Abstract
Decreased oxygen availability in sojourners requires adjustments in tissue oxygen supply, the most effective of which is an increase in the hemoglobin (Hb) concentration. It is achieved by two independent processes: a fast increase in Hb is achieved by decreasing plasma volume due to enhanced renal Na- and water excretion. A further but slow increase in Hb concentration is achieved by stimulation of erythropoiesis by mechanisms depending on stabilization of hypoxia-inducible factor 2α resulting in elevated levels of erythropoietin in blood. The magnitude of decrease in plasma volume and of stimulation of erythropoiesis depends on the degree and duration of exposure to hypoxia at high altitude. Upon descent from high to low altitude elevated O2-transport capacity is no longer needed. Thus, plasma volume can be restored and excess erythrocytes can be removed from circulation. This latter process is called erythrolysis. Its effectiveness seems to depend on the altitude to which individuals had been exposed. Whereas most of the excess erythrocytes seem to be removed from circulation within 1–2 weeks after a stay at altitudes > 3500 m, total Hb mass seems to remain elevated for up to 4 weeks when individuals had been exposed to more moderate altitudes, e.g. in the range of 2500 m. These are the altitudes where athletes typically perform altitude training. Thus, it appears that improved performance in the weeks after return from altitude training depends in part on maintaining elevated total Hb mass, which is known to increase aerobic capacity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxia at high altitude (HA) impairs tissue oxygen supply and compromises cellular functions. Lowlanders ascending to HA without any pre-acclimatization are most affected, and they usually do not tolerate altitudes > 4000 m very well in the sense that their maximal exercise performance is considerably decreased in comparison to performance at low altitude [24], which is indicated by decreased VO2max [8]. The loss in VO2max is even more pronounced in athletes than in untrained. Increased ventilation, increased oxygen affinity of hemoglobin (Hb), increased cardiac output and altered tissue perfusion, and elevated Hb concentration and hematocrit are some of the most important mechanisms of adjustments to high altitude hypoxia [6]. Despite of some acclimatization, maximal exercise performance remains hampered because normal oxygen partial pressure in arterial blood (PaO2) cannot be restored and impaired oxygen diffusion from blood to tissues persists [8]. Lowlanders travelling to high altitude are much more affected than high altitude natives, which is demonstrated best by less pronounced deterioration in high altitude-natives than in lowlanders within the first days and even weeks of their sojourns [7]. In addition, maladaptation and susceptibility increase the prevalence to suffer from high altitude-related illnesses such as acute mountain sickness (AMS) [2] and high altitude pulmonary edema (HAPE) [56]. This indicates that complete adaptation to hypoxia may require life-long residence and even residence at high altitude of many generations [4], resulting in genetic selection and complex patterns of adjustments, one of which is an increase in the Hb concentration and total Hb mass (totHb).
This review will focus on mechanisms and kinetics of increasing the Hb concentration and tot-Hb during exposure to high altitude hypoxia, which allows transport of a larger amount of oxygen by blood in compensation for decreased oxygen saturation in arterial blood (SaO2). It will also discuss kinetics and possible mechanisms to normalize Hb upon descent from high altitude when the increased oxygen carrying capacity is no longer needed. This aspect is of great significance for athletic performance after returning from altitude training because increased totHb is one of the determinants of improved aerobic capacity [50].
Increase in Hb Concentration in Lowlanders Ascending to High Altitude
The oxygen partial pressure (PO2) of inspired air is lowered at high altitude in proportion with the decrease in barometric pressure. As indicated in Fig. 1a, which summarizes means of adaptation to hypoxia, a decrease in arterial PO2 is sensed by carotid bodies, which generate signals stimulating alveolar ventilation. Hyperventilation at HA slightly raises the alveolar PO2 at the expense of decreased arterial partial pressure of CO2 [63] resulting in respiratory alkalosis. Elevated pH increases SaO2 because of an increase in the oxygen affinity of Hb [29]. However, the degree of hyperventilation to a defined hypoxic stimulus varies considerably among individuals, where those with the lowest ventilatory response to hypoxia (HVR) are the least hypoxia-tolerant indicated by increased susceptibility to high altitude pulmonary edema (HAPE) [21], maybe also to AMS [3]. Sojourners to HA also show pronounced hypoxic pulmonary vasoconstriction [58], which favors filtration of fluid into the alveolar space and causes subclinical [12] and even full-blown HAPE with massively impaired trans-alveolar oxygen diffusion [57]. Even after long-term sojourns, lowlanders do not acquire the improved gas exchange observed in native highlanders [13], and consequently lowlanders have to cope with decreased arterial oxygen loading indicated by decreased SaO2. Compensation by increasing cardiac output is insufficient. Thus, besides adjustments at the tissue level, which are incompletely understood, the only means of improving the amount of oxygen delivered to peripheral tissues remains to be an increase in the oxygen carrying capacity (Fig. 1b). This might involve an increase in the concentration of Hb in blood by increasing the hematocrit (Hct), i.e. a decrease in plasma volume, as well as an increase in the totHb due to stimulated erythropoiesis.
Oxygen transport in blood. a The amount of oxygen transported from the lungs to peripheral tissues depends on arterial oxygen loading, transport to the tissues, and unloading from Hb. Arterial oxygen content (CaO2) is thus determined by the oxygen affinity of Hb (Hb-O2-affinity), which affects SO2 at any given PO2, on arterial PO2, which is a function of alveolar ventilation, and by the concentration of Hb determined by erythropoiesis and plasma volume. The amount of oxygen delivered to peripheral tissues depends on tissue blood flow and oxygen unloading. Blood flow is a function of cardiac output and local control of tissue perfusion (Q), while the amount of oxygen unloaded from Hb depends on tissue PO2 and again on Hb-O2-affinity and, therefore, oxygen consumption can be calculated from blood flow and the arterio-to-venous difference in blood oxygen content (CaO2–CvO2) (after Bouverot [6]). b Examples indicating the magnitude of increase in the Hb concentration in blood to maintain stable arterial oxygen content despite decreased arterial SO2 in high altitude hypoxia
One gram of Hb binds 1.34 mL of oxygen [29]. It can, therefore, be calculated how much the Hb-concentration in blood has to increase to compensate for decreased SaO2 as indicated in Fig. 1b. As an example, the decreased arterial oxygen content caused by a decrease in SaO2 from 95 to 90% upon ascent to an altitude of approximately 2500 m can be compensated by an increase in the Hb concentration by 1 g/dL. Ascent to higher altitudes requires a more pronounced increase in Hb concentration (Fig. 1b). This response has been reported as early as 1890 by Viault [60], who showed a progressive increase in the number of erythrocytes in blood with continued stay at high altitude in the Andes.
Two mechanisms account for increasing the Hb concentration at high altitude: One is a decrease in plasma volume which occurs within a few days of exposure to high altitude [52], and a second, much slower mechanism, is an increase in tot-Hb in the circulation by stimulation of erythropoiesis [40, 49].
Decrease in Plasma Volume (PV) at High Altitude
A decrease in PV upon ascent to high altitude has long been recognized [31]. Its degree depends on the absolute altitude and the duration of the sojourn (summary in [49]). Literature indicates a decrease in PV within a few days after ascent [19], which reaches stable values of approximately 10% below normal at altitudes between 2900 and 4000 m, but decreases further by more than 25% at altitudes above 4000 m [41, 52]. Literature on PV-changes at high altitude appears controversial: Some studies indicate a nearly complete recovery of PV after spending > 3 months at high altitude [41], and there are also reports on an increase. Although the literature is not entirely clear, it appears that the reduction in PV and in total extracellular water is blunted by exercise [32]. Exercise like hill-walking has been shown to significantly increase PV [34]. Thus, studies using passive ascent to high altitude often report on a pronounced decrease in PV, whereas in physically active individuals such as in athletes performing altitude training, this decrease may not occur (e.g. [30]).
The primary mechanism causing the water loss at high altitude seems to be an impaired activity of the renin–angiotensin–aldosterone system that increases renal Na- and water excretion [32, 33]. A significant contribution might also come from decreased glomerular plasma flow [37]. Other contributors might be increased fractional Na-excretion because of increased levels of atrial natriuretic peptide [36] and osmotic water loss due to stimulated bicarbonate excretion, which occurs in compensation of hyperventilation-induced respiratory alkalosis [52]. Other, so far not well understood mechanisms might contribute as well [52].
The physiological consequence of a moderately increased Hct is a profound increase in tissue oxygen supply. This positive effect is explained by the increased amount of oxygen that can be delivered per stroke volume or with cardiac output. Thus, a combination of increased Hb-concentration with increased cardiac output and tissue blood flow is a powerful tool compensating for decreased SaO2 at high altitude. However, it is well recognized that massively elevated Hct increases blood viscosity and may cause stroke and thrombosis.
Erythropoiesis at High Altitude
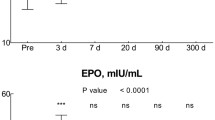
Hypoxia stimulates erythropoiesis, which affects both the Hb concentration and totHb in circulating blood. Erythropoiesis is stimulated by an elevation of erythropoietin (EPO) levels in blood in response to stabilization of hypoxia-induced transcription factor HIF-2α [18]. EPO then acts as an anti-apoptotic growth factor preventing premature death of erythroid precursor cells in the bone marrow [64]. EPO levels in blood follow a distinct pattern upon ascent to high altitude: a pronounced increase can be observed within a few hours after exposure to hypoxia, which is then followed by a sharp decrease to considerably lower levels, which are, however, higher than normoxic EPO levels. Both, initial peak and steady state EPO levels depend on the degree of hypoxia [64]. Despite this rapid increase in EPO and rapidly stimulated Hb synthesis indicated by increased iron-turnover [18, 22], it takes weeks to months to produce significant amounts of new erythrocytes and to increase totHb.
The magnitude of the increase in totHb depends on absolute altitude and duration of stay. Rasmussen et al. performed a meta-analysis that included studies with subjects spending their time continuously in hypoxia. But they also included studies on intermittent hypoxia as often applied in sleep-high-train-low altitude training modalities [40]. Both groups show quite similar responses. Results indicate that one has to spend approximately 4–9 weeks at an altitude of ~ 2000 m to increase totHb by 5%. In contrast, the same gain can be achieved by spending ~ 3 weeks at an altitude of 3500 m [40]. Gravican et al. [16] used a different approach to estimate the time and altitude required to increase totHb by introducing a measure of “altitude-kilometers × hours-at-altitude”. According to this analysis a 5% increase in totHb could be achieved by 1500 km × h, which might e.g. be 31 days at 2000 m or 18 days at an altitude of 3500 m.
There is great variability in the erythropoietic response to HA, and there are even “non-responders” [9]. This aspect is of particular importance in athletes, who chose training at HA to improve aerobic performance [9], where the availability of iron might restrict stimulation of erythropoiesis. Wachsmuth et al. [61] showed that total Hb increased in most of the highly competitive swimmers during a 3-weeks training in the Sierra Nevada (2320 m), and that changes were similar in males and females. It is of note that these changes by altitude training occur on top of an already increased totHb in well-trained athletes [23], a result that has been confirmed many times thereafter (for review see [49]). Interestingly, no change in totHb was observed in athletes who could not participate in the training program at altitude because of injury or other illness but who still spent the time in the high-altitude training camp. There is the possibility, of course, that a persisting state of inflammation might have negatively affected erythropoiesis by IL-6 and hepcidin dependent reduction in iron availability [20]. These results indicate that the effectiveness of the altitude training on totHb might not only depend on exposure to high altitude hypoxia alone but also requires the additional stress of exercise in this environment. Mechanisms and interactions are not fully understood.
Decrease in Hb Upon Return from High Altitude
Neither increased Hb concentration nor increased totHb is needed any longer after descending from high altitude, because inspired PO2 and SaO2 are now high enough to result in high arterial oxygen loading and oxygen unloading to tissue by steep oxygen gradients. Any excess Hb could, therefore, be removed from circulation. This mechanism might be beneficial because it reduces strain on the cardio-vascular system. Another advantage is a decreased requirement for iron. By contrast, maintaining elevated totHb might be of advantage because it improves aerobic capacity and thus aerobic exercise performance at low altitude [50].
Destruction of Erythrocytes in Normoxia
The average life-span of mature erythrocytes is 100–130 days. In normoxia, destruction of senescent erythrocytes amounts to approximately 0.5% of the entire erythrocyte mass per day, which is balanced by a stable rate of production of erythrocytes of approximately 160 × 106 erythrocytes per minute. Senescent erythrocytes are typically removed by the reticulo-endothelial system (RES), mainly in the spleen, where cells are tested for deformability and resistance to metabolic depletion and are sequestered “if they don’t pass the test” [43]. Also, loss of the surface expression of CD47, CD55, and CD59, which protect mature erythrocytes from being attacked by the complement system, contributes to their removal both by the RES and by circulating macrophages.
Random hemolysis of pre-senescent erythrocytes is normally negligible in humans but amounts to 0.5–1% per day in mice and rat [25]. It can be increased by mechanical strain such as muscle contraction and various other maneuvers increasing the shear stress (for review see [28]).
Destruction of Erythrocytes in Hypoxia
It is of note that erythrocytes formed in hypoxia appear to have a shortened life span likely because of increased random hemolysis and/or accelerated senescence [15]. By contrast, a normal erythrocyte life-span has been shown in a small group of highlanders [5]. In rodents, erythrocytes formed by stress erythropoiesis seem to have impaired survival because a doubling of the erythrocyte production rate was related to a 3.5% reduction in survival of erythrocytes [25].
Time Course of Decrease in Hb Concentration and totHb After Return from High Altitude
Results from the literature indicate that Hb actually decreases faster upon descent from high altitude than expected from just decreasing the rate of erythrocyte production, but results on the time course are conflicting. Decreased erythrocyte production rates are indicated by a decrease in the number of reticulocytes both after descent from moderate [16] and high altitude [31, 38]. Upon descent, EPO in plasma was decreased dramatically and sometimes even fell well below pre-altitude levels [16, 42]. Besides, the incorporation of injected 59Fe was significantly reduced in highlanders after descent to sea level, which indicates a decreased rate of heme-synthesis and erythropoiesis [22].
All studies agree in showing a decrease in Hb concentration and Hct within a few days after return from high altitude (> 3500 m) to low altitude, regardless of the altitude to which they had acclimatized (e.g. [16, 31, 51]). This rapid decrease in Hb concentration is mainly explained by an increase in plasma volume since ANP decreases and impaired function of the renin–angiotensin–aldosterone system and tubular Na-reabsorption is restored [51]. Results on renal Na- and water handling upon return from moderate altitude are less clear.
The time course of the decrease in Hb upon descent seems to depend on the altitude. A slow decrease in totHb in the course of several weeks has been observed upon return from a stay at moderate altitude (< 2700 m) [39, 61, 62]. The elevation in totHb persisted for at least 2 weeks after descent, and pre-altitude totHb levels were reached approximately 4–5 weeks after descent [16]. In contrast, rapid decrease in totHb within at most 10 days has been observed when polycythemic subjects descended from altitudes > 4000 m [42].
Markers of erythrocyte destruction were elevated in subjects after descending from high altitude. Increased exhaled carbon monoxide (CO) [11] and elevated CO-Hb [51] has been interpreted to indicate increased activity of heme-oxygenase and thus breakdown of erythrocytes and heme. It is possible, however, that increased CO is the result of inflammation, which might occur by increased levels of free oxygen radicals upon reoxygenation. However, increased values of biliverdin and, bilirubin, and of a decrease in haptoglobin in blood have also been observed after descent [31]. Those are end-products of the heme-oxygenase reaction. Therefore, their elevation might also indicate accelerated breakdown of Hb and thus the destruction of erythrocytes [31, 42, 44, 45].
Erythrolysis or Neocytolysis?
Erythrolysis is the non-selective loss off erythrocytes of all degrees of senescence. In contrast, neocytolysis refers to the selective destruction of erythrocytes formed newly during hypoxia upon return to normoxia. It is unclear, however, which fraction of erythrocytes is destroyed upon descent from high altitude. Many authors applied the term “neocytolysis” to the descent-related destruction of erythrocytes although it has never been demonstrated that selectively neocytes had been destroyed [31, 38, 51, 1, 45]. Risso et al. reported that the population of youngest cells had been missing upon descent from high altitude indicated by altered distribution of erythrocytes after density gradient centrifugation [44]. This result is in support of the neocytolysis-hypothesis. It might also be explained by decreased release of reticulocytes from the bone marrow because of reduced erythropoietic activity, and by altered cell density due to shifts in cell water. Thus, direct experimental proof is lacking, and the more appropriate term to describe this process is erythrolysis as it had been applied by several authors [31, 38, 51].
Mechanisms of Accelerated Erythrocyte Destruction
Results obtained on human erythrocytes on the mechanisms causing erythrocyte destruction upon return to low altitude are sparse. It had been found that erythrocyte fractions of different age had acquired a “senescent phenotype” indicated by decreased levels of expression of CD47, CD55, and CD59. Loss of these proteins indicates increased susceptibility to phagocytosis by macrophages [44]. The expression of these proteins seems to depend on the presence of EPO because EPO-treatment of patients with renal anemia increased the expression of CD47, CD55, and CD59 [35].
There is also evidence that survival of reticulocytes and young erythrocytes might depend on the presence of elevated levels of EPO [59]. It has been shown on a small group of subjects that loss of reticulocytes seems not to occur when subjects were treated with EPO upon descent to prevent the EPO decrease [59].
In a mouse model of neocytolysis, Song et al. [53] found that reticulocytes produced during exposure to hypoxia had a decreased activity of catalase, which was caused by elevated miR-21. This enzyme protects from damage by H2O2. Upon return to normoxia, reticulocytes produce more H2O2 and are damaged, because of the lack of defense mechanisms causing cell lysis. This report might indicate that the process of erythrocyte destruction after exposure to hypoxic might in fact be selective for neocytes produced during hypoxia, and thus the term neocytolysis appears justified. A different mechanism of impaired resilience to oxidants has also been proposed: Rogers et al. showed that deoxygenation of Hb altered erythrocyte metabolism and decreased the reduction potential [47]. However, in contrast to the mouse model this mechanism is independent of erythrocyte age and should thus put all erythrocytes in danger of oxidative damage and lysis. In this case, the process of cell destruction would be nonselective and should thus be called erythrolysis.
Significance For Athletic Performance
The totHb in circulating blood is a major determinant of aerobic exercise performance indicated by a highly significant correlation between VO2max and totHb [50], because an increased totHb increases the total amount of oxygen on blood allowing for improved oxygen supply to exercising skeletal muscle. Although an increased Hb concentration and hematocrit also increase blood oxygen carrying capacity in arterial blood [29], Hb concentration does not correlate significantly with VO2max [50]. This is likely due to increased blood viscosity and impaired micro-circulation.
Many elite athletes live and perform their training in hypoxia, staying there permanently or intermittently following a “sleep-high-train-low” strategy (e.g. [14, 26, 27, 48, 54]). The major goal is to improve performance at low altitude [55]. The altitude relevant for training is a compromise between restricted performance due to hypoxia at high altitude and a hypoxic dose high enough to allow for adjustments of erythropoiesis and other cellular functions that might be of advantage for training and competition. Most often, altitude ranges between 2000 and 2700 m are used.
Often the mechanisms causing an improvement in performance are not fully understood. One important parameter is an increase in totHb. Garvican et al. [17] and Rassmussen et al. [40] summarized the time that needs to be spent at altitude to achieve a significant increase in totHb. It is of importance to note that not everybody increases totHb, which classifies a population into non-responders and responders [9].
There seems to be great inter-individual variability in the optimal time of return from altitude on performance in training and competition, and it is not entirely clear how long a potential beneficial effect might last [10, 39, 46].
Taken together, training at high altitude induces adaptive mechanisms, which can be utilized either for improved performance in a competition that is performed within a few weeks upon return from an altitude training camp, but certainly also allows for improved effectiveness of training in normoxia.
Summary and Conclusion
Hypoxia at high altitude increases the Hb concentration in blood by decreasing the plasma volume within the first few days of exposure. This increase is absolutely required to compensate for the acute decrease in SaO2 particularly at altitudes > 4000 m where SaO2 can decrease to below 80% in some individuals. During a longer sojourn at high altitude, totHb also increases while plasma volume might still remain reduced. Whereas the higher Hb concentration increases the amount of oxygen transported per stroke volume, the higher totHb allows for improved oxygen flux to peripheral tissues without the need of restriction of supply to less active tissue and organs.
Upon return from high to low altitude elevated Hb concentration and totHb are no longer needed. Thus, it is useful to decrease elevated values, in particular when the increase was well pronounced after prolonged stay at altitudes > 3500 m. The decrease appears to be slower after acclimatization to moderate altitudes. The slower destruction rate of erythrocytes after acclimatization to moderate altitude might be of advantage for athletes because they benefit from increased totHb by increasing aerobic capacity, which allows for improved performance in training and competition.
References
Alfrey CP, Rice L, Udden MM, Driscoll TB. Neocytolysis: physiological down-regulator of red-cell mass. Lancet. 1997;349(9062):1389–90. https://doi.org/10.1016/S0140-6736(96)09208-2(PubMed PMID: 9149714).
Bärtsch P, Swenson ER. Clinical practice: acute high-altitude illnesses. N Engl J Med. 2013;368(24):2294–302. https://doi.org/10.1056/NEJMcp1214870(PubMed PMID: 23758234).
Bärtsch P, Swenson ER, Paul A, Julg B, Hohenhaus E. Hypoxic ventilatory response, ventilation, gas exchange, and fluid balance in acute mountain sickness. High Altit Med Biol. 2002;3(4):361–76. https://doi.org/10.1089/15270290260512846PubMed PMID: 12631422.
Beall CM. Andean, Tibetan, and Ethiopian patterns of adaptation to high-altitude hypoxia. Integr Comp Biol. 2006;46(1):18–24.
Berlin NI, Reynafarje C, Lawrence JH. Red cell life span in the polycythemia of high altitude. J Appl Physiol. 1954;7(3):271–2.
Bouverot P. Adaptation to altitude hypoxia in vertebrates. Berlin: Springer Verlag; 1985.
Brutsaert TD. Do high-altitude natives have enhanced exercise performance at altitude? Appl Physiol Nutr Metab. 2008;33(3):582–92. https://doi.org/10.1139/h08-009(Epub 2008/05/08. PubMed PMID: 18461115).
Calbet JA, Boushel R, Radegran G, Sondergaard H, Wagner PD, Saltin B. Why is VO2 max after altitude acclimatization still reduced despite normalization of arterial O2 content? Am J Physiol. 2003;284(2):R304–16. https://doi.org/10.1152/ajpregu.00156.2002.
Chapman RF, StrayGundersen J, Levine BD. Individual variation in response to altitude training. J Appl Physiol. 1998;85(4):1448–56.
Chapman RF, Laymon Stickford AS, Lundby C, Levine BD. Timing of return from altitude training for optimal sea level performance. J Appl Physiol. 2014;116(7):837–43. https://doi.org/10.1152/japplphysiol.00663.2013PubMed PMID: 24336885.
Christensen RD, Lambert DK, Henry E, Yaish HM, Prchal JT. End-tidal carbon monoxide as an indicator of the hemolytic rate. Blood Cells Mol Dis. 2015;54(3):292–6. https://doi.org/10.1016/j.bcmd.2014.11.018(PubMed PMID: 25624169).
Cremona G, Asnaghi P, Baderna P, Brunetto A, Brutsaert T, Cavallaro C, Clark TM, Cogo A, Donis R, Lanfranchi P, Luks A, Novello N, Panzetta S, Perini L, Putnam M, Spagnolatti L, Wagner H, Wagner PD. Pulmonary extravascular fluid accumulation in recreational climbers: a prospective study. Lancet. 2002;359(9303):303–9.
Dempsey JA, Reddan WG, Birnbaum ML, Forster HV, Thoden JS, Grover RF, Rankin J. Effects of acute through life-long hypoxic exposure on exercise pulmonary gas exchange. Respir Physiol. 1971;13(1):62–89 Epub 1971/10/01 PubMed PMID: 5112830.
Faulkner JA, Daniels JT, Balke B. Effects of training at moderate altitude on physical performance capacity. J Appl Physiol. 1967;23(1):85–9.
Fryers GR, Berlin NI. Mean red cell life of rats exposed to reduced barometric pressure. Am J Physiol. 1952;171(2):465–70 Epub 1952/11/01 PubMed PMID: 13007817.
Garvican L, Martin D, Quod M, Stephens B, Sassi A, Gore C. Time course of the hemoglobin mass response to natural altitude training in elite endurance cyclists. Scand J Med Sci Sports. 2012;22(1):95–103. https://doi.org/10.1111/j.1600-0838.2010.01145.x(Epub 2010/06/22. PubMed PMID: 20561279).
Garvican-Lewis LA, Sharpe K, Gore CJ. Time for a new metric for hypoxic dose? J Appl Physiol. 2016;121(1):352–5. https://doi.org/10.1152/japplphysiol.00579.2015(Epub 2016/02/27. PubMed PMID: 26917695).
Gassmann M, Muckenthaler MU. Adaptation of iron requirement to hypoxic conditions at high altitude. J Appl Physiol. 2015;119(12):1432–40. https://doi.org/10.1152/japplphysiol.00248.2015(PubMed PMID: 26183475).
Hannon JP, Vogel JA. Oxygen transport during early altitude acclimatization: a perspectiv study. Eur J Appl Physiol Occup Physiol. 1977;36(4):285–97.
Hentze MW, Muckenthaler MU, Galy B, Camaschella C. Two to tango: regulation of Mammalian iron metabolism. Cell. 2010;142(1):24–38.
Hohenhaus E, Paul A, McCullough RE, Kücherer H, Bärtsch P. Ventilatory and pulmonary vascular response to hypoxia and susceptibility to high altitude pulmonary oedema. Eur Respir J. 1995;8(11):1825–33.
Huff RL, Lawrence JH, Siri WE, Wasserman LR, Hennessy TG. Effects of changes in altitude on hematopoietic activity. Medicine (Baltimore). 1951;30(3):197–217 PubMed PMID: 14881989.
Kjellberg SR, Rudhe U, Sjostrand T. Increase of the amount of hemoglobin and blood volume in connection with physical training. Acta Physiol Scand. 1949;19(2–3):146–52.
Klausen K, Dill DB, Horvath SM. Exercise at ambient and high oxygen pressure at high altitude and at sea level. J Appl Physiol. 1970;29(4):456–63. https://doi.org/10.1152/jappl.1970.29.4.456(Epub 1970/10/01. PubMed PMID: 5459913).
Landaw SA. Factors that accelerate or retard red blood cell senescence. Blood Cells. 1988;14(1):47–59.
Levine BD, Stray-Gundersen J. “Living high-training low”: effect of moderate-altitude acclimatization with low-altitude training on performance. J Appl Physiol. 1997;83(1):102–12.
Lundby C, Millet GP, Calbet JA, Bärtsch P, Subudhi AW. Does ‘altitude training’ increase exercise performance in elite athletes? Br J Sports Med. 2012;46(11):792–5.
Mairbäurl H. Red blood cells in sports: effects of exercise and training on oxygen supply by red blood cells. Front Physiol. 2013. https://doi.org/10.3389/fphys.2013.00332.
Mairbäurl H, Weber RE. Oxygen transport by hemoglobin. Compr Physiol. 2012;2(2):1463–89.
Mairbäurl H, Schobersberger W, Oelz O, Bärtsch P, Eckardt KU, Bauer C. Unchanged in vivo P 50 at high altitude despite decreased red cell age and elevated 2,3-DPG. J Appl Physiol. 1990;68(3):1186–94.
Merino CF. Studies on blood formation and destruction in the polycythemia of high altitude. Blood. 1950;5(1):1–31 PubMed PMID: 15396777.
Milledge JS. Renin-Aldosterone System. In: West JB, Lahiri S, editors. High altitude and man. Bethesda: Williams & Wilkins; 1984. p. 47–57.
Milledge JS. Salt and water control at altitude. Int J Sports Med. 1992;13(Suppl 1):S61–3.
Milledge JS, Bryson EI, Catley DM, Hesp R, Luff N, Minty BD, Older MW, Payne NN, Ward MP, Withey WR. Sodium balance, fluid homeostasis and the renin-aldosterone system during the prolonged exercise of hill walking. Clin Sci (Lond). 1982;62(6):595–604.
Ohi H, Tamano M, Sudo S, Okada N. Recombinant EPO therapy increases erythrocyte expression of complement regulatory proteins. Am J Kidney Dis. 2003;41(1):179–85. https://doi.org/10.1053/ajkd.2003.50002(Epub 2002/12/25. PubMed PMID: 12500235).
Olsen NV. Ventilation, hypocapnia and hypoxia: Effects on renal function. In: Houston CS, Coates G, editors. Hypoxia: women at high altitude. Burlington: Queen City Printers; 1997. p. 284–99.
Olsen NV, Hansen JM, Kanstrup IL, Leyssac OO. Renal hemodynamics, tubular function, and response to low-dose dopamine during acute hypoxia in humans. J Appl Physiol. 1993;74(5):2166–73.
Pace N, Meyer LB, Vaughan BE. Erythrolysis on return of altitude acclimatized individuals to sea level. J Appl Physiol. 1956;9(2):141–4 PubMed PMID: 13376417.
Prommer N, Thoma S, Quecke L, Gutekunst T, Volzke C, Wachsmuth N, Niess AM, Schmidt W. Total hemoglobin mass and blood volume of elite Kenyan runners. Med Sci Sports Exerc. 2010;42(4):791–7. https://doi.org/10.1249/mss.0b013e3181badd67(Epub 2009/12/03. PubMed PMID: 19952848).
Rasmussen P, Siebenmann C, Diaz V, Lundby C. Red cell volume expansion at altitude: a meta-analysis and Monte Carlo simulation. Med Sci Sports Exerc. 2013;45(9):1767–72. https://doi.org/10.1249/MSS.0b013e31829047e5PubMed PMID: 23502972.
Reynafarje C, Lozano R, Valdivieso J. The polycythemia of high altitudes: iron metabolism and related aspects. Blood. 1959;14(4):433–55.
Rice L, Ruiz W, Driscoll T, Whitley CE, Tapia R, Hachey DL, Gonzales GF, Alfrey CP. Neocytolysis on descent from altitude: a newly recognized mechanism for the control of red cell mass. Ann Intern Med. 2001;134(8):652–6 PubMed PMID: 11304105.
Rifkind RA. Destruction of injured red cells in vivo. Am J Med. 1966;41(5):711–23 (Epub 1966/11/01 PubMed PMID: 5332170).
Risso A, Turello M, Biffoni F, Antonutto G. Red blood cell senescence and neocytolysis in humans after high altitude acclimatization. Blood Cells Mol Dis. 2007;38(2):83–92. https://doi.org/10.1016/j.bcmd.2006.10.161(PubMed PMID: 17188915).
Risso A, Ciana A, Achilli C, Antonutto G, Minetti G. Neocytolysis: none, one or many? A reappraisal and future perspectives. Front Physiol. 2014;5:54. https://doi.org/10.3389/fphys.2014.00054(PubMed PMID: 24592241; PubMed Central PMCID: PMCPMC3924315).
Rodriguez FA, Iglesias X, Feriche B, Calderon-Soto C, Chaverri D, Wachsmuth NB, Schmidt W, Levine BD. Altitude training in elite swimmers for sea level performance (Altitude Project). Med Sci Sports Exerc. 2015;47(9):1965–78. https://doi.org/10.1249/mss.0000000000000626(Epub 2015/01/30. PubMed PMID: 25628173).
Rogers SC, Said A, Corcuera D, McLaughlin D, Kell P, Doctor A. Hypoxia limits antioxidant capacity in red blood cells by altering glycolytic pathway dominance. FASEB J. 2009;23(9):3159–70. https://doi.org/10.1096/fj.09-130666(PubMed PMID: 19417084; PubMed Central PMCID: PMCPMC2735367).
Rusko HK, Tikkanen HO, Peltonen JE. Altitude and endurance training. J Sports Sci. 2004;22(10):928–44.
Sawka MN, Convertino VA, Eichner ER, Schnieder SM, Young AJ. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med Sci Sports Exerc. 2000;32(2):332–48.
Schmidt W, Prommer N. Impact of alterations in total hemoglobin mass on VO2max. Exerc Sport Sci Rev. 2010;38(2):68–75.
Siebenmann C, Cathomen A, Hug M, Keiser S, Lundby AK, Hilty MP, Goetze JP, Rasmussen P, Lundby C. Hemoglobin mass and intravascular volume kinetics during and after exposure to 3454-m altitude. J Appl Physiol. 2015;119(10):1194–201. https://doi.org/10.1152/japplphysiol.01121.2014(PubMed PMID: 25749449).
Siebenmann C, Robach P, Lundby C. Regulation of blood volume in lowlanders exposed to high altitude. J Appl Physiol. 2017;123(4):957–66. https://doi.org/10.1152/japplphysiol.00118.2017(Epub 2017/06/03. PubMed PMID: 28572493).
Song J, Sundar K, Gangaraju R, Prchal JT. Regulation of erythropoiesis after normoxic return from chronic sustained and intermittent hypoxia. J Appl Physiol. 2017;123(6):1671–5. https://doi.org/10.1152/japplphysiol.00119.2017(Epub 2017/05/20. PubMed PMID: 28522758).
Stray-Gundersen J, Levine BD. Live high, train low at natural altitude. Scand J Med Sci Sports. 2008;18(Suppl 1):21–8.
Sutton JR. Exercise training at high altitude: does it improve endurance performance at sea level? Gatorade Sports Sci Inst. 1993;6:45–58.
Swenson ER, Bärtsch P. High-altitude pulmonary edema. Compr Physiol. 2012;2(4):2753–73. https://doi.org/10.1002/cphy.c100029(PubMed PMID: 23720264).
Swenson ER, Maggiorini M, Mongovin S, Gibbs JSR, Greve I, Mairbäurl H, Bärtsch P. Pathogenesis of high-altitude pulmonary edema: inflammation is not an etiologic factor. J Am Med A. 2002;287(17):2228–35.
Sylvester JT, Shimoda LA, Aaronson PI, Ward JP. Hypoxic pulmonary vasoconstriction. Physiol Rev. 2012;92(1):367–520.
Trial J, Rice L, Alfrey CP. Erythropoietin withdrawal alters interactions between young red blood cells, splenic endothelial cells, and macrophages: an in vitro model of neocytolysis. J Investig Med. 2001;49(4):335–45. https://doi.org/10.2310/6650.2001.33899(PubMed PMID: 11478410).
Viault F. Sur la quantite d’oxygene contenue dans la sang des animoux des hauts plateaux de l’Amerique du Sud. CRH Acad Sci Paris. 1891;112:295.
Wachsmuth NB, Volzke C, Prommer N, Schmidt-Trucksass A, Frese F, Spahl O, Eastwood A, Stray-Gundersen J, Schmidt W. The effects of classic altitude training on hemoglobin mass in swimmers. Eur J Appl Physiol. 2013;113(5):1199–211. https://doi.org/10.1007/s00421-012-2536-0(Epub 2012/11/10. PubMed PMID: 23138148).
Wachsmuth N, Kley M, Spielvogel H, Aughey RJ, Gore CJ, Bourdon PC, Hammond K, Sargent C, Roach GD, Sanchez RS, Claros JC, Schmidt WF, Garvican-Lewis LA. Changes in blood gas transport of altitude native soccer players near sea-level and sea-level native soccer players at altitude (ISA3600). Br J Sports Med. 2013;47(Suppl 1):i93–9. https://doi.org/10.1136/bjsports-2013-092761(Epub 2014/01/15. PubMed PMID: 24282216; PubMed Central PMCID: PMCPMC3903154).
Weil JV, Byrne-Quinn E, Sodal IE, Friesen WO, Underhill B, Filley GF, Grover RF. Hypoxic ventilatory drive in normal man. J Clin Invest. 1970;49(6):1061–72. https://doi.org/10.1172/JCI106322(PubMed PMID: 5422012; PubMed Central PMCID: PMCPMC322574).
Wenger RH, Kurtz A. Erythropoietin. Compr Physiol. 2011;1(4):1759–94. https://doi.org/10.1002/cphy.c100075(Epub 2011/10/01. PubMed PMID: 23733688).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mairbäurl, H. Kinetics of Changes in Hemoglobin After Ascent to and Return from High Altitude. J. of SCI. IN SPORT AND EXERCISE 2, 7–14 (2020). https://doi.org/10.1007/s42978-019-00044-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42978-019-00044-2