Abstract
Purpose
Brace treatment has served as a vital non-surgical procedure for immature adolescent idiopathic scoliosis (AIS) patients with a mild or moderate curve. For the patients who fail in bracing and resort to surgery, it is unclear whether prior full-time brace treatment significantly influences outcomes. This study aims to investigate whether prior brace treatment has a negative impact upon the flexibility and correctability of the main curve in patients with AIS.
Methods
The participants were collected from female AIS patients who underwent posterior correction surgery with pedicle screw instrumentation from August 2006 to December 2010, with or without prior brace treatment. Patients included in Group A had prior brace treatment over a 1-year period, and underwent surgery within 6 months after cessation of bracing; those in Group B received no prior treatment and were randomly selected from our database. Curve flexibility pre-surgery and curve correctability post-surgery were computed and compared between both groups and subgroups according to the curve location.
Results
Each group consisted of 35 patients. Age, curve magnitude and location were comparable between the two groups. Before surgery, patients in Group A had a slightly lower curve flexibility than those in Group B (52 vs. 60 %, P = 0.036). After surgery, satisfactory correction results were observed in both groups, but the average post-operative main curve magnitude of patients in Group B was 4° less than that of Group A (10° vs. 14°, P = 0.010). The curve correctability in Group B was significantly higher than that in Group A (80 vs. 74 %, P = 0.002). No matter what curve pattern the patient had, having a prior history of brace treatment resulted in a trend of lower flexibility and correctability of their scoliosis.
Conclusions
Good surgical correction can be achieved in AIS patients who have been unsuccessful with prior brace treatment. However, a history of prior brace treatment leads to a trend of lowering the curve flexibility, and in turn, negatively impacts upon the curve correctability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is one of the most common spine deformities, occurring predominantly in peri-pubertal girls [29]. Currently, the standard of care for AIS patients includes the following options: observation, for patients with a small curve or skeletal maturity; brace treatment, for those with a mild or moderate curve and skeletal immaturity; and surgical correction, for those with a severe curve [2]. Until now, brace treatment has served as a vital non-surgical procedure for immature AIS patients with a mild or moderate curve, because bracing can effectively halt curve progression and prevent surgical intervention in some cases [17, 19, 23, 31, 34, 35]. To date, several types of brace devices have been developed, such as the Milwaukee [17], Boston [19], Charleston [25], Providence [32], Rosenberger [24], Wilmington [1] and Chêneau [34]. Brace treatment for AIS patients is largely successful but at times does fail to control curve progression. In some patients, curves progress despite brace treatment, and surgical intervention is therefore recommended.
As a pre-operative preparation for corrective surgery, the curve flexibility evaluation performed before surgery helps to clarify the fusion levels, to determine whether to fuse the compensatory curve, and to predict correction outcome [13]. Some studies have documented several factors, for example, age, curve magnitude and location, all of which serve to influence curve flexibility [6, 7].
For those patients who resort to surgical intervention after bracing treatment, it is wondered herein whether prior full-time brace treatment results in significant adverse effects. Existing literature fails to adequately address the question of the impact of full-time brace treatment on the curve flexibility and correctability in these patients. The purpose of this study is to investigate whether prior brace treatment influences the curve flexibility and correctability in AIS patients.
Methods
After obtaining approval from the ethics committee of our hospital, we performed a case–control study of patients who had undergone correction of spinal deformity from August 2006 to December 2010. Patients who underwent brace treatment before scoliosis correction surgery were identified and included after meeting the following criteria: female; age ranging from 11 to 18 years; having a main thoracic, thoracolumbar or lumbar curve; having an initial out-of-brace standing curve magnitude of 25°–45°; having a final curve magnitude of <70°, with curve magnitude narrowed to minimize bias from a possible range of curve magnitude on curve flexibility; receiving a prior brace treatment with good compliance (>90 %; compliance was computed as the ratio of the actual daily bracing time, which was recorded at each visit according to the information provided by the patient and his or her parents, to the recommended daily time) [22]; bracing duration lasting over 12 months; normal daily out-of-brace activities; undergoing one-stage posterior spinal fusion with pedicle screw-only instrumentation within 6 months after cessation of bracing; having available radiographic data before brace initiation, pre- and post-operatively. These patients constituted Group A. Another group of patients were randomly chosen from our scoliosis database, from those who did not experience any type of treatment before, serving as the control group (Group B). The inclusion criteria of Group B were the same as those of Group A, except for brace treatment history. The number of patients in Group B was set equal to that in Group A, with age, curve magnitude and curve location being well matched between both groups. Patients in both groups were managed with one-stage posterior correction and fusion surgery. All surgeries were performed by the same surgeon, the most experienced one of our team (Y.Q.), with the use of monoaxial pedicle screw instrumentation (CD-Horizon Systems, or CD-Horizon Legacy Spinal Systems, Medtronic, USA).
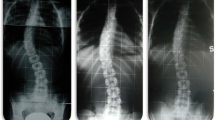
In both groups, pre-operative radiographic evaluations included standing postero-anterior (PA) and lateral radiographs, as well as supine PA and side bending (SB) radiographs [7]. Post-operative radiographic evaluations consisted of standing PA and lateral radiographs taken about 2 weeks after surgery.
Curves on the X-ray films were measured using the Cobb method. Initially, measurements were taken by two experienced investigators (X.S. and W.L.) in 20 cases randomly chosen from the two groups at an interval of 15 days and were repeated twice by one investigator (X.S.) at an interval of 20 days. The inter- and intra-observer correlation coefficients were 0.93 and 0.95, respectively, both indicating excellent inter- and intra-observer reliability. The remaining measurement work was then completed by one investigator (X.S.).
Representing the correction rate of side bending, the curve flexibility of the major curve was determined according to the following formula: \( {\text{curve flexibility = }}\frac{{ ( {\text{curve}}_{\text{pre - op}} {\text{PA}} - {\text{curve}}_{\text{pre - op}} {\text{SB) }} \times 1 0 0 {\text{\% }}}}{{{\text{curve}}_{\text{pre - op}} {\text{PA}}}} \). To evaluate the correction outcome immediately after surgery, the curve correctability of the major curve was defined as the extent to which the curve was surgically corrected and computed based on the following formula: \( {\text{curve correctability = }}\frac{{ ( {\text{curve}}_{\text{pre - op}} {\text{PA}} - {\text{curve }}_{\text{post - op}} {\text{PA) }} \times 1 0 0 {\text{\% }}}}{{ {\text{curve}}_{\text{pre - op}} {\text{PA}}}}. \)
Data were analyzed using SPSS version 13.0 (SPSS, Chicago, IL, USA). All main curve physical characteristics relevant to flexibility and correctability were compared between groups A and B, through the Student’s t test. Considering the effect of curve location on the curve flexibility and correctability, patients from both groups were further subdivided according to the curve location, i.e., thoracic and thoracolumbar/lumbar. Comparisons of groups A and B were performed. All statistical analyses in this study were two sided with statistical significance set at P < 0.05.
Results
Thirty-five patients were included in Group A, after meeting the inclusion criteria. Of all, 27 patients had worn a Milwaukee brace before, among whom three changed to a Boston brace later; an additional 8 more patients also wore a Boston brace. The mean age was 14.3 years, and the mean duration of bracing was 27 months. The mean Cobb angle of the main curve aggravated on average from 37° (range 28°–45°) before bracing to 52° (range 45°–69°) before surgery. Regarding curve location, a main thoracic curve was identified in 27 patients and a main thoracolumbar/lumbar curve in 8. Of the 35 patients in Group B, the mean age was 14.1 years and the mean Cobb angle of the main curve was 52°. Twenty-eight patients were found with a main thoracic curve, and 7 patients with a main thoracolumbar/lumbar curve. There were no significant differences between the two groups in terms of age, curve magnitude and curve pattern (P > 0.05).
After the surgery, patients of Group A experienced a correction to a mean post-operative Cobb angle of 14° and those of Group B to 10°. Patients in Group B had a significantly smaller post-operative main curve magnitude than Group A (P = 0.010).
The curve flexibility ranged from 32 to 84 % in patients of Group A and from 30 to 98 % in those of Group B; the curve correctability spanned from 54 to 95 % in Group A and from 56 to 100 % in Group B. The means of the curve flexibility and correctability of both groups are shown in Table 1. Patients in Group A had a slightly lower curve flexibility than those in Group B (52 vs. 60 %, P = 0.036). Satisfactory correction results were obtained from both groups after surgery. The curve correctability in Group B was significantly higher than that in Group A (80 vs. 74 %, P = 0.006).
After dividing patients into subgroups based on curve location, similar findings were observed. As shown in Table 2, regardless of curve location, patients who had prior brace treatment had slightly lower curve flexibility (thoracic curve, 49 vs. 56 %; thoracolumbar/lumbar curve, 61 vs. 76 %) and slightly to significantly lower correctability than those without prior brace treatment (thoracic curve, 74 vs. 79 %; thoracolumbar/lumbar curve, 73 vs. 87 %). Also, curves of a main thoracic pattern appeared less flexible than those of a thoracolumbar/lumbar pattern both in Group A (49 vs. 61 %, P = 0.017) and Group B (56 vs. 76 %, P = 0.012). After corrective surgery, the curve correctability was similar in Group A (74 vs. 73 %, P = 0.877), yet remained higher in patients with a thoracolumbar/lumbar curve in Group B (79 vs. 87 %, P = 0.030).
Discussion
Pre-operative evaluations of scoliosis are crucial in planning correction surgery. One of the most important evaluations relates to the assessment of curve flexibility [6, 7, 11, 13]. After understanding the flexibility of curves, spine surgeons are able to reasonably judge the rigidity of scoliosis, determine fusion levels and predict correction outcome. Several types of curve flexibility assessment methods have been introduced previously, such as measurements on supine side bending [7, 26], fulcrum bending [6, 15] and traction films [11, 16]. Evaluating the curve flexibility through measurement on supine side bending films is currently feasible and convenient [7].
The influencing factors of the curve flexibility have been documented in several studies [6, 7]. These factors were reported to include age, curve magnitude and curve location. Deviren et al. [7] detected that the curve flexibility was inversely correlated with both curve magnitude and age in both adolescent and adult patients with a major thoracolumbar/lumbar idiopathic scoliosis. They stated that the curve flexibility changed predictably with age and magnitude [7]. Clamp et al. [6] reported a study of 101 idiopathic scoliosis patients through measurements on standing and fulcrum bending radiographs, and found that curve magnitude and age were the only significant predictors of curve flexibility. They discovered that curve location was also important in predicting flexibility with thoracolumbar curves being significantly more flexible than thoracic curves [6]. In theory, the increase in rigidity of thoracic curves might be due to the restriction of the chest wall. Aside from the above-mentioned treatments, we know of no additional factors which contribute to the influencing of curve flexibility in the treatment of scoliosis.
Brace treatment is used as the mainstay of non-operative treatment for immature AIS patients with a mild or moderate curve [23]. Although the effectiveness of brace treatment has not yet gained unanimous agreement [9], it has been proven in many studies that bracing is an effective modality in preventing curve progression as compared to non-bracing or other types of conservative treatment [10, 14, 17, 19]. Notwithstanding the effectiveness of bracing, curve progression is observed in some AIS patients during the period of such treatment. Curve progression has been reported to be around 20 % [17, 19, 33]. Because of curve aggravation, some AIS patients resort to surgical intervention. For these patients, the result of the pre-operative evaluation for curve flexibility remains unknown. In our study, pre-operative evaluation revealed that patients with prior brace treatment had lower curve flexibility than those without, regardless of curve location. Although the difference was of marginal significance, having prior brace treatment led to a trend of lowering the curve flexibility in patients with AIS.
To achieve a relatively satisfactory outcome, AIS patients are routinely required to comply with brace policy by following adequate in-brace time per day [17, 30]. The daily step activities in AIS patients were measured with an ankle monitor and reported not to be interfered by bracing in a recent study [18]; however, the activities of the trunk and the upper extremities were ignored. An adequate in-brace time is more costly to the patient and can possibly result in decreased daily out-of-brace physical activity and a probable reduction in the use of the back muscles. Owing to the contribution of daily out-of-brace physical activity to the flexibility of scoliosis, it is hypothesized that brace treatment decreases daily physical activity, which in turn leads to decreased flexibility of scoliosis. At the same time, it cannot be denied that patients unsuccessful with brace treatment might have a slightly more rigid curve than those succeeding in bracing treatment, resulting from some unknown inherent factors. This should also be taken into account when analyzing the factors contributing to the decreased flexibility of scoliosis after bracing treatment.
The correction outcome from surgery is one of the most important concerns for both surgeons and patients. Optimal correction of scoliosis and balanced reconstruction of the spine have always been the major goal of surgical intervention. Previous studies have demonstrated a strong consistency between the curve flexibility and the correction rate [12, 15]. In a cohort of thoracic idiopathic scoliosis patients, King et al. [12] reported the coincidence between the correction rate and the curve flexibility computed through measurements on supine side bending films. Li et al. [15] found that the curve corrections of the proximal thoracic, main thoracic and thoracolumbar/lumbar curves, via posterior pedicle screw fixation and fusion, were highly correlated with flexibility assessment in AIS patients. Our study demonstrated a satisfactory curve correction in both groups, as well as a slight but significant decrease of the curve correctability in patients experiencing brace treatment before surgery. Herein, the curve correctability means the extent to which the curve can be surgically corrected. For AIS patients who resort to surgery, age, curve magnitude and curve pattern are the main factors influencing curve flexibility [6, 7]; curve pattern, flexibility and correction maneuver are the main factors influencing curve correctability [3, 5, 15]. In the current study, the physical data of patients in both groups were well matched and the surgeries were performed by the same experienced surgeon. The only difference remained in the fact that the curve flexibility was lower in Group A than in Group B. So, it is logically inferred that lower curve correctability in Group A resulted from lower curve flexibility. As mentioned previously, AIS patients with prior brace treatment had a lower flexibility than those without. Therefore, prior brace treatment led to not only a decrement in the curve flexibility, but also had a negative impact on the curve correctability.
To our knowledge, there are no published studies which concentrate on the comparisons of the flexibility and correctability of scoliosis between patients with and without a bracing history. Yet, the comparison of the curve flexibility or the curve correctability was somewhat incidentally recorded in several studies [27, 28]. In the study by Weigert et al. [28], the curve flexibility was not compared in particular, yet a little larger curve correction was noted in AIS patients who were surgically treated than those who underwent brace treatment followed by surgery (57.1°–33.7° vs. from 54.9° to 34.3°). Wang et al. [27] discussed slight and insignificant decreases in curve flexibility (50.4 vs. 56.2 %) and the correction rate (69.5 vs. 71.8 %) of the major curve in patients with brace history as compared to patients without. Nevertheless, no particular attention in these studies was paid to a number of crucial factors, which potentially impacted on the results, such as curve pattern, duration of prior brace treatment, and the interval between brace cessation and surgical intervention.
Although the values of the curve flexibility and the curve correctability were close between patients with prior brace treatment and those without, the differences in both were revealed to be statistically significant. However, it should be noted that the significant difference in radiographic outcome may not indicate a similar difference in the outcome of cosmetic appearance or of quality of life. Application of some questionnaires might be helpful to determine the variance in terms of cosmetic appearance and quality of life. Actually, several including the above-mentioned studies were performed for the purpose of investigating the impact of prior brace treatment on the quality of life after surgery [8, 20, 27, 28]. Noonan et al. [20] found that surgical intervention after brace treatment led to a more negative body image of the axial skeleton in comparison to the brace-only treatment. Using the SRS-24 questionnaire, Weigert et al. [28] reported that brace treatment followed by surgery appeared to yield a similar outcome as compared to surgery-only treatment. This was consistent with the findings of the study by Wang et al. [27], who utilized the SRS-22 questionnaire. Recently, a multi-center prospective study revealed that patients with prior brace treatment had more pain, lower activity levels, lower satisfaction and lower total SRS-30 scores at 2 years after operation than those without [8]. Although the debate continues, what is worth being mentioned is that the quality of life after brace treatment followed by surgical intervention becomes an important concern.
It deserves noting that, because of the probable potential of bracing to partially correct the deformity, the curve magnitude to be considered in patients whose brace treatment were unsuccessful should be the theoretical one in those without previous brace treatment. From a theoretical point of view, the virtual flexibility and correctability of these patients might be similar to those in non-braced patients. The clinical relevance of the results of this study relates to the pre-operative evaluation of AIS patients who have failed brace treatment for greater than 1 year. Before surgery, surgeons should inform patients and their families of this and all other issues relevant to treatment and recovery. Curve flexibility and correctability can probably be negatively influenced to a certain extent, if bracing fails to help avoid surgical correction. Moreover, this study adds some important information to brace treatment. It is of increasing importance at brace initiation to distinguish the patients in whom brace treatment is most likely to fail from those whose treatment would likely succeed. It is best to explain to the parents the therapeutic options as well as our concerns about the limitation of our knowledge about the efficacy of the braces, and to provide with the most thorough information regarding treatment cost for both the brace and surgery if necessary. Despite all this, the results of our study do not show any negative influence on the recommendations of brace treatment for an eligible candidate with AIS, due to the sound evidence of effectiveness of brace treatment [10, 14, 17, 19, 34, 35]. Also, notable in this study is how the impact of brace treatment on AIS patients differed slightly between diverse curve patterns, appearing less visible in a main thoracic curve. A possible explanation for such a finding is that the impact of brace treatment might be coupled with the extent of the inherent flexibility of a curve. In the future, a study with a larger sample needs to be done to validate this.
There are several weaknesses in this study. First, our sample size is relatively small, thus limiting the statistical power of the results. This may result largely from the restrictive inclusion criteria of patients with regard to age, curve magnitude, and the duration and compliance of brace treatment, as well as the timing and instrumentation type of surgery performed. Hopefully, the impact of prior bracing treatment on surgery can be fully and exclusively investigated in this study. Second, this study is not a prospective randomized one and fails to exclude any possible inherent differences in the initial curve characteristics between the bracing and non-bracing groups, despite the age and curve magnitude criterion being well matched. To clarify this, a prospective RCT is expected, which is however not feasible currently based on the study of Bunge EM et al. [4]. Third, this study also lacks comparisons on the quality of life after surgery between groups A and B. Assessments of quality of life were available for only a portion of patients in this study after the introduction of the simplified Chinese version of the SRS-22 questionnaire [21]. As mentioned previously, this research has been done recently in other studies [20, 28].
In conclusion, pre-operative brace treatment reduces the flexibility of the main curve in AIS to some extent, and thus has a negative impact on the correctability. Yet, it should be noted that the increased stiffness may have more clinical relevance in terms of the correction outcome and the quality of life than the cosmetic appearance. Before brace prescription, it is best to explain to the parents the therapeutic options as well as our concerns about the negative impact of brace treatment.
References
Allington NJ, Bowen JR (1996) Adolescent idiopathic scoliosis: treatment with the Wilmington brace. A comparison of full-time and part-time use. J Bone Joint Surg Am 78:1056–1062
Asher MA, Burton DC (2006) Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis 1:2
Aubin CE, Labelle H, Chevrefils C, Desroches G, Clin J, Eng AB (2008) Preoperative planning simulator for spinal deformity surgeries. Spine (Phila Pa 1976) 33:2143–2152
Bunge EM, Habbema JD, de Koning HJ (2010) A randomised controlled trial on the effectiveness of bracing patients with idiopathic scoliosis: failure to include patients and lessons to be learnt. Eur Spine J 19(5):747–753
Cheung WY, Lenke LG, Luk KD (2010) Prediction of scoliosis correction with thoracic segmental pedicle screw constructs using fulcrum bending radiographs. Spine (Phila Pa 1976) 35:557–561
Clamp JA, Andrews JR, Grevitt MP (2008) A study of the radiologic predictors of curve flexibility in adolescent idiopathic scoliosis. J Spinal Disord Tech 21:213–215
Deviren V, Berven S, Kleinstueck F, Antinnes J, Smith JA, Hu SS (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine (Phila Pa 1976) 27:2346–2349
Diab M, Sharkey M, Emans J, Lenke L, Oswald T, Sucato D, Spinal Deformity Study Group (2010) Preoperative bracing affects postoperative outcome of posterior spine fusion with instrumentation for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35:1876–1879
Dolan LA, Weinstein SL (2007) Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976) 32(19 Suppl):S91-S100
Fernandez-Feliberti R, Flynn J, Ramirez N, Trautmann M, Alegria M (1995) Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop 15:176–181
Hamzaoglu A, Talu U, Tezer M, Mirzanli C, Domanic U, Goksan SB (2005) Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 30:1637–1642
King HA, Moe JH, Bradford DS, Winter RB (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65:1302–1313
Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton J (2001) Prospective comparison of flexibility radiographs in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 26:E74–E79
Lange JE, Steen H, Brox JI (2009) Long-term results after Boston brace treatment in adolescent idiopathic scoliosis. Scoliosis 4:17
Li J, Dumonski ML, Samartzis D, Hong J, He S, Zhu X, Wang C, Vaccaro AR, Albert TJ, Li M (2011) Coronal deformity correction in adolescent idiopathic scoliosis patients using the fulcrum-bending radiograph: a prospective comparative analysis of the proximal thoracic, main thoracic, and thoracolumbar/lumbar curves. Eur Spine J 20:105–111
Liu RW, Teng AL, Armstrong DG, Poe-Kochert C, Son-Hing JP, Thompson GH (2010) Comparison of supine bending, push-prone, and traction under general anesthesia radiographs in predicting curve flexibility and postoperative correction in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35:416–422
Lonstein JE, Winter RB (1994) The Milwaukee brace for the treatment of adolescent idiopathic scoliosis: a review of one thousand and twenty patients. J Bone Joint Surg Am 76:1207–1221
Muller C, Fuchs K, Winter C, Rosenbaum D, Schmidt C, Bullmann V, Schulte TL (2011) Prospective evaluation of physical activity in patients with idiopathic scoliosis or kyphosis receiving brace treatment. Eur Spine J 20(7):1127–1136
Nachemson AL, Peterson LE (1995) Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 77:815–821
Noonan KJ, Dolan LA, Jacobson WC, Weinstein SL (1997) Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J Pediatr Orthop 17:712–717
Qiu G, Qiu Y, Zhu Z, Liu Z, Song Y, Hai Y, Luo Z, Liu Z, Zhang H, Lv G, Wang Y, Zhang J, Shen J, Sun X (2011) Re-evaluation of reliability and validity of simplified Chinese version of SRS-22 patient questionnaire: a multicenter study of 333 cases. Spine (Phila Pa 1976) 36:E545–E550
Qiu Y, Sun X, Cheng JC, Zhu F, Li W, Zhu Z, Wang B, Yu Y (2008) Bone mineral accrual in initially osteopenic and non-osteopenic adolescents with idiopathic scoliosis during bracing treatment. Spine (Phila Pa 1976) 33:1682–1689
Richards BS, Bernstein RM, D’Amato CR, Thompson GH (2005) Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS committee on bracing and nonoperative management. Spine (Phila Pa 1976) 30:2068–2075
Spoonamore MJ, Dolan LA, Weinstein SL (2004) Use of the Rosenberger brace in the treatment of progressive adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:1458–1464
Trivedi JM, Thomson JD (2001) Results of Charleston bracing in skeletally immature patients with idiopathic scoliosis. J Pediatr Orthop 21:277–280
Vaughan JJ, Winter RB, Lonstein JE (1996) Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 21:2469–2473
Wang C, Zhao Y, He S, Zhu X, Zhao Y, Chen Z, Gu S, Xie Y, Li M (2009) Effect of preoperative brace treatment on quality of life in adolescents with idiopathic scoliosis following corrective surgery. Orthopedics 32(8). pii:orthosupersite.com/view.asp?rID = 41920. doi:10.3928/01477447-20090624-10. PubMed PMID: 19708629
Weigert KP, Nygaard LM, Christensen FB, Hansen ES, Bünger C (2006) Outcome in adolescent idiopathic scoliosis after brace treatment and surgery assessed by means of the Scoliosis Research Society Instrument 24. Eur Spine J 15:1108–1117
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537
Wiley JW, Thomson JD, Mitchell TM, Smith BG, Banta JV (2000) Effectiveness of the Boston brace in treatment of large curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 25:2326–2332
Xu L, Qiu X, Sun X, Mao S, Liu Z, Qiao J, Qiu Y (2011) Potential genetic markers predicting the outcome of brace treatment in patients with adolescent idiopathic scoliosis. Eur Spine J 20:1757–1764
Yrjönen T, Ylikoski M, Schlenzka D, Kinnunen R, Poussa M (2006) Effectiveness of the Providence nighttime bracing in adolescent idiopathic scoliosis: a comparative study of 36 female patients. Eur Spine J 15:1139–1143
Yrjönen T, Ylikoski M, Schlenzka D, Poussa M (2007) Results of brace treatment of adolescent idiopathic scoliosis in boys compared with girls: a retrospective study of 102 patients treated with the Boston brace. Eur Spine J 16:393–397
Zaborowska-Sapeta K, Kowalski IM, Kotwicki T, Protasiewicz-Fałdowska H, Kiebzak W (2011) Effectiveness of Chêneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis 25 6(1):2
Zheng X, Sun X, Qian B, Wu T, Mao S, Zhu Z, Wang B, Qiu Y (2012) Evolution of the curve patterns during brace treatment for adolescent idiopathic scoliosis. Eur Spine J 21:1157–1164
Acknowledgments
A grant research support from Stryker Spine is acknowledged, which may indirectly relate to the subject of this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, X., Liu, Wj., Xu, Ll. et al. Does brace treatment impact upon the flexibility and the correctability of idiopathic scoliosis in adolescents?. Eur Spine J 22, 268–273 (2013). https://doi.org/10.1007/s00586-012-2477-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2477-7