Abstract
Purpose
This study investigates the radiological outcomes of robotic-assisted total hip arthroplasty (RATHA) compared to manual total hip arthroplasty (mTHA), addressing the ongoing debate on the effectiveness of RATHA in achieving superior implant positioning accuracy.
Methods
A prospective cohort of 212 patients (103 robotic, 109 manual) underwent THA and were evaluated for postoperative radiological outcomes, focusing on the inclination and anteversion angles of the acetabular cup. Outlier prevalence was assessed based on angles outside the defined Lewinnek safe zones. All post-operative measurements were made using the BoneNinja application.
Results
High inter-observer and intra-observer reliabilities were observed, validating the measurement accuracy. The mean anteversion and inclination angles in the RATHA cohort were 40.5 ± 1.5 and 24.5 ± 3.1° respectively; and the mTHA cohort were 42.1 ± 4.9 and 24.9 ± 4.5°. There was a statistically significant difference in inclination angles between the two cohorts whereas the anteversion angles showed no difference. Majority of the conventional THRs (N = 72, 55.4%) were placed outside the safe zone for anteversion. The inclination angles revealed a highly significant difference between the cohorts (p < 0.0001), with all the robotic THRs (N = 121, 100%) being placed within the safe zone for inclination, whereas only 70% (N = 91) of the conventional THRs were within the safe zone. 97.5% of RA-THRs were within 3° of the proposed plan, demonstrating high accuracy.
Conclusion
RATHA significantly outperforms MTHA in radiological accuracy, achieving precise acetabular cup positioning with minimal outliers. These results advocate for RATHA's adoption in THA to enhance outcome predictability and affirm its reliability and safety over manual methods.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) stands as a prevalent and efficacious orthopaedic intervention employed to alleviate pain and enhance functionality in individuals grappling with hip joint arthritis [1]. The accurate alignment of the acetabular and femoral components assumes paramount importance in augmenting post-operative results and mitigating potential complications such as dislocation [2], impingement [3], accelerated wear [4, 5], perturbed hip joint biomechanics [6], limb length disparity [7], and the necessity for revision surgeries. Consequently, there has been a burgeoning interest in devising methodologies that can enhance the precision of implant placement during THA.
To reduce incidence of complications due to component mal-positioning, technology was introduced to improve the accuracy and precision of acetabular component placement. The conventional manual manipulation of instruments persists as the most widely employed approach for implanting the acetabular component. Furthermore, various intraoperative anatomical landmarks have been identified to facilitate the secure placement of the acetabular cup [8]. With image-based robotic systems such as the mako (Mako Corp, Stryker), it is postulated that it is possible to accurately estimate femoral and acetabular component version, combined anteversion and the impingement profile after THA.
Robotic-assisted THA (RA-THA) has emerged as an alternative to the traditional manual technique, affording a more meticulous execution of the preoperative plan and superior radiological outcomes [9]. Several studies have investigated the disparities in radiological outcomes between robotic-assisted THA (RA-THA) and manual THA (mTHA) [10].
However, a consensus is lacking in the literature regarding the efficacy of robotic-assisted THR concerning radiological outcomes. While some studies have reported enhanced radiological outcomes with robotic-assisted THR, others have not. Additionally, the adoption of varying measurement parameters and safe zones for component orientation in these studies has impeded consistent comparison and interpretation of outcomes, posing a challenge in discerning the implications of these studies.
With the increasing prevalence of RA-THA [11], it becomes imperative to ascertain whether this technology can yield outcomes equivalent to or superior to those achieved with mTHA in terms of radiographic results. Thus, there arises a need for a study comparing the radiological outcomes of RA-THA to mTHA. The aim of this study was to compare radiological outcomes of component positioning with robotic versus manual total hip arthroplasty.
Methodology
Study Design, Setting and Data Collection
This study was a prospective cohort study of patients undergoing primary total hip arthroplasty, with either Mako robotic-assisted (RA-THA) or manual (M-THA) surgical technique, between January 2021 and December 2022 at a single high-volume arthroplasty centre. The reporting of this study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines. Institutional Ethical Board approval was obtained for this prospective cohort study (SIEC/2022/481). Patient demographic data, surgical data points (including component positioning in RA-THA) were collected prospectively from the institute joint registry and electronic health records. Radiological data were captured from the institute picture archiving and communication system (PACS).
Study Participants
This study included patients with end-stage arthritis of the hip secondary to any etiology (avascular necrosis of the hip, dysplasia, post-traumatic arthritis and inflammatory arthritis, consenting to undergo either manual or robotic total hip arthroplasty). Patients were counselled for both manual and robotic techniques, and they self-selected their preference. 212 consecutive patients underwent THA during the study period and were included in final analysis. 121 hips were operated with mako robotic technology (103 patients including 18 cases of bilateral THA). The manual THA cohort consisted of 130 hips (109 patients including 21 cases of bilateral THA). All surgeries were performed by a single surgeon via the posterior approach to the hip.
Preoperative Planning
Preoperative planning in robotic-assisted THA cases involved 3D CT-based surgical plans designed to adjust acetabular and femoral component positioning, with an aim to restore offset and leg length. In the manual THA group, routine 2D X-ray-based templating was done to estimate component size and placement to optimize offset restoration and length, with acetabular cup positioning based on limits of the safe zone described by Lewinnek et al. (inclination angle between 30 and 50° and anteversion angle between 5 and 25°) [12]. With the latest iteration of the mako hip software (Stryker, Mako Ver 4.0, Mahwah, New Jersey), it is possible for surgeons to adjust cup and stem anteversion to optimize combined anteversion, and also to evaluate impingement with virtual Range of motion assessment. Decisions on final anteversion and inclination are done based on surgeon preference to optimize all parameters. All cases were operated under combined spinal and epidural anaesthesia and received uncemented Stryker Accolade II femoral component and Trident uncemented acetabular components.
Radiographic Measurements
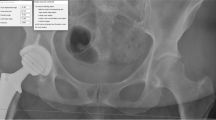
Post-operative radiographic measurements were conducted, on antero-posterior (AP) and cross-table lateral (CTL) views, obtained on the first day post-surgery. Follow-up radiographs were taken at one month and six months post-surgery, with measurements based on the one-month follow-up radiographs. Radiographs adhered to a standardized protocol. AP radiographs were taken with the X-ray beam centred over the pubic symphysis, maintaining a fixed distance of 1.2 m between the X-ray tube and the cassette. The inclination angle was defined as the angle between a tangent drawn to the face of the acetabulum and the inter-teardrop line [13]. CTL view was performed with the operated limb internally rotated by 15–20° in a supine position, aligning the X-ray beam at a 45-degree angle to the operated limb (Fig. 1).
All radiographic measurements were performed using the Bone Ninja Application (LifeBridge Health, Sinai Hospital of Baltimore, Inc) on iPad (Apple Inc.) [14]. Acetabular component anteversion angle was measured on CTL radiographs using the ischio-lateral method, which involved drawing a line perpendicular to the long axis of the ischial tuberosity and calculating the angle by drawing a tangent to the face of the acetabular cup [15]. Two independent observers randomly measured the radiographic angles to check interobserver reliability and reproducibility and the average two measurements were used for analysis. Both observers were blinded to the method of THA done as the type and company of implant used for both methods was identical. Final anteversion value was derived by the formula described by Pankaj A et al. [15] as follows: Anteversion value = (0.804 × ischio-lateral method anteversion) – 20.991. To assess implant placement accuracy, mean inclination and anteversion angles were calculated for each group, along with the identification of outliers, defined as cases with angles falling outside the "modified safe limits" as described by Callanan et al. (inclination angle between 30 and 45° and anteversion angle between 5 and 25°) as per study of Leslie et al. [5, 16].
Statistical Analysis
Continuous variables are presented as means with standard deviations. Categorical variables are presented as frequencies and percentages. Comparison of continuous variables (body mass index (BMI), and pre-operative functional scores which include WOMAC score, HHS, and Oxford Hip Score) was done using the independent samples t test or the Mann–Whitney U test based on the normality of data. The Pearson Chi-square test was used to evaluate the differences in categorical data. A significance level of p < 0.05 was set to determine statistically significant differences between the two groups for these parameters. In the RA-THA group, the paired t test was performed to compare the preoperative planned component positioning with the final implant positioning angles calculated by the robotic software after implantation, providing insight into the precision of the preoperative plan execution.
Inter-observer and intra-observer reliability for radiological measurements was assessed using the Cronbach's alpha test to ensure internal consistency and minimize observer bias. Additionally, odds ratios were calculated to measure the likelihood of an association between the surgical method and the desired outcome of achieving component positioning within defined safe limits.
Results
Patient Demographics
A total of 212 patients were eligible for final evaluation among which 121 hips were operated using MAKO robotic technology (103 patients including 18 cases of bilateral THA) and 130 hips (109 patients including 21 cases of bilateral THA) underwent conventional THA.
The demographics of the two patient groups are detailed in Table 1. The average age of the patients was 48.47 years (SD = 14.7), predominantly male (N = 124, 58.5%). The mean body mass index (BMI) was recorded as 26.67 (SD = 2.6). Demographic variables such as age, sex, BMI, side operated and ASA grade were all comparable.
Mean Pre-operative Harris Hip score (HHS) between the conventional cohort [58.98, SD-3.5] and robotic cohort [58.6, SD-3.3] were comparable.
Radiographic Measurements
Both the robotic and manual cohorts demonstrated high inter- and intra-observer reliability in measuring anteversion and inclination angles, as outlined in Table 2. This underscores the consistency in measurements and absence of observer bias.
Post-operative Inclination and Anteversion Angles
The mean post-operative inclination angles were 42.12 (SD = 4.9) and 40.51 (SD = 1.54) in the conventional and robotic THA cohort, respectively, which was found to be statistically significant with the robotic cohort showing greater precision in achieving the target value. However, the mean post-operative anteversion angles between the two cohorts did not exhibit any statistical difference. [Conventional: 24.9 (SD = 4.5) vs. Robotic: 24.55 (SD = 3.1) (Table 3) (Fig. 2).
Safe Zone Determination
According to the criteria established by Lewinnek et al. [12], we evaluated the proportion of hips within the safe zone (anteversion angles between 5 and 25° and inclination between 30 and 45°). A majority of the conventional THRs (n = 72, 55.4%) were placed outside the safe zone for anteversion, compared to the robotic THRs, which predominantly fell within it (n = 67, 55.4%) and the ones placed outside were mainly due to the functional positioning of the components. This difference, however, was not statistically significant, as depicted in Table 4 and Fig. 3. On the contrary, the inclination angles revealed a highly significant difference between the cohorts (p < 0.0001), with all the robotic THRs (N = 121, 100%) being placed within the safe zone for inclination, whereas only 70% (N = 91) of the conventional THRs were within the safe zone (Table 5) (Fig. 3).
Robotic Accuracy
The MAKO pre-plan, which allows surgeons to determine component positioning preoperatively based on spinopelvic parameters, virtual range of motion, and surgeon preference, was evaluated for its accuracy in robotic-assisted THRs (RA-THRs). A significant majority of the final RA-THRs (N = 112, 92.6%) adhered within 2° of the pre-plan for both inclination and anteversion. Furthermore, 97.5% of RA-THRs were within 3° of the proposed plan, demonstrating high accuracy, as presented in Fig. 4.
Discussion
This prospective study evaluated differences in component positioning between robotic and manual total hip arthroplasty. CT-based robotic technology showed a significantly higher accuracy for acetabular component inclination. However, there was no significant variation in cup anteversion with manual or robotic surgery. Robotic assisted THA was highly likely to match the CT-based surgical pre-plan with a significant majority of the final RA-THRs (92.6%) with radiological measurements within 2° of the pre-plan for both inclination and anteversion. Furthermore, 97.5% of RA-THRs were within 3° of the proposed plan.
Proper acetabular cup positioning in total hip arthroplasty (THA) is paramount for the durability of the prosthetic hip and implant stability, as component malposition can lead to complications such as dislocation [2], impingement [3], accelerated wear [4, 5], disturbed hip joint biomechanics [6], limb length discrepancy [7], and the need for revision surgeries. Recommended cup orientation ranges, with an inclination of 30–50° and anteversion of 0–30°, have been proposed in various studies [5, 12, 13, 16]. A widely used safe zone, as established by Lewinnek et al., suggests inclination between 30 and 50° and anteversion between 5 and 25° [12]. Callanan et al. proposed a modified safe zone (30–45° inclination and 5–25° anteversion) based on the findings of Leslie et al., highlighting increased wear and edge loading in abduction angles exceeding 45° [5, 16].
Robotic-assisted THA has demonstrated high accuracy in placing acetabular cups within safe zones, aligning with similar findings in studies comparing computer-assisted THA to conventional THA. For instance, Hohmann et al. [17] reported 76.7% of cups within the safe zone with navigation-assisted implantation compared to 20% with manual placement (p = 0.01). Similarly, Parratte and Argenson [18] found 20% outliers with imageless computer-assisted navigation compared to 57% outliers in the freehand group (p = 0.002). Kalteis et al. [19] reported only 3 of 23 cups placed outside the safe zone with navigation, compared to 11 of 22 in the conventional group (p = 0.003).
Callanan et al. [16] reported 47% of cups in their modified safe zone with conventional THA, while our study achieved better results with robotic technique, placing cups in 89.23% of patients with an inclination angle within 3° SD of the planned angle. Intraoperative determination of the 3-D pelvis position remains challenging due to factors like pelvic tilt, obesity, and hip flexion contracture. Various methods for intraoperative orientation, such as alignment jigs and landmarks, vary in accuracy. Robotic-assisted surgery improves cup placement accuracy but faces limited acceptance due to additional costs and operating room time.
Importantly, with increased research on spino-pelvic relationship, the Lewinnek safe zone is now not the universal standard for component positioning [20]. Although a safe target, component positioning has to be based on individual spino-pelvic relationship of the patient. With the Stryker Mako THA Version 4.0 software, it is now possible to assess bone-bone, component-bone or component-component impingement through virtual range of motion simulation [21]. This is the reason for variations in surgical pre-planned or proposed inclination or anteversion parameters in more recent studies on robotic THA.
This study had some potential limitations, including the exclusion of femoral anteversion and combine anteversion measurements, which are clinically relevant. Measuring femoral component anteversion requires a CT scan covering both hip and knee joints, entailing increased radiation exposure and additional costs. Despite this limitation, our study provides valuable insights into acetabular cup positioning accuracy.
This study had several strengths which include a prospective study design, with a single operating surgeon, and comparison of radiological measurements with both robotic and manual THA cohorts. Both the groups were comparable.
This study has shown the benefits of robotics in component positioning and superiority over conventional THA. However, future research should be directed on comparing the benefit of robotics in improving patient reported outcomes, dislocation rates and revision rates after THA to justify the additional costs of robotics in hip arthroplasty.
Conclusion
This study provides evidence that RATHA leads to better radiological outcomes as compared to mTHA. The study showed that RATHA is an accurate, reliable, and safe alternative to mTHA. The mean inclination angle was found to be significantly accurate in the robotic group as compared to the manual group. However, there was no difference in cup anteversion with either technique. The robotic group had a significantly lower number of outliers outside the safe zone as compared to the manual group.
Availability of Data and Material (Data Transparency)
Available.
Code Availability (Software Application or Custom Code)
Not applicable.
References
Sloan, M., Premkumar, A., & Sheth, N. P. (2018). Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. The Journal of Bone and Joint Surgery: American Volume, 100(17), 1455–1460. https://doi.org/10.2106/JBJS.17.01617
Ali-Khan, M. A., Brakenbury, P. H., & Reynolds, I. S. (1981). Dislocation following total hip replacement. The Journal of Bone and Joint Surgery: British Volume, 63-B(2), 214–218. https://doi.org/10.1302/0301-620X.63B2.7217144
Shon, W. Y., Baldini, T., Peterson, M. G., Wright, T. M., & Salvati, E. A. (2005). Impingement in total hip arthroplasty a study of retrieved acetabular components. The Journal of Arthroplasty, 20(4), 427–435. https://doi.org/10.1016/j.arth.2004.09.058
De Haan, R., Pattyn, C., Gill, H. S., Murray, D. W., Campbell, P. A., & De Smet, K. (2008). Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. The Journal of Bone and Joint Surgery: British Volume, 90(10), 1291–1297. https://doi.org/10.1302/0301-620X.90B10.20533
Leslie, I. J., Williams, S., Isaac, G., Ingham, E., & Fisher, J. (2009). High cup angle and microseparation increase the wear of hip surface replacements. Clinical Orthopaedics and Related Research, 467(9), 2259–2265. https://doi.org/10.1007/s11999-009-0830-x
Kennedy, J. G., Rogers, W. B., Soffe, K. E., Sullivan, R. J., Griffen, D. G., & Sheehan, L. J. (1998). Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. The Journal of Arthroplasty, 13(5), 530–534. https://doi.org/10.1016/s0883-5403(98)90052-3
Murphy, S. B., & Ecker, T. M. (2007). Evaluation of a new leg length measurement algorithm in hip arthroplasty. Clinical Orthopaedics and Related Research, 463, 85–89. https://doi.org/10.1097/BLO.0b013e318126c08f
Epstein, N. J., Woolson, S. T., & Giori, N. J. (2011). Acetabular component positioning using the transverse acetabular ligament: Can you find it and does it help? Clinical Orthopaedics and Related Research, 469(2), 412–416. https://doi.org/10.1007/s11999-010-1523-1
Pott, P. P., Scharf, H.-P., & Schwarz, M. L. R. (2005). Today’s state of the art in surgical robotics. Computer Aided Surgery: Official Journal of the International Society for Computer Aided Surgery, 10(2), 101–132. https://doi.org/10.3109/10929080500228753
Emara, A. K., Samuel, L. T., Acuña, A. J., Kuo, A., Khlopas, A., & Kamath, A. F. (2021). Robotic-arm assisted versus manual total hip arthroplasty: Systematic review and meta-analysis of radiographic accuracy. The International Journal of Medical Robotics Computer Assisted Surgery: MRCAS, 17(6), e2332. https://doi.org/10.1002/rcs.2332
Zheng, G., & Nolte, L. P. (2015). Computer-assisted orthopedic surgery: current state and future perspective. Frontiers in Surgery, 2, 66. https://doi.org/10.3389/fsurg.2015.00066
Lewinnek, G. E., Lewis, J. L., Tarr, R., Compere, C. L., & Zimmerman, J. R. (1978). Dislocations after total hip-replacement arthroplasties. The Journal of Bone and Joint Surgery: American Volume, 60(2), 217–220.
Murray, D. W. (1993). The definition and measurement of acetabular orientation. The Journal of Bone and Joint Surgery: British Volume, 75(2), 228–232. https://doi.org/10.1302/0301-620X.75B2.8444942
Jagadeesh, N., Kariya, A., Pammi, S., Shivalingappa, V. M., & Ramakrishna, C. (2022). Bone Ninja application is reliable alternative to PACS in measuring preoperative and postoperative alignment parameters of total knee arthroplasty. Journal of Orthopaedics, 34, 132–136. https://doi.org/10.1016/j.jor.2022.07.019
Pankaj, A., Mittal, A., & Chawla, A. (2017). The validity and reproducibility of cross table radiographs compared with CT scans for the measurement of anteversion of the acetabular component after total hip arthroplasty. The Bone & Joint Journal, 99-B(8), 1006–1011. https://doi.org/10.1302/0301-620X.99B8.BJJ-2016-1158.R2
Callanan, M. C., Jarrett, B., Bragdon, C. R., Zurakowski, D., Rubash, H. E., Freiberg, A. A., et al. (2011). The John Charnley Award: Risk factors for cup malpositioning—Quality improvement through a joint registry at a tertiary hospital. Clinical Orthopaedics and Related Research, 469(2), 319–329. https://doi.org/10.1007/s11999-010-1487-1
Hohmann, E., Bryant, A., & Tetsworth, K. (2011). A comparison between imageless navigated and manual freehand technique acetabular cup placement in total hip arthroplasty. The Journal of Arthroplasty, 26(7), 1078–1082. https://doi.org/10.1016/j.arth.2010.11.009
Parratte, S., & Argenson, J.-N.A. (2007). Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty: A prospective, randomized, controlled study. The Journal of Bone and Joint Surgery: American Volume, 89(3), 494–499. https://doi.org/10.2106/JBJS.F.00529
Kalteis, T., Handel, M., Herold, T., Perlick, L., Baethis, H., & Grifka, J. (2005). Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. International Orthopaedics, 29(5), 272–276. https://doi.org/10.1007/s00264-005-0671-5
Dorr, L. D., & Callaghan, J. J. (2019). Death of the Lewinnek “Safe Zone.” The Journal of Arthroplasty, 34(1), 1–2. https://doi.org/10.1016/j.arth.2018.10.035
Ogilvie, A., Kim, W. J., Asirvatham, R. D., Fontalis, A., Putzeys, P., & Haddad, F. S. (2022). Robotic-arm-assisted total hip arthroplasty: A review of the workflow, outcomes and its role in addressing the challenge of spinopelvic imbalance. Medicina (Kaunas, Lithuania), 58(11), 1616. https://doi.org/10.3390/medicina58111616
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
AA: conceptualization; writing—review and editing. PM: writing—original draft; methodology; formal analysis. TJ: writing—original draft; investigation; formal analysis. CS: investigation; formal analysis. VBNP: conceptualization; writing—review and editing. AVGR: manuscript editing, review and supervision.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical Approval
Obtained.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent to Participate
Obtained.
Consent to Publish
Obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Annapareddy, A., Mulpur, P., Jayakumar, T. et al. A Radiological Comparison of Robotic-Assisted Versus Manual Techniques in Total Hip Arthroplasty. JOIO (2024). https://doi.org/10.1007/s43465-024-01232-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43465-024-01232-1