Abstract
Purpose
Marfan syndrome (MFS) is a genetic disease often marked by the presence of scoliosis. There is no three-dimensional analysis of the deformity in the literature. Our aim was to determine what kind of sagittal balance defines scoliosis associated with MFS, namely a flexion deformity, as it is in scoliosis associated with Chiari I or an extension deformity, as in adolescent idiopathic scoliosis (AIS). To address this issue, we compared the presence or absence of a thoracic scoliosis with the presence or absence of a segment in extension in the thoracic spine.
Methods
In our series, 30 patients diagnosed with Marfan syndrome were prospectively included. In each patient, personalized three-dimensional reconstruction from T1 to L5 of the spine was made using stereoradiography. The patients were first separated based on the presence or absence of thoracic scoliosis, in order to compare this with the presence or absence of a segment in extension in the thoracic spine. They were then classified into two groups based on the presence or absence of the segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine.
Results
Among scoliotic patients with a thoracic scoliosis (17 cases), there were 13 (76.5% cases) with a segment in extension in the thoracic spine and 4 with no segment in extension.
Conclusions
Our results showed that scoliosis associated with MFS is somehow original, demonstrating a sagittal balance in extension (as AIS) in about 80% of thoracic curves, but without this characteristic feature in about 20%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Marfan syndrome (MFS) is a genetic disease with autosomal dominant inheritance [1] and is often marked by the presence of scoliosis [2–4]. Surprisingly, the scoliosis associated with this syndrome is very poorly described in the literature. There is no three-dimensional (3D) assessment of the deformity. The natural history of scoliosis associated with MFS is, however, known to be quite different from that of adolescent idiopathic scoliosis (AIS), with or without surgery [5–7].
In order to have a better understanding of scoliosis associated with MFS, our aim was to perform a 3D analysis of the deformity using a specific tool based on stereoradiography [8] and to determine whether the sagittal balance at the apex of scoliosis associated with MFS is in extension—as in AIS [9]—or in flexion—as in Chiari I [10, 11]. A sagittal balance in extension at the apex of the deformity would indicate that the mechanical model of column buckling is adapted to scoliosis associated with MFS. A sagittal balance in flexion would indicate that the column buckling model is not responsible for the deformity.
Materials and methods
Data collection
The series was prospective. The period of inclusion was between August 2004 and August 2006. This work has been approved by the ethics committee related to our institution. Each patient attending our institution (at the clinic of orthopedic surgery, pediatric orthopedic surgery, ophthalmology, heart surgery, vascular surgery, cardiology and genetics) was considered for inclusion. The criterion for inclusion was a diagnosis of MFS made according to the Ghent criteria [12]. Criteria for exclusion were age under 4 years, a standard radiographic examination of the spine made less than 1 year before, a pregnancy or suspicion of pregnancy in women, and patient’s refusal (or parental refusal in minor patients) to be included in the study. A total of 55 patients were considered as being possibly affected with MFS. Fourteen patients refused to be included in the series (in 12 cases, they had moved far from the area of our institution, and in 2 cases, they did not want to hear about their disease for some psychological reasons). Three eligible patients were deceased. Thirty-eight patients accepted to be included in the series. Five patients did not meet the criterion for inclusion. Three patients were excluded because of a standard radiographic examination of the spine performed less than 1 year before. No patient has been excluded because of pregnancy or suspicion of pregnancy. Eventually, 30 patients were included in our series. Each patient was proposed to undergo a stereoradiographic examination of the spine (standardized AP and lateral views) as a substitute to the standard radiographic follow-up of the spine.
Three-dimensional reconstruction of the spine
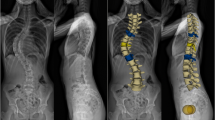
Stereoradiography and personalized 3D reconstruction of the spine from T1 to L5 were made according to the method developed by Pomero et al. [8]. This method relies on the identification of the corners of the projected vertebral plates of the vertebral body on both frontal and lateral radiographs, which can be very easily identified, even in osteoporotic bones. An a priori knowledge of vertebral and spinal 3D geometry (based on a morphological database of normal and scoliotic dry vertebrae, and on a morphological database of in vivo 3D reconstructions performed in 96 healthy and scoliotic subjects using classical methods) was used to generate a model of the spine, which is plotted on the X-ray films for a visual control of the quality of the reconstruction. Then, a supplementary manual “fine tuning” is performed in order to obtain the refined geometric model with the best matching between the projected 3D contours and the corresponding radiograph contours (Fig. 1a–d). In each patient, based on the 3D reconstruction, inter-vertebral rotations (according to SRS definitions [13]) were assessed in the sagittal plane. These rotations were noted in degrees, and the sign of the rotation was chosen arbitrarily. As a convention, a rotation in the sagittal plane “forward”, defining an inter-vertebral flexion was noted as positive, and a rotation in the sagittal plane “backward”, defining an inter-vertebral extension was noted as negative. In each patient, the Cobb angle was measured on the anteroposterior radiograph. A minimum 10° Cobb angle was used to diagnose scoliosis. The apex of each curve was identified according to recommendations by the scoliosis research society (SRS) [13]. The apex could be an inter-vertebral disc or a vertebra [13]. In each patient, a 16-cell table was constructed and filled in with the value of each inter-vertebral sagittal rotation from T1–T2 down to L4–L5.
a Lateral view of the spine. b Postero–anterior (PA) view of the spine. c A supplementary manual “fine tuning” was performed to obtain the refined geometric model with the best matching between the projected 3D contours and the corresponding radiograph contours on PA view. d A supplementary manual “fine tuning” was performed to obtain the refined geometric model with the best matching between the projected 3D contours and the corresponding radiograph contours on lateral view
The patients were first separated based on the presence or absence of thoracic scoliosis [precisely a scoliosis with one (or more) apex at the thoracic level from T4–T5 to T11–T12]. Group Thoracic scoliosis was composed of patients with a thoracic scoliosis and group Non-Thoracic scoliosis was composed of patients without any scoliosis with an apex at the thoracic level from T4–T5 to T11–T12 (meaning patients without any scoliosis, or patients with a scoliosis with an apex cephalad to T4–T5 or caudad to T11–T12).
The patients were then separated into two groups based on the presence or absence of a segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine. Group Extension was composed of patients with a segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12. The second group, named Non-Extension, was composed of patients without any segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12.
Reliability of three-dimensional reconstructions
Three investigators, two physicians and one engineer, performed the 3D-reconstruction procedure on our entire MFS population (30 patients). These three investigators were familiar with the reconstruction software. Inter-vertebral rotation in the sagittal plane of each vertebra was evaluated. To assess the interrater and intrarater reliability, we calculated an intraclass coefficient with 95% confidence interval. Intraclass coefficients greater than 0.91, between 0.71 and 0.91, between 0.51 and 0.70, or less than 0.51 were taken to mean, respectively, very good, good, moderate, or poor agreement [14].
Statistical analysis
The statistical analysis was made using SPSS 13.0 software (SPSS Inc). A four-box grid was constructed to compare the presence or absence of a scoliosis with an apex at the thoracic level from T4–T5 down to T11–T12, with the presence or absence of a segment in extension from T4–T5 down to T11–T12. A Fisher test was used to test the significance of the observed difference.
In the case of a significant difference, a graphic analysis was proposed.
Graphic analysis
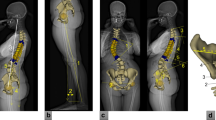
The aim of the graphic analysis was to compare the position of the pathological segment in extension in the sagittal plane with that of the apex. A “mean profile” in non-scoliotic MFS patients was constructed as follows: a 16-cell table was filled in with the mean value of all of the non-scoliotic patients from our study. Each cell (one for each inter-vertebral level, from T1–T2 to L4–L5) was filled in with the mean value of the inter-vertebral rotation in the sagittal plane from all of the non-scoliotic MFS patients in our series. This is graphically represented, showing the inter-vertebral level as abscissa and the inter-vertebral rotation as ordinate using SPSS software (SPSS Inc) (Fig. 2).
For each patient with a scoliosis with an apex at the thoracic level, a second graphic representation (showing the inter-vertebral level as abscissa and the inter-vertebral rotation as ordinate) was superimposed with the “mean non-scoliotic profile” previously described. The apical level(s) is (are) marked with a vertical line in Fig. 3. A visual analysis was performed. The following criteria were checked: Is there a segment of the curve that is located below the “mean non-scoliotic profile” curve: yes/no. If this segment exists, is it centred relatively to the apex: yes/no. If no, the position of the segment in extension was noted as cephalad, or caudad to the apex. In case of double apex curves (at the thoracic level), the previously defined items were checked twice—once for each apex. Additionally, in the case of double apex curves, the sagittal balance of the central segment separating the two pathological segments in extension was noted as flexed, extended, or neutral. The rate of patients with a segment located below the “mean non-scoliotic profile” curve, centred relative to the apex, cephalad to the apex or caudad to the apex was calculated.
Results
Thirty 3D reconstructions of the spine (T1–L5) in patients with MFS were calculated. There were 14 females and 16 males. The mean age was 25.9, ranging from 4 to 65. Of the patients, 11 were under 16 years, 19 were defined as scoliotic (Cobb angle over 10°), and 11 as non-scoliotic (Cobb angle under 10°). There were 6 single curves, 9 double curves and 4 triple curves. Thus, in 19 patients there were 36 curves with a Cobb angle over 10°.
Reliability of three-dimensional reconstructions
The intraclass correlation coefficient showed very good agreement for all of the measurements.
Statistical analysis
There were 17 patients in the group Thoracic Scoliosis, which was composed of patients with a scoliosis with one or more apex at the thoracic level from T4–T5 to T11–T12. In this group, there were 4 single thoracic curves, 9 double curves, and 4 triple curves. There were 13 patients in the group Non-Thoracic Scoliosis, which was composed of patients without any scoliosis with an apex at the thoracic level from T4–T5 to T11–T12. In this group, there were 11 patients without any scoliosis and 2 patients with a single lumbar curve.
Among group Thoracic Scoliosis patients, there were 13 patients (76.5% cases) with a segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12, and 4 patients without any segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12 . Among group Non-Thoracic Scoliosis patients, there were 4 patients (30.8% cases) with a segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12, and 9 patients without any segment in extension (meaning containing negative values of inter-vertebral sagittal rotation) in the thoracic spine from T4–T5 to T11–T12. Using the Fisher test, the rate difference was observed to be significant (P < 0.05).
Graphic analysis
There were 17 patients with one or more apex at the thoracic level. In these patients, 21 curves and 21 apices were defined. A segment below the “mean non-scoliotic profile” curve was noted in 17 curves (81% curves). In 11 curves, it was centred relative to the apex (52% curves). In 5 curves, it was cephalad to the apex (24% curves). In 1 case, it was caudad to the apex (5% curves). In 4 curves, no segment was located below the “mean non-scoliotic profile” (19% cases).
In 4 patients, two apices were observed in the thoracic position. In 3 cases, two different segments located below the “mean non-scoliotic profile” were present, each centred relative to the apices, and separated by a segment in flexion.
Discussion
MFS is a genetic disease with autosomal dominant inheritance [1]. The prevalence of the disease is about 0.01% in the general population [15]. Most of the time, it occurs due to a mutation of the FBN1 gene which codes for an extracellular matrix protein that is called fibrillin [16]. The clinical expression of the disease affects several systems of the body (skeleton, heart and vessels, eyes, skin, dura, and pleura) [1]. One of the most striking symptoms of the disease is scoliosis, which may affect more than 50% patients with MFS [2, 4]. To our knowledge, only three series in the literature have focused on scoliosis associated with MFS [2–4], and none of these included a 3D analysis of the deformity. Since 1980, and the work of Graf et al. [17] and Perdriolle [9], it has been known that adolescent idiopathic scoliosis (AIS) is a 3D complex deformity with pathological extension and axial rotation of vertebrae at the apex of the deformity. This association of both extension and axial rotation is considered by many authors as the hallmark of the column buckling model [18, 19]. Some authors support that relative anterior spinal overgrowth is responsible for the column buckling phenomenon in AIS [20]. This would explain the well-described crankshaft phenomenon seen in AIS, when a posterior fusion is performed in an immature patient [21]. In MFS, it has been shown that long bone overgrowth may be due to changes of elastic fibers in the periosteum [22]. Recently, it has been shown that scoliosis associated with Chiari I, with or without syringomyelia, is marked with the presence of a pathological flexion and axial rotation at the apex of the deformity [10, 23, 24]. Thus, the column buckling model and anterior overgrowth may not be adapted to any kind of scoliosis. Some muscular imbalance may play a major role in non-idiopathic etiologies. It has been shown that scoliosis associated with MFS is unique and does not look like AIS: its natural history is different, often more severe [2], and King’s guidelines used to determine the extension of arthrodesis in AIS [25, 26] do not fit scoliosis associated with MFS [5–7]. Thus, since the genuine curve pattern of scoliosis associated with MFS remains unknown, our aim was to answer the question: what kind of sagittal balance defines scoliosis associated with MFS. Is it a flexion deformity, as in scoliosis associated with Chiari I [10, 23, 24], or is it an extension deformity, as in AIS [9, 17].
The 3D method of reconstruction used in this work has not been validated in MFS patients. Nevertheless, this is the first 3D study to be conducted in such patients, and there is no other study available to compare it with. The method we used, described by Pomero et al. [8], was developed to simplify the classical methods based on the identification of numerous anatomical landmarks per vertebra on both radiographic films [27, 28]. These classical methods are cumbersome because the landmark identification process can be long and tedious. Conversely, the method developed by Pomero et al. [8] does not rely on the identification of anatomical landmarks, but on the identification of the corners of the projected vertebral plates of the vertebral body on both frontal and lateral radiographs. This method is easy to use and has been shown to be as accurate as CT scan 3D reconstructions [8]. We think that this method is universal and feasible under various conditions, including MFS, as long as the vertebral end plates are visible. The methodology used to check the reliability of reconstructions was based on the methodology recently published in AIS [29].
Our work pointed out that there was a segment in extension in 76.5% cases among scoliotic patients with an apex at the thoracic level located between T4–T5 and T11–T12, and the graphic analysis pointed out that a segment below the “mean non-scoliotic profile” curve was noted in 81% of curves. Focusing on the relationship between the apex and the pathological segment in extension (i.e., the segment that is more in extension than the “mean non-scoliotic profile”), we found that it was centred relative to the apex in 52% of curves, cephalad to the apex in 24%, and caudad to the apex in 5%. Conversely, there was no pathological segment in extension (i.e., no segment located below the “mean non-scoliotic profile”) in 19% of curves. These results showed that scoliosis associated with MFS is somehow original, demonstrating a sagittal balance in extension, as with AIS, in about 80% curves, although did not show this characteristic in the remaining 20%. Pathological extension at the apex of the curve is the hallmark in AIS [9, 30, 31]. This feature led some authors to support the column buckling mechanical model as an explanation for the simultaneous extension, lateral deviation, and axial rotation of the vertebrae embedded in a scoliosis [18, 19, 32]. Scoliosis associated with MFS demonstrates this feature in 80% of curves. This result is very different from the conclusion that Sponseller et al. [2] reported from their review of 113 MFS patients. They stated that the back in MFS patients was globally in flexion (with an hyperkyphosis over 50°) in about half of the cases, and that only 8% had a hypokyphosis (a thoracic kyphosis of less than 20°), regardless of the presence of a scoliosis. This gap between our result and the conclusions of Sponseller et al. [2] may come from the methodology used. In the work of Sponseller et al. [2], the sole lateral view of the spine was considered in order to determine the sagittal balance of the spine. Perdriolle [9] showed in his classical experience that the lateral view in scoliotic patients may demonstrate a kyphosis, as the real geometric pattern of the spine is actually a lordosis. Thus, our results may more accurately describe the genuine curve pattern in MFS patients with scoliosis than Sponseller et al. [2] did. The mechanical model of column buckling is well adapted to scoliosis associated with MFS. In order to strengthen this theory, prospective work assessing the anterior vertebral body overgrowth in MFS patients with scoliosis must be done. The clinical relevance of these findings is that a crankshaft phenomenon is theoretically possible in scoliosis associated with MFS, and this could take part in the bad behaviour of these deformities after fusion.
References
Pyeritz RE (1993) The Marfan syndrome. In: Royce PM, Steinmann B (eds) Connective tissue and its heritable disorders: molecular, genetic, and medical aspects. Wiley-Liss, New York, pp 437–468
Sponseller PD, Hobbs W, Riley LH 3rd, Pyeritz RE (1995) The thoracolumbar spine in Marfan syndrome. J Bone Joint Surg Am 77:867–876
Birch JG, Herring JA (1987) Spinal deformity in Marfan syndrome. J Pediatr Orthop 7:546–552
Robins PR, Moe JH, Winter RB (1975) Scoliosis in Marfan’s syndrome. Its characteristics and results of treatment in thirty-five patients. J Bone Joint Surg Am 57:358–368
Jones KB, Erkula G, Sponseller PD, Dormans JP (2002) Spine deformity correction in Marfan syndrome. Spine 27:2003–2012
Di Silvestre M, Greggi T, Giacomini S et al (2005) Surgical treatment for scoliosis in Marfan syndrome. Spine 30:E597–E604
Lipton GE, Guille JT, Kumar SJ (2002) Surgical treatment of scoliosis in Marfan syndrome: guidelines for a successful outcome. J Pediatr Orthop 22:302–307
Pomero V, Mitton D, Laporte S, de Guise JA, Skalli W (2004) Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) 19:240–247
Perdriolle R, Vidal J (1981) A study of scoliotic curve. The importance of extension and vertebral rotation (author’s transl). Rev Chir Orthop Reparatrice Appar Mot 67:25–34
Ouellet JA, LaPlaza J, Erickson MA et al (2003) Sagittal plane deformity in the thoracic spine: a clue to the presence of syringomyelia as a cause of scoliosis. Spine 28:2147–2151
Loder RT, Stasikelis P, Farley FA (2002) Sagittal profiles of the spine in scoliosis associated with an Arnold-Chiari malformation with or without syringomyelia. J Pediatr Orthop 22:483–491
De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE (1996) Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 62:417–426
Stokes IA (1994) Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3D terminology of spinal deformity. Spine 19:236–248
Giraudeau B, Mary JY (2001) Planning a reproducibility study: how many subjects and how many replicates per subject for an expected width of the 95% confidence interval of the intraclass correlation coefficient. Stat Med 20:3205–3214
Beighton P, De Paepe A, Hall JG et al (1992) Molecular nosology of heritable disorders of connective tissue. Am J Med Genet 42:431–448
Dietz HC, Cutting GR, Pyeritz RE et al (1991) Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352:337–339
Graf H, Hecquet J, Dubousset J (1983) 3-dimensional approach to spinal deformities. Application to the study of the prognosis of pediatric scoliosis. Rev Chir Orthop Reparatrice Appar Mot 69:407–416
Cruickshank JL, Koike M, Dickson RA (1989) Curve patterns in idiopathic scoliosis. A clinical and radiographic study. J Bone Joint Surg Br 71:259–263
Deacon P, Archer IA, Dickson RA (1987) The anatomy of spinal deformity: a biomechanical analysis. Orthopedics 10:897–903
Guo X, Chau WW, Chan YL, Cheng JC (2003) Relative anterior spinal overgrowth in adolescent idiopathic scoliosis. Results of disproportionate endochondral-membranous bone growth. J Bone Joint Surg Br 85:1026–1031
Dubousset J, Herring JA, Shufflebarger H (1989) The crankshaft phenomenon. J Pediatr Orthop 9:541–550
Gigante A, Chillemi C, Greco F (1999) Changes of elastic fibers in musculoskeletal tissues of Marfan syndrome: a possible mechanism of joint laxity and skeletal overgrowth. J Pediatr Orthop 19:283–288
Spiegel DA, Flynn JM, Stasikelis PJ et al (2003) Scoliotic curve patterns in patients with Chiari I malformation and/or syringomyelia. Spine 28:2139–2146
Flynn JM, Sodha S, Lou JE et al (2004) Predictors of progression of scoliosis after decompression of an Arnold Chiari I malformation. Spine 29:286–292
King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65:1302–1313
King HA (1988) Selection of fusion levels for posterior instrumentation and fusion in idiopathic scoliosis. Orthop Clin North Am 19:247–255
Dansereau J, Stokes IA (1988) Measurements of the three-dimensional shape of the rib cage. J Biomech 21:893–901
Mitton D, Landry C, Veron S et al (2000) 3D reconstruction method from biplanar radiography using non-stereo corresponding points and elastic deformable meshes. Med Biol Eng Comput 38:133–139
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine 32:568–573
Perdriolle R, Vidal J (1987) Morphology of scoliosis: three-dimensional evolution. Orthopedics 10:909–915
Perdriolle R, Le Borgne P, Dansereau J, de Guise J, Labelle H (2001) Idiopathic scoliosis in three dimensions: a succession of two-dimensional deformities? Spine 26:2719–2726
Dickson RA, Lawton JO, Archer IA, Butt WP (1984) The pathogenesis of idiopathic scoliosis. Biplanar spinal asymmetry. J Bone Joint Surg Br 66:8–15
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Glard, Y., Pomero, V., Collignon, P. et al. Sagittal balance in scoliosis associated with Marfan syndrome: a stereoradiographic three-dimensional analysis. J Child Orthop 2, 113–118 (2008). https://doi.org/10.1007/s11832-008-0083-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-008-0083-3