained for 3 days at effector:target cell ratios of 0:1 (dotted line), 0.5:1 (dashed line) or 2:1 (full line). Data are expressed as the mean±SE %HCV replication compared with that in control (target cells alone: 0.44 × 106±0.11 × 106 RLU on day 0; 0.98 × 106±0.29 × 106 RLU after 1 day; 1.42 × 106±0.44 × 106 RLU after 2 days; 1.57 × 106±1.11 × 106 RLU after 3 days; n=4). (f) Effect of freezing on antiviral activity of SGMLs. Cryopreservation did not affect the antiviral activity of SGMLs (white circles, dashed line) in the HCV replicon model, compared with fresh SGMLs (black circles, full line). Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells alone: 1.60 × 105±0.80 × 105 RLU; n=3).
The gene transfer process did not affect the antiviral activity of ex vivo-expanded lymphocytes; a similar result was obtained when SGMLs were compared with non-transduced expanded control cells (referred to as Co cells) in both the HCV replicon model (Figure 1c) and the HCVcc model (Figure 1d). Again, the antiviral effect was not associated with cytotoxic activity against target cells (Supplementary Figures S1c, d). In accordance with their known interleukin-2 (IL-2) dependence, the antiviral activity of SGMLs was more potent in the presence than in the absence of exogenous IL-2 (Figure 1c and d). Therefore, subsequent in vitro experiments were performed in the presence of 500 IU ml−1 IL-2.
The magnitude of inhibition of HCV RNA replication was lower in the HCVcc model than in the replicon model, raising the question of whether this was due to different efficiencies in transfection vs infection or because the HCVcc model constitutes the complete replication cycle of the virus rather than just subgenomic RNA replication. The percentage of transfected vs infected cells in Huh7.5.1. cells, quantified by flow cytometry after staining of the HCV core protein, was similar in both models at D1 of culture, but remained constant at D2 and D3 in the replicon model, whereas it continuously increased in the HCVcc model and was finally higher than in the replicon model (Supplementary Figure S2). These results suggest that such a higher percentage of infected cells may account, at least in part, for a less efficient inhibition of RNA replication by SGMLs.
In the HCVcc model, the antiviral effect of SGMLs was more pronounced when the coculture was initiated on the day of HCV inoculation compared with cocultures initiated 1–3 days later (Figure 1e). This result supported our hypothesis that SGMLs would be more efficient at preventing liver graft reinfection in an administration at the time of LT compared with an administration 3 days later. Cryopreservation did not affect the antiviral activity of SGMLs, as shown by the similar antiviral activity observed between fresh and frozen cells (Figure 1f). This result demonstrated that cryopreserved cells may be adequate for clinical use.
Phenotypical and functional characterization of SGMLs involved in antiviral activity
Although the low effector:target cell ratio facilitated a lack of significant SGML-mediated cytotoxicity against target cells, we could not exclude the possibility that only a few target cells were electroporated in the HCV replicon model or infected in the HCVcc infection model; the specific killing of only a few cells would not be detected in our cytotoxicity assay. Therefore, to exclude direct cell killing, antiviral assays in the HCV replicon system were performed in a transwell configuration, where effector and target cells were cultured in separate chambers, but soluble factors could diffuse between the chambers. Again, SGMLs exhibited strong, IL-2-dependent antiviral activity (Figure 2a). This result indicated that effector-target cell contact was not required for inhibiting HCV replication, and the antiviral effect was not dependent upon receptor-mediated cytotoxicity. These results suggested that the antiviral activity was mediated, at least in part, by soluble factors.
SGML antiviral activity is mediated by IFN-γ, mostly from CD56+ cells. (a) Target cells were cultured as indicated in (Figure 1c), but the target cells were separated from the effector cells in transwells, where the effector cells were placed in the upper chamber, and the target cells were placed in the lower chamber, with a permeable membrane (pore size: 0.4 μm) between the chambers. HCV replication was evaluated by quantifying luciferase activity 3 days later, expressed as the mean±s.e. %HCV replication compared with that in control (target cells alone, cultured without IL-2: 3.96 × 106±2.55 × 106 RLU; n=4). (b) SGMLs were assessed for antiviral activity in the HCV replicon model at an effector:target cell ratio of 2:1. Effector cells were cultured separate from target cells in transwells in the absence or presence of 5 μg ml−1 anti-IFN-α, anti-IFN-β, anti-IFN-γ or isotype (isot) control mAbs. Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells cultured without SGMLs: 4.71 × 106±3.14 × 106 RLU; n=3). (c) The frequency of CD56-negative cells (white bars) and CD56-positive cells (black bars) was quantified by flow cytometry; PBMC: the initial suspension, Co cells: non-transduced, expanded lymphocytes. Data are expressed as the mean±s.e. % cell subsets compared with the total number of cells (n=3). (d) CD56-depleted (CD56−; white diamonds, dashed line) and CD56-enriched (CD56+; white triangles, dashed line) fractions of SGMLs were compared with unsorted SGMLs (black circles, full line) for antiviral activity in the HCV replicon model. Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells alone: 7.62 × 106±5.96 × 106 RLU; n=4).
The addition of anti-IFN-γ monoclonal antibodies (mAbs), but not anti-IFN-α or anti-IFN-β mAbs, blocked the antiviral effect of SGMLs on HCV replication. The results were similar in a transwell assay (Figure 2b), in a coculture assay (Supplementary Figure S3a) and in the HCVcc system (Supplementary Figure S3b). The combination of anti-IFN-α, -β and –γ mAbs did not further block the antiviral activity (data not shown).
Most SGMLs are CD3+ CD56− T cells; the remaining cells are CD3+ CD56+ ‘NK-like’ T cells and CD3− CD56+ NK cells (Figure 2c and Sauce et al.16). To decipher which of these cells were involved in the antiviral activity of SGMLs, CD56+ and CD56− cells were purified by immunomagnetic sorting. We found that both fractions contributed to the antiviral activity, although CD56− cells had a slightly lower antiviral activity than CD56+ cells. The results were similar in the HCV replicon (Figure 2d) and the HCVcc systems (Supplementary Figure S3c), and again, no cytotoxic activity was detected against target cells (Supplementary Figures S3d, e).
The antiviral activity of SGMLs is not inhibited by calcineurin inhibitors
One potential limitation of our approach was the potential for allo-immunization. Indeed, the patient could develop an immune response against SGMLs, and that would result in SGML elimination. This effect would be undesirable for two reasons: (1) SGML rejection would reduce their therapeutic effect and (2) a cross-reaction could contribute to hepatic graft rejection. The calcineurin inhibitors, Cyclosporin A (CsA) and Tacrolimus (Levallois-Perret, France; FK506), are typically administered to patients with LTs to prevent graft rejection. We previously reported that the alloreactivity of ex vivo-expanded lymphocytes was resistant to CsA.18 Therefore, we reasoned that calcineurin inhibitors might prevent allo-immunization against both the liver graft and the SGMLs, but would not impair SGML antiviral activity. Thus, we evaluated in vitro the effects of CsA and FK506 on HCV replication. Electroporated Huh7.5.1 cells were incubated in the absence or presence of fixed amounts of SGMLs with increasing concentrations of CsA or FK506, in the HCV replicon model (Figure 3a and b) or in the HCVcc model (Figure 3c and d). In accordance with previous reports,19 a high concentration of CsA (Figure 3a and c), but not FK506 (Figure 3b and d), exhibited an inhibitory in vitro effect on HCV replication, and this effect was not due to a toxic effect on cell viability (Supplementary Figure S4). However, neither CsA nor FK506 blocked the antiviral effect of SGMLs (Figure 3), indicating that SGMLs were resistant to the immunosuppressive activity of calcineurin inhibitors. Similar results were observed when exogenous IL-2 was omitted in the culture (Supplementary Figure S5), indicating that a possible reversal of the SGML antiviral activity by calcineurin inhibitors is not overcome by the addition of exogenous IL-2. These results suggested that administration of calcineurin inhibitors to recipients of LTs as a prophylaxis for liver graft rejection may not prevent the antiviral activity of SGMLs.
SGML antiviral activity is resistant to calcineurin inhibitors. Huh7.5.1 target cells were incubated in the absence (white circles, dashed lines) or presence (black circles, full lines) of SGMLs at an effector:target cell ratio of 0.5:1 in the HCV replicon model (a, b) or at an effector:target cell ratio of 2:1 in the HCVcc infection model (c, d). All cultures were performed in the presence of 500 IU ml−1 IL-2 and were exposed to increasing amounts of CsA (a, c) or FK506 (b, d). HCV replication was evaluated 3 days later. Data are expressed as the mean±s.e. %HCV replication compared with that in control (target cells cultured without SGMLs nor calcineurin inhibitor: (a) 7.56 × 106±6.25 × 106, n=4; (b) 6.90 × 106±5.85 × 106, n=4; (c) 2.64 × 105±0.93 × 105, n=4; (d) 4.86 × 105±1.53 × 105, n=4).
SGML depletion is more efficient with the iCasp9 than with the HSV-tk suicide gene
We assessed the ability of the HSV-tk suicide gene to reverse SGML-induced cytotoxicity. We prepared cocultures at low (⩽1:1) and high (2:1 to 8:1) effector:target cell ratios, in the presence or absence of the prodrug, ganciclovir (GCV), added at the initiation of culture. After 3 days of coculture, a slight shift in the viability curve was observed (Figure 4a), indicating that GCV caused a small inhibition in the cytotoxic activity of HSV-tk+ SGMLs against the target cells. This weak GCV-induced depletion of HSV-tk+ SGMLs prompted us to examine SGMLs that expressed the iCasp9 suicide gene. The new-generation, iCasp9 suicide gene was reported to confer more rapid, efficient killing than the HSV-tk suicide gene, when cells were exposed to its prodrug, a chemical inducer of death (CID)20. We found that the addition of the CID at initiation of the culture indeed completely prevented the cytotoxic activity of iCasp9+ SGMLs at high effector:target cell ratios (Figure 4b), up to a 40:1 ratio (data not shown); as expected, GCV had no effect on these iCasp9+ SGMLs. Conversely, also as expected, the CID did not affect the cytotoxic activity of HSV-tk+ SGMLs (Figure 4a). When evaluated in terms of lytic units (calculated as shown in Supplementary Figure S6), GCV had no effect on HSV-tk+ SGMLs, but CID completely prevented the cytotoxicity of iCasp9+ SGMLs (Figure 4c). The greater efficacy of the iCasp9/CID system over the HSV-tk/GCV system may not result from a more pronounced SGML depletion, but rather, from a more rapid depletion. This was suggested by the observation that, after one week of SGML cultures in the presence of their respective prodrugs, both prodrugs caused a similar level of SGML depletion (Figure 4d). To further evaluate the effect of SGML depletion on antiviral activity, iCasp9+ SGMLs were cocultured with target cells in the absence or presence of CID. The antiviral activity, evaluated at noncytotoxic effector:target cell ratios (Figure 4e), was associated with an IFN-γ production (Figure 4f) and the SGML depletion by CID was associated with the abrogation of the antiviral effect (Figure 4e) and of the IFN-γ production (Figure 4f).
SGML depletion was more efficient with iCasp9/CID than with HSV-tk/GCV. SGMLs that expressed either the HSV-tk (a) or the iCasp9 (b) suicide gene were cocultured with Huh7.5.1 target cells electroporated with the HCV replicon. Cocultures were not exposed (PBS: black diamonds, full line) or exposed to either GCV (white squares, dashed line) or CID (white triangles, dashed line) at the indicated effector:target cell ratios (from 0:1 to 8:1). The target cell viability, evaluated 3 days later, is expressed as the mean±s.e. %optical density compared with that of control (target cells alone: optical density=0.97±0.03 for one donor representative of three). (c) The effect of prodrugs on SGML cytotoxicity. HSV-tk+ SGML (left) and iCasp9+ SGML (right) cytotoxicities were measured after 3 days of coculture with target cells in the presence or absence of prodrugs, CID or GCV. Data are expressed as the mean±s.e. %LU50 compared with that of control effector:target cocultures without prodrug (controls=100%). Control measurements were: CD34/HSV-tk SGMLs: 116±59 LU50 (n=3); CD19/iCasp9 SGMLs: 105±34 LU50 (n=4). (d) The efficiencies of GCV and CID in SGML depletion. SGMLs were expanded for one week in the absence (PBS) or presence of a prodrug. Data are expressed as the mean±s.e. relative cell growth during this week (n=4). (e, f) The effects of the CID prodrug on the antiviral activity and IFN-γ production by SGMLs. Huh7.5.1 target cells electroporated with the HCV replicon were cocultured with iCasp9+ SGMLs at the indicated effector:target cell ratios, in the absence (white bars) or presence (black bars) of CID and were evaluated 3 days later for HCV replication (e) and IFN-γ concentration in the culture supernatant (f). Date in (e) are expressed as the mean±s.e. %HCV replication compared with that in control (target cells cultured without SGMLs and without CID: 1.09 × 106±0.02 × 106 RLU; n=3). Data in (f) are expressed as ng ml−1 IFN-γ (mean±s.e., n=3).
Discussion
LT is the treatment of choice for end-stage liver diseases, but the systematic reinfection of the graft, associated with an accelerated recurrence of liver disease after transplantation limits its use in patients with HCV infections. A phase I clinical trial performed by Ohira et al.8 demonstrated that liver graft-derived, ex vivo-activated lymphocytes infused 3 days after transplantation could provide an antiviral effect that could prevent liver graft HCV reinfection. In that study, the activated hepatic lymphocytes had a more potent antiviral effect when the initial viral load was low. Conversely, with a high viral load, the antiviral effect was less potent. Hence, we reasoned that, at 3 days after LT, the liver graft may have already been reinfected; however, at the time of transplantation, the liver graft would be less likely to be reinfected. Therefore, the activated lymphocytes should be delivered at the time of transplantation. However, this approach requires cell preparation prior to the acquisition of the liver graft; thus, the SGMLs must be produced from other sources. Therefore, we considered the possibility of using third-party allogeneic SGMLs acquired from healthy blood donors. Indeed, this cell therapy product contains ex vivo-activated lymphocytes. We previously demonstrated that SGMLs could be safely infused into patients that had received an HSC transplantation. In that study, we showed that SGMLs could specifically control occasional side effects, such as the induction of GvHD.12 Furthermore, the prior ex vivo retroviral-mediated transfer of a suicide gene into the SGMLs allowed their specific in vivo killing with the administration of a prodrug, delivered at the time side effects were detected.
In the present study, we showed that SGMLs provided a potent antiviral effect at low effector:target cell ratios that are non-toxic for target cells. We tested SGMLs on two in vitro HCV replication models, including the widely used HCVcc infection model. We observed that the SGML-mediated antiviral effect was more efficient when SGMLs were added at time of HCV inoculation, and that the later the time of SGMLs addition, the lower the efficacy. This finding confirmed our hypothesis that activated lymphocytes, such as SGMLs, should be infused at the time of transplantation. The observation that an antiviral effect can be observed at low, non-toxic effector:target cell ratios suggest that the number of cells that need to be activated in order to produce the IFN-γ involved in the antiviral effect is lower than the number of cells required to induce a cytotoxic effect. This interpretation is substantiated by the observation that the CID-induced depletion of SGMLs abrogated completely their cytotoxic activity, but only partially their antiviral effect; at high effector-target cell ratios, few SGMLs may escape the CID-induced death and may be sufficient to generate an antiviral effect, but not a cytotoxic one.
Similarly to liver lymphocytes8, peripheral blood mononuclear cells (PBMCs) subjected to CD3+IL-2 activation present an IFN-γ-mediated antiviral activity toward HCV and an antitumor activity toward hepatocellular carcinoma, both provided mostly by CD56+ cells, including CD3− CD56+ NKs and CD3+ CD56+ NK-like T cells.21 These studies are consistent with our present results and with our recent report, demonstrating that high concentrations of SGMLs provided NK and NK-like T-cell-mediated antitumor effects in an hepatocellular carcinoma model22. However, as they were generated after short-term (3 days) activation with IL-2, this raises the question of the similitude of such activated lymphocytes, as well as of our SGMLs, with lymphokine-activated killer (LAK) cells. Indeed, the clinical use of LAK cells was limited owing to a massive release of cytokines and subsequent pulmonary edema, requiring intensive care. Our SGMLs seem to be closer to cytokine-induced killer cells than to LAK cells in terms of protocol of activation (CD3+IL-2 for SGMLs vs CD3+IL-2±IFN-γ ±IL-1 for cytokine-induced killer cells vs IL-2 for LAK cells) and culture duration (2–4 weeks for SGMLs and cytokine-induced killer cells vs 3–5 days for LAK cells). One may hypothesize that this may lead to differences between LAK vs SGML (or cytokine-induced killer cells), as an example in terms of expression of homing molecules (thus, of homing properties) and/or exhaustion (thus, of potential for cytokine release, proliferation and cytotoxicity). Indeed, SGMLs, evaluated in phase I to III clinical trials in patients transplanted with hematopoietic stem cells, induced limited toxicities9, 10, 11, 12 and, to the best of our knowledge, no pulmonary edema.
Using a humanized hepatocellular carcinoma mouse model, we previously demonstrated that, when infused intravenously, SGMLs preferentially homed to the liver and weakly migrated to the lungs.22 This property is of advantage to improve the efficacy while limiting the peripheral spreading of SGMLs. Indeed, infusing SGMLs could allow reaching high local concentrations of IFN-γ, close to the target cells while leading to low peripheral IFN-γ concentrations. In this respect, this should be of great advantage, in terms of tolerability, over infusing exogenous recombinant IFNs, such as IFN-γ or IFN-α: the IFN-α toxicity is a strong limitation of the current pegylated-IFN-α-based regimen due to the doses required to reach efficient concentrations in the liver, which also lead to high concentrations in peripheral, non-target organs and induce severe side effects. However, the use of allogeneic SGMLs is associated with complex immunological interactions involving three immunological partners: the patient’s immune system, the liver graft lymphocytes and the allogeneic SGMLs, generated from a third-party donor. Nevertheless, SGMLs also have the advantage of being resistant to CsA inhibition. Thus, an immunosuppressive regimen with CsA can control the first two partners: (1) the recipient immune system alloreactivity toward the liver graft (prevention of liver graft rejection) and toward SGMLs, and (2) the alloreactivity of grafted liver lymphocytes toward the recipient tissues (hepatic GvHD). Alternatively, the third partner, the SGMLs, can be controlled with the suicide gene approach without affecting the first two partners.
One important issue is to determine whether there is any advantage in using third-party SGMLs, which are genetically different from the liver graft, compared with using autologous liver graft-derived lymphocytes. This hypothesis is technically challenging to investigate, because HCV replication is typically evaluated in vitro, with established hepatoma cell lines. Indeed, primary human hepatocytes are mostly refractory to HCV infection in vitro. Thus, comparing the antiviral activity of SGMLs toward autologous vs allogeneic primary human hepatocytes remains unfeasible. Indirect observations have suggested that alloreactivity may provide additional benefits. When activated lymphocytes were restimulated with CD3 mAbs 24 h before evaluation of their antiviral activity, their ability to decrease HCV replication improved.21 Also, allogeneic HSC transplantation,23 but not autologous HSC transplantation,24 was reported to lead to loss of detectable HIV, which was temporally correlated with full donor chimerism, but also to the development of GVHD, a complication of HSC transplantation associated with alloreactivity. Although the mechanisms leading to a HIV cure after HSC transplantation remain to be elucidated, and although they may be different from those involved in the prevention of HCV replication, those results suggested that alloreactivity may add benefit to an antiviral effect.
To date, clinical experiences with SGMLs in an allogeneic context have shown that the potential risk of GvHD induction is low, particularly in the liver, and that, even when side effects occur, they can be efficiently controlled with the suicide gene approach.9, 12, 25 Therefore, we propose to produce a bank of ‘ready for use’ allogeneic SGMLs. Then, when a patient receives a LT, a batch of SGMLs could be selected from the bank and infused into the patient during transplantation, without wasting the time required for SGML production and qualification. Taken together, our results have provided in vitro proof-of-concept that an adoptive immunotherapy can be safely applied to the efficient prevention of liver graft reinfection by HCV. Additional in vivo experiments with human liver-chimeric mouse models of HCV infections26 will be required to demonstrate further the feasibility of our approach.
Materials and methods
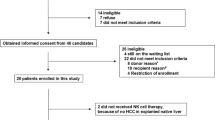
Production of SGMLs
Allogeneic SGMLs were produced as previously described.22 After informed consent from healthy blood donors, PBMCs were isolated by ficoll centrifugation of donated blood. Harvested PBMCs were activated with a CD3 mAb (10 ng ml−1 OKT3, Jansen-Cilag, Levallois-Perret, France) and human IL-2 (500 IU ml−1, Proleukin, Novartis Pharma, Dorval, Québec). Activated PBMCs were cultured for 3 days, and on day 3, they were transduced with one of two retroviral vectors. One was the MP71-T34FT vector, which encoded a truncated form of the human CD34 sequence fused to the HSV-tk sequence.17, 27 The other retroviral vector (SFG.iCasp9.2A.ΔCD19; provided by Pr M.K. Brenner, Center for Cell and Gene Therapy, Baylor College of Medicine, Houston, TX) encoded the human CD19 and iCasp9 sequences.25 Transduced cells were immunomagnetically selected on day 5 and expanded until day 14. These transduced and CD34-selected or CD19-selected cells are referred to as SGMLs. In parallel, nontransduced cells were expanded for 14 days to serve as control cells and are referred to as Co cells. Effector cells (SGMLs or, when indicated, Co cells or PBMCs) were qualified for phenotype and prodrug sensitivity. Also, they were functionally characterized in vitro for antiviral activity and cytotoxicity.
The percentage of transduced selected cells out of the total numbers of CD34+ or CD19+ cells before immunomagnetic selection (that is, the transduction efficiency) was determined by immunostaining with phycoerythrin-conjugated CD34 mAb or allophycocyanin-conjugated CD19 mAb (Miltenyi Biotec, Paris, France) and flow cytometry analyses (LSRII, Becton Dickinson, San Diego, CA, USA). The transduction efficiency was 13.1±3.1% (n=10) for CD34/HSV-tk+ SGMLs and 26.1±8.1% (n=6) for CD19/iCasp9+ SGMLs, respectively. The purity of the positive fraction after immunomagnetic sorting was 93.6±0.7% (n=10) for CD34/HSV-tk+ SGMLs and 97.2±0.9% (n=6) for CD19/iCasp9+ SGMLs, respectively. The sensitivity of SGMLs to the corresponding prodrug was confirmed by culturing HSV-tk+ SGMLs in the absence or presence of 1 μg ml−1 ganciclovir, or GCV (Cymevan; Syntex, Puteaux, France), or by culturing iCasp9+ SGMLs in the presence or absence of 10 nM of CID (BB homodimerizer; Ozyme, St Quentin en Yvelines, France). The relative cell growth was defined as the absolute number of cells obtained at the indicated time of culture to the number of input cells at the initiation of the culture.
Evaluation of SGML antiviral activity
The HCV replicon model
Huh7.5.1 cells were cultured in Dulbecco's Modified Eagle Medium (PAA Laboratories, Vélizy Villacoublay, France) supplemented with 10% fetal bovine serum (PAN Biotech GmbH, Aidenbach, Germany), non-essential amino acids (GIBCO, Invitrogen, Cergy Pontoise, France) and 10 μg ml−1 gentamycin (GIBCO). Huh7.5.1 cells were electroporated with an HCV replicon that comprised RNA corresponding to the HCV genome, genotype 2a, isolate JFH1, which was defective for virus entry, due to deletions of E1 and E2 envelope proteins and the luciferase gene (JFH1ΔE1E2-luc). In the present study, the Huh7.5.1 cells served as ‘target cells’.
Different amounts of SGML cells (effectors) were co-incubated with fixed amounts of target cells to produce effector:target cell ratios that ranged from 0.125:1 to 2:1 (cocultures that allowed contact between effector and target cells). The same cell numbers were also cultured in separate compartments (transwell cultures, which did not allow contact between effector and target cells) using transwells with a pore size of 0.4 μm (Sigma, Lyon, France). Unless otherwise indicated, all cultures were performed in the presence of 500 IU ml−1 IL-2. Target cells alone were cultured in the presence of 100 ng ml−1 IFN-γ (Clinisciences, Nanterre, France) to serve as a positive control of viral replication inhibition. After 3 days of culture, SGMLs (non-adherent cells) and dead target cells were removed by washing, and the remaining viable target cells (adherent cells) were lysed with 0.1% w/v SDS in PBS. Luciferin was then added to measure luciferase activity, which reported viral replication within target cells.
We also investigated which soluble factor(s) were involved in SGML antiviral activity. During the co-incubation of SGMLs and target cells, we added antibodies (final concentration of 5 μg ml−1; eBioscience SAS, Paris, France) that specifically blocked IFN-α, IFN-β and IFN-γ (and an isotype control). The quantification of IFN-γ in culture supernatants was performed using a Legend Max human IFN-γ ELISA kit (BioLegend, San Diego, CA, USA) according to the manufacturer’s instructions.
Where indicated, after 14 days of expansion, CD56− (T lymphocytes) and CD56+ (NK and NK-like T cells) populations were isolated from SGMLs with phycoerythrin-conjugated CD56 antibody with the anti-phycoerythrin Multisort kit (Miltenyi Biotec). The separation was performed with the autoMACS Separator (Miltenyi Biotec). The purity of each cell fraction was determined by immunostaining with Pacific Blue-conjugated CD3 mAb (Becton Dickinson) and phycoerythrin-conjugated CD56 mAb (Miltenyi Biotec), and performing flow cytometry (LSRII, Becton Dickinson). The antiviral activities of CD56− and CD56+ fractions were tested at different effector:target cell ratios, as previously described.
We intended to use these SGMLs in an immunosuppressive context; therefore, we tested SGML resistance to calcineurin inhibitors. To that end, Huh7.5.1 and SGMLs were cocultured at an effector:target cell ratio of 0.5:1 in the presence of different concentrations of either CsA or FK506 (Tacrolimus).
The cell culture produced-HCV model: The HCVcc model allowed the production of infectious viral particles. In brief, Huh7.5.1 cells were infected with the recombinant virus, Jc1 HCVcc (genotype 2a/2a chimera), which also expressed luciferase. This laboratory prototype strain, based on JFH1,28 has been used extensively to study virus–host interactions and to evaluate antivirals in vitro and in vivo.28, 29, 30, 31, 32 At different days post infection, SGMLs were added to HCVcc-infected Huh7.5.1 cells at effector:target cell ratios of 0.5:1 or 2:1. Three days after adding SGMLs, Huh7.5.1 cells were lysed and tested for luciferase activity. Huh7.5.1 cell viability was evaluated with crystal violet staining, as previously described. The antiviral activities of CD56− and CD56+ subsets of SGMLs were also tested in this system at an effector:target cell ratio of 0.5:1.
Evaluation of SGML cytotoxic activity
In each assay, effector and target cells were cocultured in parallel with the antiviral assays to monitor target cell viability. After 3 days of coculture, non-adherent effector cells and dead target cells were removed by washing with PBS; the remaining viable, adherent, target cells were stained for 15 min at room temperature with crystal violet (Sigma). Cells were then washed three times with tap water and lysed with 1% w/v SDS in PBS for 10 min at room temperature. Viable cell density was determined by the absorbance at 560 nm, measured on a Mithras LB 940 microplate reader (Berthold, Thoiry, France). Cell viability was expressed as the percent optical density of treated cells compared with control cells. We also calculated the inverse of the number of cells per 106 effector cells required to detect a 50% decrease in optical density (lytic units 50%; LU50; Supplementary Figure S6). The LU50 values of the experimental groups were normalized to the LU50 values of the corresponding control groups to control for inter-experimental variations. The results are expressed as the mean LU50±s.e.m.
References
Global surveillance and control of hepatitis C. Report of a WHO Consultation organized in collaboration with the Viral Hepatitis Prevention Board, Antwerp, Belgium. J Viral Hepatitis 1999; 6: 35–47.
Skagen C, Lucey M, Said A . Liver transplantation: an update 2009. Curr Opin Gastroenterol 2009; 25: 202–208.
Gane EJ . The natural history of recurrent hepatitis C and what influences this. Liver Transpl 2008; 14: S36–S44.
Tai AW, Chung RT . Treatment failure in hepatitis C: mechanisms of non-response. J Hepatol 2009; 50: 412–420.
Curry MP, Forns X, Chung RT, Terrault N, Brown RS, Fenkel JM et al. Pretransplant sofosbuvir and ribavirin to prevent recurrence of HCV infection after liver transplantation. Hepatology 2013; 58: 314A–315A.
Forns X, Fontana RJ, Moonka D, McHutchison JG, Symonds WT, Denning JM et al. Initial evaluation of the sofosbuvir compassionate use program for patients with severe recurrent HCV following liver transplantation. Hepatology 2013; 58: 732A–733A.
Charlton M . Telaprevir, boceprevir, cytochrome P450 and immunosuppressive agents—a potentially lethal cocktail. Hepatology 2011; 54: 3–5.
Ohira M, Ishiyama K, Tanaka Y, Doskali M, Igarashi Y, Tashiro H et al. Adoptive immunotherapy with liver allograft-derived lymphocytes induces anti-HCV activity after liver transplantation in humans and humanized mice. J Clin Invest 2009; 119: 3226–3235.
Bonini C, Ferrari G, Verzeletti S, Servida P, Zappone E, Ruggieri L et al. HSV-TK gene transfer into donor lymphocytes for control of allogeneic graft-versus-leukemia. Science 1997; 276: 1719–1724.
Ciceri F, Bonini C, Stanghellini MTL, Bondanza A, Traversari C, Salomoni M et al. Infusion of suicide-gene-engineered donor lymphocytes after family haploidentical haemopoietic stem-cell transplantation for leukaemia (the TK007 trial): a non-randomised phase I-II study. Lancet Oncol 2009; 10: 489–500.
Zhou X, Di Stasi A, Tey SK, Krance RA, Martinez C, Leung KS et al. Long-term outcome after haploidentical stem cell transplant and infusion of T cells expressing the inducible caspase 9 safety transgene. Blood 2014; 123: 3895–3905.
Tiberghien P, Ferrand C, Lioure B, Milpied N, Angonin R, Deconinck E et al. Administration of herpes simplex-thymidine kinase-expressing donor T cells with a T-cell-depleted allogeneic marrow graft. Blood 2001; 97: 63–72.
Mercier-Letondal P, Deschamps M, Sauce D, Certoux JM, Milpied N, Lioure B et al. Early immune response against retrovirally transduced herpes simplex virus thymidine kinase-expressing gene-modified T cells coinfused with a T cell-depleted marrow graft: an altered immune response? Hum Gene Ther 2008; 19: 937–950.
Deschamps M, Mercier-Lethondal P, Certoux JM, Henry C, Lioure B, Pagneux C et al. Deletions within the HSV-tk transgene in long-lasting circulating gene-modified T cells infused with a hematopoietic graft. Blood 2007; 110: 3842–3852.
Mailly L, Leboeuf C, Tiberghien P, Baumert T, Robinet E . Genetically engineered T-cells expressing a ganciclovir-sensitive HSV-tk suicide gene for the prevention of GvHD. Curr Opin Investig Drugs 2010; 11: 559–570.
Sauce D, Tonnelier N, Duperrier A, Petracca B, de Carvalho Bittencourt M, Saadi M et al. Influence of ex vivo expansion and retrovirus-mediated gene transfer on primary T lymphocyte phenotype and functions. J Hematother Stem Cell Res 2002; 11: 929–940.
Mercier-Letondal P, Montcuquet N, Sauce D, Certoux JM, Jeanningros S, Ferrand C et al. Alloreactivity of ex vivo-expanded T cells is correlated with expansion and CD4/CD8 ratio. Cytotherapy 2008; 10: 275–288.
Contassot E, Robinet E, Angonin R, Laithier V, Bittencourt M, Pavy JJ et al. Differential effects of cyclosporin A on the alloreactivity of fresh and ex vivo-expanded T lymphocytes. Bone Marrow Transplant 1998; 22: 1097–1102.
El-Farrash MA, Aly HH, Watashi K, Hijikata M, Egawa H, Shimotohno K . In vitro infection of immortalized primary hepatocytes by HCV genotype 4a and inhibition of virus replication by cyclosporin. Microbiol Immunol 2007; 51: 127–133.
Marin V, Cribioli E, Philip B, Tettamanti S, Pizzitola I, Biondi A et al. Comparison of different suicide-gene strategies for the safety improvement of genetically manipulated T cells. Hum Gene Ther Methods 2012; 23: 376–386.
Doskali M, Tanaka Y, Ohira M, Ishiyama K, Tashiro H, Chayama K et al. Possibility of adoptive immunotherapy with peripheral blood-derived CD3(−)CD56+ and CD3+CD56+ cells for inducing antihepatocellular carcinoma and antihepatitis C virus activity. J Immunother 2011; 34: 129–138.
Leboeuf C, Mailly L, Wu T, Bour G, Durand S, Brignon N et al. In vivo proof of concept of adoptive immunotherapy for hepatocellular carcinoma using allogeneic suicide gene-modified killer cells. Mol Ther 2014; 22: 634–644.
Henrich TJ, Hu Z, Li JZ, Sciaranghella G, Busch MP, Keating SM et al. Long-term reduction in peripheral blood HIV type 1 reservoirs following reduced-intensity conditioning allogeneic stem cell transplantation. J Infect Dis 2013; 207: 1694–1702.
Cillo AR, Krishnan A, Mitsuyasu RT, McMahon DK, Li S, Rossi JJ et al. Plasma viremia and cellular HIV-1 DNA persist despite autologous hematopoietic stem cell transplantation for HIV-related lymphoma. J Acquir Immune Defic Syndr 2013; 63: 438–441.
Di Stasi A, Tey SK, Dotti G, Fujita Y, Kennedy-Nasser A, Martinez C et al. Inducible apoptosis as a safety switch for adoptive cell therapy. N Eng J Med 2011; 365: 1673–1683.
Mercer DF, Schiller DE, Elliott JF, Douglas DN, Hao C, Rinfret A et al. Hepatitis C virus replication in mice with chimeric human livers. Nat Med 2001; 7: 927–933.
Fehse B, Kustikova OS, Li Z, Wahlers A, Bohn W, Beyer WR et al. A novel 'sort-suicide' fusion gene vector for T cell manipulation. Gene Ther 2002; 9: 1633–1638.
Wakita T, Pietschmann T, Kato T, Date T, Miyamoto M, Zhao Z et al. Production of infectious hepatitis C virus in tissue culture from a cloned viral genome. Nat Med 2005; 11: 791–796.
Lindenbach BD, Evans MJ, Syder AJ, Wolk B, Tellinghuisen TL, Liu CC et al. Complete replication of hepatitis C virus in cell culture. Science 2005; 309: 623–626.
Lindenbach BD, Meuleman P, Ploss A, Vanwolleghem T, Syder AJ, McKeating JA et al. Cell culture-grown hepatitis C virus is infectious in vivo and can be recultured in vitro. Proc Natl Acad Sci USA 2006; 103: 3805–3809.
Pietschmann T, Kaul A, Koutsoudakis G, Shavinskaya A, Kallis S, Steinmann E et al. Construction and characterization of infectious intragenotypic and intergenotypic hepatitis C virus chimeras. Proc Natl Acad Sci USA 2006; 103: 7408–7413.
Zhong J, Gastaminza P, Cheng G, Kapadia S, Kato T, Burton DR et al. Robust hepatitis C virus infection in vitro. Proc Natl Acad Sci USA 2005; 102: 9294–9299.
Acknowledgements
This study was supported by Inserm, the Fondation pour la Recherche Médicale (Comité Alsace), the Ligue Nationale Contre le Cancer (Conférence de Coordination Inter-Régionale Grand-Est, grant # 1FI10005LBKD), the Association pour la recherche sur le Cancer (ARC, grant # SFI20111203529), the Société d’Accélération de Transfert de Technologie (SATT) Conectus Alsace, the Agence Nationale pour la Recherche (ANR, LabEx program) and EU Interreg-IV Program Hepato-Regio-Net. Eric Robinet was supported by the Agence Nationale pour la Recherche sur le SIDA et les Hépatites Virales (ANRS, grant # 2008 059 ULP). Céline Leboeuf received fellowships from the Fondation Transplantation and the Association pour la Recherche sur le Cancer (ARC, grant # DOC20110603384); and Tao Wu received a fellowship from the Alsace Region. A European Patent application (n° EP12305259.9) related to this study, entitled ‘Method for preventing or treating HCV infection by administration of suicide gene-modified lymphocytes’, was submitted on the 2 March 2012 by the University of Strasbourg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Gene Therapy website
Supplementary information
Rights and permissions
About this article
Cite this article
Leboeuf, C., Roser-Schilder, J., Lambotin, M. et al. Prevention of hepatitis C virus infection by adoptive allogeneic immunotherapy using suicide gene-modified lymphocytes: an in vitro proof-of-concept. Gene Ther 22, 172–180 (2015). https://doi.org/10.1038/gt.2014.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2014.99
- Springer Nature Limited