Abstract
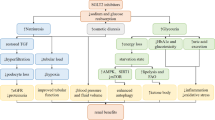
Sodium–glucose cotransporter inhibitors (SGLT2i) are a new class of anti-diabetic drugs that have beneficial cardiovascular and renal effects. These drugs decrease proximal tubular glucose reabsorption and decrease blood glucose levels as a main anti-diabetic action. Furthermore, SGLT2i decreases glomerular hyperfiltration by a tubuloglomerular feedback mechanism. However, the renal benefits of these agents are independent of glucose-lowering and hemodynamic factors, and SGLT2i also impacts the kidney structure including kidney fibrosis. Renal fibrosis is a common pathway and pathological marker of virtually every type of chronic kidney disease (CKD), and amelioration of renal fibrosis is of utmost importance to reduce the progression of CKD. Recent studies have shown that SGLT2i impact many cellular processes including inflammation, hypoxia, oxidative stress, metabolic functions, and renin–angiotensin system (RAS) which all are related with kidney fibrosis. Indeed, most but not all studies showed that renal fibrosis was ameliorated by SGLT2i through the reduction of inflammation, hypoxia, oxidative stress, and RAS activation. In addition, less known effects on SGLT2i on klotho expression, capillary rarefaction, signal transducer and activator of transcription signaling and peptidylprolyl cis/trans isomerase (Pin1) levels may partly explain the anti-fibrotic effects of SGLT2i in kidneys. It is important to remember that some studies have not shown any beneficial effects of SGLT2i on kidney fibrosis. Given this background, in the current review, we have summarized the studies and pathophysiologic aspects of SGL2 inhibition on renal fibrosis in various CKD models and tried to explain the potential reasons for contrasting findings.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
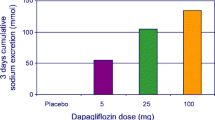
Sodium–glucose cotransporter inhibitors (SGLT2i) are a new class of anti-diabetic drugs. Randomized clinical studies have shown that SGLT2i has cardiovascular and renal protective effects [1,2,3,4]. Although the main anti-diabetic action of SGLT2i is to decrease glucose reabsorption in proximal tubules, the pleiotropic actions of SGLT2i are critical for cardio-renal protection. Indeed, studies showed that the beneficial effects of SGLT2i were independent of blood glucose reduction and HbA1c [5, 6]. These drugs are also effective in patients with heart failure (HF) both with reduced ejection [2, 7] fraction and preserved ejection fraction [8]. Besides, SGLT2i improve estimated glomerular filtration rate (eGFR), kidney failure, and mortality independent of albuminuria. Thus, SGLT2i are recommended in patients with type 2 diabetes and chronic kidney disease (CKD) [1, 9, 10]. Accordingly, the current KDIGO and ADA guidelines revised the threshold for initiation of SGLT2i therapy as eGFR > 20 mL/min/1.73 m2 instead of eGFR > 30 mL/min/1.73 m2 [11].
In diabetic state, there is increased proximal tubule absorption of glucose and sodium by SGLT2. This leads to a decrease in the luminal sodium chloride concentration, which is sensed by macula densa via the tubule glomerular feedback (TGF) mechanism, leading to dilatation of the renal afferent arteriole and glomerular hyperfiltration [12]. Experimental studies in diabetic rats demonstrated that SGLT2i reduced glomerular capillary pressure through TGF [13]. It is important to note that glomerular hyperfiltration is not unique to diabetic kidney disease (DKD), but occurs as a compensatory mechanism (increased single nephron GFR) in all progressive renal diseases. Although this initial compensation maintains the total GFR constant, the long-term consequences of mechanical stress induced by increased GFR are detrimental. High single nephron GFR damages the glomerular filtration barrier causing glomerulosclerosis and proteinuria, and eventually resulting in loss of remaining nephrons and kidney fibrosis [14,15,16]. Accordingly, the reno-protective mechanisms of SGLT2i is not unique to DKD. Indeed, recent clinical trials have shown the reno-protective effect of SGLT2i in non-diabetic kidney disease [9, 17]. Apart from these functional changes, SGLT2i-induced favorable renal structural changes, which have not been fully elucidated yet, might explain long-term effects of these agents [4]. Regardless of the cause, renal fibrosis is a common pathway and pathological marker of virtually every type of CKD [18]. Recent preclinical (Table 1) and clinical (Table 2) studies have shown that SGLT2i might modify kidney fibrosis by a variety of mechanisms. Given this background, in the current review, we have summarized the studies regarding the impact of SGLT2i on renal fibrosis in various CKD models.
Mechanisms of kidney fibrosis influenced by sodium–glucose cotransporter inhibition
Hypoxia-inducible factor, sodium–glucose cotransporter inhibition, and kidney fibrosis
As well known, hypoxia is a driver of tubulointerstitial fibrosis [19, 20]. Decreased hypoxia-inducible factor (HIF) function by SGLT2i may be one of the protective mechanisms for kidney fibrosis. Hypoxia may induce renal fibrosis by activating the HIF-1α/human epididymis protein 4 (HE4)/nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway [21]. Previously, it was suggested that there was a positive association between circulating HE4 and renal fibrosis [22, 23]. Huang et al. showed that dapagliflozin reduced HIF-1α, HE4, and NF-κB expressions along with decreased histologic kidney damage in contrast-induced acute kidney injury (AKI) model [24]. Dapagliflozin also decreased hypoxia-induced connective tissue growth factor (CTGF) and platelet-derived growth factor (PDGF) production, suggesting that its anti-fibrotic effects might be in direct connection with diminished hypoxia [25]. In diabetic mice HIF‐1α activation causes epithelial‐to‐mesenchymal transition (EMT), leading to tubulointerstitial injury and empagliflozin decreased renal fibrosis and EMT along with decreased HIF-1α [26]. In human proximal kidney 2 (HK-2) cells, HIF-1α expression is inhibited by SGLT2i during hypoxia [27, 28]. As SGLT2i decrease glucose uptake by renal proximal tubular cells (RPTCs), they reduce oxygen consumption and decrease expression, and increase proteasomal degradation of HIF1α in RPTCs [29]. However, there are also contrasting findings. Although the above studies showed that high HIF-1α in tubular epithelial cells contributes to renal fibrosis, HIF-1α stabilization by prolyl hydroxylase domain (PHD) inhibitors has shown favorable effects in ischemic kidney injury [30]. In streptozotocin (STZ)-induced diabetic mice, HIF-1α deficiency was related to more severe renal fibrosis and glomerular hypertrophy [31]. The reasons for these different findings are not exactly known, but the amount and duration of HIF activation may be an explanation. Indeed, it was suggested that the protective effect of HIF on the kidney occurs in AKI, but long-term permanent activation may be detrimental resulting in chronic inflammation, fibrosis, and extracellular matrix accumulation [32]. For example, after a 30 min period of ischemia, there is severe AKI in mice which exhibits a significant delay in the HIF response, compared to mice with mild AKI which elicits fast HIF response. In the group with a delayed response; HIF-1α and HIF-2α activation were inappropriately sustained with severe ischemia–reperfusion injury (IRI) leading to maladaptive renal repair and acute kidney injury (AKI) and that activation remained upregulated 4 weeks after injury. In contrast, HIF response in the mild AKI group, i.e., adaptive repair group, returned to normal levels well before 4 weeks [33]. Thus, it is probable that although acute short-term physiological HIF activation may be beneficial, persistent HIF activation may be detrimental in long term. In fact, there appears to be a time-dependent transition in the pattern of HIF activation from renal tubular epithelia and capillary endothelia to renal interstitial fibroblasts during chronic maladaptive renal repair resulting in renal fibrosis [34]. Thus, the role of HIF activation in fibrogenesis may be context specific (e.g., IRI), duration specific (acute vs. chronic) or amount specific (high vs. low dose HIF). Furthermore, as SGLT2i shift tubular glucose and sodium absorption from the proximal tubule to the outer medulla, where SGLT1 partially compensates for SGLT2 blockade, cortical oxygen tension is expected to increase at the expanse of lower medullary oxygen levels. This will, in turn, increase HIF signaling in the medulla, which stimulates erythropoietin (EPO) release and increases hematocrit [35]. In this regard, SGLT2 inhibition may be a double-edged sword to medullary oxygenation, and whether final outcome of medullary hypoxia is adverse or favorable to overall kidney function is unknown [32]. Furthermore, the impact of SGLT2 inhibition during AKI and CKD may operate via different mechanisms (Fig. 1). Thus, it is not hundred percent clear whether HIF-1α has a detrimental or protective effect in the context of CKD, and future research is needed to obtain a deeper understanding of HIF in kidney fibrosis.
The inhibition of sodium–glucose cotransport 2 during acute kidney injury (AKI) and chronic kidney disease may activate different mechanisms. During AKI, sodium–glucose cotransport 2 inhibitors (SGLT2i) impair proximal sodium and glucose reabsorption from the proximal tubule which results in decreased ATP consumption and increased oxygen tension in proximal tubular cells. This in turn shifts sodium glucose reabsorption to distal parts of the proximal tubule close to the medulla which SGLT1 plays a major role in reabsorption. The increased need for reabsorption in distal parts necessitates more energy consumption which results in a decrease in ATP and oxygen tension in the medulla. This in turn decreased hypoxia-inducible factor-2 alpha (HIF-2α) degradation resulting in increased EPO secretion and increased hematocrit levels. The net balance between hypoxia and increased hematocrit will determine whether the final outcome of medullary hypoxia is adverse or beneficial to overall kidney function. In chronic kidney disease, there is persistent hypoxia leading to chronic HIF-1α activation. Chronic HIF-1 activation induces kidney fibrosis by a variety of mechanisms including increased human epididymis protein 4 (HE4), connective tissue growth factor (CTGF), and epithelial-to-mesenchymal transition (EMT). SGLT2 inhibition during CKD decreases tissue hypoxia and kidney fibrosis may inhibit HE4, CTGF, and EMT downstream
Inflammation, sodium–glucose cotransporter inhibition, and kidney fibrosis
In chronic kidney disease, there is increased pro-inflammatory markers and decreased anti-inflammatory markers favoring a chronic inflammatory state [36]. SGLT2i have many anti-inflammatory effects in kidney (Fig. 2). NLR family pyrin domain containing 3 (NLRP3) is one of the most important inflammatory mediator overactivated in CKD [37] and associated with kidney fibrosis [38]. Benetti et al. showed that empagliflozin decreased NLRP3 activation in the kidney and liver induced by a high-fat–high-sugar diet [39]. In IRI-induced fibrosis model, dapagliflozin prevented activation of NLRP3 inflammasome and increased anti-inflammatory metabolite itaconate and protected kidney against fibrosis [40]. It was suggested that β-hydroxybutyrate—a type of ketone body—inhibits NLRP3 activation [41]. As SGLT2i promote the elevation of ketone bodies, this may be another mechanism to explain the reno-protective role of SGLT2i. In rats with experimentally induced DM, increased tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) levels were counterbalanced by empagliflozin [42]. Wang et al. showed that SGLT2i decrease macrophage infiltration, p65 subunit of NF-kB toll-like receptor 4 (TLR4), monocyte chemotactic protein 1 (MCP-1) and osteopontin in diabetic db/db mice [43]; which are in compliance with the findings of Tang et al. [44]. In diabetic mice, dapagliflozin inhibited pro-inflammatory macrophage (M1 type) infiltration, CD11c (a marker of M1 type macrophages), and CD14 expressions in the renal cortex with no effect on CD206 (specific for the anti-inflammatory (M2) subtype of macrophages). Both in the glomeruli and interstitial space, immunoperoxidase staining showed increased F4/80, a marker for M1 macrophages, which was reduced by dapagliflozin [45]. In high-fed mice, ipragliflozin treatment suppressed the ratio of M1-type (CD11c + CD206- cells) to M2-type tissue macrophages (CD11c-CD206 + cells) in peri-renal fat tissue [46]. In Akita mice, dapagliflozin decreased macrophage infiltration into glomeruli and interstitium, and decreased transforming growth factor β (TGF-β), C–C motif chemokine ligand 2 (CCL2), osteopontin, and intercellular adhesion molecule 1 (ICAM-1) expressions [47]. In streptozotocin-induced diabetic rats, empagliflozin reduced receptor for advanced glycation end-products (RAGE) gene and protein expressions, M1 macrophage infiltration (F4/80), and expression of pro-fibrotic markers such as MCP-1, ICAM‐1, TGF‐β, and CTGF, which are AGE–RAGE signaling [48]. In renal proximal tubular cells exposed to high glucose, dapagliflozin inhibited high mobility group box 1 (HMGB1)/RAGE/NFκB signaling pathway, leading to attenuation inflammatory (downregulation of ICAM‐1, MCP‐1, and NF‐κB mRNA levels) and fibrosis (decreased fibronectin and collagen I mRNA) markers [49]. Abbas et al. demonstrated that empagliflozin decreased NF-κB activation in the unilateral ureteric obstruction (UUO) model of nephropathy [50], which plays an important role in renal fibrosis and fibroblast activation [51]. Furthermore, empagliflozin decreased TLR4 expression, which is involved in NF-κB-mediated inflammation [52]. In a clinical study using the transcriptomics approach, Heerspink et al. demonstrated that compared with glimepiride, canagliflozin (300 mg/day) decreased plasma levels of TNF receptor 1 and IL-6 during 2 years of follow-up [53].
Sodium–glucose cotransport 2 inhibitors (SGLT2i) exert many anti-inflammatory effects which ameliorate kidney fibrosis. They increase ketone body formation including β-hydroxybutyrate which inhibits the Nod-like receptor family and pyrin domain containing 3 (NLRP3) inflammasome. SGLT2i decreases macrophage infiltration to the kidney and decreases the pro-inflammatory (M1)/anti-inflammatory (M2) macrophage ratio. They decrease many inflammatory pathways and molecules including nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), interleukin-6 (IL-6), toll-like receptors (TLRs), monocyte chemotactic protein 1 (MCP-1), intercellular adhesion molecule 1 (ICAM-1), and advanced glycation end-products (AGE)–RAGE signaling
Oxidative stress, sodium–glucose cotransporter inhibition, and kidney fibrosis
Increased oxidative stress is one of the hallmarks of CKD. In a rat model of diabetic nephropathy, Wu et al. showed that the activities of superoxide dismutase (SOD), glutathione peroxidase (GSH) in the diabetic nephropathy group were decreased and the levels of malondialdehyde (MDA) and nitric oxide (NO) were increased compared to controls. However, after treatment with empagliflozin, the activities of SOD and GSH increased and the levels of MDA and NO decreased [42]. These findings are important since the increase in reactive oxygen species (ROS) triggers inflammation, endothelial dysfunction, increases expression of TGF-β1, and induces renal fibrosis [54]. In a diabetic (db/db) mice model, dapagliflozin decreased oxidative stress and ROS production (both 0.1 mg/kg and 1 mg/kg doses) and decreased the number of apoptotic cells and the expressions of the pro-apoptotic factors, Caspase-12 and Bax [45]. Tang et al. showed that in db/db diabetic mice, dapagliflozin decreased Nox4, Nox2, and its regulatory subunit p47phox. Furthermore, thiobarbituric acid reactive substances (TBARS) levels, which show the level of lipid peroxidation, were also decreased by dapagliflozin [44]. In Akita mice, dapagliflozin decreased Nox4 both in vivo and in vitro along with decreased apoptosis [47]. In proximal tubular epithelial cells, high glucose increased superoxide and hydrogen peroxide generation, oxidative stress-dependent TRAF3IP2 upregulation, NF-κB, and p38 MAPK activation, which was inhibited by empagliflozin [55]. In New Zealand obese mice with a high-fat diet, canagliflozin ameliorated hyperglycemia-associated augmentation of urinary 8-isoprostane levels [56]. Ipragliflozin and 30% calorie restriction almost normalized the oxidized glutathione levels in the renal cortex of BTBR ob/ob diabetic mice as shown by mass spectrometry [57].
Metabolism, sodium–glucose cotransporter inhibition, and kidney fibrosis
SGLT2i has many metabolic effects, the most prominent one is shifting glucose to free fatty acid utilization (Fig. 3) [58]. Decreased toxic lipid metabolites in mesangial cells, podocytes, and proximal tubular reduce oxidative stress, endoplasmic reticulum stress, and pro-inflammatory processes [59]. SGLT2i increase ketone body formation via starvation-like response including activation of sirtuin1/activated protein kinase and adenosine monophosphate-activated protein kinase (AMPK) signaling and inhibition of protein kinase B (AKT)/mammalian target of rapamycin (mTOR) signaling [13, 60,61,62]. Increased lipid toxicity produces ROS, which induces inflammatory mediators and damages renal tubular epithelial cells. Furthermore, deficient lipophagy increases tubular lipid deposition and increased fibrosis in diabetic nephropathy [63]. Zhang et al. showed that empagliflozin decreased lipid accumulation in renal tubular cells which is associated with decreased fibrosis. Additionally, empagliflozin reduced lipid expression and showed reduced lipid droplet activity [64]. Thus, decreasing lipid toxicity may be another favorable mechanism of SGLT2i.
Sodium–glucose cotransport 2 inhibitors (SGLT2i) have many beneficial metabolic effects that retards kidney fibrosis. They block glucose entry to tubular cells and inhibit glycolysis. They simultaneously increase free fatty acid oxidation and ketone body formation resulting in decreased toxic lipid accumulation in proximal tubular cells resulting in decreased inflammation, and oxidative and endoplasmic reticulum (ER) stress. They regulate the tricarboxylic acid (TCA) cycle and decrease TCA cycle metabolites in renal proximal tubular cells. SGLT2i restore autophagy markers Beclin‐1 and LC3‐II and retard kidney fibrosis
The impact of SGLT2i on the tricarboxylic acid (TCA) cycle is also worth mentioning. Ke et al. showed that TCA cycle metabolites were accumulated, NLRP3 inflammasome, mTOR/HIF-1α signaling were increased in the IRI-induced fibrosis model in mice compared to sham, all of which are strikingly blocked by dapagliflozin. Authors suggest that TCA cycle metabolites accumulate due to decreased metabolic processes in the fibrotic kidney. However, dapagliflozin boosted TCA cycle derivative itaconate by decreasing isocitrate dehydrogenase 2 and increasing immune-responsive gene 1 and mitochondrial citrate carrier. RNA sequence data showed that dapagliflozin tended to restore decreased TCA cycle enzymes including α-ketoglutarate dehydrogenase, succinate dehydrogenase, fumarase, and malate dehydrogenase. Furthermore, itaconate prevented activation of the NLRP3 inflammasome and protected the kidney against fibrosis. These findings identify a novel mechanism coupling inflammation and metabolism for reno-protection of SGLT2 inhibition for kidney fibrosis and CKD. The accumulation of lipid droplets in renal tubules was markedly attenuated by dapagliflozin treatment. These changes were associated with a decrease in NLRP3 inflammasome activation [40]. Ding et al. demonstrated that STZ-induced CD1 mice showed aberrant glycolysis (indicated by hexokinase 2 induction, and pyruvate kinase isozyme M2 dimer formation, increased fructose-6-phosphate, glucose-6-phosphate (G6P), and phosphofructokinase) and decreased Sirt3 levels associated with EMT and kidney fibrosis. Empagliflozin and canagliflozin normalized these changes. These findings are important since inhibition of glycolysis has been demonstrated to be a relevant strategy for inhibiting kidney fibrosis [65].
Activation of AMPK, which is an important energy sensor of the cell, is also activated by SGLT2 inhibition. Inoue et al. showed that canagliflozin activated AMPK in the kidney and reduced the expression of fibrotic and inflammatory markers such as collagen I, CTGF, F4/80, TGF‐β, and MCP‐1 [66]. Supporting these findings, empagliflozin treatment restored phosphorylated AMPK levels in renal proximal tubular cells and increased autophagy markers Beclin1 and LC3II by decreasing mTOR activation [67]. SGLT2i also exerts anti-fibrotic effects via post-translational modification. Post-translational O-GlcNAcylation, which induces O-linked N-acetylglucosamine (O-GlcNAc) is a known contributor to glucose toxicity in diabetes, and increased O-GlcNAcylation increases fibrotic signaling in kidneys [68]. Hodrea et al. showed that dapagliflozin reduced O-GlcNAcylation resulting in decreased fibrosis in streptozotocin-induced type 1 diabetes in adult male Wistar rats [25].
Last but not the least, SGLT2i may decrease endoplasmic reticulum (ER) stress by downregulating key ER stress markers such as phosphorylated eukaryotic initiation factor‐2α (peIF2α), activating transcription factor 4 (ATF4), and C/EBP homologous protein (CHOP; an ER‐stress induced apoptotic marker), and the apoptotic marker Caspase 3 [69, 70], both of which are associated with kidney fibrosis [71].
Renin–angiotensin system: sodium–glucose cotransporter inhibition and kidney fibrosis
SGLT2i may impact differently on the systemic renin–angiotensin system (RAS) depending on whether inhibition is acute or occurs in the context of CKD, when RAS is already activated (Fig. 4). Not only systemic RAS, but more importantly local RAS activates fibrotic pathways in the kidney [72]. Indeed, the anti-fibrotic actions of angiotensin II (AngII) type 1 receptor (AT1R) antagonism [73] and angiotensin-converting enzyme (ACE) inhibition [74] have been already demonstrated in murine models of UUO and progressive renal fibrosis. Furthermore, RAS inhibition has already been shown to reduce renal fibrosis in DKD [75,76,77]. On the other hand, AngII type 2 receptor (AT2R) agonism, which has opposite actions to classical AT1R receptor is protective against kidney fibrosis [78]. The pro-fibrotic action of RAS activation is suggested to be due to the exacerbation of renal inflammation [79, 80], induction of abnormal autophagy [81], increase in the synthesis of TGF‐β [82], and increased collagen synthesis [83]. There is now clinical evidence suggesting that RAS activation is blunted when SGLT2i is used. In Otsuka Long-Evans Tokushima Fatty (OLETF) rats, 12 weeks of dapagliflozin reduced urinary AngII and angiotensinogen levels, and AT1R expression in a model of T2D with DKD [84]. In New Zealand obese mice with a high-fat diet, canagliflozin decreased the expression of renal angiotensinogen [56]. In non-diabetic patients with nephrotic range proteinuria, SGLT2 is positively associated with angiotensinogen, renin, and ACE mRNA levels. The same study showed that in proximal HK-2 cells, acute but not chronic (4 week) AngII stimulated SGLT2 expression in a dose-dependent manner. Incubation of HK-2 cells with losartan (AT1R antagonist) abolished the effects of AngII, indicating that AngII stimulates SGLT2 expression via AT1R [85]. In contrast, Gallo et al. showed that both plasma and intra-renal renin activity is increased after 10 weeks of empagliflozin treatment in a diabetic model of db/db mice without change in intra-renal AngII levels [86]. In patients with type 2 diabetes, 12 weeks of dapagliflozin (10 mg/day), resulted in increased plasma renin activity and aldosterone levels, possibly due to reduced plasma volume [87]. The study by Tanaka et al. showed that canagliflozin did not change plasma aldosterone levels despite increased plasma renin activity and urine volume [88]. In OLETF rats, empagliflozin treatment was associated with an increase in urinary angiotensinogen excretion [89]. These contradictory fındings may be of concern given the fact that in CKD and DKD, there is already activated RAS. However, the rise of renin activity seems to be transient. In a retrospective study performed in patients with type 2 diabetes, Sawamura et al. showed that there was no change in plasma renin activity and plasma aldosterone levels receiving SGLT2i for 2–6 months [90]. As SGLT2i decrease glucose load in proximal tubules and increase glucose load in distal tubules, the impact of SGLT2i on the RAS system may differ in proximal and distal tubules. The contradictory effects of SGLT2i on proximal (decreased RAS activation) and distal tubules (increased RAS activation) may compensate each other with resultant non-significant changes in intra-renal RAS [29]. However, more studies are warranted to understand the systemic and intra-renal RAS in the context of SGLT2 inhibition.
The inhibition of SGLT2 may impact differently on the systemic renin–angiotensin system (RAS) depending on whether inhibition is acute or occurs in the context of CKD when RAS is already activated. When SGLT2i given, they cause mild hypovolemia which results in increased temporary renin–angiotensin system activation (RAS) which is normalized in the 2–6-month period. During chronic kidney disease (CKD), there is already local kidney RAS activation and SGLT2i in CKD decreases local kidney RAS activation resulting in kidney fibrosis
Other potential mechanisms related sodium–glucose cotransporter inhibition and kidney fibrosis
The interaction with uric acid (UA) and SGLT2i is a concern for renal fibrosis. Increased UA levels were related to increased renal fibrosis [91]. SGLT2i reduce plasma UA by increased renal urate elimination by competition of extra glucose for the urate transporter GLUT9 and decreased UA levels [92, 93]. Uric acid excretion by SGLT2i was linked to urinary glucose excretion and is attenuated during the concomitant pharmacologic blockade of urate transporter 1 [94]. SGLT2i may repress tubulointerstitial fibrosis by influencing signal transducer and activator of transcription-1 (STAT-1) activity. STAT1 plays a role in high glucose-induced oxidative stress and expression of TGF-β1, as well as the production of the extra-cellular matrix proteins collagen IV and fibronectin. Concurrently, high glucose activates STAT1 and TGF β and is involved in tubulointerstitial fibrosis. It was shown that dapagliflozin suppressed pro-fibrotic factors STAT1 and TGF-β1 both in vivo (measured by mRNA in tubulointerstitium compartment of the renal biopsy cores) and in vitro (in cultured renal proximal cells) independent of glucose-lowering effect [95].
Decreased klotho expression has been suggested as a risk factor for the development of kidney fibrosis and hypertension [96]. Zhou et al. showed that klotho ameliorates kidney injury and fibrosis, and normalizes blood pressure by targeting the RAS [97]. In a model of UUO, Abbas et al. showed that prophylactic administration of empagliflozin increased klotho expression in both immediate and delayed treatment groups, which was decreased by UUO. Authors suggested that by increasing klotho, empagliflozin may be potentially protective against kidney fibrosis [50].
Renal fibrosis was associated with capillary rarefaction and the role of SGLT2i on capillary rarefaction deserves mention. Zhang et al. investigated the effect of luseogliflozin on capillary rarefaction in AKI induced by ischemia–reperfusion. They showed that IRI decreased CD31, an endothelial marker. Luseogliflozin treatment attenuated CD31-positive cell loss, suggesting a protective role for endothelial cells. The decline of CD31 during IR is also associated with increased hypoxia, and luseogliflozin treatment ameliorated hypoxia as determined by pimonidazole staining. NG2, an activated pericyte marker, was also decreased by luseogliflozin treatment suggesting that luseogliflozin ameliorated IRI-induced renal capillary rarefaction and detachment of pericytes from endothelial cells [98], both of which were implicated in the development of renal interstitial fibrosis [99]. Moreover, luseogliflozin decreased capillary rarefaction and maintained the capillary network by increasing the vascular endothelial growth factor (VEGF)-A level [98].
Another potential anti-fibrotic action of canagliflozin may be due to the suppression peptidylprolyl cis/trans isomerase (Pin 1). Pin 1 previously has been shown to play a role in tubulointerstitial fibrosis [100]. Inoue et al. showed that in type 2 diabetic model mice, Pin1 expression increased along with fibrosis, but Pin1 protein levels were normalized by canagliflozin [66].
Perspectives and conclusion
As the above discussion suggests, most, but not all, studies showed that SGLT2i are potentially protective against kidney fibrosis, a common pathway for progressive CKD. However, there are also contrasting findings. Liu et al. showed that in patients with type 2 diabetes and stage 3 CKD, ertugliflozin (5 or 15 mg/d) did not reduce fibrosis markers, such as PDGF-AA and PDGF-AB/BB [101]. In oxalate-induced nephrocalcinosis, empagliflozin did not have any protective effect against renal fibrosis, and did not decrease α-smooth muscle actin and collagen 1 staining, and mRNA levels of fibronectin-1, collagen 1a1, fibroblast-specific protein-1, and TGF-β2 expressions. Authors suggest that the reno-protective effects of SGLT2i in DK do not occur in non-diabetic oxalate-induced nephrocalcinosis, a form of progressive CKD driven by primary tubulointerstitial injury [102]. One potential explanation is that renal anti-fibrotic effects mediated by the SGLT2i empagliflozin are ambiguous, might depend on the presence of type 2 diabetes, and/or are indirect consequences of the primary metabolic/hemodynamic action in the long term [103]. Similarly, in 5/6 (subtotal) nephrectomized rats, dapagliflozin has no protective effect on glomerulosclerosis, tubulointerstitial fibrosis, or overexpression of the pro-fibrotic cytokine, TGF-ß1 [104]. Furthermore, Vallon et al. demonstrated that TGF-β and renal collagen expression, as determined by Sirius red binding, was not ameliorated in diabetic Akita mice [105]. In male C57BL/6 Enos knockout mice, empagliflozin did not decrease tubular atrophy, or tubulointerstitial fibrosis in streptozotocin-induced DM [106]. Why are the results conflicting? The exact answer is not known, but SGLT2i may impact many processes (HIF, inflammation, oxidative stress, metabolism, RAS). Besides, the impact of SGLT2 inhibition on some biological pathways (e.g., HIF, RAS) is not consistent and somewhat controversial. The type of experimental design, the duration of SGLT2 inhibition (acute vs. chronic), the time of administration (prophylactic, immediate or delayed), the dosage (low vs. high dose), and variable drug actions in different species may be responsible for these diverse findings. Unfortunately, the clinical data are scarce and most of the studies are based on in vitro and in vivo experiments. The direct extrapolation of experimental findings to humans may be problematic and specific studies should be planned to investigate the anti-fibrotic effects of SGLT2i on kidney fibrosis in humans.
There is also controversy about whether the anti-fibrotic effects of SGLT2i are independent of TGF. Zeng et al. showed that the anti-fibrotic action of empagliflozin is independent of the TGF mechanism [107]. However, Tauber et al. demonstrated that empagliflozin did not have any protective effects against kidney fibrosis in the uninephrectomy/high salt/doca model, and since functional TGF mechanism is necessary to reduce chronic hyperfiltration and protect against glomerular damage, albuminuria, and fibrosis, authors suggested TGF may not be working properly in these animals [108].
Last but not the least, most of the results are from animal studies. Besides, assessment of kidney fibrosis necessitates renal biopsy, which might not be feasible just to determine whether SGLT2i decreased renal fibrosis. Thus, it is important to remember that the animal data may not be directly translated into clinical data. However, it is advisable that specific interest could be given to assess whether SGLT2i would decrease renal fibrosis at least in patients for whom renal biopsy was performed for other reasons.
In conclusion, SGLT2 inhibition seems to be a promising alternative to retard kidney fibrosis by influencing a variety of mechanisms. Although human data are scarce, most of the experimental studies showed favorable effects in ameliorating kidney fibrosis. As direct extrapolation of experimental animal data to humans may be problematic, studies are warranted to investigate whether SGLT2i are protective against kidney fibrosis, which is a final common pathway for all kinds of CKD progression.
Data availability
The manuscript has no associated data.
Abbreviations
- AGE:
-
Advanced glycation end-products
- AKI:
-
Acute kidney injury
- α-SMA:
-
Alpha-smooth muscle actin
- CKD:
-
Chronic kidney disease
- CTGF:
-
Connective tissue growth factor
- DKD:
-
Diabetic kidney disease
- DM:
-
Diabetes mellitus
- EMT:
-
Epithelial-to-mesenchymal transition
- EPO:
-
Erythropoietin
- FN:
-
Fibronectin
- GFR:
-
Glomerular filtration rate
- HIF:
-
Hypoxia-inducible factor
- IR:
-
Ischemia–reperfusion
- MMP:
-
Matrix metalloproteinase
- MCP-1:
-
Monocyte chemoattractant protein-1
- mTOR:
-
Mammalian target of rapamycin
- PDGFB:
-
Platelet-derived growth factor subunit B
- PHD:
-
Prolyl hydroxylase domain
- ROS:
-
Reactive oxygen species
- STAT:
-
Signal transducer and activator of transcription
- SGLT2i:
-
Sodium–glucose cotransporter inhibitors
- TIMP:
-
Tissue inhibitor of metalloproteinase
- TGF-β:
-
Transforming growth factor β
- TCA:
-
Tricarboxylic acid
- TIF:
-
Tubulointerstitial fibrosis
- T2D:
-
Type 2 diabetes
- UNx:
-
Unilateral nephrectomy
- UUO:
-
Unilateral ureteric obstruction
References
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–34.
Cooper ME, Inzucchi SE, Zinman B, Hantel S, von Eynatten M, Wanner C, et al. Glucose control and the effect of empagliflozin on kidney outcomes in type 2 diabetes: an analysis from the EMPA-REG outcome trial. Am J Kidney Dis. 2019;74:713–5.
Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G, Perkovic V. Canagliflozin slows progression of renal function decline independently of glycemic effects. J Am Soc Nephrol. 2017;28:368–75.
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
Neuen BL, Young T, Heerspink HJL, Neal B, Perkovic V, Billot L, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2019;7:845–54.
de Boer IH, Khunti K, Sadusky T, Tuttle KR, Neumiller JJ, Rhee CM, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and kidney disease: improving global outcomes (KDIGO). Kidney Int. 2022;102:974–89.
Vallon V, Thomson SC. The tubular hypothesis of nephron filtration and diabetic kidney disease. Nat Rev Nephrol. 2020;16:317–36.
Vallon V, Verma S. Effects of SGLT2 inhibitors on kidney and cardiovascular function. Annu Rev Physiol. 2021;83:503–28.
Brenner BM, Lawler EV, Mackenzie HS. The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int. 1996;49:1774–7.
Denic A, Mathew J, Lerman LO, Lieske JC, Larson JJ, Alexander MP, et al. Single-nephron glomerular filtration rate in healthy adults. N Engl J Med. 2017;376:2349–57.
Fattah H, Layton A, Vallon V. How do kidneys adapt to a deficit or loss in nephron number? Physiology (Bethesda). 2019;34:189–97.
Cherney DZI, Dekkers CCJ, Barbour SJ, Cattran D, Abdul Gafor AH, Greasley PJ, et al. Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol. 2020;8:582–93.
Yan H, Xu J, Xu Z, Yang B, Luo P, He Q. Defining therapeutic targets for renal fibrosis: exploiting the biology of pathogenesis. Biomed Pharmacother. 2021;143:112115.
Fine LG, Bandyopadhay D, Norman JT. Is there a common mechanism for the progression of different types of renal diseases other than proteinuria? Towards the unifying theme of chronic hypoxia. Kidney Int Suppl. 2000;75:S22–6.
Tanaka T, Nangaku M. The role of hypoxia, increased oxygen consumption, and hypoxia-inducible factor-1 alpha in progression of chronic kidney disease. Curr Opin Nephrol Hypertens. 2010;19:43–50.
Zhang L, Liu L, Bai M, Liu M, Wei L, Yang Z, et al. Hypoxia-induced HE4 in tubular epithelial cells promotes extracellular matrix accumulation and renal fibrosis via NF-κB. Faseb j. 2020;34:2554–67.
LeBleu VS, Teng Y, O’Connell JT, Charytan D, Müller GA, Müller CA, et al. Identification of human epididymis protein-4 as a fibroblast-derived mediator of fibrosis. Nat Med. 2013;19:227–31.
Chen P, Yang Q, Li X, Qin Y. Potential association between elevated serum human epididymis protein 4 and renal fibrosis: a systemic review and meta-analysis. Medicine (Baltimore). 2017;96:e7824.
Huang X, Guo X, Yan G, Zhang Y, Yao Y, Qiao Y, et al. Dapagliflozin attenuates contrast-induced acute kidney injury by regulating the HIF-1α/HE4/NF-κB pathway. J Cardiovasc Pharmacol. 2022;79:904–13.
Hodrea J, Balogh DB, Hosszu A, Lenart L, Besztercei B, Koszegi S, et al. Reduced O-GlcNAcylation and tubular hypoxia contribute to the antifibrotic effect of SGLT2 inhibitor dapagliflozin in the diabetic kidney. Am J Physiol Renal Physiol. 2020;318:F1017–29.
Li J, Liu H, Takagi S, Nitta K, Kitada M, Srivastava SP, et al. Renal protective effects of empagliflozin via inhibition of EMT and aberrant glycolysis in proximal tubules. JCI Insight. 2020;5:1.
Ndibalema AR, Kabuye D, Wen S, Li L, Li X, Fan Q. Empagliflozin protects against proximal renal tubular cell injury induced by high glucose via regulation of hypoxia-inducible factor 1-alpha. Diabetes Metab Syndr Obes. 2020;13:1953–67.
Bessho R, Takiyama Y, Takiyama T, Kitsunai H, Takeda Y, Sakagami H, et al. Hypoxia-inducible factor-1α is the therapeutic target of the SGLT2 inhibitor for diabetic nephropathy. Sci Rep. 2019;9:14754.
Ravindran S, Munusamy S. Renoprotective mechanisms of sodium–glucose co-transporter 2 (SGLT2) inhibitors against the progression of diabetic kidney disease. J Cell Physiol. 2022;237:1182–205.
Nordquist L, Friederich-Persson M, Fasching A, Liss P, Shoji K, Nangaku M, et al. Activation of hypoxia-inducible factors prevents diabetic nephropathy. J Am Soc Nephrol. 2015;26:328–38.
Jiao Y, Jiang H, Lu H, Yang Y, Zhang Y, Zhang K, et al. Deficiency of hypoxia inducible factor-1α promoted progression of diabetic nephropathy with hypertension. Exp Ther Med. 2018;16:3658–62.
Hesp AC, Schaub JA, Prasad PV, Vallon V, Laverman GD, Bjornstad P, et al. The role of renal hypoxia in the pathogenesis of diabetic kidney disease: a promising target for newer renoprotective agents including SGLT2 inhibitors? Kidney Int. 2020;98:579–89.
Xu ZH, Wang C, He YX, Mao XY, Zhang MZ, Hou YP, et al. Hypoxia-inducible factor protects against acute kidney injury via the Wnt/β-catenin signaling pathway. Am J Physiol Renal Physiol. 2022;322:F611–24.
Chen B, Brem AS, Gong R. The Janus view: dual roles for hypoxia-inducible factor in renal repair after acute kidney injury. Am J Physiol Renal Physiol. 2022;323:F1-f3.
Kanbay M, Tapoi L, Ureche C, Tanriover C, Cevik E, Demiray A, et al. Effect of sodium–glucose cotransporter 2 inhibitors on hemoglobin and hematocrit levels in type 2 diabetes: a systematic review and meta-analysis. Int Urol Nephrol. 2022;54:827–41.
Afsar B, Afsar RE, Ertuglu LA, Covic A, Kanbay M. Nutrition, immunology, and kidney: looking beyond the horizons. Curr Nutr Rep. 2022;11:69–81.
Komada T, Muruve DA. The role of inflammasomes in kidney disease. Nat Rev Nephrol. 2019;15:501–20.
Zhang H, Wang Z. Effect and regulation of the NLRP3 inflammasome during renal fibrosis. Front Cell Dev Biol. 2019;7:379.
Benetti E, Mastrocola R, Vitarelli G, Cutrin JC, Nigro D, Chiazza F, et al. Empagliflozin protects against diet-induced NLRP-3 inflammasome activation and lipid accumulation. J Pharmacol Exp Ther. 2016;359:45–53.
Ke Q, Shi C, Lv Y, Wang L, Luo J, Jiang L, et al. SGLT2 inhibitor counteracts NLRP3 inflammasome via tubular metabolite itaconate in fibrosis kidney. Faseb j. 2022;36:e22078.
Youm YH, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, Kim D, et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med. 2015;21:263–9.
Wu X, Li H, Wan Z, Wang R, Liu J, Liu Q, et al. The combination of ursolic acid and empagliflozin relieves diabetic nephropathy by reducing inflammation, oxidative stress and renal fibrosis. Biomed Pharmacother. 2021;144:112267.
Wang XX, Levi J, Luo Y, Myakala K, Herman-Edelstein M, Qiu L, et al. SGLT2 protein expression is increased in human diabetic nephropathy: SGLT2 protein inhibition decreases renal lipid accumulation, inflammation, and the development of nephropathy in diabetic mice. J Biol Chem. 2017;292:5335–48.
Tang L, Wu Y, Tian M, Sjöström CD, Johansson U, Peng XR, et al. Dapagliflozin slows the progression of the renal and liver fibrosis associated with type 2 diabetes. Am J Physiol Endocrinol Metab. 2017;313:E563–76.
Terami N, Ogawa D, Tachibana H, Hatanaka T, Wada J, Nakatsuka A, et al. Long-term treatment with the sodium glucose cotransporter 2 inhibitor, dapagliflozin, ameliorates glucose homeostasis and diabetic nephropathy in db/db mice. PLoS ONE. 2014;9:e100777.
Okuma H, Mori K, Nakamura S, Sekine T, Ogawa Y, Tsuchiya K. Ipragliflozin ameliorates diabetic nephropathy associated with perirenal adipose expansion in mice. Int J Mol Sci. 2021;22:1.
Hatanaka T, Ogawa D, Tachibana H, Eguchi J, Inoue T, Yamada H, et al. Inhibition of SGLT2 alleviates diabetic nephropathy by suppressing high glucose-induced oxidative stress in type 1 diabetic mice. Pharmacol Res Perspect. 2016;4:e00239.
Ojima A, Matsui T, Nishino Y, Nakamura N, Yamagishi S. Empagliflozin, an inhibitor of sodium–glucose cotransporter 2 exerts anti-inflammatory and antifibrotic effects on experimental diabetic nephropathy partly by suppressing AGEs-receptor axis. Horm Metab Res. 2015;47:686–92.
Yao D, Wang S, Wang M, Lu W. Renoprotection of dapagliflozin in human renal proximal tubular cells via the inhibition of the high mobility group box 1-receptor for advanced glycation end products-nuclear factor-κB signaling pathway. Mol Med Rep. 2018;18:3625–30.
Abbas NAT, El Salem A, Awad MM. Empagliflozin, SGLT(2) inhibitor, attenuates renal fibrosis in rats exposed to unilateral ureteric obstruction: potential role of klotho expression. Naunyn Schmiedebergs Arch Pharmacol. 2018;391:1347–60.
Huang J, Chen Z, Li J, Chen Q, Li J, Gong W, et al. Protein kinase CK2α catalytic subunit ameliorates diabetic renal inflammatory fibrosis via NF-κB signaling pathway. Biochem Pharmacol. 2017;132:102–17.
Panchapakesan U, Pegg K, Gross S, Komala MG, Mudaliar H, Forbes J, et al. Effects of SGLT2 inhibition in human kidney proximal tubular cells—Renoprotection in diabetic nephropathy? PLoS ONE. 2013;8:e54442.
Heerspink HJL, Perco P, Mulder S, Leierer J, Hansen MK, Heinzel A, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia. 2019;62:1154–66.
Stieger N, Worthmann K, Teng B, Engeli S, Das AM, Haller H, et al. Impact of high glucose and transforming growth factor-β on bioenergetic profiles in podocytes. Metabolism. 2012;61:1073–86.
Das NA, Carpenter AJ, Belenchia A, Aroor AR, Noda M, Siebenlist U, et al. Empagliflozin reduces high glucose-induced oxidative stress and miR-21-dependent TRAF3IP2 induction and RECK suppression, and inhibits human renal proximal tubular epithelial cell migration and epithelial-to-mesenchymal transition. Cell Signal. 2020;68:109506.
Woods TC, Satou R, Miyata K, Katsurada A, Dugas CM, Klingenberg NC, et al. Canagliflozin prevents intrarenal angiotensinogen augmentation and mitigates kidney injury and hypertension in mouse model of type 2 diabetes mellitus. Am J Nephrol. 2019;49:331–42.
Tanaka S, Sugiura Y, Saito H, Sugahara M, Higashijima Y, Yamaguchi J, et al. Sodium–glucose cotransporter 2 inhibition normalizes glucose metabolism and suppresses oxidative stress in the kidneys of diabetic mice. Kidney Int. 2018;94:912–25.
Ferrannini E, Muscelli E, Frascerra S, Baldi S, Mari A, Heise T, et al. Metabolic response to sodium–glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124:499–508.
DeFronzo RA, Reeves WB, Awad AS. Pathophysiology of diabetic kidney disease: impact of SGLT2 inhibitors. Nat Rev Nephrol. 2021;17:319–34.
Packer M. SGLT2 inhibitors produce cardiorenal benefits by promoting adaptive cellular reprogramming to induce a state of fasting mimicry: a paradigm shift in understanding their mechanism of action. Diabetes Care. 2020;43:508–11.
Tomita I, Kume S, Sugahara S, Osawa N, Yamahara K, Yasuda-Yamahara M, et al. SGLT2 inhibition mediates protection from diabetic kidney disease by promoting ketone body-induced mTORC1 inhibition. Cell Metab. 2020;32:404-19.e6.
Hawley SA, Ford RJ, Smith BK, Gowans GJ, Mancini SJ, Pitt RD, et al. The Na+/glucose cotransporter inhibitor canagliflozin activates AMPK by inhibiting mitochondrial function and increasing cellular AMP levels. Diabetes. 2016;65:2784–94.
Han Y, Xiong S, Zhao H, Yang S, Yang M, Zhu X, et al. Lipophagy deficiency exacerbates ectopic lipid accumulation and tubular cells injury in diabetic nephropathy. Cell Death Dis. 2021;12:1031.
Zhang Z, Ni L, Zhang L, Zha D, Hu C, Zhang L, et al. Empagliflozin regulates the AdipoR1/p-AMPK/p-ACC pathway to alleviate lipid deposition in diabetic nephropathy. Diabetes Metab Syndr Obes. 2021;14:227–40.
Ding H, Jiang L, Xu J, Bai F, Zhou Y, Yuan Q, et al. Inhibiting aerobic glycolysis suppresses renal interstitial fibroblast activation and renal fibrosis. Am J Physiol Renal Physiol. 2017;313:F561–75.
Inoue MK, Matsunaga Y, Nakatsu Y, Yamamotoya T, Ueda K, Kushiyama A, et al. Possible involvement of normalized Pin1 expression level and AMPK activation in the molecular mechanisms underlying renal protective effects of SGLT2 inhibitors in mice. Diabetol Metab Syndr. 2019;11:57.
Lee YH, Kim SH, Kang JM, Heo JH, Kim DJ, Park SH, et al. Empagliflozin attenuates diabetic tubulopathy by improving mitochondrial fragmentation and autophagy. Am J Physiol Renal Physiol. 2019;317:F767–80.
Goldberg H, Whiteside C, Fantus IG. O-linked β-N-acetylglucosamine supports p38 MAPK activation by high glucose in glomerular mesangial cells. Am J Physiol Endocrinol Metab. 2011;301:E713–26.
Shibusawa R, Yamada E, Okada S, Nakajima Y, Bastie CC, Maeshima A, et al. Dapagliflozin rescues endoplasmic reticulum stress-mediated cell death. Sci Rep. 2019;9:9887.
Afsar B, Hornum M, Afsar RE, Ertuglu LA, Ortiz A, Covic A, et al. Mitochondrion-driven nephroprotective mechanisms of novel glucose lowering medications. Mitochondrion. 2021;58:72–82.
Xie Y, Jing E, Cai H, Zhong F, Xiao W, Gordon RE, et al. Reticulon-1A mediates diabetic kidney disease progression through endoplasmic reticulum–mitochondrial contacts in tubular epithelial cells. Kidney Int. 2022;102:293–306.
Siragy HM, Carey RM. Role of the intrarenal renin-angiotensin-aldosterone system in chronic kidney disease. Am J Nephrol. 2010;31:541–50.
Gross O, Schulze-Lohoff E, Koepke ML, Beirowski B, Addicks K, Bloch W, et al. Antifibrotic, nephroprotective potential of ACE inhibitor vs. AT1 antagonist in a murine model of renal fibrosis. Nephrol Dial Transpl. 2004;19:1716–23.
Rubel D, Stock J, Ciner A, Hiller H, Girgert R, Müller GA, et al. Antifibrotic, nephroprotective effects of paricalcitol versus calcitriol on top of ACE-inhibitor therapy in the COL4A3 knockout mouse model for progressive renal fibrosis. Nephrol Dial Transpl. 2014;29:1012–9.
Feldman DL, Jin L, Xuan H, Contrepas A, Zhou Y, Webb RL, et al. Effects of aliskiren on blood pressure, albuminuria, and (pro)renin receptor expression in diabetic TG(mRen-2)27 rats. Hypertension. 2008;52:130–6.
Han KH, Kang YS, Han SY, Jee YH, Lee MH, Han JY, et al. Spironolactone ameliorates renal injury and connective tissue growth factor expression in type II diabetic rats. Kidney Int. 2006;70:111–20.
Koszegi S, Molnar A, Lenart L, Hodrea J, Balogh DB, Lakat T, et al. RAAS inhibitors directly reduce diabetes-induced renal fibrosis via growth factor inhibition. J Physiol. 2019;597:193–209.
Morrissey JJ, Klahr S. Effect of AT2 receptor blockade on the pathogenesis of renal fibrosis. Am J Physiol. 1999;276:F39-45.
Crowley SD, Rudemiller NP. Immunologic effects of the renin-angiotensin system. J Am Soc Nephrol. 2017;28:1350–61.
Liu Z, Huang XR, Chen HY, Penninger JM, Lan HY. Loss of angiotensin-converting enzyme 2 enhances TGF-β/Smad-mediated renal fibrosis and NF-κB-driven renal inflammation in a mouse model of obstructive nephropathy. Lab Invest. 2012;92:650–61.
Mao N, Tan RZ, Wang SQ, Wei C, Shi XL, Fan JM, et al. Ginsenoside Rg1 inhibits angiotensin II-induced podocyte autophagy via AMPK/mTOR/PI3K pathway. Cell Biol Int. 2016;40:917–25.
Lizakowski S, Tylicki L, Renke M, Rutkowski P, Heleniak Z, Sławińska-Morawska M, et al. Aliskiren and perindopril reduce the levels of transforming growth factor-β in patients with non-diabetic kidney disease. Am J Hypertens. 2012;25:636–9.
Cuevas CA, Gonzalez AA, Inestrosa NC, Vio CP, Prieto MC. Angiotensin II increases fibronectin and collagen I through the β-catenin-dependent signaling in mouse collecting duct cells. Am J Physiol Renal Physiol. 2015;308:F358–65.
Shin SJ, Chung S, Kim SJ, Lee EM, Yoo YH, Kim JW, et al. Effect of sodium–glucose co-transporter 2 inhibitor, dapagliflozin, on renal renin-angiotensin system in an animal model of type 2 diabetes. PLoS ONE. 2016;11:e0165703.
Miyata KN, Lo CS, Zhao S, Liao MC, Pang Y, Chang SY, et al. Angiotensin II up-regulates sodium–glucose co-transporter 2 expression and SGLT2 inhibitor attenuates Ang II-induced hypertensive renal injury in mice. Clin Sci (Lond). 2021;135:943–61.
Gallo LA, Ward MS, Fotheringham AK, Zhuang A, Borg DJ, Flemming NB, et al. Once daily administration of the SGLT2 inhibitor, empagliflozin, attenuates markers of renal fibrosis without improving albuminuria in diabetic db/db mice. Sci Rep. 2016;6:26428.
Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab. 2013;15:853–62.
Tanaka H, Takano K, Iijima H, Kubo H, Maruyama N, Hashimoto T, et al. Factors affecting canagliflozin-induced transient urine volume increase in patients with type 2 diabetes mellitus. Adv Ther. 2017;34:436–51.
Takeshige Y, Fujisawa Y, Rahman A, Kittikulsuth W, Nakano D, Mori H, et al. A sodium–glucose co-transporter 2 inhibitor empagliflozin prevents abnormality of circadian rhythm of blood pressure in salt-treated obese rats. Hypertens Res. 2016;39:415–22.
Sawamura T, Karashima S, Nagase S, Nambo H, Shimizu E, Higashitani T, et al. Effect of sodium–glucose cotransporter-2 inhibitors on aldosterone-to-renin ratio in diabetic patients with hypertension: a retrospective observational study. BMC Endocr Disord. 2020;20:177.
Ryu ES, Kim MJ, Shin HS, Jang YH, Choi HS, Jo I, et al. Uric acid-induced phenotypic transition of renal tubular cells as a novel mechanism of chronic kidney disease. Am J Physiol Renal Physiol. 2013;304:F471–80.
Bailey CJ. Uric acid and the cardio-renal effects of SGLT2 inhibitors. Diabetes Obes Metab. 2019;21:1291–8.
Novikov A, Fu Y, Huang W, Freeman B, Patel R, van Ginkel C, et al. SGLT2 inhibition and renal urate excretion: role of luminal glucose, GLUT9, and URAT1. Am J Physiol Renal Physiol. 2019;316:F173–85.
Suijk DLS, van Baar MJB, van Bommel EJM, Iqbal Z, Krebber MM, Vallon V, et al. SGLT2 inhibition and uric acid excretion in patients with type 2 diabetes and normal kidney function. Clin J Am Soc Nephrol. 2022;17:663–71.
Huang F, Zhao Y, Wang Q, Hillebrands JL, van den Born J, Ji L, et al. Dapagliflozin attenuates renal tubulointerstitial fibrosis associated with type 1 diabetes by regulating STAT1/TGFβ1 signaling. Front Endocrinol (Lausanne). 2019;10:441.
Kanbay M, Demiray A, Afsar B, Covic A, Tapoi L, Ureche C, et al. Role of klotho in the development of essential hypertension. Hypertension. 2021;77:740–50.
Zhou L, Mo H, Miao J, Zhou D, Tan RJ, Hou FF, et al. Klotho ameliorates kidney injury and fibrosis and normalizes blood pressure by targeting the renin-angiotensin system. Am J Pathol. 2015;185:3211–23.
Zhang Y, Nakano D, Guan Y, Hitomi H, Uemura A, Masaki T, et al. A sodium–glucose cotransporter 2 inhibitor attenuates renal capillary injury and fibrosis by a vascular endothelial growth factor-dependent pathway after renal injury in mice. Kidney Int. 2018;94:524–35.
Gomez IG, Roach AM, Nakagawa N, Amatucci A, Johnson BG, Dunn K, et al. TWEAK-Fn14 signaling activates myofibroblasts to drive progression of fibrotic kidney disease. J Am Soc Nephrol. 2016;27:3639–52.
Shen ZJ, Hu J, Shiizaki K, Kuro-o M, Malter JS. Phosphate-induced renal fibrosis requires the prolyl isomerase pin1. PLoS ONE. 2016;11:e0150093.
Liu H, Sridhar VS, Lovblom LE, Lytvyn Y, Burger D, Burns K, et al. Markers of kidney injury, inflammation, and fibrosis associated with ertugliflozin in patients with CKD and diabetes. Kidney Int Rep. 2021;6:2095–104.
Ma Q, Steiger S, Anders HJ. Sodium glucose transporter-2 inhibition has no renoprotective effects on non-diabetic chronic kidney disease. Physiol Rep. 2017;5:1.
Droebner K, Pavkovic M, Grundmann M, Hartmann E, Goea L, Nordlohne J, et al. Direct blood pressure-independent anti-fibrotic effects by the selective nonsteroidal mineralocorticoid receptor antagonist finerenone in progressive models of kidney fibrosis. Am J Nephrol. 2021;52:588–601.
Zhang Y, Thai K, Kepecs DM, Gilbert RE. Sodium–glucose linked cotransporter-2 inhibition does not attenuate disease progression in the rat remnant kidney model of chronic kidney disease. PLoS ONE. 2016;11:e0144640.
Vallon V, Gerasimova M, Rose MA, Masuda T, Satriano J, Mayoux E, et al. SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice. Am J Physiol Renal Physiol. 2014;306:F194-204.
Gangadharan Komala M, Gross S, Mudaliar H, Huang C, Pegg K, Mather A, et al. Inhibition of kidney proximal tubular glucose reabsorption does not prevent against diabetic nephropathy in type 1 diabetic eNOS knockout mice. PLoS ONE. 2014;9:e108994.
Zeng S, Delic D, Chu C, Xiong Y, Luo T, Chen X, et al. Antifibrotic effects of low dose SGLT2 inhibition with empagliflozin in comparison to Ang II receptor blockade with telmisartan in 5/6 nephrectomised rats on high salt diet. Biomed Pharmacother. 2022;146:112606.
Tauber P, Sinha F, Berger RS, Gronwald W, Dettmer K, Kuhn M, et al. Empagliflozin reduces renal hyperfiltration in response to uninephrectomy, but is not nephroprotective in UNx/DOCA/Salt mouse models. Front Pharmacol. 2021;12:761855.
Kojima N, Williams JM, Takahashi T, Miyata N, Roman RJ. Effects of a new SGLT2 inhibitor, luseogliflozin, on diabetic nephropathy in T2DN rats. J Pharmacol Exp Ther. 2013;345:464–72.
Kojima N, Williams JM, Slaughter TN, Kato S, Takahashi T, Miyata N, et al. Renoprotective effects of combined SGLT2 and ACE inhibitor therapy in diabetic Dahl S rats. Physiol Rep. 2015;3:1.
Abdel-Wahab AF, Bamagous GA, Al-Harizy RM, ElSawy NA, Shahzad N, Ibrahim IA, et al. Renal protective effect of SGLT2 inhibitor dapagliflozin alone and in combination with irbesartan in a rat model of diabetic nephropathy. Biomed Pharmacother. 2018;103:59–66.
Jaikumkao K, Pongchaidecha A, Chueakula N, Thongnak LO, Wanchai K, Chatsudthipong V, et al. Dapagliflozin, a sodium–glucose co-transporter-2 inhibitor, slows the progression of renal complications through the suppression of renal inflammation, endoplasmic reticulum stress and apoptosis in prediabetic rats. Diabetes Obes Metab. 2018;20:2617–26.
Tahara A, Takasu T. Prevention of progression of diabetic nephropathy by the SGLT2 inhibitor ipragliflozin in uninephrectomized type 2 diabetic mice. Eur J Pharmacol. 2018;830:68–75.
Wang D, Luo Y, Wang X, Orlicky DJ, Myakala K, Yang P, et al. The sodium-glucose cotransporter 2 inhibitor dapagliflozin prevents renal and liver disease in western diet induced obesity mice. Int J Mol Sci. 2018;19:1.
Ali BH, Al Salam S, Al Suleimani Y, Al Za’abi M, Abdelrahman AM, Ashique M, et al. Effects of the SGLT-2 inhibitor canagliflozin on adenine-induced chronic kidney disease in rats. Cell Physiol Biochem. 2019;52:27–39.
Cai T, Ke Q, Fang Y, Wen P, Chen H, Yuan Q, et al. Sodium–glucose cotransporter 2 inhibition suppresses HIF-1α-mediated metabolic switch from lipid oxidation to glycolysis in kidney tubule cells of diabetic mice. Cell Death Dis. 2020;11:390.
Castoldi G, Carletti R, Ippolito S, Colzani M, Barzaghi F, Stella A, et al. Renal anti-fibrotic effect of sodium glucose cotransporter 2 inhibition in angiotensin II-dependent hypertension. Am J Nephrol. 2020;51:119–29.
Hasan R, Lasker S, Hasan A, Zerin F, Zamila M, Parvez F, et al. Canagliflozin ameliorates renal oxidative stress and inflammation by stimulating AMPK-Akt-eNOS pathway in the isoprenaline-induced oxidative stress model. Sci Rep. 2020;10:14659.
Nespoux J, Patel R, Zhang H, Huang W, Freeman B, Sanders PW, et al. Gene knockout of the Na(+)-glucose cotransporter SGLT2 in a murine model of acute kidney injury induced by ischemia-reperfusion. Am J Physiol Renal Physiol. 2020;318:F1100–12.
Yamato M, Kato N, Kakino A, Yamada KI, Inoguchi T. Low dose of sodium–glucose transporter 2 inhibitor ipragliflozin attenuated renal dysfunction and interstitial fibrosis in adenine-induced chronic kidney disease in mice without diabetes. Metabol Open. 2020;7:100049.
Castoldi G, Carletti R, Ippolito S, Colzani M, Barzaghi F, Stella A, et al. Sodium–glucose cotransporter 2 inhibition prevents renal fibrosis in cyclosporine nephropathy. Acta Diabetol. 2021;58:1059–70.
Kolkhof P, Hartmann E, Freyberger A, Pavkovic M, Mathar I, Sandner P, et al. Effects of finerenone combined with empagliflozin in a model of hypertension-induced end-organ damage. Am J Nephrol. 2021;52:642–52.
Pan X, Phanish MK, Baines DL, Dockrell MEC. High glucose-induced Smad3 linker phosphorylation and CCN2 expression are inhibited by dapagliflozin in a diabetic tubule epithelial cell model. Biosci Rep. 2021;41:1.
Ko EJ, Shin YJ, Cui S, Lim SW, Chung BH, Yang CW. Effect of dual inhibition of DPP4 and SGLT2 on tacrolimus-induced diabetes mellitus and nephrotoxicity in a rat model. Am J Transpl. 2022;22:1537–49.
Funding
None declared.
Author information
Authors and Affiliations
Contributions
BA was the owner of the project, gathered data, wrote the manuscript. REA helped to write the manuscript, reviewed, and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afsar, B., Afsar, R.E. Sodium–glucose cotransporter inhibitors and kidney fibrosis: review of the current evidence and related mechanisms. Pharmacol. Rep 75, 44–68 (2023). https://doi.org/10.1007/s43440-022-00442-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-022-00442-4