Abstract
Case
We report a rare case of a right-sided L4-5 facet osteoid osteoma in a 11-year-old female who presented with lower extremity pain, contractures, and gait disturbance in the setting of failed radiofrequency ablation. After open excision and single-level posterolateral fusion with instrumentation, her symptoms resolved and her spinopelvic parameters normalized.
Conclusions
This case highlights the contracture that may occur as a result of neurogenic pain from an osteoid osteoma in close proximity to neural structures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma (OO) of the spine is rare, accounting for 10% of OO cases [1, 2]. Radiofrequency ablation (RFA) is safe and effective in treating spinal OO when medical management fails, and thermal protection techniques during RFA may be used when a lesion is within 1 cm of a neural structure [1,2,3,4,5,6,7,8,9,10]. Open surgery is reserved for situations in which OO is not accessible via RFA or is too close to neural structures such that thermal protection cannot be performed safely [11]. We present a patient who underwent open excision with single-level posterolateral instrumented fusion for a right-sided L4-5 facet OO in close proximity to neural structures, and discuss her outcome through 2-year follow-up.
The patient and her parents were informed that the data concerning the case would be submitted for publication, and they provided consent.
Case report
Clinical presentation
Our patient was an otherwise-healthy 11-year 11-month-old female when she was referred to our clinic. Preoperatively, she reported leg cramping and right lower back pain which was present at night and relieved by NSAIDs. She had knee contractures with spasticity and numbness of bilateral lower extremities. Her symptoms had been present for 9 months. She failed nonoperative treatments and underwent RFA with 6 weeks of relief, but her symptoms returned. On exam, she ambulated with a crouched gait. She had bilateral knee flexion contractures and asymmetry on Adams forward bend. She had 5/5 strength throughout bilateral upper and lower extremities and sensation was intact in all dermatomes. She had 1 + left patellar and bilateral Achilles reflexes. Her right patellar reflex was absent and she had 4–5 beats of clonus bilaterally. Straight leg raise reproduced pain in her legs and back.
Diagnostic imaging and assessment
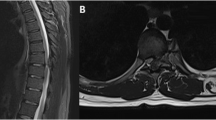
Preoperative radiographs showed that the patient was leaning forward in an effort to relieve her pain; her spinopelvic parameters normalized postoperatively (Table 1, Fig. 1). MRI was negative for neural impingement or intradural pathology. Single photon emission computed tomography (SPECT) and conventional CT showed a 0.8 × 1.3 × 0.5 cm lesion originating from the right L5 superior facet extending into the right L4-5 neuroforamen consistent with OO (Fig. 2). A second RFA procedure was considered, but in discussion with her interventionalist, it was felt that the lesion was too close to the right L4 nerve root without a sufficient cortical shell to allow for thermal protection and RFA.
Operative procedure and postoperative course
As she had failed nonoperative treatment and RFA, surgery was recommended. She underwent open excision of the right L4-5 facet OO and single-level posterolateral fusion with instrumentation. She had an uncomplicated perioperative course and surgical pathology was consistent with OO. She was discharged home on postoperative day 2. By 4 months postoperatively, her pain had resolved and her contractures (Fig. 3) and asymmetry on Adams forward bend had improved. At 2-year follow-up, she was asymptomatic without pain, numbness, or paresthesias. Her SRS scores improved from her preoperative baseline (Table 2). Her neurologic exam is normal. Her imaging shows a solid fusion mass, normal coronal balance, and improvement in her spinopelvic parameters (Table 1, Fig. 1).
Discussion
While spinal OO causing nerve root irritation has been described in the medical literature [12,13,14], our patient’s presentation with bilateral lower extremity contractures and spasticity represents a unique constellation of symptoms not routinely seen with OO. OOs have been shown to cause an inflammatory response through increased prostaglandin synthesis [15,16,17]; it is possible that our patient’s symptoms were related to the local inflammatory environment generated by her unilateral facet lesion.
Percutaneous RFA emerged as a treatment option for OO in 1989, and by the late, 1990s had replaced open excision as the dominant approach for lesions in the long bones and pelvis [18]. Numerous clinical series have supported the safety and efficacy of RFA in spinal OO; however, lesions in close proximity to neural elements present a unique treatment challenge [2, 3, 18,19,20,21]. Complications associated with RFA of spinal OO are rare but include temporary pain, limited mobility, and extremity paresthesias [2]; thermal protection techniques during RFA may be used to mitigate these risks [19, 22]. OO recurrence rates following RFA have been reported at 0–12.5% [2, 3, 11, 13]. Our patient’s symptoms returned 6 weeks after her RFA treatment and after a discussion with her interventionalist, the decision was made to proceed with open excision given the proximity of the lesion to the right L4 nerve root.
Open excision has been shown to be a safe and reliable approach for relieving pain and restoring function in patients with OO who have failed nonoperative measures [13, 14, 23,24,25]. Risks of open OO excision include incomplete removal and a potentially higher recurrence rate when compared with RFA, iatrogenic spinal instability, and nerve injury [4,5,6, 8]. We recommend performing an en-bloc resection when possible, instrumenting the area of resection to prevent instability, and using meticulous surgical technique when developing the interval between the lesion and surrounding neural tissues. Technologies including navigation and video-assisted thoracoscopic surgery may also be useful in localizing the lesion and preventing excessive bone removal. [7, 12, 24, 26].
Conclusion
We report a presentation of painful lower extremity symptoms and contractures from a right-sided L4-5 facet OO near neural elements in an adolescent female that was successfully treated using open excision and single-level posterolateral fusion with instrumentation. The authors encourage a multidisciplinary approach to the diagnostic workup and treatment of these lesions to optimize outcomes.
References
Weber MA, Sprengel SD, Omlor GW et al (2015) Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection. Skeletal Radiol 44(7):981–993. https://doi.org/10.1007/s00256-015-2139-z
Albisinni U, Facchini G, Spinnato P et al (2017) Spinal osteoid osteoma: efficacy and safety of radiofrequency ablation. Skeletal Radiol 46(8):1087–1094. https://doi.org/10.1007/s00256-017-2662-1
Faddoul J, Faddoul Y, Kobaiter-Maarrawi S et al (2017) Radiofrequency ablation of spinal osteoid osteoma: a prospective study. J Neurosurg Spine 26(3):313–318. https://doi.org/10.3171/2016.8.SPINE16462
Faraj A, Byrne P, Mehdian H (1998) Osteoid osteoma of the lateral mass of C5. Should excision be combined with fusion? Eur Spine J 7(3):242–245. https://doi.org/10.1007/s005860050065
Hempfing A, Hoffend J, Bitsch RG et al (2007) The indication for gamma probe-guided surgery of spinal osteoid osteomas. Eur Spine J 16(10):1668–1672. https://doi.org/10.1007/s00586-007-0388-9
Laus M, Albisinni U, Alfonso C et al (2007) Osteoid osteoma of the cervical spine: surgical treatment or percutaneous radiofrequency coagulation? Eur Spine J 16(12):2078–2082. https://doi.org/10.1007/s00586-007-0478-8
Rajasekaran S, Kamath V, Shetty AP (2008) Intraoperative Iso-C three-dimensional navigation in excision of spinal osteoid osteomas. Spine 33(1):E25–E29. https://doi.org/10.1097/BRS.0b013e31815e6308
Yang WT, Chen WM, Wang NH et al (2007) Surgical treatment for osteoid osteoma–-experience in both conventional open excision and CT-guided mini-incision surgery. J Chin Med Assoc 70(12):545–550. https://doi.org/10.1016/S1726-4901(08)70058-3
Filippiadis D, Mavrogenis A, Spiliopoulos S et al (2021) Percutaneous computed tomography-guided radiofrequency ablation of a spinal osteoid osteoma abutting the dura: a case report and review of the literature. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-021-02922-4
Lorenc T, Kocoń H, Gołębiowski M (2021) Computed tomography-guided percutaneous radiofrequency and laser ablation for the treatment of osteoid osteoma—long-term follow-up from 5 to 10 years. Pol J Radiol 86:e19–e30. https://doi.org/10.5114/pjr.2021.102678
Beyer T, van Rijswijk CSP, Villagran JM et al (2019) European multicentre study on technical success and long-term clinical outcome of radiofrequency ablation for the treatment of spinal osteoid osteomas and osteoblastomas. Neuroradiology 61(8):935–942. https://doi.org/10.1007/s00234-019-02226-9
Prod’homme M, Cavalié G, Kerschbaumer G et al (2019) T1 Vertebra pedicular osteoid osteoma: minimally invasive surgical resection aided by new integrated navigation to 3D imaging device. Case Rep Orthop 2019:7626454. https://doi.org/10.1155/2019/7626454
Mallepally AR, Mahajan R, Pacha S et al (2020) Spinal osteoid osteoma: surgical resection and review of literature. Surg Neurol Int 11:308. https://doi.org/10.25259/SNI_510_2020
Kirwan EO, Hutton PA, Pozo JL et al (1984) Osteoid osteoma and benign osteoblastoma of the spine. Clinical presentation and treatment. J Bone Joint Surg Br 66(1):21–26. https://doi.org/10.1302/0301-620X.66B1.6693472
Makley JT, Dunn MJ (1982) Prostaglandin synthesis by osteoid osteoma. Lancet 2(8288):42. https://doi.org/10.1016/s0140-6736(82)91174-6
Greco F, Tamburrelli F, Ciabattoni G (1991) Prostaglandins in osteoid osteoma. Int Orthop 15(1):35–37. https://doi.org/10.1007/BF00210531
Mungo DV, Zhang X, O’Keefe RJ et al (2002) COX-1 and COX-2 expression in osteoid osteomas. J Orthop Res 20(1):159–162. https://doi.org/10.1016/S0736-0266(01)00065-1
Rosenthal DI, Hornicek FJ, Wolfe MW et al (1998) Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 80(6):815–821. https://doi.org/10.2106/00004623-199806000-00005
Klass D, Marshall T, Toms A (2009) CT-guided radiofrequency ablation of spinal osteoid osteomas with concomitant perineural and epidural irrigation for neuroprotection. Eur Radiol 19(9):2238–2243. https://doi.org/10.1007/s00330-009-1404-8
Simon MA (1999) Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 81(3):437–438
Tomasian A, Wallace AN, Jennings JW (2017) Benign spine lesions: advances in techniques for minimally invasive percutaneous treatment. AJNR Am J Neuroradiol 38(5):852–861. https://doi.org/10.3174/ajnr.A5084
Rybak LD, Gangi A, Buy X et al (2010) Thermal ablation of spinal osteoid osteomas close to neural elements: technical considerations. AJR Am J Roentgenol 195(4):W293–W298. https://doi.org/10.2214/AJR.10.4192
Burn SC, Ansorge O, Zeller R et al (2009) Management of osteoblastoma and osteoid osteoma of the spine in childhood. J Neurosurg Pediatr 4(5):434–438. https://doi.org/10.3171/2009.6.PEDS08450
Kadhim M, Binitie O, O’Toole P et al (2017) Surgical resection of osteoid osteoma and osteoblastoma of the spine. J Pediatr Orthop B 26(4):362–369. https://doi.org/10.1097/BPB.0000000000000406
Ozaki T, Liljenqvist U, Hillmann A et al (2002) Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Relat Res 397:394–402. https://doi.org/10.1097/00003086-200204000-00046
Campos WK, Gasbarrini A, Boriani S (2013) Case report: Curetting osteoid osteoma of the spine using combined video-assisted thoracoscopic surgery and navigation. Clin Orthop Relat Res 471(2):680–685. https://doi.org/10.1007/s11999-012-2725-5
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, medical record review, and data collection were performed by JCFC. The first draft of the manuscript was written by JCFC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Neither Dr. Clohisy nor Dr. Rubio have any relevant financial or non-financial interests to disclose. In the past 36 months, Dr. Gupta has received royalties or honoraria, served as a paid consultant or speaker, or had paid travel from DePuy, Medtronic, Innomed, Scoliosis Research Society (SRS), AO Spine, Alphatec, Medicrea, Mizuho, Globus, and OMeGA, and has had stock in Johnson & Johnson and Procter & Gamble.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from the parents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clohisy, J.C.F., Rubio, D.R. & Gupta, M.C. Severe contracture in the lower extremity resulting from an osteoid osteoma of the lumbar spine in close proximity to neural elements in an adolescent: a case report. Spine Deform 10, 727–731 (2022). https://doi.org/10.1007/s43390-021-00449-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00449-6