Abstract
Diabetes linked reproductive complications are rising problems nowadays. The study focused on the protective efficacy of Aloe vera (L.) on sperm cell damage in an oxidative stress milieu encumbered by a chronic diabetes in human and streptozotocin treated Wistar rat (Rattus norvegicus). Spermatozoa from rat’s epididymal washing, and human semen after 3–4 days of abstinence of mating or masturbation were collected from control and diabetes groups. Spermatozoa of human and rat were incubated for 1 or 2 h at 370C in an in-vitro medium separately and considered as normo-glycemic control and diabetes sub-groups. Dose of 1 or, 2 or, 4 mg/ml of Aloe vera (L.) hydro-ethanolic (40:60) extract (AVHE) was given to diabetes samples, considered as sub-sub-group for assessing its protective effect on spermiological and oxidative stress parameters. The motility, viability, plasma membrane integrity, nuclear chromatin decondensation for DNA fragmentation, acrosome cap status, and antioxidative status of human and rat spermatozoa were decreased whereas spermatozoal apoptosis was elevated significantly (p < 0.05), noted by TUNEL assay in diabetes samples compared to the duration-matched control group. Exposure of AVHE to diabetes samples resulted significant rectification (p < 0.05) in the said parameters than the unexposed diabetes group. In control group, AVHE exposure has significant protective effect from spermiological deterioration compared to unexposed control group. Identification of major phytomolecules in AVHE was done by LC–MS study. Diabetes-induced oxidative stress-mediated spermatozoal injuries can be protected by AVHE extract, raise the possibility for potentiating sperm of human for increasing the success rate of in-vitro fertilization-blastocyst implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus, a global epidemic, presently affects 42.2 crore individuals throughout the world with impaired fecundity which is increasing but still overlooked. The reports focused that 35–51% of diabetic males have various degrees of reproductive complications [1].The actual reason behind this pathophysiological condition is not clearly known. However, in the literature, severe oxidative stress imposition induced by defective glucose metabolism in diabetes took a dominant role in the onset of male infertility [2]. Unsuccessful procreation leads to a poor quality of life associated with traumatic mental distress that further deteriorates the diabetic condition [3]. Drugs for the treatment of diabetes are available commercially, but to what extent these are efficacious in managing sexual dysfunction remains beyond knowledge. Antioxidant therapies sometimes work as a two-edged sword in challenging diabetic complications and male infertility, its one co-morbidity, but none of them are out of side effects. Butylated hydroxytoluene and butylated hydroxyanisole, two major antioxidants, are reported as hepatotoxic and carcinogenic [4]. In developing countries including India, traditional medicine is used widely while in developed countries, the complementary and alternative medicines are more popular [5]. Reasons for success of traditional medicine are easy and cheap along with minimum undesirable effects in respect to chemical drugs. Therefore, choosing an appropriate natural and health-friendly antioxidant having low or no adverse effect for such therapeutic purposes is essential to provide a cafeteria-based choice [6].
Different plant extracts are noticeably found, which are used by couples in developing countries to treat idiopathic infertility, but a few have been studied yet pre-clinically or clinically, considering their promising effects in this concern [7]. Aloe vera (L.) is one of such plants having reputed therapeutic value with medicinal properties counter to aging, inflammation, diabetes, sunburn, immune suppression, cancer, and oxidative stress. Numerous industrial uses for Aloe vera (L.) have started due to its therapeutic potential [8]. There is no information yet on the protective action of Aloe vera (L.) in diabetes-linked sperm cell co-morbidity. A pilot study was conducted regarding the potent extract selection of Aloe vera (L.) for the rectification of testicular abnormalities linked with diabetes, where hydro-ethanol (60:40) extract showed a more promising effect. In this context, spermatozoa of normo-glycemic and diabetic human as well as rat were used for the in-vitro analysis to assess the nature of the direct effect of Aloe vera (L.) enlightening different doses and times of exposure as well as its effect on control samples or not. Such study will expose the possibility and motivation for the conduction of in-vivo experiments on rat models for exploring the mode of action of concerned phytochemical(s) at the molecular level, which will help the pharma industries to develop a drug for this purpose through different levels of clinical trials. Another reason for adoption of this study was to explore the possibility for using this extract for charging sperm samples in connection with potentiating the spermiological sensors prior to in-vitro fertilization for increasing the success rate in this concern.
Materials and Methods
Chemicals
Ethanol was purchased from Changshu Hongsheng Fine Chemicals Co., Ltd. (Changshu city, Jiangu, China). Streptozotocin, sodium citrate, trichloroacetic acid, sodium chloride were purchased from Sisco Research Laboratories Pvt. Ltd. (SRL), India. Other chemicals used in the experiment, supplied by Sigma-Aldrich, Bangalore, India and Loba Chemie Pvt. Ltd. (Maharashtra, India).
Plant Collection
Fully matured leaves of 2–3 years aged Aloe vera (L.) were collected in July–August month from the local nursery of Midnapore, West Bengal, and verified (voucher specimen no. Aloe vera (L.)/VU/Bio/06/19) by the taxonomist of the Department of Botany and Forestry, Vidyasagar University.
Hydro-ethanol Extract Preparation
The gel part of the leaves was separated and pulverized by a grinder. The processed gel of 500 ml was mixed with hydro-ethanol (40:60) at the ratio of 1:2, left for 48 h, and then densed in a rotary evaporator. Subsequently, it was allowed to air dry at room temperature (25-280C) for the collection of the Aloe vera (L.) hydro-ethanol extract (AVHE) in semi-solid form.
Experimental Design
Prior to conduct the experiment, the propose investigation plan cum design was approved by the Institutional Ethics Committee (IEC) having approval no. VU/IAEC-I/DG-1/3–15/19 dated 11/12/19. In-breed, 36 healthy, fertile, and normoglycemic Wistar strain, Rattus norvegicus, male rats, weighing 130 ± 10 g and two months of age were purchased from an authorized vendor. Before starting the experiment, animals were housed in an ambient temperature (25 ± 20C) at normal humidity and a 12-h light/dark controlled room environment for ten days with sufficient water and food supply to acclimatize the animals in such laboratory conditions. After that, 20 rats were made diabetic by a single intramuscular injection of streptozotocin (STZ) in leg muscle at a quantity of 40 mg/kg of body weight. All STZ-injected rats were kept in the above condition for the next seven days to sustain the state of diabetes. This was verified and validated by noting fasting blood glucose (FBG) at an interval of 2 days for the next seven days to develop a chronic diabetic state. The other sixteen rats were left in the same atmospheric condition without STZ injection. The rats were sacrificed after 28 days for the collection of relevant samples by euthanasia followed by cervical dislocation under the guidance of a veterinary doctor to minimize stress imposition for this purpose. The cauda epididymis of each normoglycemic and diabetic rat were dissected and washed in 1 ml of 0.9% normal saline.
Filled-in consent forms, designed after consultation with our university’s medical officer and approved by Institutional Human Ethics Committee (IHEC), were collected from human participants to obtain semen samples. After 3–4 days of restrain from any sexual activity, masturbated semen samples from diabetic and normoglycemic cum control individuals were collected in separate sterilized polystyrene made wide mouth bottles.
Inclusion and Exclusion Criteria of Human and Rat
Streptozotocin-injected rats having FBG levels 250–300 mg/dl were considered as the diabetic group. From the STZ-induced 20 diabetic rats, 16 were included in the diabetes group fulfilling the criteria, and 4 failed to fulfill the said criteria, were excluded. The control group has other 16 acclimatized normoglycemic rats with FBG levels of 70 ± 10 mg/dl.
For the study on human sperm samples, healthy fertile males (25–35 years of age) with an average of ≥ 70% sperm viability, > 20 × 106 sperm/ml of semen, and ≥ 40% grade A sperm motility, have no particular complications such as long-term hyperglycemia, high blood pressure, thyroid abnormalities, or infection in the urinary tract and abstained from addiction to drugs, alcohol, and smoking were considered as inclusion criteria of normoglycemic cum control cum fertile group. Semen samples were collected from such sixteen individuals. Other sixteen individuals (25–35 years of age) with at least two years of diabetic history from the viewpoint of blood glucose after overnight fasting (≥ 200 mg/dl) and HbA1c > 6.5% without other major reproductive complications were included in the diabetes group. Semen having the spontaneous capacity of coagulation followed by reliquefaction at 370C within 1 h was another criterion for human semen sample selection in both normoglycemic and diabetic groups.
Randomisation
Subjects under control and diabetes groups were selected by simple random sampling, covering inclusion and exclusion criteria both in the case of rat and human. Involvement of minimum potential confounders was followed by keeping the animals in the said controlled animal-keeping condition as well as regular monitoring of human subjects.
Blinding of Different Stages of the Experiment
During the allocation of the tissue samples, extract exposure in test tubes for this in-vitro study and data collection, a single-blind study model was followed where the sample handler was unaware of the groups, sub-groups and sub-sub-groups. Only code marks were given and decoding was performed after collection of the data.
Preparation of the In-Vitro Media
Krebs–Ringer bicarbonate (KRB) solution (pH 7.4) was used as an in-vitro medium. The ingredients were sodium chloride, potassium chloride, calcium chloride, sodium bicarbonate and D-glucose, having strengths of 0.12 M, 0.005 M, 0.002 M, 0.025 M, and 0.0055 M mixed with 800 ml of deionized water. The final volume of one liter was adjusted with deionized water.
Blueprint of In-Vitro Study
Each of the human semen samples was mixed with KRB isotonic solution at equal amounts for double dilution. The samples were divided into four groups – AVHE-unexposed control, AVHE-exposed control, AVHE-unexposed diabetes, and AVHE-exposed diabetes. According to the exposure time, each of these groups was divided into two sub-groups i.e. 1 h and 2 h of exposure. Duration dependent AVHE-exposed control and diabetes sub-groups were further subdivided into six sub-sub-groups according to the concentration of the extract i.e. 1, 2 and 4 mg/ml AVHE-exposed control and diabetes.
The epididymal washed rat sperm samples from control and diabetes rat were also double diluted with KRB solution and divided into groups, sub-groups and sub-sub-groups same as human samples.
The samples were allocated as follows for the in-vitro study-
-
AVHE unexposed control: Double diluted epididymal sperm suspension of normoglycemic rat 0.5 ml or processed cum diluted semen of normoglycemic individual 0.5 ml + 10 ml KRB solution + gas mixture supply (30 bubbles/min) for 1 or 2 h.
-
1 mg AVHE-exposed control: Double diluted epididymal sperm suspension of normoglycemic rat 0.5 ml or processed cum diluted semen sample 0.5 ml of normoglycemic individual + 10 ml KRB solution + 10 mg AVHE + gas mixture supply (30 bubbles/min) for 1 or 2 h having extract concentration 1 mg/ml of in-vitro media.
-
2 mg AVHE-exposed control: Normoglycemic rat’s double diluted epididymal sperm suspension of 0.5 ml or processed cum diluted semen of normoglycemic individual 0.5 ml + 10 ml KRB solution + 20 mg AVHE + gas mixture supply (30 bubbles/min) for 1 or 2 h having extract concentration 2 mg/ml of in-vitro media.
-
4 mg AVHE-exposed control: Double diluted epididymal sperm suspension 0.5 ml of normoglycemic rat or 0.5 ml processed cum diluted semen of normoglycemic individual + 10 ml KRB solution + 40 mg AVHE + gas mixture supply (30 bubbles/min) for 1 or 2 h having extract concentration 4 mg/ml of in-vitro media.
-
AVHE-unexposed diabetes: Double diluted epididymal sperm suspension of 0.5 ml of diabetes rat or 0.5 ml processed cum diluted semen of diabetes individual + 10 ml KRB solution + gas mixture (30 bubbles/min) for 1 or 2 h.
-
1 mg AVHE-exposed diabetes: Double diluted epididymal sperm suspension at the volume of 0.5 ml of diabetes rat or 0.5 ml processed cum diluted semen of diabetes individual + 10 ml KRB solution + 10 mg AVHE + gas mixture (30 bubbles/min) for 1 or 2 h having extract concentration 1 mg/ml of in-vitro media.
-
2 mg AVHE-exposed diabetes: Double diluted epididymal sperm suspension of diabetes rat 0.5 ml or processed cum diluted semen 0.5 ml of diabetes individual + 10 ml KRB solution + 20 mg AVHE + gas mixture (30 bubbles/min) for 1 or 2 h having extract concentration 2 mg/ml of in-vitro media.
-
4 mg AVHE-exposed diabetes: Double diluted epididymal sperm suspension of 0.5 ml of diabetes rat or 0.5 ml processed cum diluted semen of diabetes individual + 10 ml KRB solution + 40 mg AVHE + gas mixture (30 bubbles/min) for 1 or 2 h having extract concentration 4 mg/ml of in-vitro media.
Sixteen test tubes were allotted each for AVHE unexposed control sub-group, AVHE exposed control sub-sub-group, AVHE-unexposed diabetes sub-group, and AVHE-exposed diabetes sub-sub-group. So, a total of 256 test tubes for 256 samples covering all sub-sub-groups were considered for this study. All the samples were incubated at 370C for 1 or 2 h with a constant supply of gas mixture, a combination of O2 and CO2 at the ratio of 9.5:0.5, along with the above-mentioned flow rate. After exposure of spermatozoa in the in-vitro solution for the period of 1 or 2 h, one part of the said preparation was used for spermiological sensors analysis instantly. After completion of the 2 h incubation period, the rest part of the said preparation was used for sperm pellet formation and was processed to evaluate catalase and superoxide dismutase activities as well as to quantify thiobarbituric acid reactive substances.
Spermiological Sensors
Sperm Motility and Viability
After scheduled exposure of durations and doses of AVHE, 20 µl in-vitro solution containing sperm cells from allotted test tubes were allowed under microscopic observation (400X) for counting motile sperm as per the standard method [9]. Similarly, viable sperm cells were counted after eosin-nigrosin staining followed by microscopic scanning. The unstained sperm cells were considered as alive cells, and the stained cells were indicated as dead cells. Both motile and viable sperm cell counts were expressed in percentage [9].
For rat, epididymal washed samples were also presented in groups, sub-groups and sub-sub-groups as schedule of human samples. After 1 h or 2 h exposure, the in-vitro samples containing epididymal sperm cells were used for motile and viable sperm count following previous techniques [9].
Acrosomal Intactness Status (AIS)
Human sperm cell suspension in KRB solution from all the condition-specific test tubes were collected separately at the volume of 20 µl, diluted with PBS-D glucose solution at the ratio of 1:20 and used for smear preparation on gelatin-coated glass slides. The slides were incubated at 370C for 2 h. Under microscopic study, the sperm with halo heads were counted and expressed in percentage [9].
Epididymal washed sperm cells from rat of the respective sub-sub-groups after 1 or 2 h of incubation were subjected to microscopic study after processing the samples as human [9].
Plasma Membrane Integrity (PMI) Test
For this assessment, human sperm cells from all the test tubes were exposed to the pre-warmed hypo-osmotic fluid containing 0.735 g citrate salt of sodium and 1.351 g of D (-) fructose in 0.1 L deionized water for 1 h. Microscope observation was made using a 20 µl sample under a coverslip. The spermatozoa with swelled tails were considered as PMI-positive, and the result was presented in percentage value [9].
Sperm cells from epididymal washed fluid of rat after duration and dose-specific exposure were prepared as human samples for the assessment of PMI [9].
Nuclear Chromatin Decondensation (NCD) Cum DNA Fragmentation Test
Part of the KRB solution with human sperm cells of condition-specific sub-sub-groups was centrifuged for one-fourth hour at 1600 g for pellet formation. The pellet was washed twice with 500 mM borate buffer, then exposed to SDS-EDTA (1:9 ratio) mixture, and left for 1 h at 370C. Termination of the reaction was performed by mixing 2.5 g glutaraldehyde in 50 mM borate buffer. Five µl rose bengal (0.80%) was added to 15 µl of the sample and scanned microscopically for counting nucleus decondensed sperms and presented in percentage [10].
Similarly, epididymal washed rat sperm cells of the mentioned groups undergone through same process as human samples for the evaluation of nucleus decondensed sperms and presented in percentage [10].
Oxidative Stress Markers
After completion of the incubation period, the human sperm samples with an in-vitro solution were centrifuged at 3000 g for 10 min at 40C to obtain sperm pellets. Antioxidant enzyme activities of the said pellet were measured [11], and the quantity of thiobarbituric acid reactive substances (TBARS) was assessed following the standard method [11].
In-vitro solution containing sperm cells of rat from different groups, sub-groups and sub-sub-groups were centrifuged separately for pellet formation. The pellets were used for the assessment of oxidative stress markers following standard method as human samples [11].
Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL) for Apoptosis and DNA Fragmentation
After 2 h of incubation, one million human sperm cells from in-vitro media were fixed for 30 min in paraformaldehyde 4% (w/v). Before permeabilization with 2% of Triton X-100, the samples were washed with Hepes A buffer and after permeabilization, two time washing in same buffer for 2 min was performed. A positive (50 U DNase in MgCl2 solution) and negative control (no dUTP) were used. To prepare TUNEL mixture, TdT and FITC-labeled dUTP were added at a ratio of 1:9. In each sample, 50 µl of TUNEL mixture was added and incubated for 1 h at 370 C. All the samples were washed twice with Hepes A buffer and after washing the preparation was resuspended in 500 µl of the same buffer. Five thousand sperm cells were analyzed in each determination. Electronic noise and unwanted debris were excluded by using forward-angle light scatter and side angle light scatter. In the FL1 channel of the flow cytometer (EPICs Profile II, Coulter Electronics, Krefeld, Germany), the FITC-labeled dUTP-positive spermatozoa were quantified [12].
In-vitro solution containing sperm cells from epididymal washed fluid of rat after 2 h of incubation were allowed for TUNEL assay. Sperm cells from different groups, sub-groups and sub-sub-groups of rat were processed in a same way as said earlier [12].
As 1 h of exposure did not focused any remarkable results from pilot study, so 2 h exposed samples were considered here for data collection.
DPPH Scavenging Activity
Dried plant extract was mixed with 2 ml of methanol at a concentration of 10 ppm to 100 ppm. A methanolic solution of 100 µM DPPH was made. A mixture of DPPH solution and plant extract was prepared at the ratio of 1:2 and kept for half an hour in the dark. The absorbance was assessed at 517 nm (UV-Vis spectrophotometer, Thermo Scientific, USA) considering ascorbic acid as gold standard [13].
Qualitative Analysis of Phytomolecule (s)
The qualitative analysis of phytomolecule (s) present in AVHE was conducted biochemically [14].
Estimation of Total Flavonoid and Phenolic Content
Total flavonoid and phenol were estimated by colorimetric method using aluminum chloride and Folin-Ciocalteu reagent, respectively. The standard curve was plotted using quercetin (QAE) for flavonoids and gallic acid (GA) for phenol [15].
Liquid Chromatography-Mass Spectrometry (LC–MS)
The LC–MS study was conducted using the QuattroMicroTMAPI mass spectrometer (Waters, Milford, Massachusetts, USA). Four solvent pumps, a continuous vacuum degasser, a sample injector, and a temperature-controlled column compartment comprise the liquid chromatographic apparatus connected to a multi-wavelength detector. Data was gathered and examined with the help of Waters MASS LYNX 4.1 software. Modification was done in the protocol based on existing literature [16]. The information was gathered via Mass analysis scanning with a scan range of 100–1000 (m/z), a scan length of 0.5 s, and an interscan latency of 0.1 s.
Statistical Analysis
Statistical variance analysis or ANOVA, followed by post-hoc analysis, was conducted to assess significance levels at p < 0.05 [17].
Outcome Measures
For testing the hypothesis of whether the said extract has any ability to rectify the spermiological co-morbidity in diabetes, sixteen samples in each sub-sub-group were considered for confirmation and validation of the hypothesis beyond the routine sample size, which is generally six in such case. This sample size elevation helped us with the reliability, acceptability, and validity of the data by minimizing experimental error and increasing the level of quality control in such a study.
Results
Spermiological Sensors
A significant diminution (p < 0.05) in the motile, viable, PMI and AIS percentages of sperm were observed after 1 and 2 h against 0 h values of AVHE unexposed control sub-groups in human and rat. After 1, 2, and 4 mg AVHE-exposure for 1 and 2 h in control sub-sub-groups, significant (p < 0.05) improvement was noted in all the above said sensors both in human and rat compared to AVHE unexposed duration matched sub-groups (Table 1).
Levels of all tabulated spermiological sensors in both human and rat were decreased significantly after 1 and 2 h of in-vitro incubation in diabetes AVHE unexposed sub-groups compared to the baseline value (0 h). After AVHE exposure to the media at the doses of 1, 2 and 4 mg charged sub-sub-groups resulted significant improvement in all the above sensors of both human and rat sperm samples in comparison to baseline (0 h), 1 and 2 h level of AVHE unexposed diabetes sub-groups (Table 2).
Nuclear Chromatin Decondensation (NCD) Cum DNA Fragmentation Test
Sperm DNA fragmentation was also reflected by NCD study and considered as cytological sensor in this concern. NCD-positive sperm percentage count both in human and rat samples were decreased in AVHE unexposed diabetes at 0, 1 and 2 h of duration extension sub-groups in respect to unexposed control group. After exposure of AVHE in said doses the above sensors in terms of percentage was improved in sub-sub-groups in respect to duration matched AVHE unexposed diabetes sub-groups (Table 3).
Oxidative Stress Marker
In both human and rat sperm pellet, the activities of said antioxidant enzymes were diminished, and the quantity of TBARS was increased significantly (p < 0.05) in AVHE-unexposed diabetes condition compared to the AVHE-unexposed control. After incubation with 1, 2, and 4 mg of AVHE for 2 h, improvements were noted in said parameters significantly (p < 0.05) towards the AVHE-unexposed control. In the case of SOD, the percentage of recovery against the 2 h of AVHE-unexposed diabetes sub-group of human sperm pellet was 23.59% in 1 mg, 23.79% in 2 mg, and 23.92% in 4 mg AVHE exposed diabetes sub-sub-groups. In rat sperm pellet, the percentage of recovery against the 2 h of AVHE-unexposed diabetes sub-group of the rat was 36.12% in 1 mg, 39.16% in 2 mg, and 39.54% in 4 mg AVHE exposed diabetes sub-sub-groups. But no significant (p > 0.05) alteration in SOD activity was noted after 2 h exposure of AVHE in control group of both human and rat at different doses compared to AVHE unexposed control sub-group (Fig. 1A).
In-vitro effect of AVHE exposure for 2 h on the activities of anti-oxidative enzymes and TBARS levels in sperm pellet. A Superoxide dismutase activity, B catalase activity, C TBARS level. Bars are expressed as mean ± SEM, n = 16. ANOVA followed by post-hoc analysis was used. Columns with same superscript did not differ from one another significantly, p > 0.05
The recovery percentage of catalase activity compared to 2 h of AVHE-unexposed diabetes condition in human sperm pellet was 42.87% in 1 mg, 43.48% in 2 mg, 45.67% in 4 mg AVHE exposed diabetes sub-sub-groups, and in rat sperm pellet 36.48% in 1 mg, 38.68% in 2 mg, 38.46% in 4 mg AVHE. There was no significant (p >0.05) difference in catalase activity at different doses of AVHE exposure in control group of human and rat for 2 h against AVHE unexposed control sub-group (Fig. 1B).
The percentage in recovery of TBARS level in human sperm pellet after 2 h was 4.44% in 1 mg, 6.26% in 2 mg, 6.57% in 4 mg AVHE exposed diabetes sub-sub-groups against AVHE unexposed diabetes sub-group. In rat sperm pellet the recovery was 7.06% in 1 mg, 9.44% in 2 mg, 8.83% in 4 mg AVHE exposed diabetes sub-sub-groups against 2 h of AVHE-unexposed diabetes condition. The levels of TBARS recovery were not altered significantly (p > 0.05) among different doses of exposure in AVHE exposed diabetes sub-sub-groups. In AVHE-exposed control sub-sub-groups no significant change was noted in TBARS level compared to AVHE unexposed control sub-groups of human and rat (Fig. 1C).
Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL) Assay
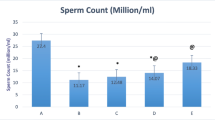
In human sample, about 4.65% of apoptotic sperm cells were observed in AVHE unexposed control sub-group after completion of the incubation period. The said percentage was 23.19% in AVHE unexposed diabetes sub-group and in 1, 2 and 4 mg AVHE exposed sub-sub-groups, the apoptotic cells percentage were 20.25%, 10.72% and 9.34% respectively (Fig. 2A). The same reflection has been presented in flow cytometric map (Fig. 2C).The mean fluorescence intensity showed a significant (p < 0.05) dose-dependent correction in apoptotic cell death after AVHE-exposure in diabetes sub-sub-groups for 2 h in respect to AVHE unexposed diabetes sub-group (Fig. 2E).
Apoptotic sperm cell death of human and rat samples under in-vitro study through TUNEL focusing DNA fragmentation. A apoptotic sperm cell death of human sample in different treatment conditions, B apoptotic sperm cell death of rat samples under various treatment conditions, C flow cytometric map of apoptotic sperm cells of human samples, D apoptotic sperm cells of rat samples through flow cytometric map presentation, E bar diagram of mean fluorescence intensity of fluorescence tagged sperm cells of human sperm samples, F mean fluorescence intensity presentation through column graphics of fluorescence tagged rat sperm samples
The TUNEL assay of rat sperm samples showed 0.01% of apoptotic cell in AVHE unexposed control sub-group whereas AVHE unexposed diabetes sub-group showed 22.64% of apoptotic sperm cell. In 1, 2, and 4 mg AVHE exposed diabetes sub-sub-groups the percentage of apoptotic cells were 16.02%, 14.37% and 7.80% respectively (Fig. 2B). The same nature of apoptotic cell death was reflected in flow cytometric map (Fig. 2D). The mean fluorescence intensity showed a significant (p < 0.05) dose-dependent protection in apoptotic cell death after AVHE exposure diabetes sub-sub-groups (Fig. 2F).
DPPH Scavenging Activity
Concentration-dependent scavenging of DPPH by AVHE was noted. IC50 values of AVHE and ascorbic acid for scavenging DPPH were 34.21 ppm and 15.76 ppm, respectively, focusing on its potent antioxidant activity through the free radical scavenging pathway (Fig. 3).
Qualitative Screening of Phytomolecule(s)
Flavonoids, alkaloids, phenol, and saponins were noted in the qualitative analysis of AVHE (Table 4).
Liquid Chromatography-Mass Spectrometry (LC–MS)
Four bioactive compounds, namely rhamnetin (m/z 316.05, molecular weight 316.05), coumaric acid (m/z 164.66, molecular weight 164.04), caffeic acid (m/z 180.71, molecular weight 180.16), and fumaric acid (m/z 116.47, molecular weight 116.07) were identified from negative ionization mode. Tentative compounds were identified from LC–MS spectrums by manual literature survey [18,19,20,21,22]. Two bioactive compounds, namely thymol (m/z 150.43, molecular weight 150.10) and apigenin (m/z 269.63, molecular weight 270.05), were identified from the positive ionization mode (Table 5) (Fig. 4).
Estimation of Total Flavonoid and Phenolic Content
One gram of Aloe vera (L.) hydro-ethanol extract contained flavonoid 223.20 mg of QAE equivalent and phenolic compound 97.34 mg of GA equivalent, respectively (Table 6).
Discussion
Reports of couples visiting fertility clinics due to difficulties in conceiving and defective spermiological sensors are mushrooming with the increased prevalence of diabetes [23]. Domination of oxidative stress over antioxidative defensive machinery has a great impact on the progression of sub-fertility associated with diabetes has been proved experimentally [11]. Approximately, 30–80% of male infertility cases are correlated with ROS linked spermatozoa damage that results injuries in cell membrane, protein and DNA [24]. Improvisation of antioxidative status through challenging oxidative stress could be an important strategy to overcome the diabetes-related reproductive disturbances. Hyperglycemia induces polyol pathway, protein glycation, advanced glycation end-product generation, and hyperinsulinemia, the main causative factors for the development of subfertility or infertility through oxidative stress imposition [25, 26]. Increased levels of ROS lead to a reduction in the intracellular adenosine triphosphate (ATP) concentration [27], sperm motility and viability [28]. Sperm NCD is an important test to find out the ROS induced effect on sperm fertility capacity. In matured spermatozoa, the chromatin present in condensed form to protect themselves from deteriorating effect of ROS. In diabetes, spermatozoal cells try to protect themselves from ROS and so NCD value is decreased, may one of the explanations. DNA fragmentation is also associated with chromatin condensation-decondensation cyclic process. After in-vitro exposure of the extract, the ROS level in sperm is decreased proved by its anti-oxidant activity that improved the NCD value of sperm. As DNA double strand break is more in condensed state [29] which has been supported here in diabetes by decreasing in NCD sperm cell count. The protective effect of AVHE from DNA fragmentation of sperm cell has been supported here by increasing NCD sperm cell count. Moreover, DNA fragmentation in spermatozoa is clearly correlated with the appearance of oxidative base adducts and chromatin condensation remodeling [30]. Sperm cells apoptosis, DNA fragmentation and sperm mitochondrial ROS have a vicious cycle. Diabetes induced sperm mitochondrial ROS which aggravates sperm cell apoptosis through triggering sperm DNA fragmentation [24] which has been supported here by the results. Moreover, apoptosis linked sperm mitochondrial ROS can aggravate sperm DNA fragmentation by feedback and feed forward processes [31]. The said extract has protective role in sperm ROS generation proved by anti-oxidant enzyme study that overcome diabetes linked spermiological sensors deterioration through rectification of sperm DNA fragmentation and sperm apoptosis, reflected in the results. The decreasing trend in the motility of spermatozoa in diabetes was protected when the male germ cells were incubated in the presence of AVHE at different doses and durations both in human and rat, possibly due to the improved ATP production by oxidative stress management. The possible mechanism may be the protective effects of flavonoids present in the extract, which are thermodynamically capable of minimizing highly oxidizing free radicals by electron donation and thus improve oxidative phosphorylation that leads to boost-up ATP synthesis [32]. High levels of ROS and lipid peroxidation end products alter membrane permeability and integrity, inhibit membrane-bound enzymes, and ultimately decrease the ability of the sperm for capacitation, acrosome reaction, and fusion with the oocyte; three important sequential processes of fertilization have been established and confirmed [33]. Staining of sperm with eosin Y and nigrosine in viability test and hypo-osmotic exposure for PMI test assessed and reflected the deterioration of the physiological state of the sperm plasma membrane in the unexposed diabetes group. A possible explanation for maintaining the integrity of the cell membrane of spermatozoa in AVHE-exposed conditions may be due to the reducing lipid peroxidation through ROS quenching or scavenging effect of the flavonoid and phenolic compounds present in the said extract or inhibiting lipooxygenases that catalyzes the reaction [34, 35]. Literature showed that 1 h of incubation of sperm cells with H202 decreased acrosome integrity [36]. As diabetes is associated with high levels of free radicals and low cytoplasmic antioxidative defense, concomitant loss of acrosome integrity was noted with the advancement of time. The explanation for inhibiting these progressive damages in AVHE-exposed conditions could be made by blocking mitochondrial ROS generation. The structure and function of mitochondria have been known to be protected and defended by phenolic compounds [37]. Blocking ROS generation in mitochondria also interferes the cytochrome-c leakage in sperm cells [38] that improve sperm acrosome status which has been supported here by interference of apoptosis and DNA fragmentation [39]. Direct ROS scavenging activity of the phytomolecule(s) present in AVHE was confirmed by the DPPH assay. Another possible way may be that the phytomolecule(s) may act as an allosteric agonist of the antioxidative enzymes and thus improve the capacity of antioxidative enzyme activities as well as decrease the lipid peroxidation, which was reflected in TBARS levels in all extract-exposed sub-sub-groups [40]. Alternatively, phytomolecule(s) may directly block the genesis of ROS by inhibiting the assembly of NADPH oxidase subunits [41]. This was further supported by the direct protective activity of leaf extract of Capparis spinosa on spermatozoa [42]. These protective activities of AVHE may be the cause of interfering the chain cascade reaction of free radicals that abrogated further deleterious sequel of oxidative injury on fertilizable spermatozoa. The AVHE exposure to control groups has no effect on spermatokinetics at initial cum baseline study (0 h) so not presented in table but the anti-oxidant role of AVHE is focused here by protecting the ROS assault of sperm cell in control state after 1 or 2 h of in-vitro exposure. All the spermiological sensor’s values which have decreased in extract unexposed control group after such period of exposure in respect to 0 h data were protected significantly after the extract exposure to the control group. Analysis of the said results from the perspective of WHO cut off value of spermiological sensors for fertility assessment referred for human and were translated for rat spermiological sensor analysis. The WHO value for motility (40%), viability (≥ 58%) [43], AIS (40%) [44], and PMI (58%) [43] where most of the said sensors were below the cut off level in AVHE unexposed diabetes condition of human and rat which were deteriorated further after 1 and 2 h duration of the exposure. After extract charging at the said doses, a significant protection in such sensors suggesting the defensive ability of the extract from DNA fragmentation cum sperm cell apoptosis and associated spermiological sensors.
Dose- and duration-dependent ameliorative capacities of AVHE focused on the maximal effect being executed at the lowest dose (1 mg/ml) by phytomolecule(s). This may be due to its effect as an agonist of androgen, responsible for the positive regulation of spermiological sensors and inhibiting oxidative stress injuries [45, 46]. The maximal protective effect of AVHE at low dose may be explained through spare receptors. As a result, dose increment (2 and 4 mg/ml) leads to the formation of inactive receptor-ligand complex and or down-regulation of receptors that lower their sensitivity and are unable to implement any further potential cellular response in this concern [47, 48]. The outcome of this experiment may be extrapolated for its application of sperm cell charging of semen samples of infertile male prior to in-vitro fertilization for improving the success rate on the basis of its promising potent anti-oxidative effect on sperm cells. The AVHE is more potent in such rectification compared to other herbal extract like Capparis spinosa from the view point of IC 50 value of free radical scavenging activity, recovery in sperm motility and viability along with the flavonoid and phenol content in this concern [42].
Conclusion
The results highlighted that the phytomolecule(s) present in AVHE have direct defensive action on sperm cells from diabetes-associated oxidative injuries. Instead of a particular antioxidant, the extract could be used as a whole to extend sperm survival of diabetic semen samples. As in-vitro spermiological results for correction of co-morbidity in chronic diabetes by AVHE in rat and human focus the same trend of effect which will help us in the future for conduction of in-vivo study in rat for unfolding the mechanism of action which may be translated to human for developing drug in this purpose as well as for sperm charger in connection with in-vitro fertilization in assisted reproductive technology.
Data Availability
The corresponding author may be communicated for concerned data availability.
Code Availability
Not applicable.
References
Lotti F, Maggi M. Effects of diabetes mellitus on sperm quality and fertility outcomes: clinical evidence. Andrology. 2023;11(2):399–416. https://doi.org/10.1111/andr.13342.
He Z, Yin G, Li QQ, Zeng Q, Duan J. Diabetes mellitus causes male reproductive dysfunction: a review of the evidence and mechanisms. In Vivo. 2021;35(5):2503–11. https://doi.org/10.21873/invivo.12531.
Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues Clin Neurosci. 2018;20(1):41–7. https://doi.org/10.31887/DCNS.2018.20.1/klrooney.
Lourenço SC, Moldão-Martins M, Alves VD. Antioxidants of natural plant origins: from sources to food industry applications. Molecules. 2019;24(22):1–25. https://doi.org/10.3390/molecules24224132.
Debas HT, Laxminarayan R, Straus SE, et al. Complementary and alternative medicine. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease control priorities in developing countries. Washington (DC): The international bank for reconstruction and development / The world bank; 2011. p. 1281–91.
World Health Organization. WHO traditional medicine strategy: 2014–2023. World Health Organization; 2013.
Abarikwu SO, Onuah CL, Singh SK. Plants in the management of male infertility. Andrologia. 2020;52(3):1–22. https://doi.org/10.1111/and.13509.
Maan AA, Nazir A, Khan MKI, Ahmad T, Zia R, Murid M, Abrar M. The therapeutic properties and applications of Aloe vera: a review. J Herb Med. 2018;12:1–10. https://doi.org/10.1016/j.hermed.2018.01.002.
Das P, Mitra D, Jana K, Ghosh D. In vitro study on spermicidal action of hydro-methanol extract of Tinospora cordifolia (Willd.) stem in rat and human sperm: a comparative analysis. Reprod Sci. 2023;30:3480–94. https://doi.org/10.1007/s43032-023-01327-4.
Gopalkrishnan K, Hinduja IN, Anand Kumar TC. In vitro decondensation of nuclear chromatin of human spermatozoa: assessing fertilizing potential. Arch Androl. 1991;27(1):43–50. https://doi.org/10.3109/01485019108987650.
Sarkar R, Ghosh P, Tripathy A, Ghosh D. Correction of diabetes-induced testicular dysfunction by a hydro-methanol (60:40) extract of Curcuma amada rhizomes: a dose-dependent study. J Food Biochem. 2019;43(5):1–13. https://doi.org/10.1111/jfbc.12829.
Oosterhuis GJ, Mulder AB, Kalsbeek-Batenburg E, Lambalk CB, Schoemaker J, Vermes I. Measuring apoptosis in human spermatozoa: a biological assay for semen quality? Fertil Steril. 2000;74(2):245–50.
Rahman MM, Islam MB, Biswas M. In vitro antioxidant and free radical scavenging activity of different parts of Tabebuia pallida growing in Bangladesh. BMC Res Notes. 2015;8:1–9. https://doi.org/10.1186/s13104-015-1618-6.
Hossain MA, AL-Raqmi KA, AL-Mijizy ZH, Weli AM, Al-Riyami Q. Study of total phenol, favonoids contents and phytochemical screening of various leaves crude extracts of locally grown Thymus vulgaris. Asian Pac J Trop Biomed. 2013;3(9):705–10. https://doi.org/10.1016/S2221-1691(13)60142-2.
Bera TK, Chatterjee K, Ghosh D. Alpha glucosidase inhibitory activity of hydro-methanolic (2: 3) extract of seed of Swietenia mahagoni (L.) Jacq. Pharmacognosy J. 2014;6(1):63–9.
Gauri SS, Mandal SM, Atta S, Dey S, Pati BR. Novel route of tannic acid biotransformation and their effect on major biopolymer synthesis in Azotobacter sp. SSB81. J App Microbiol. 2013;114(1):84–95. https://doi.org/10.1111/jam.12030.
Sokal RR, Rohle FJ. Introduction to analysis of variance. In: Sokal RR, Rohle FJ, editors. Biometry. New York: WH Freeman and Company; 1997. p. 179–206.
Mohammed HA, Almahmoud SA, Arfeen M, Srivastava A, El-Readi MZ, Ragab EA, Shehata SM, Mohammed SA, Mostafa EM, El-khawaga HA, Khan RA. Phytochemical profiling, molecular docking, and in vitro anti-hepatocellular carcinoid bioactivity of Suaeda vermiculata extracts. Arab J Chem. 2022;15(7):103950. https://doi.org/10.1016/j.arabjc.2022.103950.
Mahmoudi M, Boughalleb F, Maaloul S, Mabrouk M, Abdellaoui R. Phytochemical screening, antioxidant potential, and LC–ESI–MS profiling of Ephedra alata and Ephedra altissima seeds naturally growing in Tunisia. Appl Biochem Biotechnol. 2023;195:1–13. https://doi.org/10.1007/s12010-023-04370-8.
Mazuecos L, Contreras M, Kasaija PD, Manandhar P, Grąźlewska W, Guisantes-Batan E, Gomez-Alonso S, Deulofeu K, Fernandez-Moratalla I, Rajbhandari RM, Sojka D. Natural Clerodendrum-derived tick repellent: learning from Nepali culture. Exp Appl Acarol. 2023;90:83–98. https://doi.org/10.1007/s10493-023-00804-4.
Tang J, Dunshea FR, Suleria HA. Lc-esi-qtof/ms characterization of phenolic compounds from medicinal plants (hops and juniper berries) and their antioxidant activity. Foods. 2019;9(1):1–25. https://doi.org/10.3390/foods9010007.
Hao J, Li Y, Jia Y, Wang Z, Rong R, Bao J, Zhao M, Fu Z, Ge G. Comparative analysis of major flavonoids among parts of Lactuca indica during different growth periods. Molecules. 2021;26(24):1–13. https://doi.org/10.3390/molecules26247445.
Martins AD, Majzoub A, Agawal A. Metabolic syndrome and male fertility. World J Mens Health. 2019;37(2):113–27. https://doi.org/10.5534/wjmh.180055.
Park YJ, Pang MG. Mitochondrial functionality in male fertility: from spermatogenesis to fertilization. Antioxidants. 2021;10(1):1–24. https://doi.org/10.3390/antiox10010098.
Hiyoshi T, Fujiwara M, Yao Z. Postprandial hyperglycemia and postprandial hypertriglyceridemia in type 2 diabetes. J Biomed Res. 2017;33(1):1–16. https://doi.org/10.7555/JBR.31.20160164.
Tian Y, Song W, Xu D, Chen X, Li X, Zhao Y. Autophagy induced by ROS aggravates testis oxidative damage in diabetes via breaking the feedforward loop linking p62 and Nrf2. Oxid Med Cell Longev. 2020;2020:7156579. https://doi.org/10.1155/2020/7156579.
Ghafarizadeh AA, Malmir M, Naderi Noreini S, Faraji T, Ebrahimi Z. The effect of vitamin E on sperm motility and viability in asthenoteratozoospermic men: in vitro study. Andrologia. 2020;53(1):1–6. https://doi.org/10.1111/and.13891.
Tourmente M, Villar-Moya P, Rial E, Roldan ER. Differences in ATP generation via glycolysis and oxidative phosphorylation and relationships with sperm motility in mouse species. J Biol Chem. 2015;290(33):20613–26. https://doi.org/10.1074/jbc.M115.664813.
Higuchi Y. Chromosomal DNA fragmentation in apoptosis and necrosis induced by oxidative stress. Biochem Pharmacol. 2003;66(8):1527–35. https://doi.org/10.1016/s0006-2952(03)00508-2.
Muratori M, Marchiani S, Tamburrino L, Baldi E. Sperm DNA fragmentation: mechanisms of origin. Adv Exp Med Biol. 2019;1166:75–85. https://doi.org/10.1007/978-3-030-21664-1_5.
Chianese R, Pierantoni R. Mitochondrial reactive oxygen species (ROS) production alters sperm quality. Antioxidants. 2021;10(1):1–19. https://doi.org/10.3390/antiox10010092.
Guthrie HD, Welch GR. Effects of reactive oxygen species on sperm function. Theriogenology. 2012;78(8):1700–8. https://doi.org/10.1016/j.theriogenology.2012.05.002.
Alahmar AT. Role of oxidative stress in male infertility: an updated review. J Hum Reprod Sci. 2019;12(1):4–18. https://doi.org/10.4103/jhrs.JHRS_150_18.
Niki E, Yoshida Y, Saito Y, Noguchi N. Lipid peroxidation: Mechanisms, inhibition, and biological effects. Biochem Biophys Res Commun. 2005;338(1):668–76. https://doi.org/10.1016/j.bbrc.2005.08.072.
Sadik CD, Sies H, Schewe T. Inhibition of 15-lipoxygenases by flavonoids: structure–activity relations and mode of action. Biochem Pharmacol. 2003;65(5):773–81. https://doi.org/10.1016/s0006-2952(02)01621-0.
Bittner-Schwerda L, Malama E, Siuda M, van Loon B, Bollwein H. The sperm chromatin structure assay does not detect alterations in sperm chromatin structure induced by hydrogen peroxide. Anim Reprod Sci. 2022;247:107094. https://doi.org/10.1016/j.anireprosci.2022.107094.
Ďuračka M, Debacker M, Bučko O, Lukač N, Tvrda E. The effect of kaempferol and naringenin may improve the in vitro quality of stored boar semen. J Cent Eur Agric. 2019;20(4):1069–75. https://doi.org/10.5513/JCEA01/20.4.2294.
Asadi A, Ghahremani R, Abdolmaleki A, Rajaei F. Role of sperm apoptosis and oxidative stress in male infertility: a narrative review. Int J Reprod Biomed. 2021;19:493–504. https://doi.org/10.18502/ijrm.v19i6.9371.
Tvrdá E, Debacker M, Ďuračka M, Kováč J, Bučko O. Quercetin and naringenin provide functional and antioxidant protection to stored boar semen. Animals. 2020;10(10):1–16. https://doi.org/10.3390/ani10101930.
Rana S, Dixit S, Mittal A. In silico target identification and validation for antioxidant and anti-inflammatory activity of selective phytochemicals. Braz Arch Biol Technol. 2019;62:e19190048. https://doi.org/10.1590/1678-4324-2019190048.
Yousefian M, Shakour N, Hosseinzadeh H, Hayes AW, Hadizadeh F, Karimi G. The natural phenolic compounds as modulators of NADPH oxidases in hypertension. Phytomedicine. 2019;55:200–13. https://doi.org/10.1016/j.phymed.2018.08.002.
Khojasteh Rad M, Ghani A, Ghani E. In vitro effects of Capparis spinosa L. extract on human sperm function, DNA fragmentation, and oxidative stress. J Ethnopharmacol. 2021;269:1–19. https://doi.org/10.1016/j.jep.2020.113702.
World Health Organization. WHO laboratory manual for the examination and processing of human semen. 6th ed. Geneva: World Health Organization press. New York, NY: Cambridge University Press; 2021. pp. 9–246.
Chan PJ, Corselli JU, Jacobson JD, Patton WC, King A. Spermac stain analysis of human sperm acrosomes. Fertil Steril. 1999;72:124–8. https://doi.org/10.1016/s0015-0282(99)00201-0.
Omu AE. Sperm Parameters: Paradigmatic index of good health and longevity. Med Princ Pract. 2013;22:30–42. https://doi.org/10.1159/000354208.
Zhang L, Wu S, Ruan Y, Hong L, Xing X, Lai W. Testosterone suppresses oxidative stress via androgen receptor-independent pathway in murine cardiomyocytes. Mol Med Rep. 2011;4(6):1183–8. https://doi.org/10.3892/mmr.2011.539.
Neubig RR, Spedding M, Kenakin T, Christopoulos A. International union of pharmacology committee on receptor nomenclature and drug classification. XXXVIII. Update on terms and symbols in quantitative pharmacology. Pharmacol Rev. 2003;55(4):597–606. https://doi.org/10.1124/pr.55.4.4.
Homer LD, Nielsen TB. Spare receptors, partial agonists, and ternary complex model of drug action. Am J Physiol Endocrinol Metab. 1987;253(1):E114–21. https://doi.org/10.1152/ajpendo.1987.253.1.E114.
Acknowledgements
The authors are grateful to the Department of Science & Technology, Govt of India (GOI) for funding this project (Project no: DST/INSPIRE Fellowship/2018/IF180939). Special thanks to Dr. Kishalay Jana, District Epidemiologist of Paschim Midnapore, West Bengal, for his valuable suggestions and immense support during sample collection.
Author information
Authors and Affiliations
Contributions
Dibya Pal conducted the project, methodology, data analysis and drafted the original manuscript. Data curation and animal handling was performed by Dipanwita Mitra. Project administration and data analysis was done by Sukriti Hazra. Debidas Ghosh supervised, conceptualized the study design, and edited and validated the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The Institutional Ethics Committee (IEC) approved the experimental design conducted on rat and human, having the approval number VU/IAEC-I/DG-1/3–15/19. Animal handling and treatment protocol for diabetes induction were executed according to the guidelines of the Committee for Control and Supervision of Experiments on Animals (CCSEA), Govt. of India.
Consent to Participate
Filled-in consent forms by the candidates were collected to obtain semen samples.
Consent to Publication
All authors read and approved the final manuscript.
Conflict of Interest
No conflict of interest from our side.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pal, D., Mitra, D., Hazra, S. et al. Protective Effect of Aloe vera (L.) on Diabetes-Induced Oxidative Stress Linked Spermiological Co-Morbidity in Human and Rat: An In-Vitro Analysis. Reprod. Sci. 31, 2685–2699 (2024). https://doi.org/10.1007/s43032-024-01605-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-024-01605-9