Abstract
Since scaffolds are engineered to support functional tissue formation, their design and materials play an essential role in medical fields by providing different mechanical function. The aim of this study was to investigate the synthesis and structural characterization of collagen-gelatin (COL-GEL) composite scaffolds containing fluorapatite (FA) nanoparticles as well as evaluation of the osteogenic differentiation of human adipose-derived stem cells (hADSCs). First, the composite scaffolds were evaluated using Fourier transform infrared spectroscopy, scanning electron microscopy, and X-ray diffraction. The cytotoxicity of scaffolds and various concentrations of FA nanoparticles was studied through MTT assay and acridine orange/ethidium bromide staining. Next, the differentiated hADSCs were analyzed using Alizarin red and von Kossa staining, calcium content assay, alkaline phosphatase (ALP) activity, real-time RT-PCR, and immunocytochemical analyses. According to the characterization analyses, the composite scaffolds were properly integrated. The results also illustrated that COL-GEL composite scaffolds in the presence of FA nanoparticles not only showed no cytotoxicity but also increased ALP activity and calcium deposition as well as the expression of osteogenic genes, including Runx2, Col-I, ALP, and osteocalcin and the synthesis of proteins such as osteocalcin and osteopontin in vitro. The obtained data were confirmed by Alizarin red and von Kossa staining. These results are very promising for further tissue engineering experiments, in which FA nanoparticle incorporation into COL-GEL composite scaffolds is a novel approach that improves the surface COL-GEL composite scaffolds for tissue engineering application in vitro.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone tissue is complex, living, and dynamic and continuously involved in the bone remodeling process, resorption by osteoclasts, and bone reformation by osteoblasts (Florencio-Silva et al. 2015). Every year, millions of people suffer severe bone injuries resulted from congenital malformations, trauma, tumors, and surgery (Majidinia et al. 2018). Currently, the bone-related problems are wildly fixed by various medical treatments, including allografts, autografts, and xenografts (Soraya et al. 2021). However, these therapeutic strategies encounter some limitations and restrictions such as transplant rejection, severe pain, and infection (Shamsi et al. 2017). Tissue engineering has shown a promising approach that aims to repair and regenerate damaged tissues and reform their function using the combination of cells, biological molecules, and scaffolds (Fang et al. 2018; Guo and Ma 2018). In this interdisciplinary field, scaffolds can be fabricated based on natural and synthetic polymers with properties such as biocompatibility, non-toxic degradation, and appropriate porosity for the transportation of nutrients (Guo and Ma 2018; Nafary et al. 2017). An efficient scaffold, as a replicate of living structure inside tissues of the body, should provide a suitable surface with chemical, biocompatibility, and mechanical properties for cells to integrate with the recipient tissue (Cheng et al. 2019). Hydrogels are one of the most common scaffolds that constitute a wide spectrum of synthetic molecules to native proteins. They have peculiar features such as the capacity to fill an irregularly shaped space, hydrophilic nature, and suitable structure for cell culture, which make them a desirable candidate for therapeutic applications (Kamoun et al. 2017; Wolf et al. 2012).
Collagen has extensive applicability in tissue engineering as biomaterial due to its notable properties, including biocompatibility, biodegradability, easy availability, and high versatility (Lim et al. 2019). Moreover, collagen fibers lead to not only cell proliferation and osteogenic differentiation but also cell migration and cell attachments, which are necessary for tissue engineering (Somaiah et al. 2015). Despite all the mechanical features of the collagen fiber, this natural polymer may not be applied alone as a bone substitute due to the lack of adequate strength (Qian et al. 2019). Gelatin is obtained through the hydrolysis of collagen for biomedical and pharmaceutical applications. This denatured product is commercially available at low cost with high biocompatibility and biodegradability in addition to much less antigenic effect than collagen (Su and Wang 2015). Moreover, scaffolds made of either gelatin or collagen possess suitable hydrophilicity as well as mechanical and degradation properties (Grover et al. 2012). Nevertheless, these materials cannot provide a perfect extracellular matrix (ECM) environment with physical structural support. In the current study, based-collagen and gelatin (COL-GEL) hydrogel was fabricated, and an inorganic nanoparticle was used in the scaffold structure to enhance mechanical properties.
Fluorapatite (FA) (Ca10 (PO4)6 F2), as an inorganic material, is characterized with a high biocompatibility and bioactivity as well as the absence of toxic and allergenic properties (Guo et al. 2018; Pajor et al. 2019; Tredwin et al. 2014). All these features make them suitable use as coatings for metallic implants, components of composite materials, bone cement, and bone substitute components of dental materials (Pajoret al. 2019). The present study, for the first time, tries to elucidate the question that COL-GEL hydrogels in the presence of FA have the capability to support osteogenic differentiation and mineralization of human adipose-derived stem cells (hADSCs).
Over the past years, numerous studies have been performed using hADSCs as a cell source with multilineage differentiation capacity for tissue engineering and seeding them in particular scaffolds (Mazzoni et al. 2020). Moreover, hADSCs is easily extracted from adipose tissue in a less invasive way, and their proliferative and less-immunogenic properties make them one of the best sources to use in stem cell therapy (Mazini et al. 2020; Si et al. 2019).
The aim of this study was to find the synthesis and structural characterization of COL-GEL composite scaffolds containing FA nanoparticles as well as assessing the efficiency of osteogenic differentiation of hADSCs on fabricated scaffolds.
Materials and methods
Synthesis of gelatin-collagen scaffolds
Initially, 0.1 N hydrochloric acid solution at a concentration of 10% w/v was used to prepare the gelatin. Collagen solution was mixed in 0.1 N solution and added drop by drop to gelatin solution in a stirrer at 4 °C. Next, the two prepared dilutions were mixed for 5 h with a mass ratio of collagen/gelatin 1:20. The FA nanoparticles were prepared at 50 and 100 mg and added to the prepared fabricated scaffold at the concentrations of 0.5% and 1% (w/v). The solution was poured into a mold (5 cm in length and 2 cm in diameter) and incubated at 4 °C for 24 h. Two-step freezing was done at − 20 °C for 7 h followed by − 80 °C for 24 h. To produce a porous hydrogel, frozen hydrogels were moved to the freeze dryer at − 57 °C and 0.05 mbar for 24 h. For cross-linking, a 0.25% glutaraldehyde solution was used to immerse lyophilized hydrogel for 6 h. Finally, freeze-dried hydrogels were washed six steps with deionized distilled water to remove the glutaraldehyde.
Characterization of scaffolds
Fourier transformed infrared analysis
The method was used to examine the functional groups of composite samples. Fourier transformed infrared (FTIR) was recorded by FTIR spectrometer with 100 scans for a wavelength range of 400–4000 cm−1 at a scan speed of 23 scans/min with 4 cm−1 resolution.
X-ray diffraction measurement
To determine the structure, X-ray diffraction (XRD) was performed with a Rigaku RINT 2000 at 20 kV and 2 Ma.
Scanning electron microscopy
Scanning electron microscopy (SEM) was utilized to analyze the scaffold morphology. For this purpose, before and after the cell culturing, the supernatant was removed, and the scaffolds were washed with sterile phosphate buffered saline (PBS). Next, to fix the cells, 5.2% glutaraldehyde solution (300 μl) was added for 1 h. After removal of the glutaraldehyde solution, the surfaces of scaffolds were rinsed with PBS. The composite scaffolds were kept in ethanol solution with concentrations of 60, 70, 80, 90, and 100% for 10 min/each to dehydrate the cells. Finally, the images were obtained by SEM (Hitachi S-4500, Japan).
Biological investigation
Cell culture
Human ADSCs lines were obtained from the cell bank of Stem Cells Technology Research Center (Tehran, Iran) and cultured in Dulbecco’s modified eagle medium (DMEM) containing 10% fetal bovine serum (FBS) and 1% streptomycin/penicillin (all from Gibco, USA) in a humidified atmosphere of 5% CO2 at 37 °C. Almost 50% of the culture medium was replaced every 2 days. When the hADSCs reached 80% confluency, they were segregated by 0.25% trypsin with 0.1% EDTA to form a single cell suspension. Cells at the second passage were used for the study.
Sterilization and cell seeding
First, hydrogels were prepared in 0.5 × 0.5 cm2 samples and placed in 24-well culture plates (Orange Science, Belgium) in two groups, with and without FA nanoparticles, and then immersed in 70% ethanol for 1 h to remove all potential residues from the sample preparation. After washing three times with PBS for 2 min, cells were cultured on the scaffolds or directly onto the 24-well plate at a density of 1 × 104 cells/well with a serum medium consisting of DMEM, 10% FBS, and l % penicillin/streptomycin. Seeded cells were incubated at 37 °C and 5% CO2.
Cell viability assay
The cell viability of hADSCs on various concentrations of FA (50, 100, and 500 μg/ml), different scaffolds (pure, 0.5% and 1% COL-GEL-FA), and TCPS (control group) was evaluated via MTT assay at days 1, 3, and 5 of cell seeding. At the end of each day, the MTT (Sigma-Aldrich) was poured into each well, and the plate was kept at 37 °C for 3 h according to pervious work (Eftekhari et al. 2021). After removal of the supernatant, 100 μl of DMSO was added. The optical density was read by a microplate reader (BioTek Instruments, USA) at a wavelength of 570–630 nm.
Acridine orange/ethidium bromide staining
This staining was used to evaluate the cell viability of cells as a qualitative assay. The dual fluorescent staining solution containing 100 µg/ml AO and 100 µg/ml EB (AO/EB, Sigma) was purred to each well washed for 2 min with PBS. After 20 min of staining, each well was imaged with a fluorescent microscope (Nikon, Japan).
Osteogenic differentiation
To differentiate hADSCs into osteogenic lineages, after removing the basal media, osteogenic medium containing DMEM supplemented with 10% FBS, 50 mg/ml ascorbic acid 2-phosphate, 10 nM dexamethasone, and 10 mM P-glycerophosphate (all from Sigma Chemical Co) was added into wells. The cultures were then incubated at 37 °C and 5% CO2 for 14 days.
Alkaline phosphatase activity
Alkaline phosphatase (ALP) assay kit (Parsazmun, Iran) was used to evaluate the ALP activity during osteogenic differentiation of hADSCs after 7 and 14 days. After washing all plates with ice-cold PBS immediately, a radio immune precipitation assay (RIPA) (200 μl) was used to extract all proteins from the cells. Next, the supernatants were centrifuged for 15 min at 15,000 g and 4 °C and incubated then with an ALP assay kit according to the manufacturer’s protocol. The amount of ALP in samples was measured at 405 nm using a microplate reader (BioTek Instruments, USA).
Calcium content assay
All samples were also examined for calcium deposition using a calcium assay kit (Parsazmun, Tehran, Iran) after 7 and 14 days of osteogenic differentiation. First, each sample was slowly rinsed with PBS. Calcium extraction was done to homogenize using 0.6 mol/L hydrochloric acid (Merck) followed by shaking the supernatant for 40 min at 4 °C. Then calcium reagent working solution was mixed into each sample. The color intensity was assessed at 550 nm, and the standard solution was used to measure the calcium content.
Alizarin red and von Kossa staining
On days 7 and 14 after differentiation, Alizarin red and the von Kossa staining were performed to evaluate the osteogenic differentiation of samples. For this aim, after removal of the medium culture, the cells were washed with PBS for 2 min. Next, 4% formaldehyde (Merck, Germany) was used to fix the cell at 4 °C for 20 min, and then washing step was done with PBS to remove the formaldehyde. The cells were stained with 1% solution of Alizarin red (Merck, Germany) at a pH of 7.2 and room temperature for 5 min. Following a rinse of the additional color with distilled water several times, the stained bone cells were imaged using light microscopy (Carl Zeiss-Axiovert, Germany). Similarly, the von Kossa staining stages were done by 5% silver nitrate solution for 5 min. After the removal of the unreacted silver with 5% sodium thiosulfate, cells were washed for 4 times with double distilled water. Finally, the differentiated cells were captured by light microscopy (Carl Zeiss-Axiovert, Germany). The quantitative assessment of both methods was performed by image analysis software (ImageJ).
Real-time RT-PCR
The gene expression of the key osteogenic markers, including runt-related transcription factor2 (Runx2), collagen type 1 (Col-I), ALP, and osteocalcin, was analyzed by the real‐time reverse transcription 3polymerase chain reaction (RT‐PCR) assay at days 7 and 14 after the osteogenic induction. Following the isolation of total cellular RNA from hADSCs, cDNA synthesis was performed applying a Revert Aid first-strand cDNA synthesis kit (Fermentas, Burlington, Canada). The cDNA was applied for 40 cycles of PCR by a Rotor‐gene Q Real‐time analyzer (Corbett, Australia). Real‐time PCR was carried out using Maxima TM SYBR Green/ROX qPCR Master Mix (Fermentas) followed by melting curve analysis to confirm PCR specificity. All samples were evaluated in duplicate, and the average values were applied for quantification. It should be considered that target genes were normalized against HPRT and calibrated to TCPS. The related primer sequences are indicated in Table 1.
Immunocytochemistry
The immunocytochemistry (ICC) was done to measure the synthesis of osteogenic proteins containing osteocalcin and osteopontin at the end of the first and second weeks after the osteogenic induction. For this purpose, all wells were washed twice with PBS before fixing with 4% paraformaldehyde (Sigma) for 20 min. After washing again, 0.4% Triton Xl 00 was used to make high permeability in membrane’s hADSCs. Next, the 5% goat serum/PBS-tween-20 was added to block the cells for 30 min at 37 °C. After the removal of the block solution, the primary antibodies, including osteocalcin (1:100; Santa Cruz Biotechnology Inc.) and osteopontin (1:200; Santa Cruz Biotechnology Inc.) were added into wells that were incubated overnight at 4 °C (Azizipour et al. 2021).The next day, the cells were washed three times using PBS–Tween‐20 (0.1%) and maintained at room temperature for 2 h with the secondary antibody, fluorescein isothiocyanate (FITC)‐conjugated anti‐mouse IgG (1:100; Sigma‐Aldrich). Following a rinse with PBS, DAPI 10% (Sigma‐Aldrich) was added to counterstain the cell’s nucleus. Finally, the cells were captured with fluorescent microscopy (Nikon, Japan). The intensity of antibodies was measured by ImageJ.
Statistical analysis
All biological experiments were evaluated through a one-way analysis of variance (ANOVA). The result was reported as mean ± standard deviation (SD). P-values < 0.05 were considered statistically significant.
Results
Physico-chemical characterization of COL-GEL-FA nanocomposites
The FTIR spectroscopy was used to analyze the functional group in molecular nature of COL-GEL-FA. As results shown in Fig. 1a, the peaks of neat FA at 563 and 1056 cm−1 in the fingerprint region show the vibratory motion of the structures of nanoparticles. The absorbance band sited in 1650 cm−1 is related to carbonyl functional groups in amide bands in both materials (collagen and gelatin). On the other hand, –NH groups due to hydrogen bands show a broad peak in 3600 cm−1. In COL-GEL cross-linked sample, the amount of –NH groups decreased because cross-linker agents reacted with amin groups; this claim can be observed from the FTIR spectrum from uncross-linked COL-GEL sample. The presence of FA nanoparticles in the COL-GEL sample has created many changes in main peaks through reactions between functional groups in FA and amide bonds in collagen and gelatin materials.
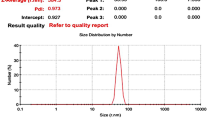
The XRD analysis was done to investigate the crystallographic of the COL-GEL-FA scaffold, as shown in Fig. 1b. The XRD pattern of the FA nanoparticle shows the peaks at 26/7°, 31°, and 49/4°. This pattern indicates that FA nanoparticles do not have significant crystal plates. The comparison between XRD patterns, uncross-linked and cross-linked samples, showed that using cross-linker agents leads to a decrease in the intensity of crystalline peaks. In nanocomposite samples (COL-GEL-FA), it suggested that the presence of nanoparticles has shown minimal effect on crystal structures. As a result, it appears that the main nanocomposite material has an almost amorphous structure.
Scanning electron microscopy
Figure 2 shows the SEM micrographs of FA nanoparticles and scaffold on the 14th day of differentiation. According to data, FA nanoparticles with 20.16, 22.01, and 26.82 nm (Fig. 2a) and with 19.31, 19.69, and 23.49 nm on the scaffold (Fig. 2b) were observed. Porous and interconnected structures seen in Fig. 2b suggested that it is effective for cell adhesion and migration in tissue engineering. Figure 2c shows the micrograph of COL-GEL prepared in high quality. As shown in Fig. 2d, all cells were attached on the surfaces of the scaffold.
SEM micrographs of a FA nanoparticle, b COL-GEL-FA0.5% scaffold, c COL-GEL scaffold without cells, and d COL-GEL-FA0.5% scaffold with attached cells. Green, yellow, and red arrows point to nanoparticle, pores, and cells, respectively. FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5%, COL-GEL hydrogel in the presence of 0.5% fluorapatite nanoparticles
Cytotoxicity assay
Figure 3a shows the hADSCs proliferation in different concentrations of FA nanoparticle and COL-GE scaffolds with and without FA nanoparticles on the 1st, 3rd, and 5th days assessed by MTT assay. There was no significant cytotoxicity for all groups at 1 and 3 days after induction, and FA at concentration of 100 μg/ml illustrated a remarkable enhancement in cell proliferation of hADSCs compared to TCPS and the other group in 3 days. Additionally, the COL-GEL-FA scaffold 0.5% and 1% represented no cytotoxicity in samples.
hADSCs proliferation in different concentrations of FA nanoparticle, COL-GEL scaffolds with and without FA nanoparticles at days 1, 3, and 5. a MTT assay (*p < .05 and **p < .01). b–h″ AO/EB staining. Scale bar b–e′′: 10 μm, f–h′′: 20 μm. TCPS, tissue culture polystyrene or control sample; FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5% and 1%, COL-GEL hydrogel in the presence of 0.5% and 1% fluorapatite nanoparticles, respectively
AO/EB staining was done to confirm the cell viability performed by MTT assay. In this assay, the nucleus of a living cell is green; in contrast, the nucleus of a dead cell represents red color. According to the result shown in Fig. 3b–h′′, all samples represent normal morphology of nucleus in comparison with TCPS after 5 days of induction. These results showed that FA at concentration of 100 μg/ml and COL-GEL-FA scaffolds had no cytotoxicity in cells. Hence, the FA at concentration of 100 μg/ml and the COL-GEL-FA0.5% scaffold were chosen for further experiments.
ALP activity measurement and calcium content assay
ALP activity and calcium content were determined quantitatively at days 7 and 14 after differentiation. In Fig. 4a, a significant enhancement in the ALP activity was observed in the hADSCs cultured under FA nanoparticles conditions on the 7th and 14th days. There was no significant increase in cells cultured on both scaffolds on the 7th day. However, on the 14th day, a clear increase in the ALP level was seen in cells cultured on the COL-GEL scaffolds in comparison with those on the COL-GEL-FA0.5% scaffolds. These results illustrated that both COL-GEL scaffold and COL-GEL-FA0.5% scaffold had an osteoinductive effect on the hADSCs.
a Alkaline phosphatase activity, b calcium content on nanoparticle and nanocomposite scaffolds during osteogenic differentiation (*p < .05, **p < .01, and ***p < .001). TCPS, tissue culture polystyrene or control sample; FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5%, COL-GEL hydrogel in the presence of 0.5% fluorapatite nanoparticles
According to calcium content test, a greater amount of calcium was produced in cells seeded on the COL-GEL-FA0.5% scaffolds in comparison with those on other groups at the end of the first and second weeks after the osteogenic induction (Fig. 4b). However, the cells treated with FA nanoparticles and COL-GEL scaffolds displayed a significant calcium deposit during differentiation days. Thus, the calcium content assay supported that COL-GEL-FA0.5% scaffolds might increase the osteogenic differentiation in hADSCs.
Alizarin Red and von Kossa staining
Qualitatively, calcium nodules were seen by Alizarin red and von Kossa staining at 7 and 14 days after osteogenic induction. Calcium sediments significantly increased in cells cultured on FA nanoparticles and COL-GEL-FA0.5% scaffolds compared to TCPS proved by Alizarin red test (Fig. 5a–a′′′). As evidence shown in Fig. 5c–c′′′, von Kossa staining illustrated that there was a heavy mineral deposition throughout the COL-GEL-FA0.5% scaffolds compared to other groups after 14 days of culture. The data obtained by ImageJ software (Fig. 5b and d) proved that COL-GEL-FA0.5% illustrated more mineralized nodule formation and intense staining compared to the other groups.
Calcium deposition staining on nanoparticle and nanocomposite scaffolds during osteogenic differentiation. a–a′′′ Alizarin red S, b the graph of % area for calcium nods, c–c′′′ von Kossa staining, and d the graph of % area for von Kossa staining. Scale bar: 10 μm. (*p < .01). TCPS, tissue culture polystyrene or control sample; FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5%, COL-GEL hydrogel in the presence of 0.5% fluorapatite nanoparticles
Gene expression analysis
Expression level of critical genes associated with the osteogenic differentiation, including ALP, Col-I, osteocalcin, and Runx2 was measured using real-time RT-PCR to study the effect of FA nanoparticle and COL-GEL-FA0.5% scaffolds at days 7 and 14 after induction (Fig. 6). On the 7th day, real-time RT-PCR illustrated that the gene expression of osteogenic markers in the cells cultured on COL-GEL-FA0.5% scaffolds was remarkably higher than those on the other groups (Fig. 6a). However, the gene expression of these transcription factors increased in all groups during the osteogenic induction. As shown in Fig. 6b, the COL-GEL-FA0.5% scaffolds significantly upregulated the osteogenic gene expression known as ALP, Col-I, osteocalcin, and Runx2 on the 14th day.
The expression level of osteogenic markers in hADSCs cultured on nanoparticle and nanocomposite scaffolds at a 7 and b 14 days after osteogenic differentiation (*p < .05, **p < .01, and ***p < .001). TCPS, tissue culture polystyrene or control sample; FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5%, COL-GEL hydrogel in the presence of 0.5% fluorapatite nanoparticles
Osteocalcin and osteopontin immunofluorescence staining
Figure 7 reveals the ICC analysis of the expression of osteocalcin and osteopontin proteins in all groups after 14 days. The expression of these osteogenic markers confirmed their presence in differentiated hADSCs in all samples. In COL-GEL-FA0.5% scaffolds, the highest expression of osteocalcin and osteopontin proteins was observed in comparison with the other groups. The intensity of osteocalcin and osteopontin was measured by ImageJ (Fig. 7i).
Immunostaining of differentiated hADSCs to exhibit a–d′′ osteocalcin and e–h′′ osteopontin expression levels on the 14th differentiation. Scale bar: 20 μm. i The graph of % area for antibodies (**p < .01). TCPS, tissue culture polystyrene or control sample; FA, fluorapatite nanoparticles; COL-GEL, collagen and gelatin hydrogel; COL-GEL-FA0.5%, COL-GEL hydrogel in the presence of 0.5% fluorapatite nanoparticles
Discussion
Over the past years, tissue engineering has been used to repair damaged and diseased tissues. The significant factors of this field are potent stem cells, biocompatible scaffolds, and effective inducers on differentiation (Bayat et al. 2019). The use of various biocompatible materials to fabricate suitable structures of scaffolds enhances cell attachment, proliferation, and differentiation of stem cells and leads to impressive results in terms of osteogenic differentiation (Markides et al. 2012). The fabricated scaffolds should be structurally similar to natural ECM to achieve an appropriate result in terms of cell functions and tissue formation (Yao et al. 2017). Although numerous studies have been performed to develop biomaterial-based tissue engineered products, more efforts should be made for producing practical techniques of fabricating suitable scaffolds. In this research, for the first time, the FA nanoparticle as an inducer was used to synthesize a COL-GEL-based scaffold for increasing the osteogenic differentiation efficiency of hADSCs. Then the physical and structural properties of nanocomposite scaffolds were evaluated.
Collagen has been reported to induce osteogenic differentiation of mesenchymal stem cells (MSCs), and researchers have extensively applied it to biological scaffolds (Akhir and Teoh 2020). Substrate attachment sites are critical for development, differentiation, and metabolic activity for various cell types. Collagen integrin-binding domains increase cell expansion and survival in culture (Reichert et al. 2009). On the other hand, the high water content of collagen hydrogels causes poorer mechanical properties so that these hydrogels are insufficiently strong and degrade quickly (Goodarzi et al. 2019). Various polymers inside the collagen network can also develop mechanical properties and biodegradability of collagen hydrogels. A large number of residues of gelatin, including glycine and proline, promote cell attachment and biomolecule sediment (Zhou et al. 2021). Interestingly, gelatin-based biomaterial properties such as biocompatibility, low antigenicity, and effective cell attachment have made gelatin as a promising candidate in tissue regeneration (Bello et al. 2020; Goodarzi et al. 2019). Despite the functional properties, gelatin-based materials possess weak mechanical properties, which make them thermally unstable, and degrade at a faster rate, and then they are not able to keep their structural integrity alone (Bello et al. 2020; Ji et al. 2020). Some studies have shown that a Gel-COL-based scaffold not only had suitable hydrophilicity and optimal mechanical and degradation properties but also enhanced cell viability and proliferation (Goodarzi et al. 2019; Grover et al. 2012). Furthermore, it was appropriate for cell adhesion and infiltration due to its highly porous structure with interconnected pores (Goodarzi et al. 2019). Based on SEM micrographs of differentiated hADSCs, the structure and porosity of synthesized nanocomposite scaffolds acted as an environment for cell attachment and growth to immigrate the cells. Moreover, the scaffolds showed a better supply in creating a proper cell behavior that can be associated to its similarity to natural ECM. Furthermore, the obtained data illustrated that COL-GEL composite scaffolds increased cell viability and the expression of osteogenic proteins and genes in vitro. In addition, this hydrogel had positive osteogenesis effects that they altered in ALP enzyme activity and calcium deposition.
Currently, osteoinductive materials have been widely utilized in tissue regeneration to promote the osteogenic processes. Azizipour et al. (2021) investigated the influence of COL-GEL hydrogel with and without nanoparticles on osteogenic differentiation of MSCs, and the cell proliferation and ability of biomineralization of MSCs increased after incorporating nanoparticles into COL-GEL hydrogel. The FA nanoparticles are capable of releasing fluoride at a regulated rate, and according to the previous findings, fluoride has the inducing effect on bone formation (Kushwaha et al. 2012). According to spectrum data, the sharp peak between 800 cm−1 and 1200 cm−1 of FA nanoparticles is associated to the PO43− group which was observed in the spectrum of COL-GEL-FA implying that it could be a reason of bonding between the FA and COL-GEL scaffolds. Indeed, the 950 cm−1 band is associated with PO43− group with FA as well as stretching and bending of scaffolds for PO43− are at 580–590 cm−1 (Montazeri et al. 2011). Additionally, studies have shown that FA surfaces promoted osteogenic differentiation and mineralization of ADSCs (Clark et al. 2015; Liu et al. 2012). In addition, it has been frequently reported that the properties of FA crystals could attract pro-osteogenic growth factors from the culture media to produce an osteoinductive microenvironment (Guo et al. 2014). As indicated in MTT assay, FA at concentration of 100 μg/ml had not only no toxicity on cells but also an effect on proliferation of hADSCs. Furthermore, compared to COL-GEL scaffolds, the COL-GEL-FA scaffolds increased the cell proliferation in MTT assay. Herein, we suggested that incorporation of FA nanoparticles into the COL-GEL hydrogel as a novel nanocomposite may activate the regulators of osteogenesis in hADSCs.
Furthermore, COL-GEL-FA scaffolds illustrated high ALP activity and calcium deposits along with enhanced production of ALP, Col-I, osteocalcin, and Runx2 compared to COL-GEL scaffolds. A synergistic effect between COL-GEL and FA nanoparticles showed that it could effectively induce the osteogenic differentiation of hADSCs. The expression levels of osteogenic genes detected by real-time RT-PCR in bone tissue engineering have been studied previously. The upregulation of osteogenic genes, including Runx2, and osteocalcin are related to the development of spontaneous osteogenesis (Akhir and Teoh 2020). Runx2 expression significantly enhances during the osteogenic differentiation of MSC in the early stage of development (Wang et al. 2019). Osteocalcin serves as a reliable indicator of osteogenic development that appears at the early stages of differentiation days (Nakamura et al. 2009). The COL-GEL-FA composite scaffolds showed a significant upregulation of Runx2 and osteocalcin expression during the first 7 days. At the end of the second week, while all groups showed a significant increase in osteocalcin expression comparable to the TCPS, it was not clear which group expressed more osteocalcin. Moreover, the COL-GEL group showed the higher gene expression of Runx2 than the other groups which was not observed as same as the first week. However, COL-GEL-FA composite scaffolds represented a remarkable increase in comparison with TCPS. The ALP as an essential enzyme provides a high phosphate concentration that combines with calcium to organize mineral deposition process (Blair et al. 2018). Moreover, Col-I binds to the cell surface with the other proteins as the main component of the ECM (Li et al. 2016). In the current research, the COL-GEL-FA composite scaffolds showed higher ALP and Col-I expression compared to TCPS and other groups on days 7 and 14.
In addition to osteocalcin, osteopontin is one of the most non-collagen proteins in bone tissue. In the current study, the presence of osteogenic proteins, osteocalcin and osteopontin, was evaluated qualitatively by the ICC method. The highest expression of these proteins was observed in differentiated cells on the COL-GEL-FA nanocomposite scaffolds compared to those on the other groups. According to the data, FA made the increased expression of osteogenic proteins and genes. FA nanoparticles with a differential induction effect stimulate cellular signaling such as FGF and VEGF signaling pathways during the osteogenesis process (Clark et al. 2015; Wang et al. 2014). Moreover, the COL-GEL-FA scaffolds increased the expression of osteocalcin and osteopontin during bone differentiation, and the results obtained from the expression of proteins in ICC are consistent with the results of real-time PCR.
Conclusion
In conclusion, as indicated by the calcium content, ALP activity, and expression levels of proteins genes involved in bone differentiation, COL-GEL-FA composite scaffolds showed a good biocompatibility for supporting the osteogenic differentiation of hADSCs in vitro. This may suggest that incorporating FA nanoparticles into COL-GEL composite scaffolds can make a beneficial scaffold for further tissue regeneration experiments by affecting the signal pathways involved in osteogenesis. Therefore, FA nanoparticles are a novel approach that improves the surface COL-GEL composite scaffolds for tissue engineering application in vitro. However, it is important that prior to in vivo assessment, additional studies about the scaffold, such as plasticity, ease of formation, and fluidity are essential.
References
Akhir HM, Teoh PL (2020) Collagen type I promotes osteogenic differentiation of amniotic membrane-derived mesenchymal stromal cells in basal and induction media. Biosci Rep 40
Azizipour E, Aghamollaei H, Halabian R, Poormoghadam D, Saffari M, Entezari M, Salimi A (2021) A novel hydrogel scaffold contained bioactive glass nanowhisker (BGnW) for osteogenic differentiation of human mesenchymal stem cells (hMSCs) in vitro. Int J Biol Macromol 174:562–572
Bayat H, Shahabinejad H, Bayat M, Shirian S, Mohamadnia A, Alijani M, Godarzi A, Shojaei P, Shojaei S, Shevidi A, Bahrami N (2019) Osteogenic differentiation of follicular stem cells on nano-Saghez scaffold containing BMP2. J Orthop Surg Res 14:442
Bello AB, Kim D, Kim D, Park H, Lee S-H (2020) Engineering and functionalization of gelatin biomaterials: from cell culture to medical applications. Tissue Eng Part B Rev 26:164–180
Blair HC, Larrouture QC, Tourkova IL, Liu L, Bian JH, Stolz DB, Nelson DJ, Schlesinger PH (2018) Support of bone mineral deposition by regulation of pH. Am J Physiol Cell Physiol 315:C587–C597
Cheng A, Schwartz Z, Kahn A, Li X, Shao Z, Sun M, Ao Y, Boyan BD, Chen H (2019) Advances in porous scaffold design for bone and cartilage tissue engineering and regeneration. Tissue Eng Part B Rev 25:14–29
Clark D, Wang X, Chang S, Czajka-Jakubowska A, Clarkson BH, Liu J (2015) VEGF promotes osteogenic differentiation of ASCs on ordered fluorapatite surfaces. J Biomed Mater Res A 103:639–645
Eftekhari E, Ghollasi M, Halabian R, Soltanyzadeh M, Enderami SE (2021) Nisin and non-essential amino acids: new perspective in differentiation of neural progenitors from human-induced pluripotent stem cells in vitro. Hum Cell
Fang W, Gu T, Liu Y, Xu L, Chen Y (2018) The application of nanotopography in the development of tissue engineered tissues using mesenchymal stem cells. Sheng wu yi xue gong cheng xue za zhi= J Biomed Eng = Shengwu yixue gongchengxue zazhi 35:145–150
Florencio-Silva R, Sasso GR, Sasso-Cerri E, Simões MJ, Cerri PS (2015) Biology of bone tissue: structure, function, and factors that influence bone cells. Biomed Res Int 2015:421746
Goodarzi H, Jadidi K, Pourmotabed S, Sharifi E, Aghamollaei H (2019) Preparation and in vitro characterization of cross-linked collagen–gelatin hydrogel using EDC/NHS for corneal tissue engineering applications. Int J Biol Macromol 126:620–632
Grover CN, Cameron RE, Best SM (2012) Investigating the morphological, mechanical and degradation properties of scaffolds comprising collagen, gelatin and elastin for use in soft tissue engineering. J Mech Behav Biomed Mater 10:62–74
Guo B, Ma PX (2018) Conducting polymers for tissue engineering. Biomacromol 19:1764–1782
Guo T, Cao G, Li Y, Zhang Z, Nör JE, Clarkson BH, Liu J (2018) Signals in stem cell differentiation on fluorapatite-modified scaffolds. J Dent Res 97:1331–1338
Guo T, Li Y, Cao G, Zhang Z, Chang S, Czajka-Jakubowska A, Nör JE, Clarkson BH, Liu J (2014) Fluorapatite-modified scaffold on dental pulp stem cell mineralization. J Dent Res 93:1290–1295
Ji X, Yuan X, Ma L, Bi B, Zhu H, Lei Z, Liu W, Pu H, Jiang J, Jiang X, Zhang Y, Xiao J (2020) Mesenchymal stem cell-loaded thermosensitive hydroxypropyl chitin hydrogel combined with a three-dimensional-printed poly(ε-caprolactone)/nano-hydroxyapatite scaffold to repair bone defects via osteogenesis, angiogenesis and immunomodulation. Theranostics 10:725–740
Kamoun EA, Kenawy ES, Chen X (2017) A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J Adv Res 8:217–233
Kushwaha M, Pan X, Holloway JA, Denry IL (2012) Differentiation of human mesenchymal stem cells on niobium-doped fluorapatite glass-ceramics. Dent Mater 28:252–260
Li J, Hao L, Wu J, Zhang J, Su J (2016) Linarin promotes osteogenic differentiation by activating the BMP-2/RUNX2 pathway via protein kinase A signaling. Int J Mol Med 37:901–910
Lim YS, Ok YJ, Hwang SY, Kwak JY, Yoon S (2019) Marine collagen as a promising biomaterial for biomedical applications. Mar Drugs 17
Liu J, Wang X, Jin Q, Jin T, Chang S, Zhang Z, Czajka-Jakubowska A, Giannobile WV, Nör JE, Clarkson BH (2012) The stimulation of adipose-derived stem cell differentiation and mineralization by ordered rod-like fluorapatite coatings. Biomaterials 33:5036–5046
Majidinia M, Sadeghpour A, Yousefi B (2018) The roles of signaling pathways in bone repair and regeneration. J Cell Physiol 233:2937–2948
Markides H, Rotherham M, El Haj A (2012) Biocompatibility and toxicity of magnetic nanoparticles in regenerative medicine. J Nanomater
Mazini L, Rochette L, Admou B, Amal S, Malka G (2020) Hopes and limits of adipose-derived stem cells (ADSCs) and mesenchymal stem cells (MSCs) in wound healing. Int J Mol Sci 21
Mazzoni E, D’Agostino A, Iaquinta MR, Bononi I, Trevisiol L, Rotondo JC, Patergnani S, Giorgi C, Gunson MJ, Arnett GW, Nocini PF, Tognon M, Martini F (2020) Hydroxylapatite-collagen hybrid scaffold induces human adipose-derived mesenchymal stem cells to osteogenic differentiation in vitro and bone regrowth in patients. Stem Cells Transl Med 9:377–388
Montazeri N, Jahandideh R, Biazar E (2011) Synthesis of fluorapatite-hydroxyapatite nanoparticles and toxicity investigations. Int J Nanomed 6:197–201
Nafary A, Seyedjafari E, Salimi A (2017) Electrospun poly-L-lactic acid coated with silicate bioceramic nanoparticles enhance osteogenic differentiation of adipose tissue derived mesenchymal stem cells. J Biomater Tissue Eng 7:91–100
Nakamura A, Dohi Y, Akahane M, Ohgushi H, Nakajima H, Funaoka H, Takakura Y (2009) Osteocalcin secretion as an early marker of in vitro osteogenic differentiation of rat mesenchymal stem cells. Tissue Eng Part C Methods 15:169–180
Pajor K, Pajchel L, Kolmas J (2019) Hydroxyapatite and fluorapatite in conservative dentistry and oral implantology-a review. Materials (Basel) 12
Qian S, Wang Z, Zheng Z, Ran J, Zhu J, Chen W (2019) A collagen and silk scaffold for improved healing of the tendon and bone interface in a rabbit model. Med Sci Monit 25:269–278
Reichert JC, Heymer A, Berner A, Eulert J, Nöth U (2009) Fabrication of polycaprolactone collagen hydrogel constructs seeded with mesenchymal stem cells for bone regeneration. Biomed Mater 4:065001
Shamsi M, Karimi M, Ghollasi M, Nezafati N, Shahrousvand M, Kamali M, Salimi A (2017) In vitro proliferation and differentiation of human bone marrow mesenchymal stem cells into osteoblasts on nanocomposite scaffolds based on bioactive glass (64SiO2-31CaO-5P2O5)-poly-l-lactic acid nanofibers fabricated by electrospinning method. Mater Sci Eng C 78:114–123
Si Z, Wang X, Sun C, Kang Y, Xu J, Wang X, Hui Y (2019) Adipose-derived stem cells: sources, potency, and implications for regenerative therapies. Biomed Pharmacother 114:108765
Somaiah C, Kumar A, Mawrie D, Sharma A, Patil SD, Bhattacharyya J, Swaminathan R, Jaganathan BG (2015) Collagen promotes higher adhesion, survival and proliferation of mesenchymal stem cells. PLoS ONE 10:e0145068
Soraya Z, Ghollasi M, Halabian R, Eftekhari E, Tabasi A, Salimi A (2021) Donepezil hydrochloride as a novel inducer for osteogenic differentiation of mesenchymal stem cells on PLLA scaffolds in vitro. Biotechnol J 2100112
Su K, Wang C (2015) Recent advances in the use of gelatin in biomedical research. Biotechnol Lett 37:2139–2145
Tredwin CJ, Young AM, Abou Neel EA, Georgiou G, Knowles JC (2014) Hydroxyapatite, fluor-hydroxyapatite and fluorapatite produced via the sol-gel method: dissolution behaviour and biological properties after crystallisation. J Mater Sci Mater Med 25:47–53
Wang X, Zhang Z, Chang S, Czajka-Jakubowska A, Nör JE, Clarkson BH, Ni L, Liu J (2014) Fluorapatite enhances mineralization of mesenchymal/endothelial cocultures. Tissue Eng Part A 20:12–22
Wang Y, Sun N, Zhang Y, Zhao B, Zhang Z, Zhou X, Zhou Y, Liu H, Zhang Y, Liu J (2019) Enhanced osteogenic proliferation and differentiation of human adipose-derived stem cells on a porous n-HA/PGS-M composite scaffold. Sci Rep 9:7960
Wolf MT, Daly KA, Brennan-Pierce EP, Johnson SA, Carruthers CA, D’Amore A, Nagarkar SP, Velankar SS, Badylak SF (2012) A hydrogel derived from decellularized dermal extracellular matrix. Biomaterials 33:7028–7038
Yao Q, Cosme JG, Xu T, Miszuk JM, Picciani PH, Fong H, Sun H (2017) Three dimensional electrospun PCL/PLA blend nanofibrous scaffolds with significantly improved stem cells osteogenic differentiation and cranial bone formation. Biomaterials 115:115–127
Zhou L, Fan L, Zhang FM, Jiang Y, Cai M, Dai C, Luo YA, Tu LJ, Zhou ZN, Li XJ, Ning CY, Zheng K, Boccaccini AR, Tan GX (2021) Hybrid gelatin/oxidized chondroitin sulfate hydrogels incorporating bioactive glass nanoparticles with enhanced mechanical properties, mineralization, and osteogenic differentiation. Bioact Mater 6:890–904
Acknowledgements
We would like to acknowledge the Clinical Research Development Center of the Baqiyatallah Hospital for their technical support. Also, we thank Ms. Elahe Eftekhari for her helpful comments in this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rohani, Z., Ghollasi, M., Aghamollaei, H. et al. A new hydrogel with fluorapatite nanoparticles for osteogenic differentiation of human adipose-derived stem cells in tissue engineering field. Cell Tissue Res 390, 399–411 (2022). https://doi.org/10.1007/s00441-022-03691-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-022-03691-0