Abstract
In vitro spermatogenesis and xenotransplantation of the immature testicular tissues (ITT) are the experimental approaches that have been developed for creating seminiferous tubules-like functional structures in vitro and keeping the integrity of the ITTs in vivo, respectively. These strategies are rapidly developing in response to the growing prevalence of infertility in adolescent boys undergoing cancer treatment, by the logic that there is no sperm cryopreservation option for them. Recently, with the advances made in the field of tissue engineering and biomaterials, these methods have achieved promising results for fertility preservation. Due to the importance of extracellular matrix for the formation of vascular bed around the grafted ITTs and also the creation of spatial arrangements between Sertoli cells and germ cells, today it is clear that the scaffold plays a very important role in the success of these methods. Decellularized extracellular matrix (dECM) as a biocompatible, functionally graded, and biodegradable scaffold with having tissue-specific components and growth factors can support reorganization and physiologic processes of originated cells. This review discusses the common protocols for the tissue decellularization, sterilization, and hydrogel formation of the decellularized and lyophilized tissues as well as in vitro and in vivo studies on the use of the testis-derived dECM for testicular organoids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spermatogenesis is the process that takes place in the seminiferous tubules of the testis, by which sperm cells are produced from spermatogonial stem cells (SSCs) [1, 2]. This process starts at puberty and continues throughout adulthood [1]. The fertility of children undergoing chemotherapy or radiotherapy for pediatric cancers or preconditioning therapies before bone marrow transplantation is severely reduced when they become adults [3]. Sperm cryopreservation is routinely used for post-pubertal patients, but in peripubertal boys who do not have any mature sperm, cryopreservation of immature testicular tissues(ITT) is the only alternative for preservation of fertility [4, 5]. This infertility is due to the loss of SSCs when exposed to cytotoxic agents. Therefore, to prevent prepubertal germ cell loss and subsequent infertility, cryopreservation of testicular tissues containing SSCs has been accepted as the gold standard protocol before oncological treatments in some centers in Europe and the USA [3]. The approaches include in vitro spermatogenesis, SSC transplantation, and testicular tissue grafting have been followed by researchers to restore male fertility in peripubertal boys using cryopreserved ITTs [6, 7]. Autotransplantation of frozen-thawed gonadal tissues has presented a significant option for restoration purposes as approved by over 100 live births worldwide using autotransplantation of the frozen-thawed ovarian cortex [8]. Autotransplantation of gonadal tissues has commonly applied only in the cases where there is no risk of retransmission of cancer cells to the cured patient, such as patients undergoing bone marrow transplantation for nonmalignant diseases like hemoglobinopathies [3]. Xenotransplantation of ITTs to nude mice, which is at a preclinical stage has presented another method suitable for those who suffer from malignant diseases [9,10,11]. However, further studies should be focused on the important loss of germ cells following transplantation due to hypoxia/reoxygenation injuries [10, 12, 13]. Different protocols based on tissue engineering approaches have been followed to limit these events, such as ITTs encapsulation in fibrin hydrogel, alginate, or using a combination of hydrogel and growth factors like vascular growth factor [14,15,16,17]. On the other hand, the three-dimensional culture of testicular cells in vitro is another option for sperm production from testicular tissue samples [3]. Since in the structure of seminiferous tubules, germ cells are immersed in the cytoplasm of Sertoli cells, and both of these cells interact with the matrix and the cells around the seminiferous tubules, such a structure cannot be reconstructed with two-dimensional cultures [2]. Therefore, three-dimensional culture has become the main focus of the researches to investigate in vitro spermatogenesis using cryopreserved ITTs. Accordingly, encapsulation of testicular cells in 3D condition using synthetic or biologically-derived matrices such as fibrin [18], matrigel [19], collagen [20], alginate [21], and agarose [22,23,24,25] has been studied to provide a condition that mimics the extracellular matrix (ECM). Today, the ECM derived from tissue decellularization, considering its multiple functions has emerged as one of the biomaterials for tissue engineering [26]. This review summarizes the methods used to decellularize tissues and obtain ECM, as well as their use in testicular tissue engineering (Fig. 1). Accordingly, a combination of the following terms without time limitation was applied to search the articles performed on PubMed: [(tissue decellularization) (179) AND (fertility) AND (restoration OR preservation)] [12]. Scientific video protocols [6], reviews [26], guidelines [10], irrelevant articles [27], articles in languages other than English [10], and articles focusing on female fertility [7] were excluded.
The schematic diagram of the use of extracellular matrix for fertility preservation in adolescent boys suffering from cancer. The ECM resulting from tissue cellularization can be used in two ways: 1 encapsulation of testicular cells in the decellularized extracellular matrix and 2 xenotransplantations of testicular tissue fragments embedded in the decellularized extracellular matrix
Decellularization, Sterilization, and Gel Formation of ECM-Derived Decellularized Tissues
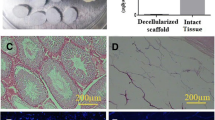
To prevent immune reaction and inflammation, tissue-derived material which are used for tissue engineering or transplantation should be decellularized. Therefore, chemical, enzymatic, physical decellularization methods have been developed to obtain dECM [28] (Fig. 2). These procedures can maintain the composition and architecture of ECM, similar to the original tissue [28]. Quantifying the DNA content of dECM is currently used as a significant tool to evaluate the effectiveness of these protocols in the removal of cellular debris [29]. Chemical agents which are used to solubilize cell membranes are detergents. One of the most common detergents used in decellularization processes is Triton X-100 targeting the lipid-lipid and lipid-protein interactions [30, 31]. It is very useful in cells removal, especially in those tissues where the key components of ECM are primarily proteins despite the limitation of that in decellularization of tissues with high content of glycosaminoglycans (GAGs) [32]. Sodium dodecyl sulfate (SDS) can also be used as a detergent with Triton but with more efficiency in solubilizing cell membranes. The main side effects of using SDS are related to the degradation of proteins that will change their structure and function, therefore, it is necessary to limit the duration of using SDS in the decellularization protocols [33, 34]. Enzymes are also applied in most decellularization protocols. Of course, the process of removing enzymes after the decellularization process, as well as the side effects that they can have on the structure and function of the tissue should not be ignored [35]. Trypsin attacking the C-side bonds in arginine and lysine can be used along with a breaking agent of cell–matrix interactions such as EDTA [36]. Of note, changes in the structure of ECM due to the removal of proteins such as laminin, and removing GAGs have been observed in cases of prolonged exposure to trypsin–EDTA treatment [37, 38]. Pepsin is another enzyme used for long-term with low-concentration in decellularization protocols [39]. Exposing cells to osmotic pressure using hypoosmotic and hyperosmotic solutions can be an effective way to disintegrate cells. Of course, it should be noted that in this method, the cellular residues can still be attached to the extracellular matrix. Accordingly, this method can be used as a complementary method with detergents [40, 41]. Freeze-thawing of tissues is The most commonly used physical technique in eliminating cells. This is done by forming ice crystals and then disrupting the plasma membranes which makes it a useful method for tissues that have a loose extracellular matrix structure [41]. Finally, it needs to be mentioned that a combination of these methods should be used to optimize decellularization, since, in a recent study, pre-frozen-thawed pig testicular tissues were exposed to hypoosmotic and hyperosmotic solutions and detergents [42]. Today, for sterilization, physical and chemical protocols are used to remove pathogens from the extracellular matrix, especially when they are to be used in vivo. In using this method, exposure time, preservation of matrix structure, and pathogen removal efficiency should be considered [43]. Physical protocols can be divided into two categories: heat and irradiation techniques. The use of the heat method is limited because it causes changes in the structure of the protein, but the irradiation method with gamma rays or ultraviolet light is more efficient such that gamma rays are used as an optimal method for sterilizing medical products today. Liquid chemicals such as alcohol, peracetic acid, and aldehydes are included in the list of chemical methods for sterilizing extracellular matrix [44]. In addition to altering the structure of the protein, these substances can be toxic. Therefore, they should be removed as much as possible after sterilization [45, 46]. After sterilization, the dECM is lyophilized for further application and then ground through a mixer mill. One of the methods of postprocessing of the dECM is gel formation. Gel formation of the dECM makes it is easily injected into the injury site and the matrix is formed based on the shape of the lesion [47]. In addition, it can include tissue-specific cells into the matrix in the laboratory and form three-dimensional structures, or it can be implanted inside the body [48]. To obtain the gel, the lyophilized and ground dECM is digested with an enzymatic agent, most often pepsin in an acidic condition (approximately Ph ~ 2) with continuous agitation from 24 to 48 h. Then, the pH and salt concentration of the solution is adjusted to physiological state, which is an aqueous solution at 4 °C, but it becomes gel at 37 °C [49].
Application of the dECM-Derived Testis Tissues: In Vitro Spermatogenesis
One of the goals of researchers working in male infertility is to produce mature sperm from the clinic from testicular cell suspensions cultured in vitro, which can be applicable in assisted reproductive techniques (reviewed in [50]). Today, due to the progress of medical treatments such as bone marrow transplantation for malignancy, hereditary and metabolic diseases, and infertility complications resulting from these treatments, methods of maintaining fertility using in vitro sperm maturation have received more and more attention [6, 51]. Tissue culture and two-dimensional culture of testicular cell suspension have been considered the primary methods used to produce in vitro mature sperm [52]. The two-dimensional culture contributed to the understanding of cellular and molecular mechanisms controlling the differentiation and proliferation of spermatogonia, but this method had low efficiency in spermatozoon cell production [2]. Unlike two-dimensional culture, testicular tissue culture was most successful in producing sperm, eventually producing a live mouse offspring using assisted reproductive techniques [27, 53,54,55]. The tissue culture method showed that the unique arrangement of testicular cells is necessary to promote spermatogenesis in vitro; hence studies shifted to three-dimensional cultures and approaches such as scaffold-free and scaffold-based cultures to configure testicular cells in vitro were considered [2, 56]. Scaffold-free approaches using methods such as hanging drops and cellular aggregates showed less meiotic progression than scaffold-based approaches [57]. Hydrogel-based scaffolds have been used to reorganize testicular cells. Hydrogels are substances that can absorb large amounts of water, a feature that greatly facilitates the transport of nutrients, gasses, and cellular wastes [58]. In addition, they can provide mechanical support for the cells embedded in them [59]. Today, hydrogels are divided into synthetic and natural (Table 1). Synthetic hydrogels form a network with high mechanical strength but instead have less biological activity[60]. Natural hydrogels can have a protein or polysaccharide structure [61]. Natural hydrogels with a polysaccharide structure provide a more stable mechanical network over time for cultured cells but biologically lack binding ligands to react with the cells [62]. Studies have shown that testicular cells in a polysaccharide-based natural hydrogel have produced many haploid cells from SSCs [21]. However, it should be noted that new products such as RGD peptide-binding alginate have been developed today that have enhanced the biological properties of alginate by binding the cell to RGD-ligand [63]. Therefore, the use of modified alginate to support spermatogenesis can be an exciting research goal. Hydrogels with protein structures such as collagen, hyaluronic acid, fibrin, and decellularized native tissue-derived ECM have been used in in vitro spermatogenesis studies to create three-dimensional cultures of testicular cells and have better results than three-dimensional studies [64].
These types of hydrogels are biologically active and can interact with cells through a surface receptor and play an essential role in the spatial arrangement of the cells, but because of their protein structure, they are gradually affected by enzymes secreted by cells. They are digested or deformed gradually, resulting in a change in the original network structure, finally leading to a weak mechanical structure [20, 65]. Therefore, for long-term culture, using this type of hydrogels cannot be a good option. Today, for the stability of polymer filaments of the protein-based hydrogels, different chemical cross-linkers such as glutaraldehyde [66], EDC(1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide)-NHS(N-hydroxysuccinimide) [67], and genipin [68] have been used, which create a covalent bond between the filaments and can help their stability and prevent their enzymatic digestion. Decellularized tissue-derived hydrogels are protein-based natural hydrogels that contain all the extracellular matrix components, such as hyaluronic acid, fibrin, laminin, collagen, and glycosaminoglycans [48]. Due to having a variety of extracellular proteins, these types of hydrogels are closer to the physiological state [69]. Organoids today refer to the use of extracellular matrices such as hydrogels to form three-dimensional structures in vitro, which can mimic many of the properties of the considered tissue [70]. In addition to having extracellular components, the tissue-derived matrix contains growth factors and tissue-specific cytokines that can control cell differentiation and proliferation [71, 72]. Today, testicular organoids have been used in studies as a tool to study the controlling mechanisms of germ cell niches and their role in infertility, the cytotoxic effects of drugs, and to produce fertilization-competent spermatozoa in vitro [64]. The testicular organoids are a combination of Sertoli, germ, and Leydig cells embedded in an extracellular matrix such as matrigel or testicular tissue-derived extracellular matrix to arrange the cells into structures such as seminiferous tubules [73]. It is thought that the extracellular matrix of testicular tissue can be effective in rearranging testicular cell suspension. In this regard, the first study using culture of adult human testicular cells on fragments of the decellularized testicular tissue was done and found that the scaffolds can help establish and maintain the spermatogonia niche. However, seminiferous tubules-like structures s were not formed [74]. Another study using cultured pig testicular suspension on decellularized testicular slices found that these scaffolds could not reorganize testicular cells into tubule-like structures [71]. Reorganization of the immature rat testicular cells to a seminiferous tube-like arrangement was achieved using matrigel hydrogel [75], while another study found that such structures were not in the suspension of adult human testicular cells embedded in a testicular tissue-derived hydrogel [75]. Therefore, the determining factor in forming a true testicular organoid seems to be the maturation status of testicular cells, not the type of extracellular matrix. In order to determine the impact of the maturation status of testicular cells on the efficiency of testicular organoid formation, the studies have been conducted using immature testicular cells and showed that immature testicular cells of humans, monkeys, and mice can form tubular-like structures [73]. Another factor that affects the formation of testicular organoids is the number of cells used for each organoid. The higher the cell concentration, the more testicular cord-like architectures appear [42, 57, 75, 76]. In addition to these factors, the effect of scaffold or matrix to support organoid formation is discussed [64]. Table 2 lists the studies that used natural or testicular matrix-derived hydrogels to form testicular organoids. Given the advantages of tissue-derived hydrogels, there are still very few studies comparing the effect of this type of hydrogel with other hydrogels such as matrigel on organoid formation. Therefore, according to the above, today, the testicular organoid is widely used in studies to investigate the pathogenesis and morphogenesis of testicular tissue, drug toxicity, and also as a tool to restore fertility (Table 2). In this regard, one of the components of organoids is scaffolding, which is used for this purpose from natural hydrogels such as collagen, matrigel, or hydrogels derived from testicular tissue [64]. Testicular tissue-derived hydrogels can be prioritized due to their biological advantages; accordingly, it seems that the use of this type of hydrogel will be more common in future studies.
Application of the dECM-Derived Testis Tissues: Xenotransplantation of ITTs
Several studies have shown that complete spermatogenesis is obtained using grafting autologous transplantation and xenotransplantation of ITTs in other species, and even offsprings have been achieved by these techniques [86,87,88,89,90]. Additionally, the success of the autotransplantation technique of frozen-thawed ovarian cortex has shown that it is a clinically efficient protocol since about 100 live births have been reported with this method [8]. However, to date, no complete spermatogenesis has been observed using xenotransplantation of human ITTs to nude mice. The failure of such a method has been attributed to the severe reduction in the number of germ cells and the poor integrity of the seminiferous tubules [10, 91]. Various factors have been mentioned in connection with massive germ cells loss following transplantation of human ITTs to nude mice, including hypoxia injuries due to the lack of blood supply around the grafted tissues [12], the phylogenetic differences between species [92], and significant difference between host environment and that of donor tissue in terms of both endocrine and paracrine factors [93]. In a review of the literature, we find that methods such as tissue encapsulation in biomaterials [14, 94], growth factors administration such as vascular endothelial growth factor [14, 95, 96], and adding anti-apoptotic agents [13, 97, 98] to accelerate blood supply and maintain the survival of germ cells have yielded promising results. Biomaterials such as collagen, fibrin, and alginate, acting as a scaffold, improve the migration of host endothelial and fibroblast cells to the grafted area [14, 99]. The results of these studies suggest that tissue-derived extracellular matrix with having substances such as laminin and fibronectin (essential components for building new blood vessels) is effective in creating a vascular substrate that leads to reduction of germ cell loss due to hypoxia. On the other hand, the dECM provides inhibitory signals of apoptosis by providing interaction with the grafted tissue cells. Despite these advantages, no studies have been reported on the use of the dECM in xenotransplantation of ITTs. This knowledge gap could be addressed in future studies.
Conclusion
Today, in US centers, nearly 74% of parents of boys under the age of 12, diagnosed with an oncological disease, want to receive the services of fertility preservation. Accordingly, freezing of ITTs is performed as a strategy to maintain fertility before starting cancer treatment in many infertility centers in Europe and the US. The existence of such testicular tissues banks has put a lot of pressure on researchers and clinicians in infertility centers to meet the expectations of parents who have been received fertility preservation procedures. The strategies we itemized for fertility restoration need to be updated by the new sciences especially tissue engineering. The testis-derived dECM has several benefits such as growth factor, fibrous structure and cell attachment can regulate organization, differentiation, and survival of the testicular cells. The dECM can also be combined with other biomaterials or drugs to optimize techniques of in vitro spermatogenesis and xenotransplantation. In addition, promising results can be achieved in future studies when proteins existing in the extracellular matrix due to their active groups on their surface are conjugated with nanoparticles or nanocapsules containing certain drugs or factors.
Abbreviations
- ITT:
-
Immature testicular tissues
- dECM:
-
Decellularized extracellular matrix
- SSCs:
-
Spermatogonial stem cells
- ECM:
-
Extracellular matrix
- GAGs:
-
Glycosaminoglycans
- DTM:
-
Decellularized testicular matrix
References
Ibtisham F, Wu J, Xiao M, An L, Banker Z, Nawab A, et al. Progress and future prospect of in vitro spermatogenesis. Oncotarget. 2017;8(39):66709–27.
Stukenborg J-B, Schlatt S, Simoni M, Yeung C-H, Elhija MA, Luetjens CM, et al. New horizons for in vitro spermatogenesis? An update on novel three-dimensional culture systems as tools for meiotic and post-meiotic differentiation of testicular germ cells. 2009;15(9):521–9.
Goossens E, Jahnukainen K, Mitchell R, Van Pelt A, Pennings G, Rives N, et al. Fertility preservation in boys: recent developments and new insights. 2020;2020(3):hoaa016.
Del Vento F, Vermeulen M, De Michele F, Giudice MG, Poels J, Des Rieux A, et al. Tissue engineering to improve immature testicular tissue and cell transplantation outcomes: one step closer to fertility restoration for prepubertal boys exposed to gonadotoxic treatments. 2018;19(1):286.
Gholami K. Experimental approaches for fertility preservation in prepubertal boys undergoing oncological therapy. 2020.
Wyns C, Kanbar M, Giudice MG, Poels JJHru. Fertility preservation for prepubertal boys: lessons learned from the past and update on remaining challenges towards clinical translation. 2021;27(3):433–59.
Giudice MG, De Michele F, Poels J, Vermeulen M, Wyns CJScr. Update on fertility restoration from prepubertal spermatogonial stem cells: how far are we from clinical practice? 2017;21:171–7.
Demeestere I, Simon P, Dedeken L, Moffa F, Tsépélidis S, Brachet C, et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. 2015;30(9):2107–9.
Wyns C, Curaba M, Martinez-Madrid B, Van Langendonckt A, François-Xavier W, Donnez JJHr. Spermatogonial survival after cryopreservation and short-term orthotopic immature human cryptorchid testicular tissue grafting to immunodeficient mice. 2007;22(6):1603–11.
Goossens E, Geens M, De Block G, Tournaye HJF, sterility. Spermatogonial survival in long-term human prepubertal xenografts. 2008;90(5):2019–22.
Sato Y, Nozawa S, Yoshiike M, Arai M, Sasaki C, Iwamoto TJHr. Xenografting of testicular tissue from an infant human donor results in accelerated testicular maturation. 2010;25(5):1113–22.
Van Eyck A-S, Jordan BF, Gallez B, Heilier J-F, Van Langendonckt A, Donnez JJF, et al. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. 2009;92(1):374–81.
Poels J, Abou-Ghannam G, Herman S, Van Langendonckt A, Wese F-X, Wyns CJFis. In search of better spermatogonial preservation by supplementation of cryopreserved human immature testicular tissue xenografts with N-acetylcysteine and testosterone. 2014;1:47.
Poels J, Abou-Ghannam G, Decamps A, Leyman M, des Rieux A, Wyns CJJoCR. Transplantation of testicular tissue in alginate hydrogel loaded with VEGF nanoparticles improves spermatogonial recovery. 2016;234:79–89.
Del Vento F, Vermeulen M, Ucakar B, Poels J, des Rieux A, Wyns CJIjoms. Significant benefits of nanoparticles containing a necrosis inhibitor on mice testicular tissue autografts outcomes. 2019;20(23):5833.
Del Vento F, Poels J, Vermeulen M, Ucakar B, Giudice MG, Kanbar M, et al. Accelerated and improved vascular maturity after transplantation of testicular tissue in hydrogels supplemented with VEGF-and PDGF-loaded nanoparticles. 2021;22(11):5779.
Del Vento F, Vermeulen M, Poels J, Wyns C, editors. Encapsulation of mice immature testicular tissue in alginate supplemented with nanoparticles delivering a necrosis inhibitor improved spermatogonial survival and seminiferous tubule integrity in autografts. Human Reproduction. Oxford: Oxford Univ Press; 2019
Stukenborg J-B, Jahnukainen K. In vitro spermatogenesis and its potential clinical implication for patients. Genetics of Human Infertility. 21: Karger Publishers; 2017. p. 162–72.
Lee J-H, Gye MC, Choi KW, Hong JY, Lee YB, Park D-W, et al. In vitro differentiation of germ cells from nonobstructive azoospermic patients using three-dimensional culture in a collagen gel matrix. 2007;87(4):824–33.
Lee JH, Kim HJ, Kim H, Lee SJ, Gye MCJB. In vitro spermatogenesis by three-dimensional culture of rat testicular cells in collagen gel matrix. 2006;27(14):2845–53.
Baert Y, Dvorakova-Hortova K, Margaryan H, Goossens EJB. Mouse in vitro spermatogenesis on alginate-based 3D bioprinted scaffolds. 2019;11(3):035011.
Huleihel M, Nourashrafeddin S, Plant TM. Application of three-dimensional culture systems to study mammalian spermatogenesis, with an emphasis on the rhesus monkey (Macaca mulatta). Asian J Androl. 2015;17(6):972.
Gholami K, Pourmand G, Koruji M, Ashouri S, Abbasi MJScr, therapy. Organ culture of seminiferous tubules using a modified soft agar culture system. 2018;9(1):249.
Gholami K, Pourmand G, Koruji M, Sadighigilani M, Navid S, Izadyar F, et al. Efficiency of colony formation and differentiation of human spermatogenic cells in two different culture systems. 2018;18(4):397–403.
Jabari A, Gilani MAS, Koruji M, Gholami K, Mohsenzadeh M, Khadivi F, et al. Three-dimensional co-culture of human spermatogonial stem cells with Sertoli cells in soft agar culture system supplemented by growth factors and Laminin. 2020;122(5):151572.
Farmani AR, Nekoofar MH, Ebrahimi Barough S, Azami M, Rezaei N, Najafipour S, et al. Application of platelet rich fibrin in tissue engineering: focus on bone regeneration. 2021;32(2):183–8.
Sato T, Katagiri K, Gohbara A, Inoue K, Ogonuki N, Ogura A, et al. In vitro production of functional sperm in cultured neonatal mouse testes. 2011;471(7339):504–7.
Mendibil U, Ruiz-Hernandez R, Retegi-Carrion S, Garcia-Urquia N, Olalde-Graells B, Abarrategi AJIJoMS. Tissue-specific decellularization methods: rationale and strategies to achieve regenerative compounds. 2020;21(15):5447.
Hernandez MJ, Yakutis GE, Zelus EI, Hill RC, Dzieciatkowska M, Hansen KC, et al. Manufacturing considerations for producing and assessing decellularized extracellular matrix hydrogels. 2020;171:20–7.
Cartmell JS, Dunn MGJJoBMRAOJoTSfB, The Japanese society for biomaterials, biomaterials TASf, Biomaterials tKSf. Effect of chemical treatments on tendon cellularity and mechanical properties. 2000;49(1):134–40.
Woods T, Gratzer PFJB. Effectiveness of three extraction techniques in the development of a decellularized bone–anterior cruciate ligament–bone graft. 2005;26(35):7339–49.
Luo Z, Bian Y, Su W, Shi L, Li S, Song Y, et al. Comparison of various reagents for preparing a decellularized porcine cartilage scaffold. 2019;11(3):1417.
Chen R-N, Ho H-O, Tsai Y-T, Sheu M-TJB. Process development of an acellular dermal matrix (ADM) for biomedical applications. 2004;25(13):2679–86.
Schmitt A, Csiki R, Tron A, Saldamli B, Tübel J, Florian K, et al. Optimized protocol for whole organ decellularization. 2017;22(1):1–9.
Giraldo-Gomez D, Leon-Mancilla B, Del Prado-Audelo M, Sotres-Vega A, Villalba-Caloca J, Garciadiego-Cazares D, et al. Trypsin as enhancement in cyclical tracheal decellularization: morphological and biophysical characterization. 2016;59:930–7.
Caralt M, Uzarski JS, Iacob S, Obergfell KP, Berg N, Bijonowski BM, et al. Optimization and critical evaluation of decellularization strategies to develop renal extracellular matrix scaffolds as biological templates for organ engineering and transplantation. 2015;15(1):64-75.
Waletzko J, Dau M, Seyfarth A, Springer A, Frank M, Bader R, et al. Devitalizing effect of high hydrostatic pressure on human cells—influence on cell death in osteoblasts and chondrocytes. 2020;21(11):3836.
Rieder E, Kasimir M-T, Silberhumer G, Seebacher G, Wolner E, Simon P, et al. Decellularization protocols of porcine heart valves differ importantly in efficiency of cell removal and susceptibility of the matrix to recellularization with human vascular cells. 2004;127(2):399-405.
Poon CJ, Cotta MVPE, Sinha S, Palmer JA, Woods AA, Morrison WA, et al. Preparation of an adipogenic hydrogel from subcutaneous adipose tissue. 2013;9(3):5609-20.
Cheng J, Wang C, Gu YJB. Combination of freeze-thaw with detergents: a promising approach to the decellularization of porcine carotid arteries. 2019;30(2):191-205.
Cornelison R, Wellman S, Park J, Porvasnik S, Song Y, Wachs R, et al. Development of an apoptosis-assisted decellularization method for maximal preservation of nerve tissue structure. 2018;77:116-26.
Vermeulen M, Del Vento F, Kanbar M, Pyr dit Ruys S, Vertommen D, Poels J, et al. Generation of organized porcine testicular organoids in solubilized hydrogels from decellularized extracellular matrix. 2019;20(21):5476.
Tao M, Ao T, Mao X, Yan X, Javed R, Hou W, et al. Sterilization and disinfection methods for decellularized matrix materials: review, consideration and proposal. 2021;6(9):2927–45.
Somers P, Cuvelier CA, Somer FD, Cornelissen M, Cox E, Verloo M, et al. Gamma radiation alters the ultrastructure in tissue-engineered heart valve scaffolds. 2009;15(11):3597-604.
Yaldiz B, Saglam-Metiner P, Cam SB, Korkusuz P, Yesil-Celiktas OJTJoSF. Effect of sterilization methods on the mechanical stability and extracellular matrix constituents of decellularized brain tissues. 2021:105299.
White LJ, Keane TJ, Smoulder A, Zhang L, Castleton AA, Reing JE, et al. The impact of sterilization upon extracellular matrix hydrogel structure and function. 2018;2:11-20.
Giobbe GG, Crowley C, Luni C, Campinoti S, Khedr M, Kretzschmar K, et al. Extracellular matrix hydrogel derived from decellularized tissues enables endodermal organoid culture. 2019;10(1):1-14.
Claudio-Rizo JA, Delgado J, Quintero-Ortega IA, Mata-Mata JL, Mendoza-Novelo BJH. Decellularized ECM-derived hydrogels: modification and properties. 2018;1.
Gaetani R, Aude S, DeMaddalena LL, Strassle H, Dzieciatkowska M, Wortham M, et al. Evaluation of different decellularization protocols on the generation of pancreas-derived hydrogels. 2018;24(12):697-708.
Reuter K, Schlatt S, Ehmcke J, Wistuba JJS. Fact or fiction: in vitro spermatogenesis. 2012;2(4):245-52.
Kanbar M, De Michele F, Giudice MG, Desmet L, Poels J, Wyns CJHR. Long-term follow-up of boys who have undergone a testicular biopsy for fertility preservation. 2021;36(1):26-39.
Oliver E, Stukenborg JBJA. Rebuilding the human testis in vitro. 2020;8(4):825-34.
Sato T, Katagiri K, Kojima K, Komeya M, Yao M, Ogawa TJPo. In vitro spermatogenesis in explanted adult mouse testis tissues. 2015;10(6):e0130171.
Komeya M, Kimura H, Nakamura H, Yokonishi T, Sato T, Kojima K, et al. Long-term ex vivo maintenance of testis tissues producing fertile sperm in a microfluidic device. 2016;6(1):1-10.
Yokonishi T, Sato T, Komeya M, Katagiri K, Kubota Y, Nakabayashi K, et al. Offspring production with sperm grown in vitro from cryopreserved testis tissues. 2014;5(1):1-6.
Edmondson R, Broglie JJ, Adcock AF, Yang LJA. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. 2014;12(4):207-18.
Yokonishi T, Sato T, Katagiri K, Komeya M, Kubota Y, Ogawa TJBor. In vitro reconstruction of mouse seminiferous tubules supporting germ cell differentiation. 2013;89(1):15, 1–6.
Nelson SR, Zhang C, Roche S, O’Neill F, Swan N, Luo Y, et al. Modelling of pancreatic cancer biology: transcriptomic signature for 3D PDX-derived organoids and primary cell line organoid development. 2020;10(1):1–12.
Zhang W, Huang G, Xu FJFiB, Biotechnology. Engineering biomaterials and approaches for mechanical stretching of cells in three dimensions. 2020;8.
Saydé T, El Hamoui O, Alies B, Gaudin K, Lespes G, Battu SJN. Biomaterials for three-dimensional cell culture: from applications in oncology to nanotechnology. 2021;11(2):481.
Liu Y, Hsu S-hJFic. Synthesis and biomedical applications of self-healing hydrogels. 2018;6:449.
Varaprasad K, Jayaramudu T, Kanikireddy V, Toro C, Sadiku ERJCp. Alginate-based composite materials for wound dressing application: a mini review. 2020;236:116025.
Kaczmarek-Pawelska A. Alginate-based hydrogels in regenerative medicine. Alginates-recent uses of this natural polymer: IntechOpen; 2019.
Kanbar M, Vermeulen M, Wyns CJR. Organoids as tools to investigate the molecular mechanisms of male infertility and its treatments. 2021;161(5):R103-R12.
Kusindarta DL, Wihadmadyatami HJTr. The role of extracellular matrix in tissue regeneration. 2018;65.
Nair M, Best SM, Cameron REJAS. Crosslinking collagen constructs: achieving cellular selectivity through modifications of physical and chemical properties. 2020;10(19):6911.
Lee J, Edwards H, Pereira C, Samii SJJoMSMiM. Crosslinking of tissue-derived biomaterials in 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide (EDC). 1996;7(9):531–41.
Výborný K, Vallová J, Kočí Z, Kekulová K, Jiráková K, Jendelová P, et al. Genipin and EDC crosslinking of extracellular matrix hydrogel derived from human umbilical cord for neural tissue repair. 2019;9(1):1-15.
Zhang W, Du A, Liu S, Lv M, Chen SJRT. Research progress in decellularized extracellular matrix-derived hydrogels. 2021;18:88-96.
Lee HJ, Mun S, Pham DM, Kim PJABS, Engineering. Extracellular matrix-based hydrogels to tailoring tumor organoids. 2021.
Vermeulen M, Del Vento F, De Michele F, Poels J, Wyns CJIjoms. Development of a cytocompatible scaffold from pig immature testicular tissue allowing human Sertoli cell attachment, proliferation and functionality. 2018;19(1):227.
Pendergraft SS, Sadri-Ardekani H, Atala A, Bishop CEJBoR. Three-dimensional testicular organoid: a novel tool for the study of human spermatogenesis and gonadotoxicity in vitro. 2017;96(3):720-32.
Sakib S, Uchida A, Valenzuela-Leon P, Yu Y, Valli-Pulaski H, Orwig K, et al. Formation of organotypic testicular organoids in microwell culture. 2019;100(6):1648-60.
Baert Y, De Kock J, Alves-Lopes JP, Söder O, Stukenborg J-B, Goossens EJSCR. Primary human testicular cells self-organize into organoids with testicular properties. 2017;8(1):30-8.
Alves-Lopes JP, Söder O, Stukenborg J-BJB. Testicular organoid generation by a novel in vitro three-layer gradient system. 2017;130:76-89.
Zhang J, Hatakeyama J, Eto K, Abe S-iJG, endocrinology c. Reconstruction of a seminiferous tubule-like structure in a 3 dimensional culture system of re-aggregated mouse neonatal testicular cells within a collagen matrix. 2014;205:121–32.
Strange DP, Zarandi NP, Trivedi G, Atala A, Bishop CE, Sadri-Ardekani H, et al. Human testicular organoid system as a novel tool to study Zika virus pathogenesis. 2018;7(1):1-7.
Goldsmith TM, Sakib S, Webster D, Carlson DF, Van der Hoorn F, Dobrinski IJC, et al. A reduction of primary cilia but not hedgehog signaling disrupts morphogenesis in testicular organoids. 2020;380(1):191-200.
Bhang DH, Kim B-J, Kim BG, Schadler K, Baek K-H, Kim YH, et al. Testicular endothelial cells are a critical population in the germline stem cell niche. 2018;9(1):1-16.
Huleihel M, Nourashrafeddin S, Plant TMJAjoa. Application of three-dimensional culture systems to study mammalian spermatogenesis, with an emphasis on the rhesus monkey (Macaca mulatta). 2015;17(6):972.
Abofoul-Azab M, Lunenfeld E, Levitas E, Zeadna A, Younis JS, Bar-Ami S, et al. Identification of premeiotic, meiotic, and postmeiotic cells in testicular biopsies without sperm from Sertoli cell-only syndrome patients. 2019;20(3):470.
Elhija MA, Lunenfeld E, Schlatt S, Huleihel MJAjoa. Differentiation of murine male germ cells to spermatozoa in a soft agar culture system. 2012;14(2):285.
Stukenborg JB, Wistuba J, Luetjens CM, Elhija MA, Huleihel M, Lunenfeld E, et al. Coculture of spermatogonia with somatic cells in a novel three‐dimensional soft‐agar‐culture‐system. 2008;29(3):312-29.
Movassagh SA, Movassagh SA, Dehkordi MB, Pourmand G, Gholami K, Talebi A, et al. Isolation, identification and differentiation of human spermatogonial cells on three-dimensional decellularized sheep testis. 2020;122(8):151623.
Legendre A, Froment P, Desmots S, Lecomte A, Habert R, Lemazurier EJB. An engineered 3D blood-testis barrier model for the assessment of reproductive toxicity potential. 2010;31(16):4492–505.
Shinohara T, Inoue K, Ogonuki N, Kanatsu-Shinohara M, Miki H, Nakata K, et al. Birth of offspring following transplantation of cryopreserved immature testicular pieces and in-vitro microinsemination. 2002;17(12):3039-45.
Jahnukainen K, Ehmcke J, Nurmio M, Schlatt SJCr. Autologous ectopic grafting of cryopreserved testicular tissue preserves the fertility of prepubescent monkeys that receive sterilizing cytotoxic therapy. 2012;72(20):5174-8.
Honaramooz A, Snedaker A, Boiani M, Schöler H, Dobrinski I, Schlatt SJN. Sperm from neonatal mammalian testes grafted in mice. 2002;418(6899):778-81.
Ohta H, Wakayama TJBor. Generation of normal progeny by intracytoplasmic sperm injection following grafting of testicular tissue from cloned mice that died postnatally. 2005;73(3):390-5.
Liu J, Cheng KM, Silversides FGJBor. Production of live offspring from testicular tissue cryopreserved by vitrification procedures in Japanese quail (Coturnix japonica). 2013;88(5):124, 1-6.
Schlatt S, Honaramooz A, Ehmcke J, Goebell P, Rübben H, Dhir R, et al. Limited survival of adult human testicular tissue as ectopic xenograft. 2006;21(2):384-9.
Wyns C, Wese F-X, Donnez J, Van Langendonckt A, Curaba MJTJoU. Long-term spermatogonial survival in cryopreserved and xenografted immature human testicular tissue editorial comment. 2009;181(5):2249.
Kuhn HE, Frontera MA, Demers LM, Bartholomew MJ, Lloyd TAJAJoDoC. The onset of sperm production in pubertal boys: relationship to gonadotropin excretion. 1989;143(2):190-3.
Chiti MC, Dolmans M-M, Donnez J, Amorim CJAobe. Fibrin in reproductive tissue engineering: a review on its application as a biomaterial for fertility preservation. 2017;45(7):1650-63.
Tian R, Yang S, Zhu Y, Zou S, Li P, Wang J, et al. VEGF/VEGFR2 signaling regulates germ cell proliferation in vitro and promotes mouse testicular regeneration in vivo. 2016;201(1):1–13.
Schmidt JA, de Avila JM, McLean DJJBor. Effect of vascular endothelial growth factor and testis tissue culture on spermatogenesis in bovine ectopic testis tissue xenografts. 2006;75(2):167-75.
Navid S, Rastegar T, Baazm M, Alizadeh R, Talebi A, Gholami K, et al. In vitro effects of melatonin on colonization of neonate mouse spermatogonial stem cells. 2017;63(6):370-81.
Gholami M, Saki G, Hemadi M, Khodadadi AJIjobms. Effect of melatonin on the expression of apoptotic genes in vitrified-thawed spermatogonia stem cells type A of 6-day-old mice. 2013;16(8):906.
Najjar M, Manzoli V, Abreu M, Villa C, Martino MM, Molano RD, et al. Fibrin gels engineered with pro‐angiogenic growth factors promote engraftment of pancreatic islets in extrahepatic sites in mice. 2015;112(9):1916-26.
Acknowledgements
The authors thank all the staff members of the Urology Research Center, especially, Zeinab Ahadi for conceiving and generating the figure.
Author information
Authors and Affiliations
Contributions
Keykavos Gholami performed the literature review and wrote the manuscript. Somayeh Solhjoo participated in the review of the literature. Seyed Mohammad Kazem Aghamir was responsible for the critical review of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Gholami, K., Solhjoo, S. & Aghamir, S.M.K. Application of Tissue-Specific Extracellular Matrix in Tissue Engineering: Focus on Male Fertility Preservation. Reprod. Sci. 29, 3091–3099 (2022). https://doi.org/10.1007/s43032-021-00823-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00823-9