Abstract
Diabetic kidney disease (DKD), a severe microvascular complication of diabetes mellitus, is the primary cause of end stage renal disease (ESRD). Sodium-glucose cotransporter 2 (SGLT2) inhibitors are a class of novel anti-diabetic drugs for DKD, which have the potential to prevent renal function from failing. The involved mechanisms have garnered considerable attention. Besides hypoglycemic effect, it seems that various glucose-independent nephroprotective mechanisms also have a role. Among them, improvement in tubuloglomerular feedback is considered as the main reason, followed by reduced intraglomerular pressure and fluid load. In addition, reduced blood pressure, anti-inflammatory effects, nutrient deprivation signaling as well as improved endothelial function are also important. In the future, clinical trials and mechanistic studies might further complement the current knowledge on SGLT2 inhibitors and facilitate to translate these agents to clinical use. Here, we review these mechanisms of SGLT2 inhibitors with an emphasis on kidney protective effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic kidney disease (DKD), one of the most common microvascular complications of diabetes mellitus, is projected to affect almost 700 million adults by 2045.[1] As the leading cause of end stage renal disease (ESRD) around the world, DKD can lead to a reduced life expectancy and tremendous economic burdens. This chronic progressive disorder is also the main reason for dialysis or kidney transplant currently.[2] In addition to the mainstay of current therapies consisting of restrict blood glucose control and blood pressure control with renin-angiotensin system (RAS) blockade, however, there is lack of long-term effective treatment for DKD.[3].
Sodium-glucose cotransporter 2 (SGLT2) inhibitors, a novel class of anti-diabetic agents, have ushered in optimism and hope for the treatment of DKD.[4] These drugs exert significant glucose-lowering effects by blunting glucose reabsorption from the glomerular filtrate through blocking SGLT2 transporter. Results from completed large clinical trials of SGLT2 inhibitors have demonstrated their surprising potential to slow the development and progression of kidney diseases in people with type 2 diabetes mellitus (T2DM) consistently. Recent large cardiovascular outcome trials with SGLT2 inhibitors, such as EMPA-REG OUTCOME with empagliflozin, the CANVAS Program with canagliflozin and DECLARE TIMI-58 with dapagliflozin, all showed unexpected amelioration in renal outcomes which were determined as secondary end points at the beginning of these trials.[5,6,7] CREDENCE with canagliflozin was a large prospective study specifically designed to explore the efficacy of canagliflozin in patients with established DKD. During this trial, canagliflozin significantly reduced relative risk of primary composite renal outcome comprising ESRD, a doubling of the serum creatinine level, or death from renal or cardiovascular causes.[8] According to the positive results from these trials linked to canagliflozin, the United States Food and Drug Administration (FDA) has approved this agent to apply to patients with diabetes and chronic kidney disease in 2019.[9].
Of note, renoprotection of SGLT2 inhibitors observed in these studies seems not only dependent on glucose-lowering effects. Many non-glycaemic pathways are likely to be involved in improved renal function with SGLT2 inhibition. As a result, emerging well-designed clinical trials and mechanistic experiments are designed to provide new insight into protective effects of these drugs. On the basis of these studies recently, we summarize available evidence and discuss potential mechanisms underlying the renal protection of SGLT2 inhibitors. In the following review, we will first describe SGLT2 and its inhibitors in brief. Next, we focus on major and secondary mechanisms of SGLT2 inhibitors in renal protection, with an emphasis on effects independent of glycaemic control. (Fig. 1)
SGLT2 and SGLT2 inhibitors
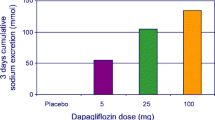
SGLTs belong to a family of membrane proteins and have the potential to transport glucose, some ions as well as amino acids. The main members of SGLT family are consist of SGLT1 and SGLT2. SGLT1 is primarily found in intestinal tract, while SGLT2 is mainly located in the early S1/S2 proximal tubule segment and responsible for approximately 80 − 90% glucose reabsorption from the glomerular filtrate. The remaining glucose is reabsorbed by SGLT1 in the late S2/S3 tubule segment.[10, 11] Ascribed to active glucose cotransport, almost all of glucose in the filtrate is reabsorbed under normoglycemic conditions. Due to the key role of SGLT2 in tubular reabsorption, inhibiting this transporter is thought to be a promising therapy in patients with T2DM. The first discovered SGLT2 inhibitor, phlorizin, extracted from the root bark of the apple tree, has non-selective inhibitory effects on SGLT2 and SGLT1. It was surprisingly found to have the potential to normalize the level of blood glucose and restore insulin sensitivity in diabetic rats without an intact pancreas in the twentieth century.[12] Owing to low oral bioavailability and adverse effects of phlorizin, it was unsuitable for clinical application. Subsequently, contemporary anti-diabetic drugs with higher selectivity for SGLT2 over SGLT1 and rapid oral absorption were developed. Four kinds of SGLT2 inhibitors are currently approved by FDA, including empagliflozin, canagliflozin, dapagliflozin, ertugliflozin. (Fig. 2)
Renoprotective effects with SGLT2 inhibitiors
Glycaemic control
Hyperglycaemia is considered as an important initial factor in DKD. Under diabetic condition, SGLT2 expression is upregulated in response to increased glucose in tubule. As a result, excessive glucose is reabsorbed from the filtrate to circulation, contributing to sustaining high plasma glucose concentrations. A great number of studies in real-world settings demonstrate that SGLT2 inhibitors reduce the level of fasting blood glucose and improve oral glucose tolerance in patients with T2DM, along with a slight amelioration in glycated hemoglobin (HbA1c) level.[13] Through blocking active reabsorption of SGLT2 and increasing urinary glucose excretion, these agents exert substantial glucose-lowering activity. Interestingly, this property is independent on insulin secretion. In addition, due to compensatory mechanism in kidney, when pharmacological inhibitor of SGLT2 is applied, SGLT1-mediated transport will be upregulated to reabsorb 40-50% glucose from the tubule. Hence, hypoglycemia is less likely to be observed with SGLT2 inhibitors than other traditional anti-diabetic agents. SGLT2 inhibitors play a significant role in maintaining glucose homoeostasis. Results from a study in mice with T2DM demonstrate dapagliflozin enhances renal gluconeogenesis and increase levels of enzyme associated with gluconeogenesis.[14] This finding is consistent with several randomized controlled researches in real-world settings. Increased endogenous glucose production is observed with SGLT2 inhibitor therapy, even in patients with T2DM after renal denervation or oral glucose load.[15, 16] Of note, the improved glycaemic control is unlikely fully to explain the renal benefits with SGLT2 inhibitors, suggesting additional renal mechanisms also work.
In addition to SGLT2 inhibition, there are many emerging anti-diabetic drugs, such as glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and dipeptidyl peptidase IV inhibitors (DPP4i). Many studies are designed to evaluate the benefits and safety of these agents combined with SGLT2 inhibitors. Data from a meta-analysis demonstrates a greater reduction in HbA1c and fasting plasma glucose is induced by combination therapy with SGLT2 inhibition and GLP-1 RAs than monotherapy.[17] This similar glucose-lowering effects are also observed in a rat model of T2DM with dual inhibition of DPP4 and SGLT2.[18] Of note, the risk of hypoglycaemia is significantly with combination therapy.
Natriuresis and reduction in blood pressure
Hypertension is of great significance in accelerating the progression of DKD. A meta-analysis based on clinical studies suggests that SGLT2 inhibitors are able to decrease both systolic and diastolic blood pressure.[19] Currently, natriuresis and osmotic diuresis are thought to be the main reason for the blood pressure-lowering effect with SGLT2 inhibitors. Due to the coupled reabsorption of glucose and sodium, inhibition of SGLT2 in the proximal tubule contributes to enhanced sodium excretion and reduced plasma volume following by decreased blood pressure. In addition, RAAS blockade with angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) is a class of traditional drugs for hypertension control in DKD. Recently, several studies are devoted to evaluate the efficiency of combination therapy with SGLT2 inhibitors and RAAS blockade in the setting of diabetes. In an animal model of DKD with established hypertension, combination treatment with lisinopril and empagliflozin demonstrates synergistic effect on renal protection with comparison to ACEI/ARBs alone.[20] The finding is further supported by evidence in real-world condition. A meta-analysis based on clinical researches suggests that the combination therapy could achieve a better control of hypertension and hyperglycaemia than monotherapy, leading to improved renal outcomes. Moreover, it should be noted that the risk of hypoglycaemia is also increased.[21].
Interestingly, aside from SGLT2, a growing body of studies have demonstrated additional ion transporters are also implicated in sodium transport and water-salt balance in the tubule. NaCl cotransporter, located in the distal convoluted tubule, is one of the important transporters responsible for blood pressure control. In a model of obesity and diabetes, SGLT2 inhibitors enhance natriuresis and reduce renal reabsorption via regulating activity of this cotransporter indirectly.[22] What’s more, another ion transporter, sodium-hydrogen exchanger 3 (NHE3), which functions to mediate almost 70% of sodium reabsorption in the proximal tubule, is found to be upregulated in the context of diabetes. The upregulation of NHE3 expression is complicated in maintaining high level of blood pressure. Interestingly, NHE3 is colocalized with SGLT2 in the kidney and their activity is tightly linked to each other.[23] Inhibition of SGLT2 has been proved to effectively modulating NHE3 activity negatively, while natriuresis induced by SGLT2 inhibitors is reduced in tubule-specific NHE3 knock-down mice. The phenomenon suggests that part of natriuresis by SGLT2 inhibitors is mediated by suppressing NHE3, resulting in improved renal salt and water handling, reduced fluid load and relieved hypertension.[24,25,26] Of note, in the setting of non-diabetic heart failure, empagliflozin also exerts inhibitory effect on NHE3, suggesting that suppression on NHE3 by this agent is present in both absence and presence of diabetes, while the detailed mechanism remains to be elucidated. Furthermore, another sodium-hydrogen exchanger NHE1 which is ubiquitously expressed in the heart, provides a novel insight into off-target effects by SGLT2 inhibitors in cardiomyocytes.[27] Whether the downregulation of NHE3 in response to SGLT2 inhibitors in kidney could exert similar influence which is analogous to NHE1 in cardiomyocytes has not been determined.
Restored tubuloglomerular feedback
Hyperfiltration in glomeruli is one of the key characters of DKD. In the setting of diabetes, renal proximal tubule will become maladaptive hypertrophy and SGLT2 expression is also excessively upregulated in response to heavy glucose load in tubule. Hence, upstream glucose and sodium reabsorption is increased through active transporters, resulting in reduced sodium delivery to the macula densa of the juxtaglomerular apparatus. As a consequence, decreased sodium concentration is sensed by the macula densa, which contributes to the activation of tubuloglomerular feedback (TGF) and changes in diameters of afferent and efferent arteriolar. Excessive TGF activation plays a central role in sustained hyperfiltration and high intraglomerular pressure, leading to serious glomerular basement membrane (GBM) damage and podocyte loss.[28] It is generally recognized that restoration in TGF is the primary mechanism responsible for the glucose-independent benefits of SGLT2 inhibitors in kidney. In many large clinical trials, a slight estimated glomerular filtration rate (eGFR) dip after initial treatment with SGLT2 inhibitors is observed, suggesting direct hemodynamic effects of these drugs.[29] SGLT2 inhibitors will blunt upstream sodium and glucose reabsorption, hence increase sodium delivery to macula densa. As a result, this signal received by macula densa leads to a reduction in intraglomerular pressure and hyperfiltration via restored TGF. Of interest, Adenosine signaling is proved to play an important role in this process, although there are some differences in different models of diabetes. In a murine model of type 1 diabetes (T1DM), empagliflozin activates A1 adenosine receptor which resulted in afferent arteriolar vasoconstriction, while efferent vasodilation via A2 adenosine receptor is observed in response to dapagliflozin among T2DM population.[30] Altered adenosine signaling seems to work in a context-dependent manner. There may be an explanation for this difference that increased vasoactive prostaglandin will counteract the vasoconstrictive effect of A1 adenosine activation in the setting of T2DM.[31] In addition, functional and structural variances in DKD between T1DM and T2DM are equally important. The restoration of TGF and decrease of intraglomerular pressure with SGLT2 inhibitors protect podocyte integrity and function and reduce excretion of proteinuria.[32] Clinical evidence in patients with SGLT2 inhibition supports this notion that these agents exert structural benefits on glomerular health.[33] Furthermore, hyperreabsorption and activated TGF also contribute to heavy energy consumption and hypoxia in kidney. Renal hemodynamic effects with SGLT2 inhibition mitigate tubular workload and improve renal cortical oxygenation, thus protecting tubular epithelial cells from injuries.
Reduced inflammation
Chronic inflammation is a significant factor accounting for initiation and progression of renal dysfunction. Macrophages are considered as the primary immune cells mediating inflammatory process, which are mainly consist of two subsets: pro-inflammatory M1 subset and anti-inflammatory M2 subset. They will differentiate into M1 phenotype and be recruited into injured kidney under hyperglycaemic condition. There is mounting evidence indicating that SGLT2 inhibitors function to decrease the cellular inflammation responses through limiting activation of macrophages and releases of inflammatory markers. Data from a randomized controlled trial in people with T2DM shows empagliflozin switches circulating monocytes to M2 phenotype and leads to a decline in systemic inflammatory granulocyte burden.[34] A downregulation in inflammatory and fibrotic biomarkers, including TNF receptor 1 (TNFR1), IL-6, matrix metalloproteinase 7 (MMP7) and fibronectin 1 (FN1), is also observed in a study with a clinically relevant concentration of canagliflozin, while another anti-diabetic drug glimepiride fails to reduce these molecules.[35] This finding is consistent with a recent human clinical trial with empagliflozin. Compared to sulfonylurea, this agent induces a greater reduction in pyrin domain-containing 3 (NLRP3) inflammasome and IL-1β secretion in macrophages, secondary to decreased levels of serum insulin, glucose, as well as increased serum β-hydroxybutyrate (BHB).[36, 37] With the development of co-culture technology, more and more studies are designed to explore the communication between parenchymal kidney cells and circulating pro-inflammatory cells. A recent study reveals that injured tubular epithelial cells (TECs) could communicate with inflammatory cells and facilitate macrophages polarization through releasing exosomes, leading to exacerbated renal injuries.[38] Nevertheless, improved TECs function with SGLT2 inhibitors may prevent this vicious circle, providing a new insight into reduced level of inflammation induced by these drugs. kidney is widely known as a heterogeneous organ containing various cells. Further researches are needed to elucidate the sophisticated crosstalk among other cell types including mesangial cells, endothelial cells and podocytes during DKD.
Besides these molecules above, high level of plasma uric acid is also related to inflammatory process in DKD progression. Recently, in an analysis of randomized clinical trials, enhanced uric acid excretion and reduced circulating uric acid are observed with dapagliflozin, which are strongly associated with increased urinary glucose excretion.[39] Restored uric acid level is proved to contribute to mitigated inflammation.[40] In addition, SGLT2 inhibitors have been reported to decrease kidney injury molecule-1 (KIM-1) previously, one of proximal biomarkers in diseases regarding kidney injury.[41] Lately, an interesting study in mice with KIM-1 mucin domain mutant shows that KIM-1 contributes to tubulointerstitial inflammation by mediating proximal tubule cells uptake of fatty acid (FA)-bound albumin.[42] Further study is required to illustrate whether renal anti-inflammatory benefits with SGLT2 inhibitors are associated with suppression of KIM-1.
Nutrient deprivation signaling
Besides the mechanisms described above, emerging studies offer further insights into metabolic alterations and energy homeostasis after SGLT2 inhibitors treatment. Aberrant glycolysis and impaired fatty acid oxidation (FAO) followed by remarkable lipid accumulation in kidney are observed in people and mice in the context of diabetes, a state of energy overabundance.[43] Excitingly, dapagliflozin and ipragliflozin have the potential to suppress this abnormal metabolic state, through increasing the level of key enzyme carnitine palmitoyl-transferase-1α (CPT1α) associated with FAO and decreasing accumulation of tricarboxylic acid (TCA) cycle metabolites.[44] In addition, people and animals with SGLT2 inhibitors manifest a consistent reduction in body weight, which is thought to result from enhanced urinary glucose excretion and calorie loss. Hence, there is a novel hypothesis that these agents have the potential to switch perceived nutrient overabundance to an energy-preserving state, reminiscent of a state occurring in hibernating animals.[45] In a randomized, double-blind trial, five weeks treatment with dapagliflozin results in improved systemic energy metabolism and increased lipolysis and ketogenesis.[46] The improvement in extracellular lipidome secondary to restored FAO is also observed in db/db mice and Zucker diabetic fatty rats through non-targeted and targeted metabolome technologies.[47, 48] Studies in diabetic mouse models have further shown SGLT2 inhibitors contribute to increased circulating ketone bodies by modulation of rate-limiting enzyme for ketogenesis in various organs.[49] Ketogenesis in the context of SGLT2 inhibitors is thought to be a result of activation of low-energy sensors including 5′ AMP–activated protein kinase (AMPK) and sirtuin-1 (SIRT1), along with the upregulation of hypoxia-inducible factor (HIF)-2α. Ketone is used to be considered as a preferred energy source for injured proximal tubular epithelial cells (PTECs), leading to efficient energy utilization in kidney.[50] Of interest, it is also observed to act as a signal mediator of fasting and induce inhibition of mechanistic target of rapamycin (mTOR) recently. Inhibition of mTOR complex1 has been found to have effects on reducing renal fibrogenesis, mediating the beneficial effects of SGLT2 inhibitors.[51,52,53] In addition to elevated ketone bodies, reduced branched-chain amino acids transport is also responsible for fasting-like transcriptional paradigm. Changes in key nutrient-sensing pathways facilitate adaption to a low-energy state, with inhibition of energy storage and promotion of energy utilization, ultimately protect the kidney.[54] It should be mentioned that most findings presented herein are based on studies performed in animal models. Well-designed studies will be required urgently to determine the hypothesis and gather further evidence from human studies.
Interestingly, coordinated activation of SIRT1 and AMPK, as well as downregulation of mTOR stimulate autophagy in the setting of SGLT2 inhibitors, leading to clearance of dysfunctional mitochondria and peroxisomes. This reduces major sources of reactive oxygen species (ROS), thus mitigating oxidative stress in kidney.[55, 56] Of note, hyperactive autophagy as well as insufficient autophagy are both considered to be harmful. Reduction of autophagy activity by SGLT2 inhibitors was found recently to protect myocardial cell from death during ischemia-reperfusion injury. It is in contradiction with previous studies in kidney. The exact mechanism by which SGLT2 inhibition optimizes autophagy process in different contexts remains to be illuminated.
Improved endothelial function
Vascular stiffness, endothelial dysfunction and secondary glomerulosclerosis under hyperglycemic condition, as we all know, are critically linked to pathogenesis of DKD.[57] Reduced inflammation and mitochondria dysfunction mentioned above by SGLT2 inhibitors have been proved to involve in the mitigation of endothelial dysfunction. In a mechanistic study, inhibition with SGLT2 ameliorates renal endothelial rarefaction which often contributes to secondary glomerulosclerosis, through restoring level of vascular endothelial growth factor (VEGF)-A.[58] In addition, oxidative stress in the context of diabetes plays an important role in endothelial injuries. A recent study in human cardiac myocytes provides a novel translational link between the dual SGLT2 inhibitor canagliflozin and oxidative stress regulation. Canagliflozin exerts remarkable anti-oxidative effects through a SGLT1 dependent mechanism, resulting in inhibition of NADPH oxidase activity and improvement of nitric oxide synthases function.[59] Interestingly, reduced ROS production with empagliflozin is also observed in human endothelial cells, which is attributed to inhibition on NHE1.[60] Of note, increased the level of circulating pro-vascular cells in the context of SGLT2 inhibitors is also thought to be related to improved endothelial repair.[34] Dapagliflozin is observed to have the potential to improve vascular endothelial healing in diabetic mice, at least in part by recruitment of bone marrow derived hematopoietic cells.[61] Recently, data from human and rodent cells shows canagliflozin inhibits excessive replication and migration of vascular smooth muscle cells (SMCs), as well as mitigates endothelial inflammation, resulting in blunting atherosclerosis and glomerulosclerosis.[62] Regretfully, the exact molecule mechanisms have not been determined. Going forward, it will be important to examine further the dedicated mechanisms of SGLT2 inhibitors on vascular endothelial benefits.
Apart from mechanisms mentioned, suppression of AGE-RAGE signaling, increased hematocrit, provide additional support to improved kidney outcomes by these drugs.[63,64,65] Taken together, SGLT2 inhibitors should be considered as a predominant clinical therapy after metformin in most people with DKD as a consequence of organ protective effects.
Conclusions
Traditional studies in the past have shown that glomerular lesions play a pivotal role in development of DKD, while recent findings indicate tubular damage may precede lesions in podocytes in early DKD. This observation makes the tubular hypothesis popular.[66] As a class of drugs directly targeting tubular function in kidney, SGLT2 inhibitors receive great notice. Furthermore, consistent beneficial renal results from recent clinical trials contribute to considerable attention to clinical application of SGLT2 inhibitors in people with diabetes and chronic kidney disease.[67] Emerging studies are designed to explore reno-protective effects with SGLT2 inhibition in people with T1DM, and even without diabetes. Currently, another large clinical study, the EMPA-KIDNEY trial, will provide extra evidence about renal benefits of SGLT2 inhibitors in the context of T1DM.[68] Of interest, many extrarenal effects with these agents also come into notice. In a randomized controlled trial, empagliflozin is associated with improved hypothalamus functions and cognition which indicates a promising approach to treat diabetes-related brain diseases.[69] Significant changes in gut microbiota are also observed with dapagliflozin, suggesting pleiotropic effects of SGLT2 inhibition.[70] Furthermore, it is noteworthy that increased risk of diabetic ketoacidosis (DKA), an off-target adverse effect of these drugs, has been reported in some randomized controlled trials.[71, 72] Although the risk of DKA is rather low, it is necessary to pay attention to monitoring the level of ketones when doctors consider these agents for their patients.[73] Timely recognition and appropriate management are also of great significance when patients present with vague symptoms. In addition, compared to monotherapy, combination therapies with SGLT2 inhibitors and other anti-diabetic drugs are preferred in clinical practice. Internists are supposed to be careful of the increased risk of hypoglycaemia in the setting of combination treatment. In conclusion, SGLT2 inhibitors would be a promising option for the treatment of DKD.
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R, Committee IDFDA (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 157:107843. doi: https://doi.org/10.1016/j.diabres.2019.107843
Disease GBD, Injury I, Prevalence C (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1545–1602. doi: https://doi.org/10.1016/S0140-6736(16)31678-6
Lytvyn Y, Bjornstad P, van Raalte DH, Heerspink HL, Cherney DZI (2020) The New Biology of Diabetic Kidney Disease-Mechanisms and Therapeutic Implications. Endocr Rev 41. doi: https://doi.org/10.1210/endrev/bnz010
Khunti K (2021) SGLT2 inhibitors in people with and without T2DM. Nat Rev Endocrinol 17:75–76. doi: https://doi.org/10.1038/s41574-020-00453-2
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE, Investigators E-RO (2015) Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 373:2117–2128. doi: https://doi.org/10.1056/NEJMoa1504720
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR, Group CPC (2017) Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med 377:644–657. doi: https://doi.org/10.1056/NEJMoa1611925
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS, Investigators D-T (2019) Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 380:347–357. doi: https://doi.org/10.1056/NEJMoa1812389
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW, Investigators CT (2019) Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med 380:2295–2306. doi: https://doi.org/10.1056/NEJMoa1811744
Vallon V, Verma S (2021) Effects of SGLT2 Inhibitors on Kidney and Cardiovascular Function. Annu Rev Physiol 83:503–528. doi: https://doi.org/10.1146/annurev-physiol-031620-095920
Zhang J, Wei J, Jiang S, Xu L, Wang L, Cheng F, Buggs J, Koepsell H, Vallon V, Liu R (2019) Macula Densa SGLT1-NOS1-Tubuloglomerular Feedback Pathway, a New Mechanism for Glomerular Hyperfiltration during Hyperglycemia. J Am Soc Nephrol 30:578–593. doi: https://doi.org/10.1681/ASN.2018080844
Wilcox CS (2020) Antihypertensive and Renal Mechanisms of SGLT2 (Sodium-Glucose Linked Transporter 2) Inhibitors. Hypertension 75:894–901. doi: https://doi.org/10.1161/HYPERTENSIONAHA.119.11684
Cowie MR, Fisher M (2020) SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol 17:761–772. doi: https://doi.org/10.1038/s41569-020-0406-8
DeFronzo RA, Reeves WB, Awad AS (2021) Pathophysiology of diabetic kidney disease: impact of SGLT2 inhibitors. Nat Rev Nephrol 17:319–334. doi: https://doi.org/10.1038/s41581-021-00393-8
Kim JH, Ko HY, Wang HJ, Lee H, Yun M, Kang ES (2020) Effect of dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on gluconeogenesis in proximal renal tubules. Diabetes Obes Metab 22:373–382. doi: https://doi.org/10.1111/dom.13905
Solis-Herrera C, Daniele G, Alatrach M, Agyin C, Triplitt C, Adams J, Patel R, Gastaldelli A, Honka H, Chen X, Abdul-Ghani M, Cersosimo E, Del Prato S, DeFronzo R (2020) Increase in Endogenous Glucose Production With SGLT2 Inhibition Is Unchanged by Renal Denervation and Correlates Strongly With the Increase in Urinary Glucose Excretion. Diabetes Care 43:1065–1069. doi: https://doi.org/10.2337/dc19-2177
Alatrach M, Agyin C, Solis-Herrera C, Lavryneko O, Adams J, Gastaldelli A, Triplitt C, DeFronzo RA, Cersosimo E (2022) Dapagliflozin Impairs the Suppression of Endogenous Glucose Production in Type 2 Diabetes Following Oral Glucose. Diabetes Care. doi: https://doi.org/10.2337/dc21-1798
Li C, Luo J, Jiang M, Wang K (2022) The Efficacy and Safety of the Combination Therapy With GLP-1 Receptor Agonists and SGLT-2 Inhibitors in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis. Front Pharmacol 13:838277. doi: https://doi.org/10.3389/fphar.2022.838277
Ko EJ, Shin YJ, Cui S, Lim SW, Chung BH, Yang CW (2022) Effect of dual inhibition of DPP4 and SGLT2 on tacrolimus-induced diabetes mellitus and nephrotoxicity in a rat model. Am J Transplant. doi: https://doi.org/10.1111/ajt.17035
Storgaard H, Gluud LL, Bennett C, Grondahl MF, Christensen MB, Knop FK, Vilsboll T (2016) Benefits and Harms of Sodium-Glucose Co-Transporter 2 Inhibitors in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. PLoS ONE 11:e0166125. doi: https://doi.org/10.1371/journal.pone.0166125
Ostergaard MV, Secher T, Christensen M, Salinas CG, Roostalu U, Skytte JL, Rune I, Hansen HH, Jelsing J, Vrang N, Fink LN (2021) Therapeutic effects of lisinopril and empagliflozin in a mouse model of hypertension-accelerated diabetic kidney disease. Am J Physiol Renal Physiol 321:F149–F161. doi: https://doi.org/10.1152/ajprenal.00154.2021
Tian B, Deng Y, Cai Y, Han M, Xu G (2022) Efficacy and safety of combination therapy with sodium-glucose cotransporter 2 inhibitors and renin-angiotensin system blockers in patients with type 2 diabetes: a systematic review and meta-analysis. Nephrol Dial Transplant 37:720–729. doi: https://doi.org/10.1093/ndt/gfab048
Ishizawa K, Wang Q, Li J, Xu N, Nemoto Y, Morimoto C, Fujii W, Tamura Y, Fujigaki Y, Tsukamoto K, Fujita T, Uchida S, Shibata S (2019) Inhibition of Sodium Glucose Cotransporter 2 Attenuates the Dysregulation of Kelch-Like 3 and NaCl Cotransporter in Obese Diabetic Mice. J Am Soc Nephrol 30:782–794. doi: https://doi.org/10.1681/ASN.2018070703
Thomson SC, Vallon V (2019) Renal Effects of Sodium-Glucose Co-Transporter Inhibitors. Am J Cardiol 124(Suppl 1):S28–S35. doi: https://doi.org/10.1016/j.amjcard.2019.10.027
Li XC, Zhu D, Chen X, Zheng X, Zhao C, Zhang J, Soleimani M, Rubera I, Tauc M, Zhou X, Zhuo JL (2019) Proximal Tubule-Specific Deletion of the NHE3 (Na(+)/H(+) Exchanger 3) in the Kidney Attenuates Ang II (Angiotensin II)-Induced Hypertension in Mice. Hypertension 74:526–535. doi: https://doi.org/10.1161/HYPERTENSIONAHA.119.13094
Li XC, Soleimani M, Zhu D, Rubera I, Tauc M, Zheng X, Zhang J, Chen X, Zhuo JL (2018) Proximal Tubule-Specific Deletion of the NHE3 (Na(+)/H(+) Exchanger 3) Promotes the Pressure-Natriuresis Response and Lowers Blood Pressure in Mice. Hypertension 72:1328–1336. doi: https://doi.org/10.1161/HYPERTENSIONAHA.118.10884
Borges-Junior FA, Silva Dos Santos D, Benetti A, Polidoro JZ, Wisnivesky ACT, Crajoinas RO, Antonio EL, Jensen L, Caramelli B, Malnic G, Tucci PJ, Girardi ACC (2021) Empagliflozin Inhibits Proximal Tubule NHE3 Activity, Preserves GFR, and Restores Euvolemia in Nondiabetic Rats with Induced Heart Failure. J Am Soc Nephrol. doi: https://doi.org/10.1681/ASN.2020071029
Jiang K, Xu Y, Wang D, Chen F, Tu Z, Qian J, Xu S, Xu Y, Hwa J, Li J, Shang H, Xiang Y (2022) Cardioprotective mechanism of SGLT2 inhibitor against myocardial infarction is through reduction of autosis. Protein Cell 13:336–359. doi: https://doi.org/10.1007/s13238-020-00809-4
Ellison DH (2021) SGLT2 inhibitors, hemodynamics, and kidney protection. Am J Physiol Renal Physiol 321:F47–F49. doi: https://doi.org/10.1152/ajprenal.00092.2021
van Bommel EJM, Lytvyn Y, Perkins BA, Soleymanlou N, Fagan NM, Koitka-Weber A, Joles JA, Cherney DZI, van Raalte DH (2020) Renal hemodynamic effects of sodium-glucose cotransporter 2 inhibitors in hyperfiltering people with type 1 diabetes and people with type 2 diabetes and normal kidney function. Kidney Int 97:631–635. doi: https://doi.org/10.1016/j.kint.2019.12.021
Kidokoro K, Cherney DZI, Bozovic A, Nagasu H, Satoh M, Kanda E, Sasaki T, Kashihara N (2019) Evaluation of Glomerular Hemodynamic Function by Empagliflozin in Diabetic Mice Using. Vivo Imaging Circulation 140:303–315. doi: https://doi.org/10.1161/CIRCULATIONAHA.118.037418
van Bommel EJM, Muskiet MHA, van Baar MJB, Tonneijck L, Smits MM, Emanuel AL, Bozovic A, Danser AHJ, Geurts F, Hoorn EJ, Touw DJ, Larsen EL, Poulsen HE, Kramer MHH, Nieuwdorp M, Joles JA, van Raalte DH (2020) The renal hemodynamic effects of the SGLT2 inhibitor dapagliflozin are caused by post-glomerular vasodilatation rather than pre-glomerular vasoconstriction in metformin-treated patients with type 2 diabetes in the randomized, double-blind RED trial. Kidney Int 97:202–212. doi: https://doi.org/10.1016/j.kint.2019.09.013
Hudkins KL, Li X, Holland AL, Swaminathan S, Alpers CE (2022) Regression of diabetic nephropathy by treatment with empagliflozin in BTBR ob/ob mice. Nephrol Dial Transplant 37:847–859. doi: https://doi.org/10.1093/ndt/gfab330
Durcan E, Ozkan S, Saygi HI, Dincer MT, Korkmaz OP, Sahin S, Karaca C, Sulu C, Bakir A, Ozkaya HM, Trabulus S, Guzel E, Seyahi N, Gonen MS (2022) Effects of SGLT2 inhibitors on patients with diabetic kidney disease: A preliminary study on the basis of podocyturia. J Diabetes 14:236–246. doi: https://doi.org/10.1111/1753-0407.13261
Hess DA, Terenzi DC, Trac JZ, Quan A, Mason T, Al-Omran M, Bhatt DL, Dhingra N, Rotstein OD, Leiter LA, Zinman B, Sabongui S, Yan AT, Teoh H, Mazer CD, Connelly KA, Verma S (2019) SGLT2 Inhibition with Empagliflozin Increases Circulating Provascular Progenitor Cells in People with Type 2 Diabetes Mellitus. Cell Metab 30:609–613. doi: https://doi.org/10.1016/j.cmet.2019.08.015
Heerspink HJL, Perco P, Mulder S, Leierer J, Hansen MK, Heinzel A, Mayer G (2019) Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia 62:1154–1166. doi: https://doi.org/10.1007/s00125-019-4859-4
Kim SR, Lee SG, Kim SH, Kim JH, Choi E, Cho W, Rim JH, Hwang I, Lee CJ, Lee M, Oh CM, Jeon JY, Gee HY, Kim JH, Lee BW, Kang ES, Cha BS, Lee MS, Yu JW, Cho JW, Kim JS, Lee YH (2020) SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat Commun 11:2127. doi: https://doi.org/10.1038/s41467-020-15983-6
Lei Y, Devarapu SK, Motrapu M, Cohen CD, Lindenmeyer MT, Moll S, Kumar SV, Anders HJ (2019) Interleukin-1beta Inhibition for Chronic Kidney Disease in Obese Mice With Type 2 Diabetes. Front Immunol 10:1223. doi: https://doi.org/10.3389/fimmu.2019.01223
Lv LL, Feng Y, Wu M, Wang B, Li ZL, Zhong X, Wu WJ, Chen J, Ni HF, Tang TT, Tang RN, Lan HY, Liu BC (2020) Exosomal miRNA-19b-3p of tubular epithelial cells promotes M1 macrophage activation in kidney injury. Cell Death Differ 27:210–226. doi: https://doi.org/10.1038/s41418-019-0349-y
Suijk DLS, van Baar MJB, van Bommel EJM, Iqbal Z, Krebber MM, Vallon V, Touw D, Hoorn EJ, Nieuwdorp M, Kramer MMH, Joles JA, Bjornstad P, van Raalte DH (2022) SGLT2 Inhibition and Uric Acid Excretion in Patients with Type 2 Diabetes and Normal Kidney Function. Clin J Am Soc Nephrol 17:663–671. doi: https://doi.org/10.2215/CJN.11480821
La Grotta R, de Candia P, Olivieri F, Matacchione G, Giuliani A, Rippo MR, Tagliabue E, Mancino M, Rispoli F, Ferroni S, Berra CC, Ceriello A, Prattichizzo F (2022) Anti-inflammatory effect of SGLT-2 inhibitors via uric acid and insulin. Cell Mol Life Sci 79:273. doi: https://doi.org/10.1007/s00018-022-04289-z
Oraby MA, El-Yamany MF, Safar MM, Assaf N, Ghoneim HA (2019) Dapagliflozin attenuates early markers of diabetic nephropathy in fructose-streptozotocin-induced diabetes in rats. Biomed Pharmacother 109:910–920. doi: https://doi.org/10.1016/j.biopha.2018.10.100
Mori Y, Ajay AK, Chang JH, Mou S, Zhao H, Kishi S, Li J, Brooks CR, Xiao S, Woo HM, Sabbisetti VS, Palmer SC, Galichon P, Li L, Henderson JM, Kuchroo VK, Hawkins J, Ichimura T, Bonventre JV (2021) KIM-1 mediates fatty acid uptake by renal tubular cells to promote progressive diabetic kidney disease. Cell Metab 33:1042–1061e7. doi: https://doi.org/10.1016/j.cmet.2021.04.004
Cai T, Ke Q, Fang Y, Wen P, Chen H, Yuan Q, Luo J, Zhang Y, Sun Q, Lv Y, Zen K, Jiang L, Zhou Y, Yang J (2020) Sodium-glucose cotransporter 2 inhibition suppresses HIF-1alpha-mediated metabolic switch from lipid oxidation to glycolysis in kidney tubule cells of diabetic mice. Cell Death Dis 11:390. doi: https://doi.org/10.1038/s41419-020-2544-7
Tanaka S, Sugiura Y, Saito H, Sugahara M, Higashijima Y, Yamaguchi J, Inagi R, Suematsu M, Nangaku M, Tanaka T (2018) Sodium-glucose cotransporter 2 inhibition normalizes glucose metabolism and suppresses oxidative stress in the kidneys of diabetic mice. Kidney Int 94:912–925. doi: https://doi.org/10.1016/j.kint.2018.04.025
Avogaro A, Fadini GP, Del Prato S (2020) Reinterpreting Cardiorenal Protection of Renal Sodium-Glucose Cotransporter 2 Inhibitors via Cellular Life History Programming. Diabetes Care 43:501–507. doi: https://doi.org/10.2337/dc19-1410
Op den Kamp YJM, de Ligt M, Dautzenberg B, Kornips E, Esterline R, Hesselink MKC, Hoeks J, Schrauwen-Hinderling VB, Havekes B, Oscarsson J, Phielix E, Schrauwen P (2021) Effects of the SGLT2 Inhibitor Dapagliflozin on Energy Metabolism in Patients With Type 2 Diabetes: A Randomized, Double-Blind Crossover Trial. Diabetes Care 44:1334–1343. doi: https://doi.org/10.2337/dc20-2887
Bamba R, Okamura T, Hashimoto Y, Majima S, Senmaru T, Ushigome E, Nakanishi N, Asano M, Yamazaki M, Takakuwa H, Hamaguchi M, Fukui M (2022) Extracellular lipidome change by an SGLT2 inhibitor, luseogliflozin, contributes to prevent skeletal muscle atrophy in db/db mice. J Cachexia Sarcopenia Muscle 13:574–588. doi: https://doi.org/10.1002/jcsm.12814
Aragon-Herrera A, Otero-Santiago M, Anido-Varela L, Morana-Fernandez S, Campos-Toimil M, Garcia-Caballero T, Barral L, Tarazon E, Rosello-Lleti E, Portoles M, Gualillo O, Moscoso I, Lage R, Gonzalez-Juanatey JR, Feijoo-Bandin S, Lago F (2022) The Treatment With the SGLT2 Inhibitor Empagliflozin Modifies the Hepatic Metabolome of Male Zucker Diabetic Fatty Rats Towards a Protective Profile. Front Pharmacol 13:827033. doi: https://doi.org/10.3389/fphar.2022.827033
Kim JH, Lee M, Kim SH, Kim SR, Lee BW, Kang ES, Cha BS, Cho JW, Lee YH (2019) Sodium-glucose cotransporter 2 inhibitors regulate ketone body metabolism via inter-organ crosstalk. Diabetes Obes Metab 21:801–811. doi: https://doi.org/10.1111/dom.13577
Marton A, Kaneko T, Kovalik JP, Yasui A, Nishiyama A, Kitada K, Titze J (2021) Organ protection by SGLT2 inhibitors: role of metabolic energy and water conservation. Nat Rev Nephrol 17:65–77. doi: https://doi.org/10.1038/s41581-020-00350-x
Tomita I, Kume S, Sugahara S, Osawa N, Yamahara K, Yasuda-Yamahara M, Takeda N, Chin-Kanasaki M, Kaneko T, Mayoux E, Mark M, Yanagita M, Ogita H, Araki SI, Maegawa H (2020) SGLT2 Inhibition Mediates Protection from Diabetic Kidney Disease by Promoting Ketone Body-Induced mTORC1 Inhibition. Cell Metab 32:404–419e6. doi: https://doi.org/10.1016/j.cmet.2020.06.020
Packer M (2020) SGLT2 Inhibitors Produce Cardiorenal Benefits by Promoting Adaptive Cellular Reprogramming to Induce a State of Fasting Mimicry: A Paradigm Shift in Understanding Their Mechanism of Action. Diabetes Care 43:508–511. doi: https://doi.org/10.2337/dci19-0074
Kogot-Levin A, Hinden L, Riahi Y, Israeli T, Tirosh B, Cerasi E, Mizrachi EB, Tam J, Mosenzon O, Leibowitz G (2020) Proximal Tubule mTORC1 Is a Central Player in the Pathophysiology of Diabetic Nephropathy and Its Correction by SGLT2 Inhibitors. Cell Rep 32:107954. doi: https://doi.org/10.1016/j.celrep.2020.107954
Packer M (2020) Role of Impaired Nutrient and Oxygen Deprivation Signaling and Deficient Autophagic Flux in Diabetic CKD Development: Implications for Understanding the Effects of Sodium-Glucose Cotransporter 2-Inhibitors. J Am Soc Nephrol 31:907–919. doi: https://doi.org/10.1681/ASN.2020010010
Saxena S, Mathur A, Kakkar P (2019) Critical role of mitochondrial dysfunction and impaired mitophagy in diabetic nephropathy. J Cell Physiol 234:19223–19236. doi: https://doi.org/10.1002/jcp.28712
Packer M (2020) Autophagy stimulation and intracellular sodium reduction as mediators of the cardioprotective effect of sodium-glucose cotransporter 2 inhibitors. Eur J Heart Fail 22:618–628. doi: https://doi.org/10.1002/ejhf.1732
Ugusman A, Kumar J, Aminuddin A (2021) Endothelial function and dysfunction: Impact of sodium-glucose cotransporter 2 inhibitors. Pharmacol Ther 224:107832. doi: https://doi.org/10.1016/j.pharmthera.2021.107832
Zhang Y, Nakano D, Guan Y, Hitomi H, Uemura A, Masaki T, Kobara H, Sugaya T, Nishiyama A (2018) A sodium-glucose cotransporter 2 inhibitor attenuates renal capillary injury and fibrosis by a vascular endothelial growth factor-dependent pathway after renal injury in mice. Kidney Int 94:524–535. doi: https://doi.org/10.1016/j.kint.2018.05.002
Kondo H, Akoumianakis I, Badi I, Akawi N, Kotanidis CP, Polkinghorne M, Stadiotti I, Sommariva E, Antonopoulos AS, Carena MC, Oikonomou EK, Reus EM, Sayeed R, Krasopoulos G, Srivastava V, Farid S, Chuaiphichai S, Shirodaria C, Channon KM, Casadei B, Antoniades C (2021) Effects of canagliflozin on human myocardial redox signalling: clinical implications. Eur Heart J 42:4947–4960. doi: https://doi.org/10.1093/eurheartj/ehab420
Uthman L, Li X, Baartscheer A, Schumacher CA, Baumgart P, Hermanides J, Preckel B, Hollmann MW, Coronel R, Zuurbier CJ, Weber NC (2022) Empagliflozin reduces oxidative stress through inhibition of the novel inflammation/NHE/[Na(+)]c/ROS-pathway in human endothelial cells. Biomed Pharmacother 146:112515. doi: https://doi.org/10.1016/j.biopha.2021.112515
Albiero M, Tedesco S, Amendolagine FI, D’Anna M, Migliozzi L, Zuccolotto G, Rosato A, Cappellari R, Avogaro A, Fadini GP (2021) Inhibition of SGLT2 Rescues Bone Marrow Cell Traffic for Vascular Repair: Role of Glucose Control and Ketogenesis. Diabetes 70:1767–1779. doi: https://doi.org/10.2337/db20-1045
Behnammanesh G, Durante GL, Khanna YP, Peyton KJ, Durante W (2020) Canagliflozin inhibits vascular smooth muscle cell proliferation and migration: Role of heme oxygenase-1. Redox Biol 32:101527. doi: https://doi.org/10.1016/j.redox.2020.101527
Li J, Neal B, Perkovic V, de Zeeuw D, Neuen BL, Arnott C, Simpson R, Oh R, Mahaffey KW, Heerspink HJL (2020) Mediators of the effects of canagliflozin on kidney protection in patients with type 2 diabetes. Kidney Int 98:769–777. doi: https://doi.org/10.1016/j.kint.2020.04.051
Hesp AC, Schaub JA, Prasad PV, Vallon V, Laverman GD, Bjornstad P, van Raalte DH (2020) The role of renal hypoxia in the pathogenesis of diabetic kidney disease: a promising target for newer renoprotective agents including SGLT2 inhibitors? Kidney Int 98:579–589. doi: https://doi.org/10.1016/j.kint.2020.02.041
Shao Q, Meng L, Lee S, Tse G, Gong M, Zhang Z, Zhao J, Zhao Y, Li G, Liu T (2019) Empagliflozin, a sodium glucose co-transporter-2 inhibitor, alleviates atrial remodeling and improves mitochondrial function in high-fat diet/streptozotocin-induced diabetic rats. Cardiovasc Diabetol 18:165. doi: https://doi.org/10.1186/s12933-019-0964-4
Vallon V, Thomson SC (2020) The tubular hypothesis of nephron filtration and diabetic kidney disease. Nat Rev Nephrol 16:317–336. doi: https://doi.org/10.1038/s41581-020-0256-y
Alicic RZ, Neumiller JJ, Johnson EJ, Dieter B, Tuttle KR (2019) Sodium-Glucose Cotransporter 2 Inhibition and Diabetic Kidney Disease. Diabetes 68:248–257. doi: https://doi.org/10.2337/dbi18-0007
Rhee JJ, Jardine MJ, Chertow GM, Mahaffey KW (2020) Dedicated kidney disease-focused outcome trials with sodium-glucose cotransporter-2 inhibitors: Lessons from CREDENCE and expectations from DAPA-HF, DAPA-CKD, and EMPA-KIDNEY. Diabetes Obes Metab 22(Suppl 1):46–54. doi: https://doi.org/10.1111/dom.13987
Kullmann S, Hummel J, Wagner R, Dannecker C, Vosseler A, Fritsche L, Veit R, Kantartzis K, Machann J, Birkenfeld AL, Stefan N, Haring HU, Peter A, Preissl H, Fritsche A, Heni M (2022) Empagliflozin Improves Insulin Sensitivity of the Hypothalamus in Humans With Prediabetes: A Randomized, Double-Blind, Placebo-Controlled, Phase 2 Trial. Diabetes Care 45:398–406. doi: https://doi.org/10.2337/dc21-1136
Yang M, Shi FH, Liu W, Zhang MC, Feng RL, Qian C, Liu W, Ma J (2020) Dapagliflozin Modulates the Fecal Microbiota in a Type 2 Diabetic Rat Model. Front Endocrinol (Lausanne) 11:635. doi: https://doi.org/10.3389/fendo.2020.00635
Hampp C, Swain RS, Horgan C, Dee E, Qiang Y, Dutcher SK, Petrone A, Chen Tilney R, Maro JC, Panozzo CA (2020) Use of Sodium-Glucose Cotransporter 2 Inhibitors in Patients With Type 1 Diabetes and Rates of Diabetic Ketoacidosis. Diabetes Care 43:90–97. doi: https://doi.org/10.2337/dc19-1481
Griffin TP, Dinneen SF (2020) SGLT2 inhibitors increase risk for diabetic ketoacidosis in type 2 diabetes. Ann Intern Med 173:JC40. doi: https://doi.org/10.7326/ACPJ202010200-040
Musso G, Saba F, Cassader M, Gambino R (2020) Diabetic ketoacidosis with SGLT2 inhibitors. BMJ 371:m4147. doi: https://doi.org/10.1136/bmj.m4147
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 81,974,110, 81,770,812].
Author information
Authors and Affiliations
Contributions
All authors contributed to this work and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare. This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gan, T., Song, Y., Guo, F. et al. Emerging roles of Sodium-glucose cotransporter 2 inhibitors in Diabetic kidney disease. Mol Biol Rep 49, 10915–10924 (2022). https://doi.org/10.1007/s11033-022-07758-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07758-7