Abstract
Neurodegenerative diseases (NDDs) encompass a range of conditions characterized by the specific dysfunction and continual decline of neurons, glial cells, and neural networks within the brain and spinal cord. The majority of NDDs exhibit similar underlying causes, including oxidative stress, neuroinflammation, and malfunctioning of mitochondria. Elevated levels of acetylcholinesterase (AChE) and butyrylcholinesterase (BChE), alongside decreased expression of brain-derived neurotrophic factor (BDNF) and glutamate transporter subtype 1 (GLT-1), constitute significant factors contributing to the pathogenesis of NDDs. Additionally, the dual-specificity tyrosine phosphorylation-regulated kinase 1 A (DYRK1A) gene has emerged as a significant target for the treatment of NDDs at the preclinical level. It significantly contributes to developmental brain defects, early onset neurodegeneration, neuronal loss, and dementia in Down syndrome. Moreover, an impaired ubiquitin-proteosome system (UPS) also plays a pathological role in NDDs. Malfunctioning of UPS leads to abnormal protein buildup or aggregation of α-synuclein. α-Synuclein is a highly soluble unfolded protein that accumulates in Lewy bodies and Lewy neurites in Parkinson’s disease and other synucleinopathies. Recent research highlights the promising potential of natural products in combating NDDs relative to conventional therapies. Alkaloids have emerged as promising candidates in the fight against NDDs. Harmine is a tricyclic β-carboline alkaloid (harmala alkaloid) with one indole nucleus and a six-membered pyrrole ring. It is extracted from Banisteria caapi and Peganum harmala L. and exhibits diverse pharmacological properties, encompassing neuroprotective, antioxidant, anti-inflammatory, antidepressant, etc. Harmine has been reported to mediate its neuroprotective via reducing the level of inflammatory mediators, NADPH oxidase, AChE, BChE and reactive oxygen species (ROS). Whereas, it has been observed to increase the levels of BDNF, GLT-1 and anti-oxidant enzymes, along with protein kinase-A (PKA)-mediated UPS activation. This review aims to discuss the mechanistic interplay of various mediators involved in the neuroprotective effect of harmine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurodegeneration refers to the progressive and irreversible loss of structure or function of neurons, which represents the principal pathological hallmark of neurodegenerative diseases (NDDs) [1, 2]. Neurodegenerative ailments such as Alzheimer’s disease, Huntington’s disease, Parkinson’s disease and Amyotrophic lateral sclerosis stand as prominent contributors to global disability and morbidity [3]. The occurrence of NDDs is progressively increasing around the globe. Approximately 6.2 million individuals aged 65 and above in the United States are currently living with Alzheimer’s disease. Without the emergence of medical advancements to prevent, decelerate, or cure Alzheimer’s disease, this figure could escalate to 13.8 million by 2060 [4]. Furthermore, a 2019 figure states that an estimated 50 million people experienced NDDs leading to dementia globally, and by 2060, that figure is predicted to increase to 152 million [5, 6]. Oxidative stress and neuroinflammation are the key culprits of the pathophysiology that underlies all types of NDDS [7]. Nucleotide-binding domain, leucine-rich–containing family, pyrin domain–containing-3 (NLRP3) inflammasome is a crucial innate immune response regulator that stimulates microglial cells to secrete pro-inflammatory cytokines such as interleukin-1beta (IL-1β) and interleukin-18 (IL-18) which further, leads to neuroinflammation and neurodegeneration [8]. Evidence suggests that inhibiting the NLRP3 inflammasome can increase brain-derived neurotrophic factor (BDNF) expression by suppressing IL-1β [9]. Neurotrophic factors, BDNF have the potential to decelerate neurodegeneration progression, presenting a hopeful avenue for intervening in Alzheimer’s disease [10]. Besides, NLRP3, acetylcholinesterase (AChE) significantly contributes to the development of neurodegenerative disorders by impacting the inflammatory response, apoptosis, oxidative stress, and the aggregation of pathological proteins [11].
Furthermore, evidence suggests that astrocytes play a crucial role in promoting neuronal survival and mitigating the detrimental effects of glutamate [12]. Glutamate transporter subtype 1 (GLT-1) is a crucial regulator of glutamate balance within astrocytes and plays a crucial role in preventing excitotoxic neuronal damage [13]. It has been reported that malfunctioning of GLT-1 protein contributes to neurotoxicity and neurodegeneration [14]. Besides this, the overexpression of the dual-specificity tyrosine phosphorylation-regulated kinase 1 A (DYRK1A) gene, found on chromosome 21q22.2 is overexpressed in Down syndrome. It has a considerable impact on the occurrence of developmental brain abnormalities as well as the onset of neurodegeneration, neuronal decline, and dementia in individuals with Down syndrome [15]. Elevated DYRK1A immunoreactivity has been linked to neurofibrillary tangle pathology in Alzheimer’s disease [16]. Thus, considering these literature reports, directing therapeutic interventions collectively toward the aforementioned cellular mechanisms could offer a promising avenue for treating NDDS.
Harmine is a plant-derived (7-methoxy-1–9 H-pyrido[3,4-b]-indole) beta-carboline alkaloid, firstly isolated from the seeds of Peganum harmala. It is also found in Banisteriopsis caapi and B. metallicolor [17, 18]. Overwhelming evidence suggests that harmine possesses a wide spectrum of pharmacological activity including immunomodulatory, antidiabetic, antioxidant, neuroprotective, anti-inflammatory and antidepressant [19,20,21,22]. According to toxicity studies, harmine has an LD50 of 200 mg/kg when administered subcutaneously to rabbits and 60 mg/kg when administered through the intravenous route to rats and mice [23, 24]. Several in-vitro and in-vivo studies have delineated the neuroprotective effect of harmine through the modulation of different mediators including GLT-1, DYRK1A, BDNF, NLRP3 inflammasome, AChE, butyrylcholinesterase (BChE), pro-inflammatory cytokines and the ubiquitin-proteasome system (UPS) [25,26,27,28,29,30,31] (Tables 1 and 2). However, these reports detailing the neuroprotective effect of harmine have not been consolidated into a single platform. Moreover, the mechanistic interplay of these mediators leading to the neuroprotective effect of harmine has not yet been discussed. Therefore, by utilizing various reports discussing the neuroprotective effect of harmine through the modulation of different mediators, this review article was designed to comprehensively explore the mechanistic interplay among these mediators contributing to the neuroprotective effects of harmine.
Modulation of inflammatory stress-mediated downregulation of GLT-1: impact on glutamate excitotoxicity
GLT-1 is one of the major glutamate transporters primarily expressed in astroglial cells and is responsible for 90% of the total glutamate uptake. It is also crucial for maintaining low extracellular glutamate levels, which prevent glutamate neurotoxicity [13]. GLT-1 primarily transports glutamate, whereas, L-glutamate/L-aspartate transporter (GLAST) transports both glutamate and aspartate [32]. While both GLT-1 and GLAST are expressed in astrocytes, they are found in different regions of the brain and in different cellular compartments within astrocytes. GLT-1 is more abundant in regions like the cortex and hippocampus, whereas GLAST is more abundant in the cerebellum [12]. GLT-1 is better suited for clearing high levels of glutamate from the synaptic cleft during periods of intense neuronal activity, whereas GLAST may play a more significant role in maintaining baseline levels of glutamate [32]. Neuronal loss of the glutamate transporter GLT-1 promotes excitotoxic injury in the hippocampus and cerebral cortex [33, 34]. The dysregulation of astroglial glutamate transporters GLAST and GLT-1 has been linked to various neurodegenerative disorders, such as amyotrophic lateral sclerosis (ALS) and Alzheimer’s disease, where a decrease in GLT-1 protein expression and function has been observed [34, 35]. Overwhelming evidence documented that drugs like dexmedetomidine and ceftriaxone significantly upregulated the expression of GLT-1 protein to confer neuroprotection [36, 37]. Thus, uplifting the expression of neuronal GLT could effectively reduce glutamate excitotoxicity, thereby conferring neuroprotection. In the context of harmine, several animal and cell line reports have studied the role of GLT in the neuroprotective effect of harmine [25, 38,39,40] (Tables 1 and 2). Sun et al. demonstrated that the administration of harmine (30 mg/kg; ip) in global cerebral ischemia (GCI) induced rats, reduced the cerebral infarct volume and neuron death in the cortex region. In Western blot analysis, harmine treatment significantly increased the mRNA and protein expression of GLT-1. In immunofluorescence analysis, harmine treatment downregulated the activation of astrocytes [39]. Building upon this, Meijboom et al. assessed GLT-1 protein level in the P7 spinal cord of untreated and harmine-treated Smn-/-; SMN2 and Smn+/-; SMN2 mice with spinal muscular atrophy. The author revealed that harmine (10 mg/kg) administration significantly increased GLT-1 expression in treated mice as compared to the untreated group of animals [38]. Furthermore, at the preclinical level, it has been established that partial reduction in the GLT-1 levels exacerbates spatial memory deficits [34], whereas upregulation of GLT-1 promotes cognitive functions [41]. Moreover, evidence states that inhibition of the GLT-1 impairs the performance of animals in memory-related tasks [42]. According to findings reported by Zong et al. harmine treatment (30 mg/kg/day for 5 days) dramatically reduced cerebral edema after experimental traumatic brain injury (TBI) and enhanced learning and memory functions. Western blot analysis demonstrated that harmine administration considerably increased the expression of GLT-1 in the hippocampus. Whereas, it reduced the expression levels of IL-1β and caspase-3. Moreover, hematoxylin and eosin staining revealed that harmine suppressed neuronal death in the hippocampal region and improved motor function as evidenced by an increase in neurologic severity score [43]. Evidence states that inflammatory cytokines, such as IL-1β, play a role in the loss of astroglial glutamate transport, thereby contributing to excitotoxic neuronal injury [44]. Taking together these supporting evidences and the aforementioned studies on the neuroprotective effect of harmine, it might be suggested that harmine-mediated upregulation of GLT-1 could be attributed to its anti-inflammatory effect (Fig. 1).
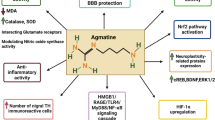
Proposed pathway depicting the molecular modulations produced by harmine that confer neuroprotection. The figure illustrates that harmine’s neuroprotective effects may be mediated through modulation of various pathways: upregulation of GLT-1 through anti-inflammatory action, restoration of BDNF/Trk-B signaling via NLRP3 inflammasome inhibition, activation of the ubiquitin-proteasome system to degrade α-syn and inhibit synphilin-1 aggregation, inhibition of DYRK1A-mediated tau phosphorylation, restoration of APP axonal transport, suppression of Aβ aggregation by AChE inhibition, potentiation of AMPK/Nrf2 antioxidant signaling, and enhancement of mitochondrial respiratory complex activity. (AChE, Acetylcholinesterase; AMPK, Adenosine monophosphate-activated protein kinase; Aβ, Amyloid beta; BDNF, Brain-derived neurotrophic factor; CAT, Catalase; DYRK1A, Dual-specificity tyrosine regulated kinase 1 A; GLAST, L-glutamate/L-aspartate transporter; GLT-1, Glutamate transporter subtype 1; GPx, Glutathione peroxidase; HO1, Heme oxygenase 1; NLRP3, Nucleotide-binding domain, leucine-rich–containing family, pyrin domain–containing-3; NRF2, Nuclear factor erythroid 2-related factor; PKA, Protein kinase-A; ROS, Reactive oxygen species; SOD, Superoxidase; TrkB, Tyrosine-protein kinase-B; UPS, Ubiquitin proteasome system; α-synuclein, alpha-synuclein)
Alongside the GLT-1 upregulating potential of harmine, Li et al., have also explored the GLAST modulatory role of harmine and in vitro cell culture. The primary human cortical neuron-astrocyte co-culture and primary mouse cortex co-culture study showed the harmine (10 µM) treatment significantly increased the expression of both human excitatory amino acid transporter i.e., GLAST and GLT-1. It also uplifted the GLT-1 and GLAST-dependent uptake 48 h after treatment. Moreover, in the transgenic ALS mice model (SOD1G93A mice), harmine (10 mg/kg; ip) treatment significantly increased the GLT-1 protein expression in the cortex region of the brain. An in-vitro assay revealed that harmine (EC50 of 3.2 µM) increased the luciferase activity of CC4 cells through transcriptional regulation and acted as a transcriptional activator of GLT-1 [25]. Furthermore, evidence suggests that besides the modulatory of IL-1β on GLT-1, BDNF has been reported to upregulate the expression of the glutamate transporter GLT-1 in astrocytes [45]. Liu et al. documented that regulation of GLT-1 on hippocampal astrocytes, which accounts for 90% of glutamate reuptake from the synapse, occurs through BDNF-tyrosine protein kinase B (TrkB) signaling in rats exposed to chronic unpredictable stress (CUS) [40]. Additionally, BDNF has also been found to upregulate the expression of GLAST and enhance the uptake of glutamate during hypoxia, which underlies its neuroprotective effects [46]. By using CUS-induced astrocyte dysfunction in mice model, Liu et al. observed the effect of effect of harmine on behavioral parameters along with the GLT-1 and BDNF expression in the hippocampus. Behavioral estimation showed that harmine treatment (20 mg/kg) significantly reduced the immobile duration of mice in the forced swim test and tail suspension test. Moreover, the author also delineated that harmine treatment (20 mg/kg) significantly increased the GLT-1 and BDNF protein expression in the prefrontal cortex and hippocampus region of the brain of the CUS-treated group of mice [40]. Besides this number of other studies utilizing the CUS model have also documented the BDNF protein upregulating effect of harmine [27].
Furthermore, taking inflammatory stress and BDNF together, evidence suggests that inhibiting the NLRP3 inflammasome can increase BDNF expression by suppressing IL-1β [9]. Another study has delineated that inhibiting NLRP3 results in an increased level of BDNF levels and mitigates the decline in cognitive function [47]. Inflammasome is a crucial innate immune response regulator that controls the expression of caspase-1 and inflammatory cytokines during neuroinflammation in NDDS [48, 49]. NLRP3 stimulates the microglia to secrete IL-1β and IL-18, which further promote neuroinflammation, thus leading to neurodegenerative disorders [8, 50]. Liu et al. evaluated the protective effect of harmine in in-vivo (streptozotocin (STZ) treated mice) and in-vitro (HG-treated SH-SY5Y cells). In-vivo examination showed that harmine (20 mg/kg; po) treatment ameliorated the STZ-induced learning and memory impairment as evidenced by reduced swimming distance, escape latency and increased number of platform crossings in the Morris water maze. An immunohistology study indicated that harmine treatment significantly decreased the level of NLRP3, caspase-1 and IL-1β. Whereas, harmine-treated mice exhibited higher levels of BDNF protein and phosphorylated TrkB in diabetes mellitus rats. Moreover, western blot analysis revealed that harmine (1 µM) inhibited NLRP3 inflammasome activation and enhanced the expression of BDNF protein, as well as elevated the BDNF/TrkB signaling pathway in HG-treated neuronal cells [28]. Conclusively, the aforementioned evidence indicates that harmine may exert its neuroprotective effect by restoring the expression of GLT-1 on astrocytes through inhibition of the NLRP3 inflammasome-mediated downregulation of BDNF/Trk-B signaling (Fig. 1).
Facilitation of α-Synuclein degradation via protein kinase A (PKA)-mediated ubiquitin-proteasome system activation
PKA is a Ser/Thr kinase that is crucial for sustaining key neural operations such as mitochondrial homeostasis, neural proliferation, bioenergetics, and neurotransmission [51]. Within neurons, PKA governs various facets of mitochondrial functions, such as fostering interconnectivity among mitochondria, facilitating forward mitochondrial movement in dendrites, and regulating mitophagy [52]. Research employing a cell culture model of Parkinson’s disease revealed that mitochondrial PKA phosphorylates serine 637 on the mitochondrial fission regulator Drp1 in human Drp1 isoform 1. This phosphorylation suppresses mitochondrial fission, fostering neuroprotection against glutamate excitotoxicity and oxidative stress in the context of Parkinson’s disease in cell culture [53]. UPS is a sizable multi-catalytic proteinase complex that is present in the nucleus and cytoplasm of eukaryotic cells. The primary function of the UPS is the destruction of damaged, mutated, misfolded, or unfolded intracellular proteins [54]. Evidence delineates that alpha-synuclein (α-syn) can be degraded by both autophagy and the ubiquitin-proteasome system (UPS) [55]. Various studies revealed that malfunctioning and impairment of UPS leads to abnormal protein buildup or aggregation of α-syn [56,57,58,59]. Cai-C et al. demonstrated that harmine (10 µM) significantly reduced the doxycycline-induced over-expression of α-syn in Tet-on PC12 neuronal cells. Western blot analysis revealed that harmine (10 µM) significantly degraded the WT, A53T and A30P mutant of α-syn and promoted the clearance of over-expressed α-syn. Furthermore, to find the mode of degradation of α-syn by harmine, authors used autophagy inhibitor (SAR405) or the small interfering RNA (siRNA) of autophagy-related genes (ATG7 and ATG5) and ubiquitin-proteasome pathway inhibitors (MG132 and bortezomib). Western blot analysis showed that neither autophagy inhibitors nor siRNA of autophagy-related genes had any significant effect on the harmine (10µM) induced degradation of α-syn. Whereas, ubiquitin-proteasome pathway inhibitors significantly abrogated the harmine (10 µM) induced degradation of α-syn. Thus, delineating that harmine-induced degradation of α-syn is mediated through the UPS-dependent manner rather than the autophagy-lysosomal pathway [31]. Evidence states that α-syn aggregation is also enhanced by its interacting protein called synphilin-1 [60]. Cai-C et al. also assessed the effect of harmine on synphilin-1 aggregation by utilizing Tet-on inducible PC12 cells transfected with GFP-synphilin-1 plasmids and with 2 µg/ml doxorubicin for 48 h. Outcomes showed that harmine treatment for 24 h significantly reduced the aggregation of GFP-synphilin-1. Whereas, a proteasome inhibitor, MG132 abrogated this varied effect of harmine, delineating that harmine also inhibits synphilin-1 aggregation through the ubiquitin-proteasome system [31]. Furthermore, the level of PKA and its role in modulating the UPS pathway was studied in the aforementioned study. PKA is known to regulate the Ubiquitin Proteasome system. Activation of PKA can modulate the UPS by phosphorylating various proteins involved in the pathway, thereby affecting protein degradation [61, 62]. In PC12 cells, harmine promoted PKA phosphorylation at Thr197. q-PCR analysis showed that harmine upregulated the expression of proteasome 26 S subunit non-ATPase 1 (PSMD1) mRNA (one of the 40 subunits of proteasomes). Whereas, pretreatment with PKA inhibitor, H89 significantly abrogated the harmine-induced PKA phosphorylation, α-syn clearance and proteasome activity [31]. Overall, these studies delineate that harmine could potentially facilitate the degradation of α-syn by activating the ubiquitin-proteasome system through PKA mediation. Moreover, it also inhibits synphilin-1 aggregation via UPS (Fig. 1).
Impact of harmine, a DYRK1A inhibitor, on tau expression and phosphorylation
DYRK1A is an evolutionary protein kinase, a member of the family of Dual- Specificity Tyrosine- Regulated kinase (DYRK) [63]. Overwhelming evidence highlighted that overexpression of DYRK1A leads to neurodevelopmental delay, motor abnormalities and cognitive deficits [64, 65]. Likewise, it has been shown that overexpression of DYRK1A results in neuroinflammation by promoting the release of inflammatory cytokines, thus promoting the progression of neurodegenerative disease [66,67,68]. In addition, elevated DYRK1A immunoreactivity has been linked to neurofibrillary tangles in Alzheimer’s disease (16), 3R- tau expression in Down Syndrome mice [69] and impairment of hippocampal-dependent memory in DYRK1A BAC transgenic mice [70]. Several pieces of evidence have documented the DYRK1A inhibitory potential of harmine [71,72,73] (Table 2). Till now many reports have discussed its potential against different NDDS as a DYRK1A inhibitor [26, 69, 74,75,76]. It has been well established that the accumulation of phosphorylated tau leads to synaptic dysfunction, neuronal impairment, and the formation of neurofibrillary tangles, thereby contributing to neurodegenerative processes [77]. Frost et al. delineated that harmine (0.8 µM and 8 µM) significantly reduced the expression of all three phosphorylated forms of tau protein (12E8, pT231 and pS396). Moreover, it also inhibited the DYRK1A-catalyzed direct phosphosphorylation of tau protein on serine 396 (pS396) with an IC50 of 0.7 µM in H4 neuroglioma cells [26]. Furthermore, research findings indicate that Dyrk1A induces the exclusion of tauE10, thereby resulting in elevated levels of 3R-tau and an imbalance between 3R-tau and 4R-tau within the brain of individuals with Down syndrome [74]. Yin et al. explored the potential of DYRK1A inhibitor, harmine in maintaining the 4R-tau/3R-tau ratio in human neuronal progenitor cells. The author stated that harmine (20 µM) suppressed the expression of 3R-tau and promoted the expression of 4R-tau and led to the increase in 4R-tau/3R-tau ratio at both mRNA and protein levels in retinoid acid (10 µM) differentiated human neuronal progenitor cells [69]. In addition to this, Sitz et al. reported that harmine (1 µM) inhibited the DYRK1A -dependent phosphorylation of SF3b1 at Thr434 and prevented the mobility shift of the cytoplasmic SEPT4 substrate of Dyrk1A in doxycycline-treated EGFP-DYRK1A overexpressed HEK293 cells [74]. In Parkinson’s disease (PD), the aggregation of Lewy bodies frequently entails the sequestration of Septin4 (Sept4), a polymerizing scaffold protein [78]. SF3B1 has been previously identified as a specific target site of DYRK1A [79].
Furthermore, evidence delineates that a compound possessing dual inhibitory properties against glycogen synthase kinase-3 beta (GSK3β) and DYRK1A effectively decreases Tau hyperphosphorylation and improves conditions in Alzheimer’s disease models [80]. Liu et al. explored the potential of harmine derivatives as potent dual inhibitors of DYRK1A/GSK-3β for Alzheimer’s treatment by employing okadaic acid-induced SH-SY5Y cells. The author reported that among the various derivatives of harmine, ZDWX-25 (1-(Cyclopropanecarboxamido)-9 H-pyrido (3,4-b)indole-7-carboxylic acid methyl ester) showed a potent inhibitory effect on DYRK1A and GSK-3β with IC50 values of 103 and 71 nM, respectively in kinase-Glo luminescent assay. Moreover, western blot analysis revealed that ZDWX-25 inhibited the okadaic acid-induced hyperphosphorylation of tau protein in SH-SY5Y cells. In-silico analysis showed that ZDWX-25 could better interact with Lys85 and Val135 residues of the ATP binding pocket of GSK-3β (4PTC) and Leu241 and Lys188 residues of the ATP binding pocket of DYRK1A (3ANR) with hydrogen bonding. Besides that, ZDWX-25 (20 and 30 mg/kg) showed good blood-brain barrier penetrability (Pe > 4.7 × 10− 6 cm/s). Whereas, the in-vivo analysis revealed that ZDWX-25 improved the learning and memory in amyloid precursor protein/presenilin 1/Tau (APP/PS1/Tau) transgenic mice [75]. Overall evidence delineates that harmine inhibits the DYRK1A-catalyzed phosphorylation of tau protein, which might be the reason for the improvement of learning and memory (Fig. 1).
Evidence states that axonal defects in Alzheimer’s disease affect the intracellular distribution of amyloid precursor protein (APP) and the extent to which it is exposed to amyloid beta (Aβ) peptide [81]. Bessone et al. investigated that harmine modulated APP axonal transport by inhibiting DYRK1A in human induced pluripotent stem cells. Photomicrographs of human-derived neuronal cells treated with harmine (7.5 µM) or by overexpressing the negative DYRK1A showed a reduction in the axonal APP vesicle density and upregulated the processivity of retrograde APP [76]. Thus, delineating that harmine might restore the APP axonal transport by inhibiting the DYRK1A.
Inhibition of cholinesterase activity by harmine: in-vitro and in-vivo evidence
AChE is a crucial enzyme in the cholinergic nervous system, which facilitates the hydrolysis of acetylcholine into choline and acetate ions [82, 83]. Acetylcholinesterase disrupts the function of acetylcholine, contributing to symptomatic cognitive impairment observed in patients with Alzheimer’s disease [84, 85]. Several earlier studies have elucidated an effective strategy for enhancing cognitive function and providing neuroprotection through the inhibition of the acetylcholinesterase enzyme [86, 87]. Jyothi et al. performed the in-silico analysis to study the binding affinity of harmine at AChE and BChE. Outcomes delineated that harmine showed a good binding affinity with AChE (5FPQ) and BChE (2Y1K). Harmine exhibited a one hydrogen bond interaction with the glutamate 199 amino acid residue of AChE and showed a binding energy of -8.4 Kcal/mol. Whereas in the case of BChE, harmine showed one hydrogen bond interaction with glycine 115 residue. This complex exhibited a binding energy of -7.9 Kcal/mol [88]. Besides this, researchers have also evaluated the in-vitro and in-vivo AChE and BChE inhibitory potential of harmine derivatives [29, 89,90,91]. Liu et al. evacuated that, ZLWH-23, a derivative of harmine containing N-benzyl-piperidine moiety exhibited potent AChE, BChE and GSK3B inhibitory activity with an IC50 value of 0.27, 20.82 and 6.78 µM, respectively. Along with this, it also reduced tau hyperphosphorylation of tau at Ser-396 in Tau (P301L) 293T cells [89]. Moreover, Filali et al., explored the in vitro AChE inhibitory potential of harmine using an enzymatic assay. Harmine derivative, harmine 1 (7-methoxy-1-methyl-9 H-pyrido (3,4–6) indole) significantly inhibited the AChE enzyme, with an IC50 value of 10.4 µM in comparison to the standard galanthamine with IC50 value of 4.1 µM [29]. Biochemical studies have shown that AChE triggers the formation of amyloid fibrils, leading to the creation of highly toxic AChE-Aβ complexes [92, 93]. In consistence with the above findings, Du et al. also showed the Aβ aggregation and acetylcholinesterase inhibitory activity of novel derivatives of harmine. By employing Ellman’s assay, authors revealed that many of the harmine derivatives modified at position 9 with benzyl piperazinyl showed greater inhibitory activity against hAChE than standard donepezil. Furthermore, by using the Thioflavin-T (ThT) fluorescence assay, the author demonstrated that the two compounds 13 and 17a (Check ref. 95 for structure and properties) displayed significant inhibition of Aβ1–42 aggregation with an IC50 value of 9.31 and 6.74 µM respectively, which were less than that of resveratrol (IC50 11.51 µM) and curcumin (IC50 15.47 µM) standards [94]. Besides the in-silico and in-vitro AChE inhibitory potential of harmine, there have been studies that explored the in-vivo AChE inhibitory potential of harmine [90, 91]. Furthermore, He et al. delineated that harmine potentiates acetylcholine transmission by inhibiting the AChE enzyme. Harmine treatment (20 mg/kg; oral gavage for 2 weeks) ameliorated the scopolamine-induced impairment of spatial memory in C57BL/6 mice. Moreover, by utilizing the APP/PS1 chronic mice model, authors explored the effect of long-term treatment of harmine on memory. Harmine (20 mg/kg) treatment for 10 weeks also exhibited a slight improvement in memory. Biochemical analysis showed that harmine significantly inhibited the APP/PS1-induced increase in AChE activity in the cerebral cortex region [90]. Other than the APP/PS1 model, Li et al. demonstrated the AChE inhibitory potential of harmine in the scopolamine mice model. Harmine treatment (30 mg/kg) significantly abrogated the scopolamine-induced cognitive impairment. It decreased and increased the AChE and choline acetyltransferase (ChAT) activity, respectively [91]. Overall, these studies suggest that harmine might inhibit Aβ aggregation by suppressing AChE activity (Fig. 1).
Boosting AMPK/Nrf2 pathway and optimizing mitochondrial respiratory complexes
Free radicals, also known as reactive anions or molecules with oxygen atoms, such as superoxide, hydroxyl radical and hydrogen peroxide [95]. Reactive oxygen species (ROS)-triggered oxidative stress can harm cells by inhibiting the activity of the number of enzymes and by oxidizing the lipids [96, 97]. In the realm of neurodegeneration, oxidative stress is a crucial contributor to the development of several neurological disorders. Neurons, in particular, are highly susceptible to oxidative harm because of their elevated metabolic activity, rich lipid accumulation, and comparatively modest antioxidant defenses relative to other cell types in the body [98]. Till now several studies have demonstrated the oxidative stress-relieving effect of harmine at different dose levels through different pathways [91, 99,100,101] (Table 1). The recognition of oxidative stress-induced neurotoxicity is growing as a significant neuropathological mechanism contributing to the motor and behavioral symptoms linked with Huntington’s disease [102]. Furthermore, Jain et al., showed that harmine exerts a protective effect against Huntington’s disease by inhibiting aggregation of mutant huntingtin fragment (103Q-htt) through its antioxidant potential in a yeast model. This study on yeast cells (S. cerevisiae BY4742) revealed that harmine (25 µg/ml) significantly increased the cell viability and reduced the aggregation of 103Q-htt protein. Moreover, the authors also stated that harmine only reduces the level of ROS when it exceeds a certain limit in yeast cells expressing 25Q-htt. Whereas, harmine had no significant effect on the basal ROS level. The aggregation of 103Q-htt uplifted the generation of ROS. Thus, delineating that harmine reduces huntingtin protein aggregation, resulting in the reduction of oxidative stress that slows down intracellular protein aggregation [100]. The transcription factor known as nuclear factor E2-related factor 2 (Nrf2) reacts to oxidative stress by attaching itself to the antioxidant response element (ARE) located within the promoter region of genes responsible for encoding antioxidant enzymes [103]. Reports have also demonstrated that adenosine monophosphate-activated protein kinase (AMPK) can directly phosphorylate Nrf2. Within cellular contexts, it has been observed that the activation of AMPK induces the migration and aggregation of the transcription factor Nrf2 into the nucleus [104, 105]. A study by Habib et al. demonstrated that harmine treatment (10 mg/kg) alleviates 3-Nitropropionic acid-induced motor, cognitive and histological dysfunction by inhibiting oxidative stress/neurotoxicity in male Wistar rats. Western blot analysis revealed that harmine significantly increased the protein level of Nrf2, AMPK and p21 and the gene expression of haem oxygenase-1 (HO1), quinone oxidoreductase-1 and p62 in the striatum, prefrontal cortex and hippocampus region of the rat brain [101]. Nrf2, functioning as a pivotal regulatory factor, governs the transcription of numerous enzymatic antioxidants, thereby influencing the modulation of ROS levels, including superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and HO1. These antioxidants play crucial roles in preserving redox equilibrium and cellular stability [106]. Reus et al. evaluated the antioxidant potential of harmine in the prefrontal cortex and hippocampus of rats. The authors showed that acute and chronic administration of harmine (5, 10 and 15 mg/kg; ip) reduced the lipid and protein peroxidation in the prefrontal cortex and hippocampus region of the rat brain. Whereas, it increased the SOD and CAT activity [99]. In the scopolamine-induced cognitive dysfunctioning mice model, Li et al. showed the cognition-improving effect of harmine through the modulation of oxidative stress and AChE activity. Authors delineated that harmine significantly uplifted the SOD (10 and 20 mg/kg) and GPx levels (30 mg/kg). Whereas, it reduced the production of maleic dialdehyde (20 and 30 mg/kg) and AChE activity (30 mg/kg) [91].
Besides AMPK/NRF2 antioxidant signaling, nicotinamide adenine dinucleotide hydrogen (NADH) dehydrogenase (complex I) and cytochrome c oxidase (complex IV) contribute greatly to oxidative stress by increasing ROS production, ATP depletion and lactic acidosis [107, 108]. Acute treatment with harmine (10, 20 and 30 mg/kg) in rats significantly increased creatine kinase activity in the prefrontal cortex region. Moreover, chronic treatment of harmine at 20 mg/kg (for 14 days) also increased creatine kinase activity in the striatum of the rat brain. The author also analyzed the mitochondrial respiratory complex activity and demonstrated that chronic treatment with harmine at 5 mg/kg increased NADH dehydrogenase (complex I) and cytochrome c oxidase (complex IV) activity in the mitochondrion of the prefrontal cortex and striatum, respectively. Whereas, acute treatment with 10 and 15 mg/kg of harmine uplifted the complex I activity in the striatum and prefrontal cortex regions, respectively. Additionally, a 20 mg/kg dose of harmine also uplifted the complex II activity in the mitochondrion of the prefrontal cortex [109]. Overall, these supporting and direct reports delineate that harmine might also confer neuroprotection by potentiating the AMPK/Nrf2 antioxidant signaling pathway and enhancing the activity of mitochondrial respiratory complexes. An increase in the activity of mitochondrial respiratory complexes might also be the reason for the harmine-mediated reduction in ROS production (Fig. 1). Furthermore, this reduction in the ROS might also be linked to the monoamine oxidase (MAO) inhibitory potential of harmine. MAO is an enzyme that plays a crucial role in the metabolism of neurotransmitters such as serotonin, dopamine, and norepinephrine. It catalyzes the oxidation of these neurotransmitters, producing hydrogen peroxide (H2O2) and other ROS as byproducts, leading to increased oxidative stress [110]. So far, several reports have documented harmine’s monoamine oxidase-A (MAO-A) inhibitory potential [111, 112]. Evidence also suggests that harmine possesses both antidepressant and anti-inflammatory properties [113]. MAO-A inhibitors have been utilized for many decades in the treatment of depression, while MAO-B inhibitors are employed in Parkinson’s disease therapy [114]. Taken together, these studies suggest that harmine-mediated reduction in oxidative stress might also be attributed to its MAO inhibitory potential.
Besides the reports discussing the neuroprotective potential of β-carboline harmine, however, there have been studies delineating the neurotoxic effects of β-carbolines [115,116,117,118]. A report has delineated that harmine induces hypothermia and tremor, which serve as measures of neurotoxicity in rodent models of neurodegenerative disorders [115]. This piece of evidence also stated that human CYP2D6 in the brain is essential to neutralize the harmine-induced neurotoxic effect. A 4-h intracerebroventricular pre-exposure to the CYP2D inhibitor propranolol amplified harmine-triggered hypothermia and tremors in transgenic mice expressing humanized CYP2D6 [115]. In addition, Sun et al. tried to explore the neurotoxic mechanism of harmine in Caenorhabditis elegan. The study’s findings indicated that harmine has the potential to directly impede the activity of acetylcholinesterase, resulting in the excessive buildup of acetylcholine, which could represent one of the mechanisms underlying harmine-induced neurotoxicity [116]. Furthermore, other β-carbolines such as harmane and norharmane are also reported to be neurotoxic [117, 118]. By utilizing E17 rat primary midbrain cultures, the authors tested the dopaminergic and non-dopaminergic neurotoxicity induced by harmane and norharmane. The outcomes revealed that concentrations of harmane and norharmane ranging from 100 nM to 5 µM were found to be neurotoxic, as evidenced by the reduced percentage of dopaminergic neurons [117]. Moreover, treatment with norharmane in cultured PC12 cells resulted in mitochondrial dysfunction and an elevation in the number of caspase-3 and TUNEL-positive cells [118].
Conclusion
In conclusion, the comprehensive evidence suggests that harmine exerts its neuroprotective effects through multiple mechanisms. Firstly, it may restore the expression of GLT-1 on astrocytes by inhibiting the NLRP3 inflammasome-mediated downregulation of BDNF/Trk-B signaling. Additionally, harmine could potentially facilitate the degradation of α-syn and inhibit synphilin-1 aggregation via the ubiquitin-proteasome system, mediated by PKA. Furthermore, it inhibits DYRK1A-catalyzed phosphorylation of tau protein, potentially contributing to improvements in learning and memory. Moreover, harmine might confer neuroprotection by activating the AMPK/Nrf2 antioxidant signaling pathway and enhancing the activity of mitochondrial respiratory complexes, thereby reducing ROS production. These findings collectively highlight the multifaceted neuroprotective properties of harmine. This review will serve as a valuable resource for directing future researchers toward delving deeper into the mechanistic aspects of harmine, facilitating the discovery of promising lead compounds. While preclinical research has provided valuable insights, further investigation, particularly in human subjects, is necessary to validate these effects and determine their potential therapeutic relevance in clinical settings. Moreover, the translation of these findings into viable therapeutic interventions could encounter challenges pertaining to pharmacokinetics, dosing, and potential adverse effects, all of which warrant further examination in future studies.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Amor S, Puentes F, Baker D, Van Der Valk P. Inflammation in neurodegenerative diseases. J Immunol. 2010;129(2):154–69.
Dugger BN, Dickson DW. Pathology of neurodegenerative diseases. CSH Perspect Biol. 2017;9(7):a028035.
Teleanu DM, Niculescu AG, Lungu II, Radu CI, Vladâcenco O, Roza E, et al. An overview of oxidative stress, neuroinflammation, and neurodegenerative diseases. Int J Mol Sci. 2022;23(11):5938.
2021 Alzheimer’s disease facts and figures. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 2021;17(3), 327–406.
Onohuean H, Akiyode AO, Akiyode O, Igbinoba SI, Alagbonsi AI. Epidemiology of neurodegenerative diseases in the East African region: a meta-analysis. Front Neurol. 2022;13:1024004.
Armstrong R. What causes neurodegenerative disease? Folia Neuropathol. 2020;58(2):93–112.
Rekatsina M, Paladini A, Piroli A, Zis P, Pergolizzi JV, Varrassi G. Pathophysiology and therapeutic perspectives of oxidative stress and neurodegenerative diseases: a narrative review. Adv Ther. 2020;37:113–39.
Ren C, Chen M, Mu G, Peng S, Liu X, Ou C. NLRP3 inflammasome mediates neurodegeneration in rats with chronic neuropathic pain. Shock: Injury, inflammation, and Sepsis. Clin Lab. 2021;56(5):840–9.
Fu Q, Li J, Qiu L, Ruan J, Mao M, Li S, et al. Inhibiting NLRP3 inflammasome with MCC950 ameliorates perioperative neurocognitive disorders, suppressing neuroinflammation in the hippocampus in aged mice. Int Immunopharmacol. 2020;82:106317.
Chen AI, Xiong LJ, Tong YU, Mao M. The neuroprotective roles of BDNF in hypoxic ischemic brain injury. Biomed Rep. 2013;1(2):167–76.
Walczak-Nowicka ŁJ, Herbet M. Acetylcholinesterase inhibitors in the treatment of neurodegenerative diseases and the role of acetylcholinesterase in their pathogenesis. Int J Mol Sci. 2021;22(17):9290.
Todd AC, Hardingham GE. The regulation of astrocytic glutamate transporters in health and neurodegenerative diseases. Int J Mol Sci. 2020;21(24):9607.
Maragakis NJ, Dietrich J, Wong V, Xue H, Mayer-Proschel M, Rao MS, et al. Glutamate transporter expression and function in human glial progenitors. Glia. 2004;45(2):133–43.
Lauderback CM, Hackett JM, Huang FF, Keller JN, Szweda LI, Markesbery WR, et al. The glial glutamate transporter, GLT-1, is oxidatively modified by 4‐hydroxy‐2‐nonenal in the Alzheimer’s disease brain: the role of Aβ1–42. J Neurochem. 2001;78(2):413–6.
Wegiel J, Gong CX, Hwang YW. The role of DYRK1A in neurodegenerative diseases. FEBS J. 2011;278(2):236–45.
Wegiel J, Dowjat K, Kaczmarski W, Kuchna I, Nowicki K, Frackowiak J, et al. The role of overexpressed DYRK1A protein in the early onset of neurofibrillary degeneration in Down syndrome. Acta Neuropathol. 2008;116(4):391–407.
Patel K, Gadewar M, Tripathi R, Prasad SK, Patel DK. A review on medicinal importance, pharmacological activity and bioanalytical aspects of beta-carboline alkaloid Harmine. Asian Pac J Trop Biomed. 2012;2(8):660–4.
Moloudizargari M, Mikaili P, Aghajanshakeri S, Asghari MH, Shayegh J. Pharmacological and therapeutic effects of Peganum harmala and its main alkaloids. Pharmacogn Rev. 2013;7(14):199.
Al-shaibani MB, Al-mafrachi HT. Antitumor and Immunomodulatory activities of Peganum harmala extracts. J Biotechnol Res. 2013;7(1):11–20.
Waki H, Park KW, Mitro N, Pei L, Damoiseaux R, Wilpitz DC, et al. The small molecule harmine is an antidiabetic cell-type-specific regulator of PPARγ expression. Cell Metab. 2007;5(5):357–70.
Ferraz CA, de Oliveira Junior RG, Picot L, da Silva Almeida JR, Nunes XP. Pre-clinical investigations of β-carboline alkaloids as antidepressant agents: a systematic review. Fitoterapia. 2019;137:104196.
Zhang L, Li D, Yu S. Pharmacological effects of harmine and its derivatives: a review. Arch Pharm Res. 2020;43:1259–75.
Mahmoudian M, Salehian P, Jalilpour H. Toxicity of Peganum harmala: review and a case report. Iran J Pharmacol Ther. 2002;1:1–4.
Brito-da-Costa AM, Dias-da-Silva D, Gomes NG, Dinis-Oliveira RJ, Madureira-Carvalho Á. Toxicokinetics and toxicodynamics of ayahuasca alkaloids N, N-dimethyltryptamine (DMT), harmine, harmaline and tetrahydroharmine: clinical and forensic impact. J Pharm. 2020;13(11):334.
Li Y, Sattler R, Yang EJ, Nunes A, Ayukawa Y, Akhtar S, et al. Harmine, a natural beta-carboline alkaloid, upregulates astroglial glutamate transporter expression. J Neuropharmacol. 2011;60(7–8):1168–75.
Frost D, Meechoovet B, Wang T, Gately S, Giorgetti M, Shcherbakova I, et al. β-carboline compounds, including harmine, inhibit DYRK1A and tau phosphorylation at multiple Alzheimer’s disease-related sites. PLoS ONE. 2011;6(5):e19264.
Fortunato JJ, Réus GZ, Kirsch TR, Stringari RB, Fries GR, Kapczinski F, et al. Effects of β-carboline harmine on behavioral and physiological parameters observed in the chronic mild stress model: further evidence of antidepressant properties. Brain Res Bull. 2010;81(4–5):491–6.
Liu P, Li H, Wang Y, Su X, Li Y, Yan M, et al. Harmine ameliorates cognitive impairment by inhibiting NLRP3 inflammasome activation and enhancing the BDNF/TrkB signaling pathway in STZ-induced diabetic rats. Front Pharmacol. 2020;11:535.
Filali I, Bouajila J, Znati M, Bousejra-El Garah F, Ben Jannet H. Synthesis of new isoxazoline derivatives from harmine and evaluation of their anti-Alzheimer, anti-cancer and anti-inflammatory activities. J Enzyme Inhib Med Chem. 2015;30(3):371–6.
Jin SJ, Song Y, Park HS, Park KW, Lee S, Kang H. Harmine Inhibits Multiple TLR-Induced Inflammatory Expression through Modulation of NF-κB p65, JNK, and STAT1. Life. 2022;12(12):2022.
Cai CZ, Zhou HF, Yuan NN, Wu MY, Lee SMY, Ren JY, et al. Natural alkaloid harmine promotes degradation of alpha-synuclein via PKA-mediated ubiquitin-proteasome system activation. Phytomed. 2019;61:152842.
Pajarillo E, Rizor A, Lee J, Aschner M, Lee E. The role of astrocytic glutamate transporters GLT-1 and GLAST in neurological disorders: potential targets for neurotherapeutics. Neuropharmacol. 2019;161:107559.
Rimmele TS, Li S, Andersen JV, Westi EW, Rotenberg A, Wang J, et al. Neuronal loss of the glutamate transporter GLT-1 promotes excitotoxic injury in the hippocampus. Front Cell Neurosci. 2021;15:788262.
Mookherjee P, Green PS, Watson G, Marques MA, Tanaka K, Meeker KD, et al. GLT-1 loss accelerates cognitive deficit onset in an Alzheimer’s disease animal model. JAD. 2011;26(3):447–55.
Dumont AO, Goursaud S, Desmet N, Hermans E. Differential regulation of glutamate transporter subtypes by pro-inflammatory cytokine TNF-α in cortical astrocytes from a rat model of amyotrophic lateral sclerosis. PLoS ONE. 2014;9(5):e97649.
Peng M, Ling X, Song R, Gao X, Liang Z, Fang F, et al. Upregulation of GLT-1 via PI3K/Akt pathway contributes to neuroprotection induced by dexmedetomidine. Front Neurol. 2019;10:1041.
Cui C, Cui Y, Gao J, Sun L, Wang Y, Wang K, et al. Neuroprotective effect of ceftriaxone in a rat model of traumatic brain injury. Neurol Sci. 2014;35(4):695–700.
Meijboom KE, Volpato V, Monzón-Sandoval J, Hoolachan JM, Hammond SM, Abendroth F et al. Combining multiomics and drug perturbation profiles to identify muscle-specific treatments for spinal muscular atrophy. JCI Insight 2021;6(13).
Sun P, Zhang S, Li Y, Wang L. Harmine mediated neuroprotection via evaluation of glutamate transporter 1 in a rat model of global cerebral ischemia. Neurosci Lett. 2014;583:32–6.
Liu F, Wu J, Gong Y, Wang P, Zhu L, Tong L, et al. Harmine produces antidepressant-like effects via restoration of astrocytic functions. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79:258–67.
Ramandi D, Elahdadi Salmani M, Moghimi A, Lashkarbolouki T, Fereidoni M. Pharmacological upregulation of GLT-1 alleviates the cognitive impairments in the animal model of temporal lobe epilepsy. PLoS ONE. 2021;16(1):e0246068.
Tian SW, Yu XD, Cen L, Xiao ZY. Glutamate transporter GLT1 inhibitor dihydrokainic acid impairs novel object recognition memory performance in mice. Physiol Behav. 2019;199:28–32.
Zhong Z, Tao Y, Yang H. Treatment with harmine ameliorates functional impairment and neuronal death following traumatic brain injury. Mol Med Rep. 2015;12(6):7985–91.
Prow NA, Irani DN. The inflammatory cytokine, interleukin-1 beta, mediates loss of astroglial glutamate transport and drives excitotoxic motor neuron injury in the spinal cord during acute viral encephalomyelitis. J Neurochem. 2008;105(4):1276–86.
Rodriguez-Kern A, Gegelashvili M, Schousboe A, Zhang J, Sung L, Gegelashvili G. Beta-amyloid and brain-derived neurotrophic factor, BDNF, up-regulate the expression of glutamate transporter GLT-1/EAAT2 via different signaling pathways utilizing transcription factor NF-κB. Neurochem Int. 2003;43(4–5):363–70.
Dai M, XIA XB, XIONG SQ. BDNF regulates GLAST and glutamine synthetase in mouse retinal Müller cells. J Cell Physiol. 2012;227(2):596–603.
Ward R, Li W, Abdul Y, Jackson L, Dong G, Jamil S, et al. NLRP3 inflammasome inhibition with MCC950 improves diabetes-mediated cognitive impairment and vasoneuronal remodeling after ischemia. Pharmacol Res. 2019;142:237–50.
Guan Y, Han F. Key mechanisms and potential targets of the NLRP3 inflammasome in neurodegenerative diseases. Front Integr Neurosci. 2020;14:37.
Heneka MT, Kummer MP, Stutz A, Delekate A, Schwartz S, Vieira-Saecker A, et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493(7434):674–8.
Hung WL, Ho CT, Pan MH. Targeting the NLRP3 inflammasome in neuroinflammation: health promoting effects of dietary phytochemicals in neurological disorders. Mol Nutr Food Res. 2020;64(4):1900550.
Zhang J, Feng J, Ma D, Wang F, Wang Y, Li C, et al. Neuroprotective mitochondrial remodeling by AKAP121/PKA protects HT22 cell from glutamate-induced oxidative stress. Mol Neurobiol. 2019;56(8):5586–607.
Dagda RK, Gusdon AM, Pien I, Strack S, Green S, Li C, et al. Mitochondrially localized PKA reverses mitochondrial pathology and dysfunction in a cellular model of Parkinson’s disease. Cell Death Differ. 2011;18(12):1914–23.
Merrill RA, Dagda RK, Dickey AS, Cribbs JT, Green SH, Usachev YM, et al. Mechanism of neuroprotective mitochondrial remodeling by PKA/AKAP1. PLoS ONE. 2011;6(4):e1000612.
Moore DJ, Dawson VL, Dawson TM. Role for the ubiquitin-proteasome system in Parkinson’s disease and other neurodegenerative brain amyloidoses. Neuromol Med. 2003;4(1–2):95–108.
Webb JL, Ravikumar B, Atkins J, Skepper JN, Rubinsztein DC. α-Synuclein is degraded by both autophagy and the proteasome. J Bio Chem. 2003;278(27):25009–13.
Kumar V, Singh D, Singh BK, Singh S, Mittra N, Jha RR, et al. Alpha-synuclein aggregation, ubiquitin proteasome system impairment, and L-Dopa response in zinc-induced parkinsonism: resemblance to sporadic Parkinson’s disease. Mol Cell Biochem. 2018;444(1–2):149–60.
McNaught KS, Jenner P. Proteasomal function is impaired in substantia nigra in Parkinson’s disease. Neurosci Lett. 2001;297(3):191–4.
Ebrahimi-Fakhari D, Cantuti-Castelvetri I, Fan Z, Rockenstein E, Masliah E, Hyman BT, et al. Distinct roles in vivo for the ubiquitin–proteasome system and the autophagy–lysosomal pathway in the degradation of α-synuclein. J Neurosci. 2011;31(41):14508–20.
McKinnon C, De Snoo ML, Gondard E, Neudorfer C, Chau H, Ngana SG, et al. Early-onset impairment of the ubiquitin-proteasome system in dopaminergic neurons caused by α-synuclein. Acta Neuropatholo Commun. 2020;8(1):17.
Alvarez-Castelao B, Castaño JG. Synphilin-1 inhibits alpha-synuclein degradation by the proteasome. Cell Mol Life Sci. 2011;68(15):2643–54.
Yaku K, Matsui-Yuasa I, Kojima-Yuasa A. 1′-Acetoxychavicol acetate increases Proteasome Activity by activating cAMP-PKA signaling. Planta Med. 2018;84(03):153–9.
Myeku N, Wang H, Figueiredo-Pereira ME. cAMP stimulates the ubiquitin/proteasome pathway in rat spinal cord neurons. Neurosci Lett. 2012;527(2):126–31.
Yang Y, Fan X, Liu Y, Ye D, Liu C, Yang H et al. Function and inhibition of DYRK1A: emerging roles of treating multiple human diseases. Biochem Pharmacol 2023;115521.
Altafaj X, Dierssen M, Baamonde C, Martí E, Visa J, Guimerà J, et al. Neurodevelopmental delay, motor abnormalities and cognitive deficits in transgenic mice overexpressing Dyrk1A (minibrain), a murine model of Down’s syndrome. Hum Mol Genet. 2001;10(18):1915–23.
Duchon A, Herault Y. DYRK1A, a dosage-sensitive gene involved in neurodevelopmental disorders, is a target for drug development in Down syndrome. Front Behav Neurosci. 2016;10:104.
Lee HJ, Hoe HS. Inhibition of CDK4/6 regulates AD pathology, neuroinflammation and cognitive function through DYRK1A/STAT3 signaling. Pharmacolo Res. 2023;190:106725.
Araldi GL, Hwang YW. Development of Novel Fluorinated polyphenols as selective inhibitors of DYRK1A/B kinase for treatment of Neuroinflammatory diseases including Parkinson’s Disease. J Pharm. 2023;16(3):443.
Lee HJ, Woo H, Lee HE, Jeon H, Ryu KY, han Nam J, et al. The novel DYRK1A inhibitor KVN93 regulates cognitive function, amyloid-beta pathology, and neuroinflammation. Free Radic Biol Med. 2020;160:575–95.
Yin X, Jin N, Shi J, Zhang Y, Wu Y, Gong CX, et al. Dyrk1A overexpression leads to increase of 3R-tau expression and cognitive deficits in Ts65Dn down syndrome mice. Sci Rep. 2017;7(1):619.
Ahn KJ, Jeong HK, Choi HS, Ryoo SR, Kim YJ, Goo JS, et al. DYRK1A BAC transgenic mice show altered synaptic plasticity with learning and memory defects. Neurobiol Dis. 2006;22(3):463–72.
Adayev T, Wegiel J, Hwang YW. Harmine is an ATP-competitive inhibitor for dual-specificity tyrosine phosphorylation-regulated kinase 1A (Dyrk1A). Arch Biochem Biophys. 2011;507(2):212–8.
Bain J, Plater L, Elliott M, Shpiro N, Hastie CJ, Mclauchlan H, et al. The selectivity of protein kinase inhibitors: a further update. Biochem J. 2007;408(3):297–315.
Göckler N, Jofre G, Papadopoulos C, Soppa U, Tejedor FJ, Becker W. Harmine specifically inhibits protein kinase DYRK1A and interferes with neurite formation. FEBS J. 2009;276(21):6324–37.
Sitz JH, Baumgärtel K, Hämmerle B, Papadopoulos C, Hekerman P, Tejedor FJ, et al. The Down syndrome candidate dual-specificity tyrosine phosphorylation-regulated kinase 1A phosphorylates the neurodegeneration-related septin 4. Neurosci. 2008;157(3):596–605.
Liu W, Liu X, Tian L, Gao Y, Liu W, Chen H, et al. Design, synthesis and biological evaluation of harmine derivatives as potent GSK-3β/DYRK1A dual inhibitors for the treatment of Alzheimer’s disease. Eur J Med Chem. 2021;222:113554.
Bessone IF, Navarro J, Martinez E, Karmirian K, Holubiec M, Alloatti M, et al. DYRK1A regulates the bidirectional axonal transport of APP in human-derived neurons. J Neurosci. 2022;42(33):6344–58.
Drummond E, Pires G, MacMurray C, Askenazi M, Nayak S, Bourdon M, et al. Phosphorylated tau interactome in the human Alzheimer’s disease brain. Brain. 2020;143(9):2803–17.
Ihara M, Yamasaki N, Hagiwara A, Tanigaki A, Kitano A, Hikawa R, et al. Sept4, a component of presynaptic scaffold and Lewy bodies, is required for the suppression of α-synuclein neurotoxicity. Neuron. 2007;53(4):519–33.
de Graaf K, Czajkowska H, Rottmann S, Packman LC, Lilischkis R, Lüscher B, et al. The protein kinase DYRK1A phosphorylates the splicing factor SF3b1/SAP155 at Thr434, a novel in vivo phosphorylation site. BMC Biochem. 2006;7(1):1–3.
Liu X, Lai LY, Chen JX, Li X, Wang N, Zhou LJ, et al. An inhibitor with GSK3β and DYRK1A dual inhibitory properties reduces tau hyperphosphorylation and ameliorates disease in models of Alzheimer’s disease. Neuropharmacol. 2023;232:109525.
Choy RW, Cheng Z, Schekman R. Amyloid precursor protein (APP) traffics from the cell surface via endosomes for amyloid β (Aβ) production in the trans-golgi network. Proc Natl Acad Sci. 2012;109(30):E2077–82.
Thapa S, Lv M, Xu H. Acetylcholinesterase: a primary target for drugs and insecticides. Mini Rev Med Chem. 2017;17(17):1665–76.
Vecchio I, Sorrentino L, Paoletti A, Marra R, Arbitrio M. The state of the art on acetylcholinesterase inhibitors in the treatment of Alzheimer’s disease. J Cent Nerv Syst Dis. 2021;13:11795735211029113.
Herholz K. Acetylcholine esterase activity in mild cognitive impairment and Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2008;35:25–9.
Bohnen NI, Kaufer DI, Hendrickson R, Ivanco LS, Lopresti B, Davis JG, et al. Cognitive correlates of alterations in acetylcholinesterase in Alzheimer’s disease. Neurosci Lett. 2005;380(1–2):127–32.
Husain I, Akhtar M, Abdin MZ, Islamuddin M, Shaharyar M, Najmi AK. Rosuvastatin ameliorates cognitive impairment in rats fed with high-salt and cholesterol diet via inhibiting acetylcholinesterase activity and amyloid beta peptide aggregation. Hum Exp Toxicol. 2018;37(4):399–411.
Phyu MP, Tangpong J. Protective effect of Thunbergia laurifolia (Linn) on lead induced acetylcholinesterase dysfunction and cognitive impairment in mice. BioMed Res Int 2013.
Jyothi P, Yellamma K. Molecular docking studies on the therapeutic targets of Alzheimer’s disease (AChE and BChE) using natural bioactive alkaloids. Int J Pharm Sci. 2016;8(12):108–12.
Liu W, Liu X, Liu W, Gao Y, Wu L, Huang Y, et al. Discovery of novel β-carboline derivatives as selective AChE inhibitors with GSK-3β inhibitory property for the treatment of Alzheimer’s disease. Eur J Med Chem. 2022;229:114095.
He D, Wu H, Wei Y, Liu W, Huang F, Shi H, et al. Effects of harmine, an acetylcholinesterase inhibitor, on spatial learning and memory of APP/PS1 transgenic mice and scopolamine-induced memory impairment mice. Eur J Pharmacol. 2015;768:96–107.
Li SP, Wang YW, Qi SL, Zhang YP, Deng G, Ding WZ, et al. Analogous β-carboline alkaloids harmaline and harmine ameliorate scopolamine-induced cognition dysfunction by attenuating acetylcholinesterase activity, oxidative stress, and inflammation in mice. Front Pharmacol. 2018;9:346.
Inestrosa NC, Sagal JP, Colombres M. Acetylcholinesterase interaction with Alzheimer amyloid beta. Subcell Biochem. 2005;38:299–317.
Carvajal FJ, Inestrosa NC. Interactions of AChE with Aβ aggregates in Alzheimer’s brain: therapeutic relevance of IDN 5706. Front Mol Neurosci. 2011;4:19.
Du H, Song J, Ma F, Gao H, Zhao X, Mao R, He X, Yan Y. Novel harmine derivatives as potent acetylcholinesterase and amyloid beta aggregation dual inhibitors for management of Alzheimer’s disease. J Enzyme Inhib Med Chem. 2023;38(1):2281893.
Gandhi S, Abramov AY. Mechanism of oxidative stress in neurodegeneration. Oxid Med Cell Longev. 2012;2012:428010.
Lushchak VI. Free radicals, reactive oxygen species, oxidative stress and its classification. Chem Biol Interact. 2014;224:164–75.
Preiser JC. Oxidative stress. J Parenter Enter Nutr. 2012;36(2):147–54.
Olufunmilayo EO, Gerke-Duncan MB, Holsinger RD. Oxidative stress and antioxidants in neurodegenerative disorders. Antioxidants. 2023;12(2):517.
Reus GZ, Stringari RB, de Souza B, Petronilho F, Dal-Pizzol F, Hallak JE, et al. Harmine and imipramine promote antioxidant activities in prefrontal cortex and hippocampus. Oxid Med Cell Longev. 2010;3(5):325–31.
Jain S, Panuganti V, Jha S, Roy I. Harmine acts as an indirect inhibitor of intracellular protein aggregation. ACS Omega. 2020;5(11):5620–8.
Habib MZ, Tadros MG, Abd-Alkhalek HA, Mohamad MI, Eid DM, Hassan FE, et al. Harmine prevents 3-nitropropionic acid-induced neurotoxicity in rats via enhancing NRF2-mediated signaling: involvement of p21 and AMPK. Eur J Pharmacol. 2022;927:175046.
Singh A, Kukreti R, Saso L, Kukreti S. Oxidative stress: a key modulator in neurodegenerative diseases. Molecules. 2019;24(8):1583.
He F, Ru X, Wen T. NRF2, a transcription factor for stress response and beyond. Int J Mol Sci. 2020;21(13):4777.
Joo MS, Kim WD, Lee KY, Kim JH, Koo JH, Kim SG. AMPK facilitates nuclear accumulation of Nrf2 by phosphorylating at serine 550. Mol Cell Biol. 2016;36(14):1931–42.
Xu W, Zhao T, Xiao H. The implication of oxidative stress and AMPK-Nrf2 antioxidative signaling in pneumonia pathogenesis. Front Endocrinol. 2020;11:400.
Hammad M, Raftari M, Cesário R, Salma R, Godoy P, Emami SN, Haghdoost S. Roles of oxidative stress and Nrf2 signaling in pathogenic and non-pathogenic cells: a possible general mechanism of resistance to therapy. Antioxidants. 2023;12(7):1371.
Srinivasan S, Avadhani NG. Cytochrome c oxidase dysfunction in oxidative stress. Free Radic Biol Med. 2012;53(6):1252–63.
Murali M, Carvalho MS, Shivanandappa T. Oxidative stress-mediated cytotoxicity of Endosulfan is causally linked to the inhibition of NADH dehydrogenase and Na+, K+-ATPase in Ehrlich ascites tumor cells. Mol Cell Biochem. 2020;468(1–2):59–68.
Réus GZ, Stringari RB, Gonçalves CL, Scaini G, Carvalho-Silva M, Jeremias GC, et al. Administration of harmine and imipramine alters creatine kinase and mitochondrial respiratory chain activities in the rat brain. Depress Res Treat. 2012;2012:987397.
Uzbekov MG. Monoamine oxidase as a potential biomarker of the efficacy of treatment of mental disorders. Biochem. 2021;86(6):773–83.
Balint B, Wéber C, Cruzalegui F, Burbridge M, Kotschy A. Structure-based design and synthesis of harmine derivatives with different selectivity profiles in kinase versus Monoamine Oxidase Inhibition. Chem Med Chem. 2017;12(12):932–9.
Son SY, Ma J, Kondou Y, Yoshimura M, Yamashita E, Tsukihara T. Structure of human monoamine oxidase A at 2.2-Å resolution: the control of opening the entry for substrates/inhibitors. Proc Natl Acad Sci. 2008;105(15):5739–44.
Giacobbo BL, Doorduin J, Moraga-Amaro R, Nazario LR, Schildt A, Bromberg E, et al. Chronic harmine treatment has a delayed effect on mobility in control and socially defeated rats. Psychopharmacol. 2020;237:1595–606.
Myburg T, Petzer A, Petzer JP. The inhibition of monoamine oxidase by harmine derivatives. Res Chem. 2022;4:100607.
Stocco MR, Tolledo C, Wadji FB, Gonzalez FJ, Miksys S, Tyndale RF. Human CYP2D6 in the brain is protective against harmine-induced neurotoxicity: evidence from humanized CYP2D6 transgenic mice. Mol Neurobiol. 2020;57(11):4608–21.
Sun Q, Liu C, Jiang K, Fang Y, Kong C, Fu J, et al. A preliminary study on the neurotoxic mechanism of harmine in Caenorhabditis elegans. Comp Biochem Physio C Toxicol Pharmacol. 2021;245:109038.
Cruz-Hernandez A, Agim ZS, Montenegro PC, McCabe GP, Rochet JC, Cannon JR. Selective dopaminergic neurotoxicity of three heterocyclic amine subclasses in primary rat midbrain neurons. Neurotoxicol. 2018;65:68–84.
Ostergren A, Fredriksson A, Brittebo EB. Norharman-induced motoric impairment in mice: neurodegeneration and glial activation in substantia nigra. J Neural Trans. 2006;113:313–29.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Pankaj Kadyan and Dr. Lovedeep Singh performed the original drafting. Dr. Lovedeep Singh also undertook the conceptualization and reviewing tasks.
Corresponding author
Ethics declarations
Conflict of interest
Lovedeep Singh and Pankaj Kadyan declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kadyan, P., Singh, L. Unraveling the mechanistic interplay of mediators orchestrating the neuroprotective potential of harmine. Pharmacol. Rep 76, 665–678 (2024). https://doi.org/10.1007/s43440-024-00602-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-024-00602-8