Abstract
Study design
Retrospective comparative study.
Objectives
We hypothesize that preoperative bracing for idiopathic scoliosis results in increased stiffness, as measured by reduced correction on bending films, ultimately leading to decreased surgical correction.
Summary of background data
Bracing is the primary nonoperative treatment for immature AIS patients with mild to moderate curves. For patients who fail bracing and proceed to operative intervention, it is unknown whether their nonoperative treatment impacts their surgical results.
Methods
We conducted a single-center, retrospective, comparative study on 181 consecutive adolescent idiopathic scoliosis patients, aged 11–17 years, who underwent posterior spine fusion between 2011 and 2013. Patient flexibility was measured as percent change in the curve angle of the spine from standing to supine bend. Overall curve correction was calculated as the preoperative to postoperative change in standing coronal measure divided by the preoperative measurement and reported as a percentage.
Results
One hundred and twelve subjects (62%) underwent bracing prior to fusion. Braced patients had similar preoperative major Cobb angles than unbraced patients (56.5 vs 59.0, p = 0.07). Preoperatively, braced patients achieved less primary curve correction in bending films (33.6%) than unbraced patients (40.6%, p = 0.003). Postoperatively, Cobb angle correction was not different between the braced (75.7%) and unbraced group (77.2%) overall (p = 0.41). There was no difference in blood loss (p = 0.14) or surgical time (p = 0.96) between braced and unbraced groups when adjusted for surgeon and number of levels fused.
Conclusions
While braced patients may demonstrate less preoperative flexibility, there is no evidence that braced patients experience decreased curve correction compared to unbraced patients. Bracing treatment did not impact operative results, as indicated by similar Cobb angle correction, estimated blood loss, and surgical time in both groups.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bracing has the potential to alter the natural progression of idiopathic spinal deformity and therefore often precedes posterior spinal fusion (PSF). For adolescent idiopathic scoliosis (AIS) patients with mild to moderate curves (Cobb angle between 10° and 40°), bracing can halt or slow curve progression and reduce the need for surgical intervention [1,2,3,4,5]. However, it is unclear whether failed nonoperative treatment influences surgical outcomes and patient flexibility. To date, the few studies that have examined the effects of bracing on curve flexibility [6, 7] demonstrate inconsistent findings. While some studies have established a correlation between flexibility and age, curve magnitude, and curve location, factors affecting flexibility have yet to be definitively discerned [8, 9]. The purpose of this study is to investigate the effect of preoperative bracing for AIS on coronal curve stiffness. We hypothesize that preoperative bracing for AIS results in increased stiffness, as measured by reduced correction on bending films, and therefore may affect surgical correction.
Methods
We retrospectively reviewed patients, aged 10 to 18 years, who underwent posterior spine fusion for idiopathic scoliosis between 2011 and 2013 at our institution. All Lenke types and brace styles were included. Patients diagnosed with syndromic, congenital, and neuromuscular scoliosis were excluded, as well as patients undergoing revision for previous spine fusion. Patient characteristics including age, sex, BMI percentile, and Lenke curve classification as well as fusion characteristics including estimated blood loss (EBL), surgical time, osteotomy type, rod diameter and metal type, number of levels fused, number of screws, screw density, the number of implants and implant density were collected for all patients and summarized by bracing group (brace versus no brace). For our analysis, we defined screw density as the total number of poly-, mono-, and uniaxial screws used divided by the number of levels fused. Implant density was defined as the number of screws, rods, and hooks used divided by the number of levels fused. Continuous characteristics were summarized by mean and standard deviation (SD) or median and interquartile range (IQR, 25th–75th percentile), as appropriate, while categorical characteristics were summarized by frequency and percent.
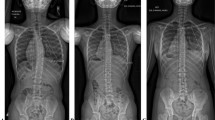
Major Cobb angle was measured in standing and supine bending positions preoperatively, and again in the standing position postoperatively. For supine maximal voluntary side-bending films, radiology technicians asked the patient to bend as far laterally as possible while maintaining a level pelvis. Supine bending films are less susceptible to errors due to technician skill compared with active bending radiographs, but both depend on the patient’s willingness and effort to bend. In cases with a double major curve pattern, only the dominant curve was analyzed. Patient flexibility was measured as the change in curve angle from standing to supine bend radiograph. The percent change was calculated as the change in curve measurement divided by the pre-bend measurement and multiplied by 100. Overall curve correction was calculated as the change in preoperative to postoperative standing coronal measure divided by the preoperative measurement and multiplied by 100. A negative/smaller curve percentage indicates a decrease in the curve magnitude, whereas a positive/larger percentage indicates an increase in curve magnitude. Change in curve measurements was summarized by group and 95% confidence intervals were estimated. Curve measurements and corresponding changes were compared across bracing groups using a Student’s t test.
Subgroup analysis was conducted on patients with a lumbar major curve. Curve correction was summarized for the lumbar subgroup and comparisons were conducted between the two bracing groups using multivariable regression analysis. Patient and surgical characteristics were compared across treatment groups using Student’s t tests, Mann–Whitney U tests, and χ2 tests, as appropriate, to assess comparability of the two groups. Finally, the bracing compliance and flexibility were assessed using general linear modeling. All tests were two-sided and p values less than 0.05 were considered significant.
Reducibility of the Cobb
Results
One hundred and eighty-one patients (16% male) who underwent PSF for AIS at an average age of 14.3 years (range 11 to 17 years) were identified (Table 1). The majority of curves were Lenke 1 (49%), the majority of surgeries used cobalt chromium rods (55%), and the average number of levels fused was 9.7 ± 2.11 (Table 1).
One hundred and twelve subjects (62%) underwent bracing prior to fusion. No differences were detected between braced and non-braced subjects with respect to age (p = 0.10), sex (p = 0.85), BMI percentile (p = 0.10), curve type (p = 0.10), or any surgical characteristics including EBL (p = 0.14), surgical time (p = 0.96), rod diameter (p = 0.19), metal type (p = 0.11), or the number of levels fused (p = 0.34).
Braced subjects had slightly lower, though non-significant, preoperative curve measurements compared with non-braced subjects (56.5 ± 8.6 vs 59.0 ± 9.4; p = 0.07) (Table 2). No difference was observed in curve measurement on bending films (p = 0.16) or postoperative films (p = 0.99) between the two bracing groups. However, unbraced subjects exhibited a greater percent change between preoperative standing and bending films over bracing subjects (41% vs 34%; p = 0.003) (Table 2). For both groups, the preoperative to postoperative curve corrections were similar and followed a similar trend (p = 0.41) (Table 2).
Twenty-two subjects (12%) presented with lumbar major curves. Curve progression was greater in the lumbar subgroup when controlling for bracing (77.9% vs 68.9%; p = 0.01). There was no difference, however, in curve correction in the lumbar subgroup between bracing groups (p = 0.09) (Table 3).
Discussion
Bracing is the primary nonoperative treatment for skeletally immature AIS patients with mild to moderate curves [10]. A strong correlation has been established between brace compliance and treatment outcomes in these patients; in the BRAIST study, patients who wore their braces at least 12.9 h per day saw a 90–93% success rate [11]. Even with excellent compliance, however, about 15% of curves will progress to the operative range [1,2,3,4, 11,12,13]. Despite reported successes with bracing, some curves progress to needing surgical intervention. The majority of the patients in this study underwent nonoperative treatment prior to fusion. For patients who fail bracing, the impact of nonoperative treatment on the surgical results is unknown.
Preoperatively, braced patients achieved less primary curve correction over unbraced patients, as determined by bending films. This is consistent with our hypothesis that bracing increases stiffness and decreases flexibility on bending films. Braced patients exhibited lower major Cobb angles at the time of surgery, but there was no difference in postoperative Cobb angle correction between the groups. There was no difference in the number of levels fused between the braced and unbraced groups, which may reflect patient or physician preference.
Analysis of the flexibility of different curves is essential for characterizing the deformity and planning surgery. The Lenke classification depends on side-bending radiographs to classify structural and non-structural curves [14]. Preoperative bending films may be used to decide the extent of fusion and appropriateness of selective versus non-selective fusion [8, 9, 15, 16]. Comparison between standard AP and active side-bending radiographs is often used to quantify flexibility [15, 17]. In general, the adult scoliotic spine is stiffer than that of an adolescent; however, the factors that cause this difference are unclear [18]. Based on our results, age prior to skeletal maturity is not a determining factor of flexibility.
A previous study by Sun et al. claimed that braced patients, regardless of curve pattern, had lower curve flexibility and significantly poorer surgical correct ability than unbraced patients [6]. Our results challenge both claims. Brace-induced changes in flexibility may depend on curve pattern and location; among our 22 subjects with lumbar curve patterns, we did not find the braced curves to be more or less flexible than their unbraced counterparts. Overall, however, braced curves were generally less flexible than unbraced curves. Regarding surgical correction, there was no difference between braced and unbraced patients overall or within the lumbar-only cohort.
Studies consistently show that thoracolumbar and lumbar curve patterns display greater flexibility than thoracic curves on bending films [6,7,8]. Our results reveal that curve pattern is only one part of the equation; prior brace treatment measures may affect flexibility.
We sought to evaluate the impact of bracing on curve characteristics and increased operative risks. Scoliosis bracing programs do not affect bone density accumulation in adolescent patients [19, 20], but other consequences of bracing remain unknown. Minimizing perioperative blood loss is a major concern for pediatric spine surgeons, as greater blood loss may lead to increased patient costs, inferior outcomes, and greater complication risks [21]. Perioperative blood loss varies significantly, with average blood loss during PSF procedures ranging between 275 and 907 mL [22,23,24,25]. Our results indicate no difference in blood loss or surgical time between braced and unbraced groups when adjusted for surgeon and number of levels fused.
Significance
This research shows that bracing, the most common nonoperative treatment for AIS, may increase coronal stiffness. However, surgical intervention resulted in comparable correction between braced and unbraced groups. Decreased flexibility was not associated with increased EBL, surgical time, or frequency of adverse outcomes.
When choosing a treatment strategy, surgeons should inform patients and their families of this and all other issues relevant to treatment and recovery.
Limitations
This study only analyzes radiographic outcomes of surgery. Patients’ increased stiffness may have more clinical relevance when examining scores on quality of life that are not evaluated in this study. We cannot attribute clinical significance to the differing implant densities between groups.
A major limitation is the retrospective nature of this study. Our data suggest that braced patients have greater implant density (Table 1); however, we cannot prove that implant density is related to preoperative curve stiffness. We also cannot prove that bracing directly causes stiffness in the scoliotic spine. It is possible that patients who failed bracing and resorted to surgical intervention had less flexible curves prior to brace treatment. We do not have bending films at the pre-brace, post-brace, and preoperative time points for all patients. Additionally, our analysis is limited by the binary categories of braced versus unbraced.
To further understand the impact of bracing on curve correctability, we propose a prospective study in which bending films are obtained at brace initiation and preoperatively for patients who fail bracing.
Conclusions
While braced patients may demonstrate less preoperative flexibility, we found that bracing treatment prior to surgical intervention does not impart differential operative results with respect to Cobb angle correction, blood loss, or surgical time.
Key Points
-
Patients who attempt bracing prior to surgery demonstrate less coronal flexibility on preoperative bending films when compared to unbraced patients.
-
Bracing treatment prior to surgical intervention does not impart differential operative results with respect to Cobb angle correction, blood loss, or surgical time.
-
Despite increased curve stiffness, braced patients achieve similar operative correction with greater implant density than unbraced patients.
Data availability
Permission is granted to reproduce copyrighted materials upon request.
References
Lonstein JE, Winter RB (1994) The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Jt Surg Am 76(8):1207–1221
Nachemson AL, Peterson LE (1995) Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Jt Surg Am 77(6):815–822
Zaborowska-Sapeta K, Kowalski IM, Kotwicki T, Protasiewicz-Faldowska H, Kiebzak W (2011) Effectiveness of Cheneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis 6(1):2
Zheng X, Sun X, Qian B, Wu T, Mao S, Zhu Z et al (2012) Evolution of the curve patterns during brace treatment for adolescent idiopathic scoliosis. Eur Spine J 21(6):1157–1164
Hong A, Jaswal N, Westover L, Parent EC, Moreau M, Hedden D et al (2017) surface topography classification trees for assessing severity and monitoring progression in adolescent idiopathic scoliosis. Spine (Phila PA 1976) 42(13):E781–E787
Sun X, Liu WJ, Xu LL, Ding Q, Mao SH, Qian BP et al (2013) Does brace treatment impact upon the flexibility and the correctability of idiopathic scoliosis in adolescents? Eur Spine J 22(2):268–273
Hirsch C, Ilharreborde B, Mazda K (2016) Flexibility analysis in adolescent idiopathic scoliosis on side-bending images using the EOS imaging system. Orthop Traumatol Surg Res 102(4):495–500
Clamp JA, Andrews JR, Grevitt MP (2008) A study of the radiologic predictors of curve flexibility in adolescent idiopathic scoliosis. J Spinal Disord Tech 21(3):213–215
Deviren V, Berven S, Kleinstueck F, Antinnes J, Smith JA, Hu SS (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine 27(21):2346–2349
Richards BS, Bernstein RM, D'Amato CR, Thompson GH (2005) Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS committee on bracing and nonoperative management. Spine (Phila PA 1976) 30(18):2068–2075 (discussion 76–77)
Weinstein SL, Dolan LA, Wright JG, Dobbs MB (2013) Effects of Bracing in adolescents with idiopathic scoliosis. N Engl J Med 369(16):1512–1521
Lange JE, Steen H, Gunderson R, Brox JI (2011) Long-term results after Boston brace treatment in late-onset juvenile and adolescent idiopathic scoliosis. Scoliosis 6:18
Fernandez-Feliberti R, Flynn J, Ramirez N, Trautmann M, Alegria M (1995) Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr orthop 15(2):176–181
Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am 83-a(8):1169–1181
Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton J (2001) Prospective comparison of flexibility radiographs in adolescent idiopathic scoliosis. Spine 26(5):E74–E79
Hamzaoglu A, Talu U, Tezer M, Mirzanli C, Domanic U, Goksan SB (2005) Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine 30(14):1637–1642
Davis BJ, Gadgil A, Trivedi J, Ahmed el NB (2004) Traction radiography performed under general anesthetic: a new technique for assessing idiopathic scoliosis curves. Spine 29(21):2466–2470
Lonstein JE (2006) Scoliosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 443:248–259
Snyder BD, Zaltz I, Breitenbach MA, Kido TH, Myers ER, Emans JB (1995) Does bracing affect bone density in adolescent scoliosis? Spine 20(14):1554–1560
Snyder BD, Katz DA, Myers ER, Breitenbach MA, Emans JB (2005) Bone density accumulation is not affected by brace treatment of idiopathic scoliosis in adolescent girls. J Pediatr orthop 25(4):423–428
Oetgen ME, Litrenta J (2017) Perioperative blood management in pediatric spine surgery. J Am Acad Orthop Surg 25(7):480–488
Fletcher ND, Shourbaji N, Mitchell PM, Oswald TS, Devito DP, Bruce RW (2014) Clinical and economic implications of early discharge following posterior spinal fusion for adolescent idiopathic scoliosis. J Child Orthop 8(3):257–263
Fletcher ND, Andras LM, Lazarus DE, Owen RJ, Geddes BJ, Cao J et al (2017) Use of a novel pathway for early discharge was associated with a 48% shorter length of stay after posterior spinal fusion for adolescent idiopathic scoliosis. J Pediatr orthop 37(2):92–97
Ialenti MN, Lonner BS, Verma K, Dean L, Valdevit A, Errico T (2013) Predicting operative blood loss during spinal fusion for adolescent idiopathic scoliosis. J Pediatr orthop 33(4):372–376
Shapiro F, Sethna N (2004) Blood loss in pediatric spine surgery. Eur Spine J 13(Suppl 1):S6–17
Funding
This work was funded internally through the Boston Children’s Hospital Orthopaedic Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Institutional Review Board approval at Boston Children’s Hospital was received for this research.
Informed consent
A waiver of informed consent was requested and approved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hogue, G., DeWitt, L., Grzywna, A. et al. Does bracing for adolescent idiopathic scoliosis affect operative results?. Spine Deform 8, 427–432 (2020). https://doi.org/10.1007/s43390-020-00066-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00066-9