Abstract
Background
Several studies have reported that the transverse acetabular ligament (TAL) can be used to orient the acetabular component during total hip arthroplasty and that it can be identified in nearly all patients.
Questions/purposes
We attempted to determine how often the TAL could be identified during primary THA and its accuracy as a guide for acetabular component positioning.
Methods
In a prospective series of 63 patients (64 hips) undergoing primary THA, two surgeons attempted to identify the TAL and, if it was found, to use it for acetabular component orientation. Patients in whom the TAL was identified served as the study group and the ligament was used for cup orientation in those patients; the remaining patients in whom the ligament could not be identified served as a control group and had free-hand cup positioning. Anteversion was determined by radiographic measurement from true lateral views.
Results
The TAL was identified in only 30 hips (47%) and was more likely to be found in patients who did not have inferior acetabular osteophytes. Acetabular position was not improved using this ligament for reference.
Conclusions
The TAL could not be routinely identified at surgery and when used for cup orientation it was no more accurate for cup positioning than free-hand technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetabular malposition is recognized as a risk factor for dislocation [4, 6, 7] and increased wear [5, 8, 10] after total hip arthroplasty (THA), both of which may contribute to implant failure. Increased rates of dislocation have been associated with acetabular components placed outside the most commonly quoted “safe zones” of 5° to 25° of anteversion and 30° to 50° of abduction [3, 9]. The transverse acetabular ligament (TAL) has been reported to provide an anatomic landmark for referencing acetabular orientation during THA by several authors. Archbold et al. [1] identified the TAL in 99.7% of 1000 consecutive THAs despite the ligament being obscured by soft tissue or osteophytes in 50% of the cases. These authors used the TAL to guide acetabular reaming and positioning and noted a 0.6% postoperative dislocation rate; however, no radiographic measurements of acetabular component orientation were reported. Prior to beginning this study we believed that the ability to identify this ligament in more than 99% of arthritic hips was unlikely.
More recently, these same authors examined the orientation of the TAL in MRI studies of nonarthritic hips and found it to lie within 5.3° to 36.1° of version in the sagittal plane [2]. Acetabular component position was within the “safe zone” in 14 of 14 hips using the TAL as a guide in cadaveric specimens [11]. However, it is unclear whether using the TAL for a reference point during primary THA improves radiographic acetabular component orientation, since no clinical measurements have been reported.
Therefore, we prospectively studied a series of primary THA patients to determine the percentage of hips in which the TAL could be positively identified during primary THA. Furthermore, we compared radiographic acetabular component orientation in patients in whom the cup was positioned using the TAL to a control group in whom standard positioners were used.
Patients and Methods
In a prospective study of all 63 patients (64 hips) who underwent primary THA by two surgeons (STW and NJG) at one hospital from March 2008 to February 2009, we carefully attempted to identify the TAL and, if found, it was used as a reference landmark to judge acetabular component orientation. The control group was comprised of patients in whom the TAL could not be identified. In this group, standard free-hand techniques were used to position the acetabular component. Postoperative AP and crosstable lateral radiographs were obtained and acetabular component orientation was compared between the two groups. We retrospectively reviewed the charts to collect demographic data. There were 59 male and four female patients whose mean age was 64 years and whose average height, weight, and body mass index were 176 cm, 97 kg, and 31, respectively. Thirty-eight (59%) of the hips were right, and the preoperative diagnosis was osteoarthritis in 49 (77%), osteonecrosis in five (8%), congenital dysplasia in three (5%), and miscellaneous conditions in the remaining seven (11%) hips. All of the patients were followed for a minimum of three months. Approval for the study was obtained from our institutional review board.
Two fellowship-trained surgeons performed all of these procedures at a Veteran’s Administration hospital and orthopaedic residents participated in all of the cases. All implants were cementless using porous-coated metal-backed acetabular components with polyethylene liners and porous-coated femoral components from two manufacturers. One surgeon used all neutral liners and the other used a 10 degree elevated lip liner in 10 of 34 cases. A posterolateral approach was used for all procedures. Inferior acetabular osteophytes were identified on all preoperative radiographs and confirmed intraoperatively by the surgeon.
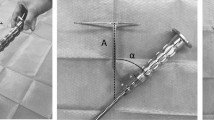
All patients had a posterolateral approach with the patient in the lateral decubitus position with the pelvis stabilized with a standard pelvic holding device. A cobra retractor was placed over the anterior lip of the acetabulum to retract the femur forward. Another cobra retractor was placed at the inferior aspect of the acetabulum to expose the TAL or any inferior osteophytes. Removal of osteophytes or soft tissue obscuring the inferior portion of the socket was performed carefully in order not to disrupt this ligament. However, in many cases, the TAL could not be positively identified despite careful dissection. In patients in whom the TAL could be identified at surgery, the surgeon attempted to position the acetabular component in anteversion so that the inferior rim of the cup was parallel to the TAL and just below it as recommended by Archbold et al. [1] for the correct depth and abduction angle. If the TAL was not identified, the surgeon tried to position the acetabular component in 45° of abduction and 20° of anteversion with a free-hand positioning instrument supplied by the manufacturer of the implant being used. Each surgeon attempted to position the patients’ pelvis with the stabilizer so that utilization of a standard acetabular positioning guide would be as accurate as possible. The pelvic stabilizer pads (Stuhlberg, Innomed, Inc., Savannah, GA) were placed on the sacrum and on either the pubic symphysis or both anterior superior iliac spines with the coronal plane of the pelvis perpendicular to the floor. If there were no anterior or posterior acetabular rim osteophytes present, the anatomical rim of the socket was also used for orientation.
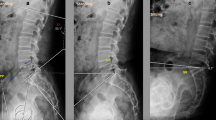
Each patient had a postoperative AP radiograph of the pelvis used to measure the abduction angle of the cup from lines drawn through the face of the cup and the interteardrop line. Abduction angles that were 30° or less or 50° or more were classified as outliers from the “safe zone”. A standardized crosstable true lateral view of the hip was taken with the patient supine on the radiographic table with the contralateral lower extremity flexed as much as possible to eliminate lumbar lordosis and place the pelvis in a standard position. The film cassette was placed parallel to the radiographic table and the x-ray beam was directed from the medial proximal thigh laterally. All but two patients (two hips, 3%) had a crosstable lateral view of the hip. The anteversion angle of the acetabular component was measured according to the technique of Woo and Morrey [12] by one of us (NJE) who did not participate in any of the procedures and who was blinded to whether the TAL had been identified or not. Both surgeons attempted to place the acetabular component at 20 degrees of anteversion, since they believed the “safe zone” (proposed by Lewinnek et al. [9]) should be at an anteversion range of 10 to 30 degrees to protect against posterior dislocation rather than in a range from 5 to 25 degrees. However, we used the “safe zone” (> 5 or < 25 degrees [9]) to define anteversion outliers in our analysis of results. The femoral component was anteverted by 15 degrees.
Patients were followed clinically for a minimum of three months to determine the incidence of early postoperative dislocation.
We determined the differences in patient demographic characteristics and in radiographic acetabular positioning in the coronal and sagittal planes between groups using the Student’s t test with 95% confidence intervals and for nominal variables using Chi square analysis. Statistical analysis was performed using Statworks from Abacus Concepts, Inc. (Berkeley, CA).
Results
The TAL was identified in 30 patients (30 hips [47%]) (the TAL group), but could not be found in 33 patients (34 hips) (the control group). There were strong trends for patients in the TAL group to be shorter and to weigh less than the control group, although there was no difference in the average body mass index between groups (Table 1). The average abduction angle and number of hips that were outliers for abduction were similar between groups (Table 2). Although there was a strong trend in the difference in the mean anteversion angle between groups (p = 0.0586), there was no statistical difference between the number of cup outliers for anteversion between groups. However, there were 19% more cup outliers in acetabular components implanted by free-hand positioning than in the TAL group and studying larger numbers of patients may have resulted in a statistical difference favoring using the TAL for orientation. More control patients had inferior acetabular osteophytes seen on the preoperative radiographs and intraoperatively (Table 2).
One surgeon was more successful (p = 0.01) in identifying the TAL in his patients than the other surgeon: 19 of 30 hips (63%) versus 11 of 34 hips (32%) (Table 3). There was no difference between the surgeons regarding the percentage of their patients with hips that were outliers for abduction; however, one surgeon had fewer anteversion outliers (p = 0.042). Considering each surgeon’s results separately in using the TAL for positioning, neither surgeon had fewer abduction or anteversion outliers when using the TAL for positioning. There was no difference in the comparison of demographic characteristics in patients operated on by each surgeon.
None of the patients studied sustained a postoperative dislocation during this short followup period.
Discussion
Acetabular positioning remains a challenge in THA. Several published studies have recommended the use of the TAL for acetabular component positioning (1, 2, 11). One of these studies reported that the senior author was able to identify the TAL in virtually all primary THA patients despite obscuring soft tissue or inferior acetabular osteophytes. However, none of these studies reported the results of acetabular positioning in THA patients by measuring cup abduction or anteversion from postoperative radiographs. We attempted to confirm this author’s extraordinary success in these studies in identifying the TAL by prospectively trying to visualize the TAL in a series of patients undergoing primary THA. We also determined the radiographic results of using the ligament as a guide for acetabular component positioning and compared this result with a concurrent control group in whom the ligament could not be identified and in whom standard acetabular component positioners and pelvic stabilizers were used.
We recognize some limitations of our study. First, the anteversion angle was measured from a crosstable true lateral view of the hip rather than from CT scans. However, all of these lateral radiographs were standardized and this technique has been used for these measurements in many previous studies. Since both groups had the same measurement technique, any error in this measurement would not have affected the statistical results. Also, the expense of obtaining CT scans for this group of patients was prohibitive in this clinical setting. Secondly, we made comparisons of acetabular component alignment between the two groups, but assignment to the TAL or the control group was not randomized, as it was based on whether the TAL could be identified or not. We did not randomize patients to either of these two groups, since prior studies have implied improvement of acetabular positioning when the TAL is used and we believed that using standard positioners to orient the cup in patients who had an identifiable TAL could be interpreted as unethical.
We were able to identify the TAL during primary THA in only 47% of these hips. This appeared to be largely dependent on whether there were inferior acetabular osteophytes. We are unsure of why one surgeon was more successful in identifying the ligament than the other one. Osteophytes located at the inferior aspect of the acetabulum were present in 50% (32 of 64) of the hips, which was consistent with the findings of Archbold et al. [1] in their study of 1000 hips. In our experience with patients who had inferior osteophytes, the TAL could be identified in only 31% (10 of 32 hips) of the procedures compared to 62% (20 of 32 hips) in hips without inferior osteophytes (p = 0.01). The surgeons in our study were much less successful in removing these osteophytes to expose the TAL than was the senior surgeon in the study of Archbold et al. [1]. We believe, however, in general practice this ligament cannot realistically be identified as often as was reported by Archbold et al. (99.7%) [1]. The TAL appeared to be more easily identified in patients who were shorter and weighed less, a finding that was not unexpected. It is possible that the differences seen in the two groups are simply due to the differences in these patients’ height, weight, or severity of arthritis.
We were unable to conclude that the TAL was a helpful guide in orienting the acetabular component in appropriate anteversion, since there was no difference in the number of outliers using the ligament than without with respect to anteversion. This result may have been different if larger numbers of patients had been studied, as the TAL reduced the number of anteversion outliers by 19%. For our entire series of 64 hips we found that acetabular components were more likely to be oriented out of the “safe zone” with respect to anteversion than abduction (50% versus 14%). In our experience standard pelvic positioners used to stabilize the patient during THA from a posterior approach can prove inadequate in preventing rotation of the pelvis in the coronal plane during retraction of the femur during acetabular exposure. Rotation of the pelvis in the coronal plane will result in inaccurate sagittal plane assessment and can affect abduction as well.
Given emerging evidence supporting the utility of the TAL in THA, we believe this study represents the results that can be expected in the hands of an arthroplasty surgeon who is beginning to incorporate the use of the TAL into his or her surgical practice. Such a surgeon may expect to identify the TAL in approximately 30 to 60% of their cases, and in those cases, when the ligament is used to orient the acetabular component in anteversion, the radiographic results are comparable but no better than from the use of standard positioning guides.
References
Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br. 2006;88:883–886.
Archbold HA, Slomczykowski M, Crone M, Eckman K, Jaramaz B, Beverland DE. The relationship of the orientation of the transverse acetabular ligament and acetabular labrum to the suggested safe zones of cup positioning in total hip arthroplasty. Hip Int. 2008;18:1–6.
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769.
Coventry MB, Beckenbaugh RD, Nolan DR, Ilstrup DM. 2,012 total hip arthroplasties: a study of postoperative course and early complications. J Bone Joint Surg Am. 1974;56:273–284.
Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis: factors influencing generation of polyethylene debris. J Arthroplasty. 1997;12:256–266.
Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop Relat Res. 1980;151:169–178.
Hedlunch U, Fredin H. Patient characteristics in dislocations after primary total hip arthroplasty: 60 patients compared with a control group. Acta Orthop Scand. 1995;66:225–228.
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220.
Patil S, Bergula A, Chen PC, Colwell CW Jr, D’Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85(Suppl 4):56–63.
Pearce CJ, Sexton SA, Davies DC, Khaleel A. The transverse acetabular ligament may be used to align the acetabular cup in total hip arthroplasty. Hip Int. 2008;18:7–10.
Woo RY, Morrey BF. Dislocation after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that the IRB waived each participants consent for participation in the study.
This work was performed at Palo Alto Veteran’s Administration Hospital.
About this article
Cite this article
Epstein, N.J., Woolson, S.T. & Giori, N.J. Acetabular Component Positioning Using the Transverse Acetabular Ligament: Can You Find It and Does It Help?. Clin Orthop Relat Res 469, 412–416 (2011). https://doi.org/10.1007/s11999-010-1523-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1523-1