Abstract
Background
In bone tissue engineering segment, numerous approaches have been investigated to address critically sized bone defects via 3D scaffolds, as the amount of autologous bone grafts are limited, accompanied with complications on harvesting. Moreover, the use of bone-marrow-derived stem cells is also a limiting factor owing to the invasive procedures involved and the low yield of stem cells. Hence, research is ongoing on the search for an ideal bone graft system promoting bone growth and regeneration.
Purpose of the Study
This study aims to develop a unique platform for tissue development via stem cell differentiation towards an osteogenic phenotype providing optimum biological cues for cell adhesion, differentiation and proliferation using biomimetic gelatin-based scaffolds. The use of adipose-derived mesenchymal stem cells in this study also offers an ideal approach for the development of an autologous bone graft.
Methods
A gelatin-vinyl acetate-based 3D scaffold system incorporating Bioglass was developed and the osteogenic differentiation of adipose-derived mesenchymal stem cells (ADMSCs) on the highly porous freeze-dried gelatin-vinyl acetate/ Bioglass scaffold (GB) system was analyzed. The physicochemical properties, cell proliferation and viability were investigated by seeding rat adipose tissue-derived mesenchymal stem cells (ADSCs) onto the scaffolds. The osteogenic differentiation potential of the ADMSC seeded GeVAc/bioglass system was assessed using calcium deposition assay and bone-related protein and genes and comparing with the 3D Gelatin vinyl acetate coppolymer (GeVAc) constructs.
Results and Conclusion
According to the findings, the 3D porous GeVAc/bioglass scaffold can be considered as a promising matrix for bone tissue regeneration and the 3D architecture supports the differentiation of the ADMSCs into osteoblast cells and enhances the production of mineralized bone matrix.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autologous bone grafts have been used to replace diseased or compromised bone tissue owing to their osteogenic, osteoconductive and osteoinductive capabilities. However, due to limited availability, donor site morbidity and persistent pain, alternatives via tissue engineering strategies are being explored, that includes, use of 3D scaffolds in the form of biopolymeric grafts [1,2,3]. These grafts include biodegradable polymer systems both of synthetic and natural origin, ceramics and metals. The natural polymers such as Gelatin have been of special interest owing to its unique biocompatibility. The osteogencity of these graft materials is explored by seeding with osteoprogenitor cells and analysed for their osteogenic differentiation and proliferation [4,5,6]. For the regeneration of osseous tissues, numerous 3D gelatin-based scaffolds and different composites have been developed [7]. Among the cell sources used, bone-marrow mesenchymal stem cells (BMSCs) have been the most extensively used [8, 9]. However, owing to the issues with harvesting BMSCs associated with the bone-marrow aspiration procedure and the limited number of MSCs obtained (0.001–0.01%) from the harvested tissue, and the cell senescence observed during expansion, alternative cell sources have been explored [10]. This has led to the emerging use of adipose-derived stem cells (ASCs) owing to the ease of isolation through a minimally invasive procedure and acquiring the adequate cell population [11].
In this study, we compared the osteogenic differentiation potential of adipose-derived mesenchymal stem cells in a gelatin-based scaffold system that is incorporated with bioglass. This study enabled us to understand how a biomimetic gelatin-based scaffold system promotes the osteogenic differentiation of ADMSCs without any growth factors induced. The 3D interconnected porous structure was fabricated via freeze drying process and the biodegradation, mechanical properties and cytocompatibility were assessed. We hypothesized that the incorporation of bioglass into the gelatin-vinyl acetate polymer could promote the differentiation of adipose-derived mesenchymal stem cells to osteogenic lineage which was assessed through functional assays and gene expression analysis. In addition, the physicochemical characteristics of the scaffolds were assessed. The system served as an ideal bone autograft that helped to promote the differentiation of the seeded stem cells towards an osteogenic lineage.
Methodology
Gelatin and vinyl acetate monomer was procured from Sigma Merck, India. Dulbecco’s modified essential medium–low glucose (DMEM-LG), foetal bovine serum (FBS), phosphate buffered saline (PBS), antibiotic–antimycotic (AB-AM), and 0.25% trypsin–EDTA (Invitrogen, USA), osteogenic differentiation medium composition (0.1 µM dexamethasone, 10 mM sodium β-glycerophosphate, and 0.05 mM ascorbic acid-2-phosphate) (Merck Sigma), Calcium colorimetric assay kit (Merck Sigma), Collagenase Type 2 (Invitrogen) and live dead assay kit (Invitrogen) was used for the study. 4% Paraformaldehyde were used for fixing samples for SEM analysis, DNA Diluent (HiMedia, India) for RNA isolation, cDNA kit (Applied Biosytems™) for cDNA synthesis, PowerUP SYBR green master mix (Applied Biosytems™) for RT PCR. All other reagents used were of analytical grade or procured locally. The rat adipose mesenchymal stem cells used for the study were isolated after obtaining the Institutional Animal Ethical Clearance (IAEC). All institutional and national guidelines for the care and use of laboratory animals were followed.
Preparation of Freeze-Dried GeVAc and Bioglass-Loaded GeVAc Scaffold
Gelatin-vinyl acetate (GeVAc) was synthesized as described in our earlier study [12]. GeVac bare scaffolds and GeVac incorporating bioglass that was synthesized through a sol–gel process, (designated as GB) was fabricated using a lyophilisation technique. For preparing the porous scaffolds, GeVAc (10%, w/v) and Bioglass (1% w/w) was dissolved in distilled water and subjected to high-speed stirring at 1500 rpm for 1 h. The foamed gelatin co-polymer was poured into the cylindrical mould, frozen and lyophilized to obtain porous cylinders which are then cut into small discs of diameter 3 mm and thickness 1.5 mm. The discs were then cross-linked using 1-ethyl-3-[3-dimethylaminopropyl] carbodiimide hydrochloride (EDC) and washed several times with water to remove traces of unreacted compounds. The discs were further lyophilised, packed and EtO sterilised.
Fourier Transform Infrared Spectroscopy Analysis
The reaction protocol was confirmed using Fourier transform infrared spectroscopy (FT-IR) which provides information about the specific chemical groups of the materials. FT-IR spectrum of 3 mm thickness sample was recorded at room temperature in the range of 5000–500 cm−1 region using BRUKER optic FTIR, GmbH.
Swelling Study
The study was performed to understand the water holding capacity and stability of the scaffold. For this study, freeze dried scaffolds were immersed in PBS and kept in pre-weighed containers for known intervals of time. The samples were withdrawn at regular intervals and wet weight measured. The % Swelling was calculated as per the equation:
Degradation Study
Biodegradation of the scaffolds was assessed via immersion in PBS (pH = 7.4) at 37 °C for a period of 28 days. At 7, 14, 21 and 28 days, the samples were removed from the solution, washed with double distilled water, frozen and lyophilized. Finally, the samples’ dry weight (Wd) after degradation was calculated, and the percentage of biodegradation was measured using the equation:
Compressive Mechanical Properties of the Developed Freeze-Dried Scaffolds
The compressive modulus of the GeVAc and Bioglass-loaded GeVAc (GB) scaffolds was evaluated using Instron Series 3365. The dry samples were tested with a 5kN load cell at 1 mm/min and the wet samples (incubated in PBS for 4 h) was tested with a 10N Load cell at 10 mm/min. Cylindrical samples (n = 4) with height twice that of the diameter was used for testing. The samples were compressed at the said speeds to half height and at this point maximum load and modulus is measured.
Cytotoxicity Analysis
Direct Contact Assay
To determine the cytocompatibility of the scaffold, L929 mouse fibroblast cells were seeded onto a 6 well plate. Once the cells reached 75% confluence, scaffolds (GeVac and GB) were placed on the monolayer of cells and observed after 24 h in direct contact. Cells grown on a culture plate without any scaffolds were taken as control. Images were taken using phase contrast microscope (Olympus1X71). The cells were incubated with test samples and controls at 37 ± l °C for 24 h, and then examined microscopically for cellular response which were scored as 0, l, 2, 3 and 4 based on the following observations as shown in Table 1.
Test on Extract (MTT Assay)
To evaluate the viability of cells, MTT assay was performed. L929 mouse fibroblast cells were seeded on to a 96 well plate at a density of about (1 × 102 cells per well) and was incubated for 24 h at 37 °C with 5% CO2. GeVac and GB scaffolds were kept in extraction medium (DMEM) at 37 °C for 24 h. 100% and 50% of extracts was added to the wells. Cells incubated with DMEM alone were kept as the control. After 24 h of incubation, the extract was removed and incubated with 20 μl of 10 mg/ml MTT reagent for 3 h. Then MTT was completely discarded and each well was dissolved in 100 μl DMSO to solubilise the formazan crystals formed and was kept in dark for 10–20 min. Optical density was measured at 530 nm with the use of ASYS UVM 340. Percentage viability of cells was calculated by:
Isolation of Rat MSCs
Rat adipose mesenchymal stem cells were isolated after obtaining institutional animal ethical clearance and Stem cell clearance. Adipose MSCs were isolated from the scapular region of rats. The isolated MSCs were cultured in DMEM (Dulbecco’s Modified Eagle Medium) containing 2%(v/v) fetal bovine serum (FBS), 1% (v/v) AB-AM and 3.7 gm Sodium Bicarbonate (NaHCO3) under a humidified atmosphere of 5% CO2 at 37 °C. Fresh culture medium was added every 2–3 days. Once the cells reached about 90% confluence (in 10 days), the P0 cells were digested with 0.25% trypsin–EDTA solution, centrifuged and pellets were flushed using a fresh medium. Then the cells were transferred into new T25 flasks. Cells from passages P2 and P3 were used for further studies.
Characterisation of the Isolated Mesenchymal Stem Cells
Confirmation and morphological studies of isolated MSC were done by immunostaining methods. MSCs were seeded in a 24-well plate, followed by fixation in 4% paraformaldehyde for 15 min and stored in 2 ml PBS. Permeation was done with 50% methanol for 1 h. After incubation with 0.5% BSA for 30 min at room temperature, the cells were treated with primary antibodies (1:50 dilution) for 2 h at room temperature. The positive stem cell markers studied included Vimentin, Endoglin and CD-90 (Santa Cruz Biotechnology) and negative marker used was CD-34 (Santa cruz Biotechnology). Following washing using PBS, a secondary PE-labelled antibody (1:50 dilution) was supplemented and incubated for 1 h at room temperature away from the light. The cells were washed with PBS and stained with nuclear stain 4′,6-diamidino-2-phenylindole (DAPI) for 15 min. Subsequently, images were viewed using an inverted fluorescence microscope (OLYMPUS IX-71S1F3).
Trilineage Differentiation
Trilineage differentiation of Mesenchymal Stem Cells (MSCs) into Osteocytes, Adipocytes and Chondrocytes was carried out by culturing the cells in a 6-well plate and providing the specific induction medium. At the end of the culture periods, the cells were rinsed in PBS and fixed in 4% paraformaldehyde. The trilineage differentiation was confirmed on performing the specific staining for the different lineages.
Biological Assays
Differentiation Study
Osteogenic Differentiation
The scaffolds seeded with rat ADMSCs were cultured in osteogenic differentiation medium (DMEM-LG with 1% FBS, 1% AB–AM, 0.1 µM dexamethasone, 10 mM sodium β-glycerophosphate, and 0.05 mM ascorbic acid-2-phosphate) to evaluate the induction potential. The cells were retrieved on 7th, 14th and 28th day of differentiation for various analysis. ADMSCs alone cultured in HG-DMEM were taken as the control for the whole study.
Viability Assays
Live Dead Assay
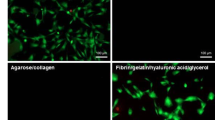
The adipose MSC cell viability and the pattern of growth at different periods of time assessed using live dead assay kit (Invitrogen). Scaffolds after 28 days were treated for 15 min in the dark with 4 mM calcein and 2 mM ethidium homodimer (in DMEM). The samples were then rinsed in PBS and examined using a Confocal microscope (Olympus). Live cells fluoresced green with calcein, while dead cells fluoresced red with ethidium homodimer.
Morphology of ADMSC During Differentiation
The morphology of adipose-derived mesenchymal stem cells during differentiation on GeVac and GB scaffolds were analysed using scanning electron microscopy (JEOL JSM 6390LV, Japan) on day 14 and day 28. Scaffolds were fixed in 4% paraformaldehyde and kept for 15 min incubation at 27 °C followed by PBS washing. Dehydration was given in graded alcohol (10–100%) for 15 min each, followed by critical point drying and gold sputter coating.
Functional Assays
Calcium Colorimetric Assay
In vitro mineralization on scaffolds (GeVac and GB), suggestive of the differentiation of ADMSCs to osteoblast was quantified by Calcium assay using calcium colorimetric assay kit (Sigma-Aldrich, USA). Scaffolds were retrieved after 7, 14 and 28 days. The absorbance of the standard and test sample was measured in a microplate spectrophotometer at 575 nm against the blank samples using fluorescent plate reader (Synergy H1 Microplate reader).
DNA Quantification
Assessment of DNA content in constructs and their proliferation at 7-, 14- and 28-day time period was performed using a fluorometric dye assay. Triplicate samples were used for the study. The samples were washed with PBS and frozen at −20 °C for storage. For analysis, samples were lyophilized for 4–8 h, and then digested in Proteinase K (Sigma Chemical Co.) lyses buffer at 55 °C for 12–16 h until complete dissolution of the construct had occurred. Samples were mixed well and diluted if necessary and were then loaded in triplicate into Microfluor 96-well plates (Dynex Technologies, Chantilly, VA). Blanks and a series of DNA standards (Sigma Chemical Co) were also loaded, and Hoechst 33258 dye solution (Sigma) was added to each well. The plate was allowed to incubate in the dark at room temperature for 15 min. Fluorescence was measured on a plate reader (Synergy H1 Microplate reader) at 25 °C using an excitation wavelength of 360 nm and an emission wavelength of 460 nm. The blank readings were subtracted from all samples and the cell and DNA standards were used to calculate the DNA concentration in the initial samples.
Gene Expression Analysis of Osteogenic Markers Using RT-PCR
After retrieving the scaffolds on 14th and 28th day of culture period, total RNA was extracted using Trizol reagent (Invitrogen) according to the manufacturer’s protocol. The RNA pellet was diluted with RNAse-free water, and RNA concentration was measured using the Nanodrop Spectrophotometer. cDNA was synthesized using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems) using a PCR thermal cycler, and real-time reverse transcription polymerase chain reaction was performed using the Analytik Jena RT-PCR system (Germany) with PowerUp™ SYBR™ green master mix(Applied Biosystems).The protocol included 95 °C for 30 s, followed by 40 cycles of 95 °C for 5 s, 60 °C for 30 s, and dissociation (95 °C for 15 s, 60 °C for 30 s, and 95 °C for 15 s). The osteogenic markers assessed included RUNX2, COL1A2, SOX9 and ALP with GAPDH as the housekeeping gene. The relative expression level of each target gene was then calculated using the 2−ΔΔCt method. The PCR primer sequences used are listed in Table 2.
Statistical Analysis
The results are presented as mean ± standard deviation (SD). Statistical analysis was performed using standard T- test. The results were considered significant at a p value of < 0.05.
Results and Discussion
Analysis of the Freeze Dried GeVAc and GB Scaffolds
Bone is composed of both organic and inorganic phases. The mechanical strength and durability of the bone is a result of the organization of both organic and inorganic phases. Based on the structure the bones are classified into trabecular and cortical. The two pathways through which bone formation occurs are endochondral ossification or intramembranous ossification [13, 14]. The two different cell types, osteoblast and osteoclast are responsible for the dynamic remodelling of bone, and they mediate the building of bone and remodelling of bone respectively [15]. The bone regeneration is not possible to repair the injured bone without external support, it can be either implanted bone or a substitute biomaterial [16]. The success of a TE construct depends on three main factors known as tissue engineering triad: selection of cells, a biomaterial scaffold and presence of cell signals that mediate and coordinate to recreate the tissue [17]. The tissue generated depends upon the cells used, the scaffold acts as a carrier and the bioactive components are responsible for the cell proliferation [18]. The scaffolds used in osteochondral reconstruction should be osteoinductive, meaning they should promote the maturation of progenitor cells into bone and cartilage [19].
Biodegradable polymers are used as scaffolds, which can either be synthetic or natural. Composition of polymers can also be customised due to their flexible design, structure and chemical composition [20]. Gelatin is a naturally occurring biopolymer that is made from animal collagen found in skin, bones, and tendons and is either partially hydrolysed in acid (Gelatin type A) or alkaline (Gelatin type B) [21]. For the regeneration of osseous tissues, numerous 3D gelatin-based prototypes and different composites have been explored [22]. Gelatin-vinyl acetate and Bioglass loaded Gelatin vinyl acetate was synthesised and fabricated into 3D porous scaffolds using freeze drying technique. The synthesis and fabrication were confirmed using ATR–FTIR technique. Figure 1a shows the ATR–FTIR spectra of the gelatin-vinyl acetate and Fig. 1 b shows the spectra of gelatin-vinyl acetate–bioglass polymer. Strong absorption peak groups appear at 1630 cm−1 and 1530 cm-1, respectively which are attributed to the amide I and amide II peaks of the gelatin structure. The intense C–O stretch at 1018 cm−1 in the spectrum, clearly indicates presence of ester carbonyl group of vinyl acetate moiety, indicating that grafting of synthetic polymers onto Gelatin has been achieved. The intense –CH2 peaks at 2924 cm−1 and that at 2856 cm−1 also confirms the copolymerization of vinyl acetate onto Gelatin. Moreover, blending with bioglass is evidenced from the peak at 1032 cm−1 and that at 820 cm−1 shows the characteristic peaks attributed to PO4 and Si–O–Si bonds and the symmetric stretch of P–O bond at PO43− at 614 cm−1.
Swelling Study
The interconnected porous structure is a promising characteristic for cell colonization rate, nutrient perfusion, and functionality of the tissue-engineered construct [23, 24]. Porosity, pore interconnectivity, pore architecture, that is, pore shape, size, distribution, and orientation also affect the mechanical properties and degradation rate of the scaffolds [25].
The swelling study gives an idea of the swelling rate of the scaffold when it is seeded with cells and brought into contact with media. The swelling rate of GeVac (Fig. 1c) within 5 min was seen to be less than 1000% which equilibriates to about 1400% in 120 min. In the case of the Bioglass incorporated GeVAc (GB) scaffold, in the first 5 min, a higher swelling rate is attained i.e. around 1300% which equilibriates within 30 min. A higher swelling rate of GB scaffold may be attributed to the decrease in the crosslinking density due to the presence of bioglass in the scaffold matrix.
Degradation Assay
Degradation assay was used to determine the stability of the scaffold construct (Fig. 1d). The GeVac construct was seen to have a degradation rate of about 45.1 ± 5.03% in 1 week timepoint. However, a higher mass loss of 63.8 ± 7.05% was observed for GB in 1 week due to the lower crosslinking induced by bioglass which was incorporated into the system. However, in the following weeks not much increase in the degradation rate was observed. This may be due to the process of biomineralization happening within the system after a period of 1 week. The biomineralization was also confirmed via SEM imaging to substantiate the above findings (Fig. 5d, f, h).
Mechanical Testing
In a study conducted by Madihally and Mattew the influence of porous structure on tensile testing of hydrated porous and nonporous membranes was evaluated [26]. The results obtained in their study revealed that elastic moduli of porous membrane are tenfold lower than those of nonporous membrane. In our study, the compression-based mechanical testing was performed on the GeVAc and GB samples in both dry and wet forms. The results showed that the GB scaffold had more compression mechanical strength when compared to the GeVAc scaffold in both the dry and wet state (Table 3). GB had a compressive strength of 0.45 ± 0.045 MPA when compared to the 0.35 ± 0.019 MPa exhibited by the GeVAc construct. The modulus was also higher for the GB construct (4.33 ± 1.70 MPa) when compared to the GeVAc construct (3.49 ± 0.77 MPa) in the dry as well as in the wet state. This may be due to the presence of Bioglass that may contribute to the higher compressive strength.
Cytotoxicity Analysis
Direct Contact Assay
Direct contact test is a primary in-vitro cell cytotoxicity assay, performed to show an initial confirmation that the scaffold does not elicit any harmful effects on the cell viability. The scaffolds were placed on a monolayer of L929 fibroblast cells for 24 h (Fig. 2). It was observed that both the scaffolds GeVAc and GB, did not elicit any harmful leachants and the cells maintained their characteristic spindle shaped morphology and hence the scaffolds are non-cytotoxic. The cells were well spread like the blank control cells incubated with media alone.
a Microscopic images of blank L929 fibroblast cells. b Cells in direct contact with GeVAc; c Cells in direct contact with GB; d Positive control: Polyvinyl chloride, e Negative Control: High molecular weight polyethylene. Scale bar: 50 μm; f Assessment of mitochondrial activity by MTT assay on treatment with extracts (50% and 100% w/v)
Test on Extract (MTT ASSAY)
To ascertain the viability of the L929 cells an indirect assay was also performed where media extracts were taken after incubating the media with scaffolds for 24 h (Fig. 2f). Then, 100% and 50% extracts were incubated with the cells for 24 h and the viability was ascertained by extracting tetrazolium salts from the metabolically active cells and percentage viability was calculated. The percentage viability of Gelatin vinyl acetate associated Bioglass scaffold was 109.199 ± 5.09% for 50% extract and 119.45 ± 5.34% cell viability for 100% extract, and that of Gelatin vinyl acetate was found to be 99.97 ± 0.59% viability for 50% extract and 106.48 ± 3.85% cell viability for 100% extracts. From this, the extracts from both the scaffolds were seen to significantly increase the proliferative rate of the cells and showed no cytotoxic effects. This may be attributed to the fact that gelatin has a lot of innate sequences which allow for cell attachment and growth.
Adipose-Derived Mesenchymal Stem Cell Isolation and Characterisation
Various cell types are used for bone defect mechanisms, such as embryonic stem cells, induced pluripotent stem cells, adult stem cells etc. [27]. In this study, mesenchymal stem cells (MSC) which is a subtype of adult stem cells are used. The MSCs are capable of self-replication and can be expanded to sufficient numbers for tissue and organ regeneration [28]. The MSCs in bone marrow has a potential to differentiate into osteoblasts that mature to osteocytes and this process is initiated by transforming growth factor β1 (TGF β1) which is released from the neighbouring osteoclasts [29].
For ascertaining the plasticity of stem cells, trilineage differentiation assay was performed. The isolated adipose-derived stem cells showed lineage specificity towards osteogenic, adipogenic and chondrogenic lineages on providing the appropriate differentiation inducing media. The study was performed for a period of 28 days. Osteogenic lineage was confirmed on performing alizarin red staining (Fig. 3d), adipogenic lineage was confirmed on performing Oil red O staining (Fig. 3b) and chondrogenic lineage was confirmed using safranin O staining (Fig. 3f). The stem cells were also confirmed via immunostaining for mesenchymal stem cell markers specifically vimentin, endoglin, CD 90 and stained negative for CD 34 marker stain (Fig. 3g, h, i, j).
Trilineage differentiation of MSCs showing (a) Oil red O staining on control MSCs without induction, (b) Oil red O staining of lipid vacuoles on differentiated adipogenic lineage; (c) Alizarin red staining on MSCs without induction, (d) Alizarin red staining on differentiating to osteogenic lineage, (e) Safranin O staining on control MSCs without induction; (f) Safranin O staining on differentiated chondrocytes; Immunofluoresence staining of MSC specific markers; (g) Vimentin, (h) CD90, (i) Endoglin and (j) Negative marker CD 34
Live Dead Assay
The viability of the seeded ADMSCs were ascertained using Live dead assay for a 28 day culture period. Uniform distribution of viable cells was observed in both the scaffolds at the 28 day timepoint, as shown in Fig. 4. This showed that the cells were able to infiltrate within the scaffold and were viable after a culture period of 28 days. This also proved that the cells could undergo effective differentiation as they were viable even at extended periods of time and provided a cytocompatible environment for the cells to attach and grow.
SEM Analysis
The morphological analysis of bare GeVac and GB scaffolds and the ADMSCs seeded scaffolds retrieved on 1st,14th and 28th day were performed using SEM imaging (Fig. 5). From the data obtained it was observed that both the gelatin-based scaffolds—GeVac and GB supported the osteogenic differentiation of ADMSCs. There was a gradual change in the morphology of the ADMSCs to osteoblast as evident from the SEM images. When compared to the bare control and first day retrieved samples, pores on both the scaffolds become dense when they reached 14th and 28th day. In terms of osteogenic differentiation potential, it is evident that even though both the scaffold supported the osteoblast formation, the GB scaffolds showed higher cell density with increased mineralisation and uniform cell distrtibution.
Morphological analysis of scaffolds by Scanning electron microscope: (a) GV bare, (b) GB bare, (c) GV scaffold retrieved after 1 day of cell seeding, (d) GB scaffold retrieved after 1 day of cell seeding, (e) GV scaffold after 14 days of cell seeding, (f) GB scaffold after 14 days of cell seeding, (g) GV scaffold after 28 day of cell seeding, (h) GB scaffold after 28 day of cell seeding
DNA Proliferation Assay
The cell proliferation rate was also assessed through the quantification of DNA in the constructs. Fluorescence detection was employed to find the DNA content and it was observed that for both the GeVac and the GB scaffolds the DNA content was increased in the 28-day timepoint (Fig. 6a). It was also observed that after 14 days, there was a decrease in the DNA content. This may be attributed to the differentiation of stem cells in the 14th day and thereafter an increase in DNA content is experienced which may be due to the proliferation of the differentiated cells.
Calcium Assay
Calcium assay was performed to ascertain the bioactivity of the scaffolds in culture which can also be considered as osteogenic induction of the adipose stem cells in culture. The assay also helped to ascertain if there were differences in the mineralization levels in the constructs. It was observed that the calcium release was significantly higher for the GB scaffolds when compared with the GeVac constructs (Fig. 6b). The calcium released was found to be significantly higher for the GB constructs at the 14-day timepoint which may be due to the degradation of the GB constructs by the 14th day. The GeVac constructs however did not show a pronounced increase in the Calcium content in all the three timepoints as it did not induce any bioactivity as in the bioglass loaded scaffolds.
Osteogenic Gene Expression Analysis by RT-PCR
The gene expression of osteogenic specific markers (RUNX2, COL1A2, SOX9, ALP) were analysed for ADMSCs seeded on scaffolds—gelatin vinyl acetate and gelatin vinyl acetate associated with bioglass on days 14 and 28 (Fig. 7). RUNX2 is known as the master transcription factor for osteogenic differentiation [30]. They are essential for osteoblast differentiation, matrix production, and mineralisation during bone formation [31]. From the results it was observed that the expression of RUNX2 increased from day 14 to day 28 for both the scaffolds. A study conducted by Zhang et al. showed that the mineralisation in a RUNX2 transduced ADSCs increased compared to that of the control groups, suggesting that RUNX2 favours or enhances the mineralisation of bones [32]. There was no significant difference in the expression of COL1A2 in day 14 for both the scaffold but as it reached 28th day, there was a gradual decrease in the expression of COL1A2 in GB scaffold and the expression slightly increased in case of GeVac. A study done by Zhou et al. showed that the expression of COL1A2 was maximum on day 7, i.e., on the 1st construct retrieval and it gradually decreased on proceeding days. This may be indicating that COL1A is an early osteogenic marker which is mostly seen in the immature osteoblast. In another study M Dahl et al. showed that the expression of COL1A decreases from day 1 to day 8 [33]. The ALP expression on day 14 for GB was slightly less than that of GeVac and on day 28th there was no significant expression of ALP. As inferred from many studies it is seen that the ALP is an early osteogenic marker, and its expression decreases to negligible value as it reaches mineralisation phase as in the case of COL1A. This fact was more evidently reported by the study of Dahl et al. that showed a lowered expression of ALP from day 1 to day 8. In the case of SOX9, it is said to be the master transcription factor of chondrogenesis, but it is also expressed in osteo-chondroprogenitor cells. Here in our study the expression of SOX 9 is less than that of RUNX2 and this enhances delayed endochondral ossification which was also reported by Stock et al. in their study [34]. These results confirm the osteogenic differentiation potential of the AdMSC seeded GB constructs.
Conclusion
In this study, the two scaffolds—gelatin vinyl acetate (GeVac) and gelatin vinyl acetate incorporated with Bioglass (GB) was compared based on the osteogenic differentiation potential of adipose-derived mesenchymal stem cells. From the results obtained we found that GB scaffold enhanced the osteogenic differentiation of ADMSCs as it can promote the osteoblast differentiation without induction of any growth factors. This was also confirmed by the expression of osteogenic gene markers and morphological analysis using SEM which showed enhanced mineralisation in the GB scaffolds. This study also proves that use of adipose-derived mesenchymal stem cells is an ideal alternate cell source in combination with our scaffold system for use as an bone autograft. However, further preclinical studies are warranted to assess the efficacy of this system for the treatment of bone defects. Nevertheless, the findings of the study demonstrated that the bioglass incorporated GeVAc scaffold shows more bioactivity with osteogenic differentiation potential without any external induction of growth factors and hence is an ideal scaffold for bone tissue engineering.
Data Availability
The data that support the findings of this study are available from the corresponding author [Lynda V Thomas], upon reasonable request.
References
Mueller, T. L., Wirth, A. J., van Lenthe, G. H., Goldhahn, J., Schense, J., Jamieson, V., et al. (2011). Mechanical stability in a human radius fracture treated with a novel tissue-engineered bone substitute: A non-invasive, longitudinal assessment using high-resolution pQCT in combination with finite element analysis. Journal of Tissue Engineering and Regenerative Medicine, 5(5), 415–420. https://doi.org/10.1002/term.325
Younger, E. M., & Chapman, M. W. (1989). Morbidity at bone graft donor sites. Journal of Orthopaedic Trauma, 3(3), 192.
Robinson, P. G., Abrams, G. D., Sherman, S. L., Safran, M. R., & Murray, I. R. (2020). Autologous bone grafting. Operative Techniques in Sports Medicine, 28(4), 150780. https://doi.org/10.1016/j.otsm.2020.150780
Tang, G., Liu, Z., Liu, Y., Yu, J., Wang, X., Tan, Z., et al. (2021). Recent Trends in the Development of Bone Regenerative Biomaterials. Frontiers in Cell and Developmental Biology. https://doi.org/10.3389/fcell.2021.665813
Wang, W., & Yeung, K. W. K. (2017). Bone grafts and biomaterials substitutes for bone defect repair: a review. Bioactive Materials, 2(4), 224–247. https://doi.org/10.1016/j.bioactmat.2017.05.007
Koons, G. L., Diba, M., & Mikos, A. G. (2020). Materials design for bone-tissue engineering. Nature Reviews Materials, 5(8), 584–603. https://doi.org/10.1038/s41578-020-0204-2
Echave, M. C., Sánchez, P., Pedraz, J. L., & Orive, G. (2017). Progress of gelatin-based 3D approaches for bone regeneration. Journal of Drug Delivery Science and Technology, 42, 63–74. https://doi.org/10.1016/j.jddst.2017.04.012
Zha, K., Tian, Y., Panayi, A. C., Mi, B., & Liu, G. (2022). Recent advances in enhancement strategies for osteogenic differentiation of mesenchymal stem cells in bone tissue engineering. Frontiers in Cell and Developmental Biology. https://doi.org/10.3389/fcell.2022.824812
Mazzoni, E., Mazziotta, C., Iaquinta, M. R., Lanzillotti, C., Fortini, F., D’Agostino, A., et al. (2021). Enhanced osteogenic differentiation of human bone marrow-derived mesenchymal stem cells by a hybrid hydroxylapatite/collagen scaffold. Frontiers in Cell and Developmental Biology. https://doi.org/10.3389/fcell.2020.610570
Rada, T., Reis, R. L., & Gomes, M. E. (2009). Adipose tissue-derived stem cells and their application in bone and cartilage tissue engineering. Tissue Engineering Part B: Reviews, 15(2), 113–125. https://doi.org/10.1089/ten.teb.2008.0423
Mende, W., Götzl, R., Kubo, Y., Pufe, T., Ruhl, T., & Beier, J. P. (2021). The role of adipose stem cells in bone regeneration and bone tissue engineering. Cells, 10(5), 975. https://doi.org/10.3390/cells10050975
Thomas, L. V., & Nair, P. D. (2012). Influence of mechanical stimulation in the development of a medial equivalent tissue-engineered vascular construct using a gelatin-g-vinyl acetate co-polymer scaffold. Journal of Biomaterials Science, Polymer Edition, 23(16), 2069–2087. https://doi.org/10.1163/092050611X607148
Aghajanian, P., & Mohan, S. (2018). The art of building bone: emerging role of chondrocyte-to-osteoblast transdifferentiation in endochondral ossification. Bone Research, 6(1), 1–9. https://doi.org/10.1038/s41413-018-0021-z
Galea, G. L., Zein, M. R., Allen, S., & Francis-West, P. (2021). Making and shaping endochondral and intramembranous bones. Developmental Dynamics, 250(3), 414–449. https://doi.org/10.1002/dvdy.278
Kenkre, J., & Bassett, J. (2018). The bone remodelling cycle. Annals of Clinical Biochemistry, 55(3), 308–327. https://doi.org/10.1177/0004563218759371
Perić, K. Ž, Rider, P., Alkildani, S., Retnasingh, S., Pejakić, M., Schnettler, R., et al. (2020). An introduction to bone tissue engineering. The International Journal of Artificial Organs, 43(2), 69–86. https://doi.org/10.1177/0391398819876286
Almouemen, N., Kelly, H. M., & O’Leary, C. (2019). Tissue engineering: understanding the role of biomaterials and biophysical forces on cell functionality through computational and structural biotechnology analytical methods. Computational and Structural Biotechnology Journal, 17, 591–598. https://doi.org/10.1016/j.csbj.2019.04.008
Turnbull, G., Clarke, J., Picard, F., Riches, P., Jia, L., Han, F., et al. (2018). 3D bioactive composite scaffolds for bone tissue engineering. Bioactive Materials, 3(3), 278–314. https://doi.org/10.1016/j.bioactmat.2017.10.001
Ramzan, F., Salim, A., & Khan, I. (2023). Osteochondral tissue engineering dilemma: scaffolding trends in regenerative medicine. Stem Cell Reviews and Reports, 19(6), 1615–1634. https://doi.org/10.1007/s12015-023-10545-x
Khan, M. U. A., Aslam, M. A., Bin Abdullah, M. F., Hasan, A., Shah, S. A., & Stojanović, G. M. (2023). Recent perspective of polymeric biomaterial in tissue engineering– a review. Materials Today Chemistry, 34, 101818. https://doi.org/10.1016/j.mtchem.2023.101818
Echave, C. M., Burgo, S. L., Pedraz, L. J., & Orive, G. (2017). Gelatin as biomaterial for tissue engineering. Current Pharmaceutical Design, 23(24), 3567–3584. https://doi.org/10.2174/0929867324666170511123101
Lukin, I., Erezuma, I., Maeso, L., Zarate, J., Desimone, M. F., Al-Tel, T. H., et al. (2022). Progress in gelatin as biomaterial for tissue engineering. Pharmaceutics, 14(6), 1177. https://doi.org/10.3390/pharmaceutics14061177
Yin, S., Zhang, W., Zhang, Z., & Jiang, X. (2019). recent advances in scaffold design and material for vascularized tissue-engineered bone regeneration. Advanced Healthcare Materials, 8(10), 1801433. https://doi.org/10.1002/adhm.201801433
Hernandez, J. L., & Woodrow, K. A. (2022). Medical applications of porous biomaterials: features of porosity and tissue-specific implications for biocompatibility. Advanced Healthcare Materials, 11(9), 2102087. https://doi.org/10.1002/adhm.202102087
Abbasi, N., Hamlet, S., Love, R. M., & Nguyen, N.-T. (2020). Porous scaffolds for bone regeneration. Journal of Science: Advanced Materials and Devices, 5(1), 1–9. https://doi.org/10.1016/j.jsamd.2020.01.007
Madihally, S. V., & Matthew, H. W. T. (1999). Porous chitosan scaffolds for tissue engineering. Biomaterials, 20(12), 1133–1142. https://doi.org/10.1016/S0142-9612(99)00011-3
Amini, A. R., Laurencin, C. T., & Nukavarapu, S. P. (2012). Bone tissue engineering: recent advances and challenges critical reviews&trade. Biomedical Engineering, 40(5), 363–408.
Marion N. W., & Mao J. J. (2006). Mesenchymal Stem Cells and Tissue Engineering. In: Methods in Enzymology Stem Cell Tools and Other Experimental Protocols, Academic Press, 339–361, doi: https://doi.org/10.1016/S0076-6879(06)20016-8
Shibli, J. A., Nagay, B. E., Suárez, L. J., Urdániga, H. C., Bertolini, M., Barão, V. A. R., et al. (2022). Bone tissue engineering using osteogenic cells: from the bench to the clinical application. Tissue Engineering Part C: Methods, 28(5), 179–192. https://doi.org/10.1089/ten.tec.2022.0021
Komori, T. (2010). Regulation of bone development and extracellular matrix protein genes by RUNX2. Cell and Tissue Research, 339(1), 189–195. https://doi.org/10.1007/s00441-009-0832-8
Zhang, X., Yang, M., Lin, L., Chen, P., Ma, K. T., Zhou, C. Y., et al. (2006). Runx2 overexpression enhances osteoblastic differentiation and mineralization in adipose - derived stem cells in vitro and in vivo. Calcified Tissue International, 79(3), 169–178. https://doi.org/10.1007/s00223-006-0083-6
Zhou, X., Moussa, F. M., Mankoci, S., Ustriyana, P., Zhang, N., Abdelmagid, S., et al. (2016). Orthosilicic acid, Si(OH)4, stimulates osteoblast differentiation in vitro by upregulating miR-146a to antagonize NF-κB activation. Acta Biomaterialia, 39, 192–202. https://doi.org/10.1016/j.actbio.2016.05.007
Dahl, M., Syberg, S., Jørgensen, N. R., & Pinholt, E. M. (2013). Adipose derived mesenchymal stem cells – their osteogenicity and osteoblast in vitro mineralization on titanium granule carriers. Journal of Cranio-Maxillofacial Surgery, 41(8), e213–e220. https://doi.org/10.1016/j.jcms.2013.01.021
Stöckl, S., Göttl, C., Grifka, J., & Grässel, S. (2013). Sox9 modulates proliferation and expression of osteogenic markers of adipose-derived stem cells (asc). Cellular Physiology and Biochemistry, 31(4–5), 703–717. https://doi.org/10.1159/000350089
Acknowledgements
The authors acknowledge the Director, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) and Head of Biomedical Technology Wing, SCTIMST, for their support and facilities provided. We would also like to acknowledge the funding from DST, Government of India, and the DST–SCTIMST Summer Scholarship support.
Funding
Funding provided by Department of Science and Technology, Government of India and the DST-SCTIMST Summer Scholarship support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical Standard Statement
This study was approved by the Institutional Animal Ethics Committee (approval no. IAEC/DLAS/TR007.Y18) on March 31, 2018.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prasad, A.S., Banu, S., Das, S.S. et al. A Gelatin-Based Biomimetic Scaffold Promoting Osteogenic Differentiation of Adipose-Derived Mesenchymal Stem Cells. JOIO 58, 932–943 (2024). https://doi.org/10.1007/s43465-024-01182-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01182-8